Professional Documents
Culture Documents
Bowel Obstructions
Bowel Obstructions
Uploaded by
Dicky Aditya DwikaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bowel Obstructions
Bowel Obstructions
Uploaded by
Dicky Aditya DwikaCopyright:
Available Formats
BY :
1.DICKY ADITYA DWIKA
2.MARADEWI MAKSUM
Bowel obstruction occurs when the normal
propulsion and passage of intestinal contents
does not occur. This obstruction can involve
only the small intestine (small bowel
obstruction), the large intestine (large bowel
obstruction), or via systemic alterations,
involving both the small and large intestine
(generalized ileus).
The "obstruction" can involve a mechanical
obstruction or, in contrast, may be related to
ineffective motility without any physical
obstruction, so-called functional obstruction,
"pseudo-obstruction," or ileus.
This term is used to define intestinal
obstruction caused by a physical blockage
of the intestinal lumen. This blockage may
be intrinsic or extrinsic to the wall of the
intestine or on occasion may occur
secondary to luminal obstruction arising
from the intraluminal contents.
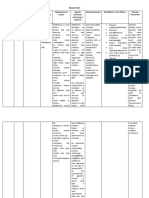
Lesions Extrinsic to the
Intestinal Wall
Lesions Intrinsic to the
Intestinal Wall
ADHESIONS:
Post-operative, Congenital, Postinflammatory
CONGENITAL:
Intestinal atresia, Meckels
diverticulum, duplications
HERNIA:
H. External abdominal wall, H.
Internal, H. Incisional
INFLAMMATORY:
Chrons disease, eosinophilic
granuloma
CONGENITAL:
Annular pancreas, malrotation,
Omphalomesenteric duct remnant
INFECTIONS:
Tuberculosis, actinomycosis,
complicated diverticulitis
NEOPLASTIC:
Carcinomatosis, Extraintestinal
neoplasm
NEOPLASTIC:
Primary or metastatic neoplasms,
appendicitis
INFLAMMATORY:
Intra-abdominal abscess, Starch
peritonitis
MISCELLANEOUS:
Intussusception, endometriosis,
radiation stricture, intramural
hematoma, ischemic stricture
MISCELLANEOUS:
Volvulus, Gossypiboma, Superior
mesentric artery syndrome
INTRALUMINAL/OBTURATOR
OBSTRUCTION:
Gallstone, enterolith, phytobezoar,
parasite infestaion, swallowed foreign
body
When the obstruction is secondary to
factors that cause either paralysis or
dysmotility of intestinal peristalsis that
prevents coordinated aboral transit of
luminal contents, the obstruction is called a
functional or pseudo-obstruction. With
functional obstruction, no physical site of
mechanical obstruction is present.
The most common cause is POSTOPERATIVE ILEUS
It is correlate with the degree of surgical trauma as well
as the type of operation.
Different anatomic segments of the
gastrointestinal tract also recover at
different rates after manipulation and
trauma.
The small bowel recovers within several
hours post-operatively. Stomach within one
day later. Colon about 3-5 days later.
Intra-Abdominal Causes
Extra-Abdominal Causes
INTRAPERITONEAL
PROBLEMS:
peritonitis, intra-abdominal
abscess, post-operative ,
chemical (gastric juice, bile,
blood), Autoimmune (Serositis,
vasculitis) & Intestinal ischemia
(arterial or venous, sickle cell
disease)
METABOLIC ABNORMALITIES:
Electrolyte imbalance, sepsis,
lead poisoning, porphyria,
hyperglicemia, hypothiroidsm,
uremia
RETROPERITONEAL
PROBLEMS:
Urolithiasis, pyelonefphritis,
metastasis, pancreatitis,
retroperitoneal trauma
THORACIC PROBLEMS:
Myocardial infarction, congestive
heart failure, pneumonia, thoracic
trauma
MEDICINES:
opiates, anti-cholinergic, alphaadrenergik agonists,
antihistamines
MISCELLANEOUS:
Spinal cord injury, pelvic fracture,
Luminal obstruction results in prominent
alterations of the normal intestinal
physiology. Despite the many changes
noted, the pathophysiology of bowel
obstruction remains incompletely
understood. Bowel distension, decreased
absorption, intraluminal hypersecretion, and
alterations in motility are found universally,
yet the mechanisms responsible for these
pathophysiologic derangements are not
clear.
