Professional Documents
Culture Documents
Skills Lab Presentation 4
Skills Lab Presentation 4
Uploaded by
skyblueali0 ratings0% found this document useful (0 votes)
40 views32 pagesCopyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
40 views32 pagesSkills Lab Presentation 4
Skills Lab Presentation 4
Uploaded by
skybluealiCopyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 32
The pressure within the superior vena cava,
reflecting the pressure under which the blood
is returned to the superior vena cava and
right atrium.
Determine by the vascular tone, blood
volume, and the ability of the right heart to
receive and pump blood.
Excellent way to evaluate child’s
fluid volume status.
1. Identify the client and explain the procedure.
2. Check for the IV fluid (name, amount, color)
3. Check drip chamber if half full.
4. Check drop factor. (should be KVO)
5. Check tubing for kinks and check insertion
site for complications.
6. Check manometer if working.
7. Check the patients CVP. (normal CVP should
be 2 to 12mmHg)
8. Check again after 15 minutes. The client’s
position should be the same to prevent
inaccuracy of the measurement.
9. Instruct client to report any
complications.
10. Wash hands.
11. Document.
In measuring CVP, the nurse makes certain
that the client is relaxed at the time of the
measurement.
Straining, coughing, or any other activity
that increase the intrathoracic pressure
causes falsely high measurements.
Monitor for any Complications
1. Pneumothorax 5. Fluid overload
2. Phlebitis 6. Sepsis
3. Air embolism 7. Dysrrhythmia
4. Pulmonary 8. Microelectric shock
embolism
Normal CVP – 2 to 12mmhg
Drop in CVP indicates;
Rise in CVP indicates;
• A decrease in • Increase in blood
circulating volume volume due to a
which may result from sudden shift in fluid
fluid imbalance balance
• Hemorrhage or severe • IVF infusion
vasodilation • Renal failure or
• Pooling of blood in the Sodium and H2O
extremities with limited retention
venous return
A process used for patient who
are actually ill and require
short term dialysis or for
patient with end-stage renal
disease who require long term
or permanent therapy
To extract toxic nitrogenous
substance from the blood
To remove excess water
To prevent death
1.Verify the doctor’s order
2.Check for the consent form
3.Prepare the client
-Level of alertness of the patient
-Understanding of the patient
about the procedure
4.Check the vital signs of the patient
5.Prepare the materials to be use
6.Wash hands
7.Wear gloves
8.Put tourniquet to the arm of the patient
9.Clean the insertion site
10.Insert the needle
11.Secure it with micropore tape
12.Remove the tourniquet
13.Start the hemodialysis
When the hemodialysis is done
14.Remove the needle
15.Check for any complication
16.Assess the comfortability of the patient
17.Check the vital signs
18.Wash hands
19.Documentation
Check for redness, swelling, and irritation.
Instruct the client to inform the nurse if any signs
and symptoms are present.
Instruct client to give pressure to the insertion site
if there is bleeding.
The choice procedure for acute
conditions
Is relatively easy to learn , and safe
to perform
Requires minimum equipment and
specially trained nurses
1. Continuous Ambulatory Peritoneal Dialysis:
-> Left in place for 4 to 8hours
2. Continuous Cycle Peritoneal Dialysis:
-> Same as CAPD but different in that it
requires a peritoneal cycling machine
-> 3 cycles done at night and 1 cycle with
an 8hours dwell done in the monitoring
3. Intermittent Peritoneal Dialysis:
-> 10 to 14hours
-> 3 to 4 times a week with peritoneal cycling
machine
To remove toxic substance and
metabolic wastes
To establish normal fluid balance
(by removing excessive fluids)
To restore electrolyte balance
1. Verify the doctor’s order
2. Check the consent form signed by the
patient or family of the patient.
3. Prepare the materials.
4. Identify the client & explain the procedure.
5. Prepare the client
> level of consciousness
> previous experience with dialysis
> assess the understanding of the patient
> relieve patient’s anxiety
6. Check the VS, weight, and serum electrolyte
level are recorded.
7. Ask the patient to void first before the
procedure.
8. Wear Gloves.
9. Insertion of the catheter.
> Clean the site
> Stab wound is in the lower abdomen
(3 to 5cm below the umbilicus)
10. Infused the diasylate into the peritoneal
cavity.
*Diasylate is allowed to flow freely into the
peritoneal cavity.
*5 to 10mins. is usually required for infusion
of 2L of fluid.
11. After infusion of solution, close roller
clamp.
12. Unclamped the draining tube.
* usually draining is completed after 10
to 30 mins. (colorless)
13. Health Teaching.
> instruct the client to notify the nurse
if the draining bottle is almost full.
> instruct the client to notify the nurse
if there is swelling or irritation in the
site.
