Professional Documents
Culture Documents
Designing Hospital For Better Infection Control
Designing Hospital For Better Infection Control
Uploaded by
Mohd Salahuddin0 ratings0% found this document useful (0 votes)
16 views13 pagesThe document discusses guidelines for hospital design to minimize infection transmission. It recommends separating clean and dirty areas, adequate ventilation, and single-bed patient rooms. Specific areas like OT, ICU, wards should be isolated from general traffic. Wards should have separate clean and dirty corridors. Handwashing stations should be conveniently placed. The OPD, ICU, OT and other departments should follow ventilation and isolation guidelines to control infections. Proper zoning and air flow is important in critical areas like OT.
Original Description:
Hai
Original Title
Hai
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses guidelines for hospital design to minimize infection transmission. It recommends separating clean and dirty areas, adequate ventilation, and single-bed patient rooms. Specific areas like OT, ICU, wards should be isolated from general traffic. Wards should have separate clean and dirty corridors. Handwashing stations should be conveniently placed. The OPD, ICU, OT and other departments should follow ventilation and isolation guidelines to control infections. Proper zoning and air flow is important in critical areas like OT.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
16 views13 pagesDesigning Hospital For Better Infection Control
Designing Hospital For Better Infection Control
Uploaded by
Mohd SalahuddinThe document discusses guidelines for hospital design to minimize infection transmission. It recommends separating clean and dirty areas, adequate ventilation, and single-bed patient rooms. Specific areas like OT, ICU, wards should be isolated from general traffic. Wards should have separate clean and dirty corridors. Handwashing stations should be conveniently placed. The OPD, ICU, OT and other departments should follow ventilation and isolation guidelines to control infections. Proper zoning and air flow is important in critical areas like OT.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 13
Designing Hospital for
better Infection Control
The physical design of hospital is an essential
component of a hospitals infection control strategy,
incorporating infection control issues to minimize the
risk of infection transmission.
Hospital design therefore, needs to consider the
separation of dirty and clean areas, adequate
ventilation, lighting and storage facilities and
design of patient accommodation areas, including
adequate number of wash hand basins and
single bed facilities.
Planning parameters (an e.g of 250
bedded)
Most of the hospitals in developing countries
are not
scientifically designed, physical facilities are most inadequate
and wards are overcrowded.
The design should support functional segregation of OPD,
inpatients, diagnostic services and supportive services so that
mixing of patient flow is avoided.
Separation of critical areas like OT, ICU from general traffic
and avoidance of air movement from areas like laboratories
and infectious diseases wards towards critical areas.
The design should support concept of zoning and ventilation
standards in acute care areas.
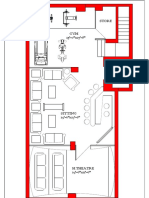
WARDS
The clean corridor and dirty corridor should not be
adjacent and they should facilitate traffic flow of clean and
dirty items separately.
Isolation wards for infectious cases to be kept out of
routine circulation.
Adequate number of wash hand basins should be
provided within the patient care areas and nursing stations
with a view to facilitate hand washing practice.
Separate arrangements for garbage and infectious
waste removal from wards and departments in the form of
separate staircases and lifts.
Construction of isolation rooms within the wards including
ICU and acute care areas.
Provision of airlock and anteroom before entering into
critical care area
A general ward was planned based on bed strength
ranging from 24-32 beds on rigs pattern where 2 single bed
rooms, 2 four bedded rooms and rest 6 bedded rooms were
Floor space area per bed -7 sqm excluding central
corridor of 2.4 meters.
Single bed rooms were given 14 sqm
Distance between centers of beds in 6 bedded rooms
-2.5 meters
Dirty utility and soiled linen room of size 10.5
sqm per ward with facilities for bed pan sink
Water supply of hot and cold water was catered and in
addition janitors closet of 3.5 sqm for keeping mops
and detergents was provisioned in each ward
There should be a sufficient number of single rooms (at
least one per 100 Beds) with adequately filtered airconditioning which should have external exhaust
systems
OPD
WC male- 1 per 100 person
Urinal- 1 per 50 person
WC female- 2 per 100 person
Wash basins 1 for every 100 male and 1 for every
100 female
Waiting-1 sq. ft per average daily patient with
minimum 400 sq. ft (37 sq. m)area to be provided
The clinics for infectious and communicable diseases
should be located in isolation
provided by
independ3ent access.