Mechanical bowel obstruct
DISTENTION
BOWEL
Early phases of obstruct, accumulates gas from
swallowed air (75% nitrogen).
The next phases, gas arise from the fermentation of
sugars, production of carbon dioxide by interaction of
gastric acid and bicarbonates in pancreatic and biliary
secretions, and diffusion of oxygen and carbon
dioxide from the blood.
Intestinal motility are disruption of the normal
autonomic parasympathetic (vagal) and
sympathetic splanchnic innervation.
Early phase of bowel obstruction,
Intestinal contractile activity increases propel
intraluminal contents past the obstruction
Later phase of bowel obstruction,
The contractile activity diminishes intestinal wall hypoxia
exaggerated intramural inflammation
Distention
of the bowel lumen with a
concomitant results in increased
transmural pressure on capillary
blood flow within the wall of the bowel risk
ischemic.
of
Intestinal wall ischemia is real concern in Large
Bowel Obstruction. The Ascending
Colon luminal diameter is the greatest and
(by Laplace's law) the wall tension (and ischemia)
is also the greatest high risk to ischemia.
Upper small intestine gram-positive facultative
organisms in small concentrations, <106
colonies/mL. More distally, in the distal ileum the
bacterial count increases in concentration to about
108 colonies/mL, the flora primarily coliforms and
anaerobic organisms
in the presence of obstruction, a rapid proliferation
of bacterial organisms occurs consisting
predominantly of fecal-type organisms. reaching a
plateau of 1091010 colonies/mL after 1248 hours of
an established obstruction.
Bacterial toxins have an important role in the
mucosal response to bowel obstruction .
The
diagnosis of bowel obstruction is
suspected clinically based on the presence
of classic signs and symptoms and then
confirmed by some form of imaging test,
such as abdominal radiography or more
recently by computed tomography. The
etiology can often be pinpointed by careful
history-taking complemented with imaging
studies.
You might also like
- Pharmacology Questions With AnswersDocument84 pagesPharmacology Questions With AnswersAquiles Vaesto100% (9)
- NURS 1566 Clinical Form 3: Clinical Medications WorksheetsDocument1 pageNURS 1566 Clinical Form 3: Clinical Medications WorksheetsAdhaNo ratings yet
- IB Psychology Option: Abnormal - Revision NotesDocument4 pagesIB Psychology Option: Abnormal - Revision NotesNoor MohsinNo ratings yet
- Laboratory Test Report: Test Name Result Biological Reference Interval Serum Status: TriglyceridesDocument1 pageLaboratory Test Report: Test Name Result Biological Reference Interval Serum Status: TriglyceridesUpender Rao SunkishalaNo ratings yet
- Disturbed Sleep PatternDocument3 pagesDisturbed Sleep PatternYah Genn QuibenNo ratings yet
- Acute Intestinal Obstruction...Document42 pagesAcute Intestinal Obstruction...Ali100% (2)
- Systemic Consequences of IleusDocument13 pagesSystemic Consequences of IleusranirahmaniNo ratings yet
- Problem 5 GIT Kelompok 16Document116 pagesProblem 5 GIT Kelompok 16Andreas AdiwinataNo ratings yet
- Large Bowel Obstruction by Nic MDocument42 pagesLarge Bowel Obstruction by Nic MRisky OpponentNo ratings yet