14. Wash Hands.
15. Document the procedure.
Promote patient comfort during procedure
Maintain peritoneal dialysis fluid infusion
and drainage
Monitor changes in fluid and electrolyte
status, weight changes, vital signs, and
intake and output records
Monitor for any complications
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Textbook Clinical Skills For Paramedic Practice Anz 1E Dianne Inglis Jeff Kennally Ebook All Chapter PDFDocument53 pagesTextbook Clinical Skills For Paramedic Practice Anz 1E Dianne Inglis Jeff Kennally Ebook All Chapter PDFdaniel.willmore318100% (16)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CARTE ABSTRACT FINAL FINAL FINAL Coperta PDFDocument145 pagesCARTE ABSTRACT FINAL FINAL FINAL Coperta PDFCristina LefterNo ratings yet
- CMC On Slim PossibleDocument8 pagesCMC On Slim PossibleIrene MadzNo ratings yet
- DGFHJKDocument3 pagesDGFHJKRavish MalhotraNo ratings yet
- Canine - Leptospirosis Marge PoughDocument1 pageCanine - Leptospirosis Marge Poughw00fNo ratings yet
- Case Study TBDocument4 pagesCase Study TBMichael Baylon DueñasNo ratings yet
- Organophosphate PoisoningDocument31 pagesOrganophosphate Poisoningjosecarlo_masangkay100% (1)
- Ferrous Sulfate MSDSDocument5 pagesFerrous Sulfate MSDSJonathan GonzalesNo ratings yet
- Research Article: Kasturba Gandhi Nursing CollegeDocument5 pagesResearch Article: Kasturba Gandhi Nursing CollegesanthiyasandyNo ratings yet
- Olanzapine Drug StudyDocument5 pagesOlanzapine Drug Studyjohnlester_jlfNo ratings yet
- Drug PresentationDocument9 pagesDrug PresentationAddah, Dhenaraiza H.No ratings yet
- SPM TRIAL 2007 English Paper 2Document19 pagesSPM TRIAL 2007 English Paper 2Raymond Cheang Chee-CheongNo ratings yet
- Ashrae170 - 2017 AddendumDocument18 pagesAshrae170 - 2017 AddendumABHIJITHNo ratings yet
- Physical Therapy in Critically Ill Adult Patients PDFDocument17 pagesPhysical Therapy in Critically Ill Adult Patients PDFSoledad Cayupi TrafilafNo ratings yet
- Iryu.4 Team - Medical.Dragon.E07.1280x720 ENGDocument41 pagesIryu.4 Team - Medical.Dragon.E07.1280x720 ENGcintoyNo ratings yet
- SOPDocument253 pagesSOPMuhammad Younis BhatNo ratings yet
- Reabilitare Dupa AvcDocument91 pagesReabilitare Dupa AvcDiana StancaNo ratings yet
- Neonatal PharmacologyDocument61 pagesNeonatal PharmacologyAnaNo ratings yet
- HIV and Islam Is HIV Prevalence Lower Am PDFDocument6 pagesHIV and Islam Is HIV Prevalence Lower Am PDFPriyo DjatmikoNo ratings yet
- Theory and Science Specimen PaperDocument12 pagesTheory and Science Specimen PaperAhmed Yousef100% (3)
- Journal SeptemberDocument36 pagesJournal Septemberramkumarm05No ratings yet
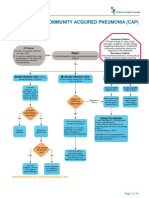
- Complicated Community Acquired Pneumonia Clinical PathwayDocument14 pagesComplicated Community Acquired Pneumonia Clinical PathwayFaisalMuhamadNo ratings yet
- REVIEW SHEET CHAPTER 6 - The Language of MedicineDocument1 pageREVIEW SHEET CHAPTER 6 - The Language of MedicineDaively De Mota JNo ratings yet
- Eye AnatomyDocument21 pagesEye AnatomyHammad afzal100% (2)
- Common Health Problems of Infancy PowptDocument78 pagesCommon Health Problems of Infancy PowptCiella Dela CruzNo ratings yet
- Medical Devices Manufacturing in India:: A Sunrise SegmentDocument2 pagesMedical Devices Manufacturing in India:: A Sunrise SegmentDevasyaNo ratings yet
- IMNCI Chart Booklet (New) OrignalDocument36 pagesIMNCI Chart Booklet (New) OrignaleresdNo ratings yet
- Janumet PM eDocument62 pagesJanumet PM eRaffi DerderianNo ratings yet
- A Seminar Report On Pharmacy ServicesDocument20 pagesA Seminar Report On Pharmacy Servicesrimjhim chauhanNo ratings yet
- Hazelnuts - 7 Benefits of These Heart-Healthy, Brain-Boosting Nuts - DRDocument18 pagesHazelnuts - 7 Benefits of These Heart-Healthy, Brain-Boosting Nuts - DRRajib DasNo ratings yet