ICU
No. of ICU- 5-10% of total bed numbers
Ventilation including positive and negative pressure ventilation for
high risk patients and sufficient storage and utility space
American Institute of Architects (AIA) guidelines for new
constructions recommends the minimum number of hand washing
facilities for patients, as one in the toilet room plus having a
sink in patients room, will support infection control practices.
Air lock is supposed to have following functions:
a) They provide a barrier against loss of pressurization and against
entry / exit of contaminated air into / out of the isolation room.
b) They provide a controlled environment in which protective garments
can be donned without contamination before entry into the room.
c) They also provide a physical and psychological barrier to control
behavior of staff in adopting infection control practices.
ICU is planned with 15 air changes per hour (5 fresh + 10
re-circulation) as per minimum ASHRAE standards
Automatic air curtain has been planned at the air lock and entry
into patient care area in ICU, acute care wards, OT sterile area,
neonatal ICU, delivery suites.
OT
There is a general agreement that the factors affecting
occurrence of infection in operation theatres are siting and
design of OT, ventilation, temperature, staff discipline, use of
protective clothing and cleaning programme.
British Medical Council has recommended the following basic
requirements for control of infections in OT:
a) Separation from general traffic and air movement of
hospital.
b) Zoning i.e. sequence of increasingly clean zones from the
entrance to the operating area with the aim of reaching
absolute asepsis at operating site.
c) Easy movement of staff from one clean area to another
without passing through dirty areas.
d) Removal of dirty materials from the suite without passing
through clean areas.
Objectives of ventilation system in OT are recommended to be
as follows :a) To dilute the bacteria generated by the operating
team and patients in the theatre by appropriate air
volume changes.
b) To prevent less clean air from neighboring rooms
entering the OT by using different air pressures.
c) To create an air flow pattern that carries
contaminated air away from the operating table.
d) To provide a comfortable environment for the operating
team and patients with controlled temperature, humidity
and ventilation.
One separate dedicated AHU designed to maintain positive
pressure gradient so as to ensure flow of air from sterile to
clean and protective zone. Aluminium air conditioning ducts
with differential pressure gauge / manometer across HEPA
filters so as to detect clogging or reduced flow of air.
No shelves will be provided inside OT.
Recommended floor surface is epoxy resin flooring, Epoxy flooring
has been found to be seamless, scratch proof, hard enough for
wheeled trolleys, stain free and antistatic.
Laminar flow which is a low turbulence downward displacement air
flow towards the operation zone through stainless steel perforated
grill.
Air curtains at the entry of sterile zone.
Drains, sewerage pipes and water line have been avoided at least
near and above OT sterile zones.
Handwash Bays should be provided in the
following ratios:
Intensive/ Critical Care Units - one per
enclosed room, one per two open Bays
Emergency Unit - one per four open bays
Other patient treatment areas generally staff should not be more than
10 -12 metres from a Hand wash Bay.