- Intestinal Obstruction PDFDocument7 pagesIntestinal Obstruction PDFmist73No ratings yet
- Bowel ObstructionDocument36 pagesBowel ObstructionResti Fratiwi FitriNo ratings yet
- Intestinal Obstruction AditiDocument67 pagesIntestinal Obstruction Aditiaditi BahugunaNo ratings yet
- Intestinal Diseases in Cattle 2023Document30 pagesIntestinal Diseases in Cattle 2023Krystyna WędrychowskaNo ratings yet
- Intestinal ObstructionDocument47 pagesIntestinal ObstructionAstrid Kurniawati AyuningtyasNo ratings yet
- Intestinal ObstructionDocument74 pagesIntestinal Obstructionmehroksukhwinder439No ratings yet
- Problem 4 GIT Josephine AngeliaDocument35 pagesProblem 4 GIT Josephine AngeliaAndreas AdiwinataNo ratings yet
- Intestinal Obstruction: EpidemiologyDocument11 pagesIntestinal Obstruction: EpidemiologyBereket temesgenNo ratings yet
- Intestinal ObstructionDocument157 pagesIntestinal ObstructionOmar SuleimanNo ratings yet
- Acquiredintestinalileus 131003164413 Phpapp01Document53 pagesAcquiredintestinalileus 131003164413 Phpapp01fandiroziNo ratings yet
- 9 Intestinal ObstructionDocument7 pages9 Intestinal ObstructionMAH pedNo ratings yet
- Problem 5 GIT AndreasDocument114 pagesProblem 5 GIT AndreasAndreas AdiwinataNo ratings yet
- Pathologies of GitDocument50 pagesPathologies of GitSajjad AliNo ratings yet
- გაუვალობაDocument37 pagesგაუვალობაMalak A MahadeenNo ratings yet
- Intestinal ObstructionDocument48 pagesIntestinal ObstructionMahmoud AbuAwadNo ratings yet
- Intestinal ObstructionDocument9 pagesIntestinal ObstructionMuhammad Fuad Jaafar100% (1)
- K26 Ileus ObsDocument18 pagesK26 Ileus ObsmitrajoeNo ratings yet
- MODULE 2 - Diseases and MalfunctionsDocument47 pagesMODULE 2 - Diseases and MalfunctionsVicKy AmaliaNo ratings yet
- Intestinal Diseases: Gastrointestinal shengjing Hospital of Medical youwei kou (寇有为)Document80 pagesIntestinal Diseases: Gastrointestinal shengjing Hospital of Medical youwei kou (寇有为)Abhirami AnilNo ratings yet
- NCM 3260 - Gastro - Intestinal ObstructionDocument36 pagesNCM 3260 - Gastro - Intestinal ObstructionCherish Marie HurbodaNo ratings yet
- Ocluzia IntestinalDocument56 pagesOcluzia Intestinalgabi12cNo ratings yet
- Paralytic Ileus: Prepared By: Laurence A. Adena, ManDocument43 pagesParalytic Ileus: Prepared By: Laurence A. Adena, ManJanah Beado PagayNo ratings yet
- Chronic Diarrhoea SaqlainDocument116 pagesChronic Diarrhoea SaqlainMohammed SaqlainNo ratings yet
- Acute Gastritis CiciDocument43 pagesAcute Gastritis CiciDwi Rezky AmaliaNo ratings yet
- Intestinal ObstructionDocument42 pagesIntestinal ObstructionSaurabh SharmaNo ratings yet
- Peptic Ulcer DiseaseDocument36 pagesPeptic Ulcer DiseaseRamanujam Sekar100% (1)
- Intestinal ObstructionDocument46 pagesIntestinal ObstructioninnocentsagemambweNo ratings yet
- Intestinal Obstruction: MSU Medical Students. Batch 2. Group 2Document31 pagesIntestinal Obstruction: MSU Medical Students. Batch 2. Group 2Qp Nizam100% (2)
- Problem 4 GITDocument94 pagesProblem 4 GITArioNo ratings yet
- Small Bowel: Alaa MaaliDocument78 pagesSmall Bowel: Alaa MaaliHalima AssiNo ratings yet
- INTESTINAL OBSTRUC PremierDocument52 pagesINTESTINAL OBSTRUC Premierapi-19641337No ratings yet
- Van Der Aa July 2012Document8 pagesVan Der Aa July 2012ValNo ratings yet