You might also like
- Folded PlatesDocument12 pagesFolded PlatesMohd Salahuddin100% (1)
- Ancillary ServicesDocument88 pagesAncillary ServicesSangeeta BSR0% (1)
- Guideline For Ideal OT LayoutDocument36 pagesGuideline For Ideal OT Layoutjake369100% (2)
- Planning and Designing of OTDocument42 pagesPlanning and Designing of OTPaul Priyaraj100% (3)
- Operating RoomDocument23 pagesOperating RoomTheresa Bread86% (7)
- Design of Isolation RoomDocument3 pagesDesign of Isolation Room791221No ratings yet
- ADW PP Perdalin 2020 VentilasiDocument51 pagesADW PP Perdalin 2020 VentilasiNursidahNo ratings yet
- Peri-Operative Care (Theatre Nursing) : Learning ObjectivesDocument21 pagesPeri-Operative Care (Theatre Nursing) : Learning ObjectivesGabriel GagaNo ratings yet
- Isolated Inpatient Ward of 50 Beds: Plan, Staff Organise and Develop AnDocument8 pagesIsolated Inpatient Ward of 50 Beds: Plan, Staff Organise and Develop AnakinravNo ratings yet
- Differences Between HVAC For Hospitals and That For Other BuildingsDocument29 pagesDifferences Between HVAC For Hospitals and That For Other BuildingsMostafa Elmaghraby 467No ratings yet
- Physical Environment (Household Cleaning) : 5.2 VentilationDocument12 pagesPhysical Environment (Household Cleaning) : 5.2 VentilationliuslinoNo ratings yet
- ADW Presentasi Desain Ruangan RS Perdalin 2021Document50 pagesADW Presentasi Desain Ruangan RS Perdalin 2021Fergy puspitaNo ratings yet
- OT Complex Design GuidelinesDocument14 pagesOT Complex Design GuidelinesBirupakshya Rout100% (1)
- Designing Ideal Operating Room ComplexDocument7 pagesDesigning Ideal Operating Room ComplexAliyya RifkiNo ratings yet
- Report of Departmental Study On Ot Complex: ObjectivesDocument52 pagesReport of Departmental Study On Ot Complex: Objectivesvvvvtusebt100% (1)
- Faculty of Nursing & Health Science Advance Nursing Nurse 337Document18 pagesFaculty of Nursing & Health Science Advance Nursing Nurse 337Yousef JafarNo ratings yet
- Guide To Infection Control in The HospitalDocument16 pagesGuide To Infection Control in The HospitalpsikubNo ratings yet
- Chapter 1Document67 pagesChapter 1Abel AbebeNo ratings yet
- Premises SanitationDocument80 pagesPremises SanitationKHYATI BHINDENo ratings yet
- Omicron: Public Health Response: Dr.K.Kolanda SwamyDocument30 pagesOmicron: Public Health Response: Dr.K.Kolanda SwamyPramod PatidarNo ratings yet
- Introduction To Theatre Nursing B.MDocument46 pagesIntroduction To Theatre Nursing B.MBwalya MunjiliNo ratings yet
- Chapter 3 - Operating Theater DesignDocument69 pagesChapter 3 - Operating Theater Designmarye agegnNo ratings yet
- Theatre Nursing: By: Gachuhi WangariDocument130 pagesTheatre Nursing: By: Gachuhi WangariJonah nyachae100% (1)
- Designing An Ideal Operating Room Complex: Indian Journal of Anaesthesia 2007 51 (3) : 193-199 Special ArticleDocument7 pagesDesigning An Ideal Operating Room Complex: Indian Journal of Anaesthesia 2007 51 (3) : 193-199 Special ArticleFrederick Atienza ReyesNo ratings yet
- Housekeeping Practices in Offices, Hospital & MallDocument6 pagesHousekeeping Practices in Offices, Hospital & MallSudarshan MoreNo ratings yet
- Designing Effective Ventilation Strategy For An Airborne InfectionDocument18 pagesDesigning Effective Ventilation Strategy For An Airborne InfectionShohei Namjoon LetoNo ratings yet
- CSSDDocument43 pagesCSSDMohd SalahuddinNo ratings yet
- Office of The SecretaryDocument11 pagesOffice of The SecretaryFranchise AlienNo ratings yet