- Obstruction EDocument10 pagesObstruction ECorina MunteanuNo ratings yet
- Surgical ConditionsDocument116 pagesSurgical ConditionsFan EliNo ratings yet
- Intestinal ObstructionDocument9 pagesIntestinal ObstructionHamss AhmedNo ratings yet
- Intestinal Obstruction (PBL) (Teaching)Document40 pagesIntestinal Obstruction (PBL) (Teaching)Nur FadzilahNo ratings yet
- "Peptic Ulcer": Presented By, Archana Devi M.Sc. (N) 1 Year EconDocument27 pages"Peptic Ulcer": Presented By, Archana Devi M.Sc. (N) 1 Year EconArchana VermaNo ratings yet
- StomachDocument204 pagesStomachrajmv7No ratings yet
- Askep Ileus Paralitik PDFDocument12 pagesAskep Ileus Paralitik PDFniaNo ratings yet
- Management of Upper GI BleedingDocument70 pagesManagement of Upper GI BleedingaboubakarylwabukobaNo ratings yet
- Intestinal Obstruction: by Dr. Shereen Abd El-MoniemDocument44 pagesIntestinal Obstruction: by Dr. Shereen Abd El-MoniemフセインNo ratings yet
- Abdominal Wall Defects: Omphalocele and Gastroschisis: DR - Enono Yhoshu Department of Pediatric SurgeryDocument42 pagesAbdominal Wall Defects: Omphalocele and Gastroschisis: DR - Enono Yhoshu Department of Pediatric SurgeryYogi drNo ratings yet
- Esophageal DisordersDocument37 pagesEsophageal DisordersDanielle FosterNo ratings yet
- GastroenteritisDocument20 pagesGastroenteritisSuresh ThanneruNo ratings yet
- NCMB 316 M1 Cu2Document14 pagesNCMB 316 M1 Cu2shawdino03No ratings yet
- GI Notes For Exam 3Document4 pagesGI Notes For Exam 3cathyNo ratings yet
- I Digestive SystemDocument45 pagesI Digestive SystemAhmed - SawalhaNo ratings yet
- Dr. Arif Gunawan Teguh WDocument64 pagesDr. Arif Gunawan Teguh WarifgteguhNo ratings yet
- 58.intestinal ObstructionDocument18 pages58.intestinal ObstructionAdenegan Adesola RaymondNo ratings yet
- Intestinal ObstructionDocument52 pagesIntestinal ObstructionArcr BbNo ratings yet
- Gastrointestinal Fistula: DR Vihar Kotecha M.D, M.MED Gen Surg (Nbi), FCS Gen Surg (ECSA) Lecturer CUHASDocument60 pagesGastrointestinal Fistula: DR Vihar Kotecha M.D, M.MED Gen Surg (Nbi), FCS Gen Surg (ECSA) Lecturer CUHASSangija kamataNo ratings yet
- Paralytic IleusDocument2 pagesParalytic Ileusrjalavazo100% (2)
- Intestinal Obstruction in Paediatrics - James GathogoDocument21 pagesIntestinal Obstruction in Paediatrics - James GathogoMalueth Angui100% (1)
- Lect 3 Disorder of Mouth and EsophagusDocument42 pagesLect 3 Disorder of Mouth and EsophagusShayan ShayanNo ratings yet
- Dr. Pankaj Kumar Assistant Professor Surgical GastroenterologyDocument39 pagesDr. Pankaj Kumar Assistant Professor Surgical GastroenterologyIlham Suryo Wibowo AntonoNo ratings yet
- Diverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandDiverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesRating: 1 out of 5 stars1/5 (1)
- Apley's System of Orthopaedics and Fractures 9th EdDocument7 pagesApley's System of Orthopaedics and Fractures 9th EdDicky Aditya DwikaNo ratings yet
- Memory Test Performance On Analogous Verbal and Nonverbal Memory Tests in Patients With Frontotemporal Dementia and Alzheimer's DiseaseDocument8 pagesMemory Test Performance On Analogous Verbal and Nonverbal Memory Tests in Patients With Frontotemporal Dementia and Alzheimer's DiseaseDicky Aditya DwikaNo ratings yet
- Chest X-Ray: Haemothorax: Erect Haemothorax: ErectDocument1 pageChest X-Ray: Haemothorax: Erect Haemothorax: ErectDicky Aditya DwikaNo ratings yet
- 06 - 200hiperkolesterolemia Bagaimana Peran HesperidinDocument5 pages06 - 200hiperkolesterolemia Bagaimana Peran HesperidinTosanajikuNo ratings yet
- Test Your Knowledge About Pneumonia - ProProfs QuizDocument8 pagesTest Your Knowledge About Pneumonia - ProProfs QuizNaresh Kumar SoniNo ratings yet
- Cane Corso PDFDocument3 pagesCane Corso PDFjesus Ortiz100% (1)
- Greco 2007Document4 pagesGreco 2007Martha RodriguezNo ratings yet
- Childhood Immunizations: Department of PediatricsDocument17 pagesChildhood Immunizations: Department of PediatricsLyrah AlbertoNo ratings yet
- Vaginal Medications Vaginal MedicationsDocument4 pagesVaginal Medications Vaginal MedicationsSilpa Jose TNo ratings yet
- Patenting in BiotechnologyDocument6 pagesPatenting in BiotechnologyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Drug Study #1Document7 pagesDrug Study #1Sarah Kaye BañoNo ratings yet
- Bone Marrow TransplantationDocument21 pagesBone Marrow TransplantationMorrison George100% (1)
- Oral Contra Ceptive S Pills: Famlily PlanningDocument6 pagesOral Contra Ceptive S Pills: Famlily PlanningnutriNo ratings yet
- Best Practice Statement AuditDocument2 pagesBest Practice Statement Auditns officeNo ratings yet
- ActaHortic 2005 680 19Document6 pagesActaHortic 2005 680 19JithinNo ratings yet
- The University of The West Indies Faculty of Medical Sciences Department of Clinical Medical Sciences Years 5 Medicine ClerkshipDocument4 pagesThe University of The West Indies Faculty of Medical Sciences Department of Clinical Medical Sciences Years 5 Medicine ClerkshipRyubusa HayabusaNo ratings yet
- Six Principle of Cavity PreparationDocument6 pagesSix Principle of Cavity PreparationAsma MustafaNo ratings yet
- Deepak Kademani - Improving Outcomes in Oral Cancer - A Clinical and Translational Update-Springer International Publishing (2020)Document189 pagesDeepak Kademani - Improving Outcomes in Oral Cancer - A Clinical and Translational Update-Springer International Publishing (2020)Shantanu DixitNo ratings yet
- ++serrapeptase The Miracle EnzymeDocument2 pages++serrapeptase The Miracle EnzymeabazanNo ratings yet
- Family Centered CareDocument39 pagesFamily Centered Caredinda pristyNo ratings yet
- Science Test For Grade 6Document12 pagesScience Test For Grade 6Umme EiliyahNo ratings yet
- Pcog LabDocument244 pagesPcog LabdavenNo ratings yet
- Addis Ababa University School of Graduate StudiesDocument90 pagesAddis Ababa University School of Graduate StudiesRuth BekeleNo ratings yet
- EthambutolDocument1 pageEthambutolSibel ErtuğrulNo ratings yet
- Autism EnglishDocument129 pagesAutism EnglishRaí Caetano de JesusNo ratings yet
- Brain Death & Organ ProcurementDocument10 pagesBrain Death & Organ ProcurementkencheenNo ratings yet
- What Are Negative Ions?Document4 pagesWhat Are Negative Ions?Kedar KelkarNo ratings yet
- Drugs and DosagesDocument30 pagesDrugs and DosagesvanessaNo ratings yet
- Juvenile DermatomyositisDocument22 pagesJuvenile DermatomyositisEmily EresumaNo ratings yet