- Nabh Hvac Guidelines - Dr. Nirmal - Lecture Slides - Acrehealth 2017Document52 pagesNabh Hvac Guidelines - Dr. Nirmal - Lecture Slides - Acrehealth 2017senthilarasu5No ratings yet
- Guidelines For Routine Environmental Cleaning of The Operating RoomDocument13 pagesGuidelines For Routine Environmental Cleaning of The Operating RoomYnaffit Alteza UntalNo ratings yet
- Physical Layout The Operating RoomDocument8 pagesPhysical Layout The Operating RoomJunk YardNo ratings yet
- Hospital Isolation Rooms - EnglishDocument46 pagesHospital Isolation Rooms - EnglishRami Allouh Abu OmarNo ratings yet
- Ot OrientationDocument10 pagesOt OrientationKshayna 1234No ratings yet
- Aseptic TechniquesDocument26 pagesAseptic TechniquesShashidhar ShashiNo ratings yet
- Blood Banking ServicesDocument90 pagesBlood Banking Servicessyed salmanNo ratings yet
- Ventilation GuidanceDocument4 pagesVentilation GuidanceEVONNENo ratings yet
- OTDocument7 pagesOTDharmendra Kumar VermaNo ratings yet
- Prevention of Infection in OTDocument12 pagesPrevention of Infection in OTniraj_sdNo ratings yet
- Infection Control and Prevention in ICUDocument26 pagesInfection Control and Prevention in ICUIsiakpona AdaNo ratings yet
- Operating Room 2Document66 pagesOperating Room 2Ogy Ayop Mummy UddinNo ratings yet
- Week-10 - Sterile Admixture ProgramsDocument28 pagesWeek-10 - Sterile Admixture Programssq9ssv6gqhNo ratings yet
- Appasaheb Birnale College of Architecture: Topic: Central Sterile Supply DepartmentDocument25 pagesAppasaheb Birnale College of Architecture: Topic: Central Sterile Supply DepartmentRevati shindeNo ratings yet
- TNSOP - 5.1 Guidelines For Setting Up Isolation Facility/WardDocument5 pagesTNSOP - 5.1 Guidelines For Setting Up Isolation Facility/WardPradeep kumarNo ratings yet
- Operation Theater 1Document24 pagesOperation Theater 1Susmita BeheraNo ratings yet
- DR - Sharad H.Gajuryal JR, MD (Hospital Administration) B.P Koirala Institue of Health Sciences, Dharan, NepalDocument36 pagesDR - Sharad H.Gajuryal JR, MD (Hospital Administration) B.P Koirala Institue of Health Sciences, Dharan, Nepalvartika chaudharyNo ratings yet
- Multi-Speciality Hospital Design@Viruthunagar: Data Collection-Background StudyDocument19 pagesMulti-Speciality Hospital Design@Viruthunagar: Data Collection-Background StudygayathiriNo ratings yet
- HVAC Design For Healthcare Facilities R1Document60 pagesHVAC Design For Healthcare Facilities R1Sagar BahiratNo ratings yet
- Organization of Intensive Care UnitDocument39 pagesOrganization of Intensive Care UnitHarshil Dave100% (2)
- CSSDDocument25 pagesCSSDVikas Sangwan100% (2)
- Infection Prevention in Design and Construction of The Healthcare EnvironmentDocument69 pagesInfection Prevention in Design and Construction of The Healthcare EnvironmentjariyarasheedNo ratings yet
- Theatre TechniqueDocument85 pagesTheatre Techniquestartizo001No ratings yet
- Standar Ruangan Untuk Pelayanan Infeksi Airborne Disease Di Fasyankes Dengan Fasilitas Terbatas, Budiman Bela, 2021-12-8 PDFDocument59 pagesStandar Ruangan Untuk Pelayanan Infeksi Airborne Disease Di Fasyankes Dengan Fasilitas Terbatas, Budiman Bela, 2021-12-8 PDFPPI RSUDBBNo ratings yet
- Theatre and CSSD Issues in Infection Control FINAL DOCUMENTDocument57 pagesTheatre and CSSD Issues in Infection Control FINAL DOCUMENTRanganathan IyerNo ratings yet
- Cleanrooms and Clean AirDocument5 pagesCleanrooms and Clean AirTim SandleNo ratings yet
- HVAC Design For Healthcare Facilities: Course No: M06-011 Credit: 6 PDHDocument60 pagesHVAC Design For Healthcare Facilities: Course No: M06-011 Credit: 6 PDHNelson VargasNo ratings yet
- Ultra Clean Operating TheatreDocument6 pagesUltra Clean Operating Theatreyogi_rulz_4evaNo ratings yet
- Ot Physical Envmt Notes MadeDocument9 pagesOt Physical Envmt Notes Madesaranya amuNo ratings yet
- Intraoperative LectureDocument249 pagesIntraoperative Lecturelouradel100% (1)
- Solutions For PandemicDocument3 pagesSolutions For Pandemicmiis einalemNo ratings yet
- TÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANOFrom EverandTÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANONo ratings yet
- Thermal Performance of BuildingsDocument25 pagesThermal Performance of BuildingsMohd SalahuddinNo ratings yet
- Electrical Services: AR 307: Building Services-IIDocument24 pagesElectrical Services: AR 307: Building Services-IIMohd SalahuddinNo ratings yet
- View EnclosureDocument11 pagesView EnclosureMohd SalahuddinNo ratings yet
- Truss: Submitted By-Roohul AmeenDocument10 pagesTruss: Submitted By-Roohul AmeenMohd SalahuddinNo ratings yet
- Reinforcement: "If Replace Reinforcement in Structure Then What Should Be Next"Document12 pagesReinforcement: "If Replace Reinforcement in Structure Then What Should Be Next"Mohd SalahuddinNo ratings yet
- Typal and Typological Reasoning A Diagrammatic Practice of Architecture PDFDocument25 pagesTypal and Typological Reasoning A Diagrammatic Practice of Architecture PDFMohd SalahuddinNo ratings yet
- Cement Based PaintsDocument16 pagesCement Based PaintsMohd SalahuddinNo ratings yet
- Part-II ORDINANCE (Administrative/General) : Ordinance No. Date and Notifications NosDocument185 pagesPart-II ORDINANCE (Administrative/General) : Ordinance No. Date and Notifications NosMohd SalahuddinNo ratings yet
- Question Paper of PH - D - Entrance Test Paper '1' Session 2013-14Document12 pagesQuestion Paper of PH - D - Entrance Test Paper '1' Session 2013-14Mohd SalahuddinNo ratings yet
- List of AAMC Rented: S. No. District CenterDocument3 pagesList of AAMC Rented: S. No. District CenterMohd SalahuddinNo ratings yet
- Architecture and Planning 4th Feb 2017 180 100: Question Paper Name: Subject Name: Duration: Total MarksDocument18 pagesArchitecture and Planning 4th Feb 2017 180 100: Question Paper Name: Subject Name: Duration: Total MarksMohd SalahuddinNo ratings yet
- Global Green and Healthy Hospitals AgendaDocument44 pagesGlobal Green and Healthy Hospitals AgendaMohd SalahuddinNo ratings yet
- Punjab Technical University: Entrance Test For Enrollment in PH.D ProgrammeDocument17 pagesPunjab Technical University: Entrance Test For Enrollment in PH.D ProgrammeMohd SalahuddinNo ratings yet
- BSES Rajdhani Power LimitedDocument1 pageBSES Rajdhani Power LimitedMohd SalahuddinNo ratings yet
- Architecture Syllabus: PH.D Eligibility Entrance Test (Peet) :2012-13Document7 pagesArchitecture Syllabus: PH.D Eligibility Entrance Test (Peet) :2012-13Mohd SalahuddinNo ratings yet
- BSES RajdhaniDocument1 pageBSES RajdhaniMohd SalahuddinNo ratings yet
- An Analysis of Urban Growth Trends in The Post-Economic Reforms Period in IndiaDocument14 pagesAn Analysis of Urban Growth Trends in The Post-Economic Reforms Period in IndiaMohd SalahuddinNo ratings yet
- University of Bath Journal of Transport Economics and PolicyDocument8 pagesUniversity of Bath Journal of Transport Economics and PolicyMohd SalahuddinNo ratings yet
- GYM1Document1 pageGYM1Mohd SalahuddinNo ratings yet
- Pengaruh Pelatihan Berbasis Mindfulness Terhadap Tingkat Stres Pada Guru PaudDocument11 pagesPengaruh Pelatihan Berbasis Mindfulness Terhadap Tingkat Stres Pada Guru PaudafrilianaNo ratings yet
- PiptazDocument2 pagesPiptazZyrah Ziska Zafra100% (1)
- Posterior Tibialis Tendon Dysfunction (PTTD)Document11 pagesPosterior Tibialis Tendon Dysfunction (PTTD)bigpawn13No ratings yet
- CH3. Focusing On CustomersDocument52 pagesCH3. Focusing On CustomersQuan Trinh100% (1)
- Dapagliflozin LinagliptinDocument13 pagesDapagliflozin Linagliptinkristie.kankenNo ratings yet
- Substance Abuse NclexDocument4 pagesSubstance Abuse NclexCristina Centurion100% (3)
- PAFP Journal - May 59 1 2021 Pages 82 89Document8 pagesPAFP Journal - May 59 1 2021 Pages 82 89ojbutlanganNo ratings yet
- Rourke LaDocument5 pagesRourke LaPrarthana MohapatraNo ratings yet
- Prematurity and Low Birth Weight: Sumaiya Bushra Farzana Mahbub Afrina Anjuman SaimaDocument51 pagesPrematurity and Low Birth Weight: Sumaiya Bushra Farzana Mahbub Afrina Anjuman SaimaBiscuits and milkNo ratings yet
- Infectious Disease Questions 1Document36 pagesInfectious Disease Questions 1Jelly BeansNo ratings yet
- MS Ii MT2Document11 pagesMS Ii MT2Rika MaeNo ratings yet
- Supplemental Request 2019-1-639021 7Document30 pagesSupplemental Request 2019-1-639021 7Devon MahieuNo ratings yet
- Solar Panel Wash SDS NAM enDocument6 pagesSolar Panel Wash SDS NAM enDr. Ghulam FareedNo ratings yet
- SD ReviewDocument16 pagesSD ReviewShreyas WalvekarNo ratings yet
- Sample VerbatimDocument6 pagesSample VerbatimHarsha VincentNo ratings yet
- Occupational and Environmental Health: Prepared by Ms Yasmeen Bibi MR Asif ShahDocument67 pagesOccupational and Environmental Health: Prepared by Ms Yasmeen Bibi MR Asif ShahAamirNo ratings yet
- Therapeutic ApproachesDocument5 pagesTherapeutic ApproachesSneha HudiyaNo ratings yet
- Beamotil Tablet Information LeafletDocument3 pagesBeamotil Tablet Information Leafletadam malikNo ratings yet
- An Update On The Diagnosis and Treatment of LeprosyDocument10 pagesAn Update On The Diagnosis and Treatment of LeprosyChlarissa WahabNo ratings yet
- Ams t17 Rev0 Ucua ReportDocument2 pagesAms t17 Rev0 Ucua ReportJeet SinghNo ratings yet
- NAEMT AMLS CommitteeDocument2 pagesNAEMT AMLS CommitteeJim ThorntonNo ratings yet
- Medley 2018Document67 pagesMedley 2018Tú TúNo ratings yet
- Module 2 Assessing Community Health Needs and Coverage (User's Guide)Document244 pagesModule 2 Assessing Community Health Needs and Coverage (User's Guide)adkittipong100% (1)
- 23rd EADPH Congress Joint With SESPO Authors Abstracts ListDocument3 pages23rd EADPH Congress Joint With SESPO Authors Abstracts ListAdminNo ratings yet
- NURS18 RLE Week2 - Activity - Role Play.1Document2 pagesNURS18 RLE Week2 - Activity - Role Play.1teuuuuNo ratings yet
- Nursing Procedure Checklist: Administering An Eye IrrigationDocument1 pageNursing Procedure Checklist: Administering An Eye IrrigationOrl Trinidad100% (1)
- Dialog Bhs InggrisDocument6 pagesDialog Bhs InggrisDheya AprianiNo ratings yet
- 3.2.2.3 Penyakit AutoimunDocument64 pages3.2.2.3 Penyakit AutoimunKhairani HakimNo ratings yet
- A Rauf (Clinical Pathways) L.MDocument17 pagesA Rauf (Clinical Pathways) L.MShahab AlamNo ratings yet
- Regulatory Framework For Cell Therapies - Europe, US, and JapanDocument60 pagesRegulatory Framework For Cell Therapies - Europe, US, and JapannovrodNo ratings yet