Professional Documents
Culture Documents
Comport. Sexual NOU - 2016
Comport. Sexual NOU - 2016
Uploaded by
MohamadMahdiKesserwan0 ratings0% found this document useful (0 votes)
22 views37 pagescompartament sexual Al doilea Curs de S.C.U ( stinta comportament uman ) ...
Original Title
Comport. Sexual NOU- 2016
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentcompartament sexual Al doilea Curs de S.C.U ( stinta comportament uman ) ...
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
22 views37 pagesComport. Sexual NOU - 2016
Comport. Sexual NOU - 2016
Uploaded by
MohamadMahdiKesserwancompartament sexual Al doilea Curs de S.C.U ( stinta comportament uman ) ...
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 37
Comportamentul
sexual
Conf. Dr. Daniel Grigorie
Catedra de Endocrinologie,
UMF Carol Davila,
Institutul C.I.Parhon, Bucureti
ISTORIC
Kamasutra primul tratat explicit de sexologie umana
Kinsey variabilitatea practicilor sexuale la americani
Masters si Johnson : la ambele sexe exista raspunsuri
fiziologice previzibile dupa stimularea sexuala si au
descris ciclul raspunsului sexual normal pe baza caruia
se clasifica disfunctiile sexuale
Freud atribuie problemele sexuale ale adultului
dificultatilor maturarii sexuale in copilarie si dezvoltarii
relatiilor parinte-copil
1980 elucidarea mec. fizico-chimice ale erectiei, care
este consecinta relaxarii muschilor cavernosi si a
cresterii fluxului sg. penian, mediate de NO
INTRODUCERE
Endocrine disease and its treatment can frequently
disturb sexual function in men and women.
In addition, patients may believe, often incorrectly,
that their sexual dysfunction must necessarily be due
to hormonal imbalance and seek management from
endocrinologists.
Patients consider their sexual lives to be important;
recognizing the importance of sexual function as a
determinant of quality of life, the World Health
Organization declared sexual health a fundamental
right of men and women
FAZELE CICLULUI SEXUAL
The traditional model of human sexual response
stemming from the research of Masters, Johnson, and
Kaplan envisioned a linear progression from desire to
arousal to a plateau of high arousal followed by
orgasm/ejaculation, followed by a phase of resolution.
In marked contrast to this earlier model depicting a
linear invariable progression of discrete phases, recent
research conceptualizes sexual response as a
motivation/incentive-based cycle comprising phases of
physiologic response and subjective experience.
The phases of the cycle overlap and their order is
variable
RASPUNSUL SEXUAL ESTE CIRCULAR
Poate incepe cu stimuli nu neaparat sexuali
Dorinta si excitatia co-exista si se potenteaza
reciproc.
In both men and women, the relationship
between desire and arousal is variable and
complex, and both are often unable to
separate the two.
Excitatia subiectiva este mai importanta
decat congestia genitala
Prcesarea cerebrala e esentiala
Even with sufficient sexual motivation and the
presence of adequate stimuli, the arousal and
pleasure may not occur if attention is not focused.
Sexual information is processed in the mind both
automatically and consciousl.The sexual nature of the
stimuli is processed by the limbic system, allowing
genital congestion (observed to be quick and
automatic in women and slower but still involuntary in
men).
Conscious appraisal of the sexual stimuli and the
contextual cues can lead to subjective arousal.
MOTIVATII/STIMULI
The motivations and incentives for sex are multiple and
varied and enhance emotional intimacy between the
partners is important for both men and women.
Depression is a major cause of reduced sexual motivation
in otherwise healthy persons and in those with endocrine
disease: repeatedly, comorbid depression has been
identified as a factor underlying increased sexual
dysfunction in women with diabetes.
Even in the absence of clinical depression, low sexual
interest is associated with having more depressed and
more anxious thoughts and lower sexual self-image than
that in control subjects.
Endocrine disorders can markedly lessen sexual self-image
especially when associated with altered appearances,
infertility, or ability to be gainfully employed.
Physiology of Desire and Arousal
Functional Brain Imaging of Sexual
Arousal in Men and Women
S-au identificat arii activatoare (cortexul orbitofrontal)
si arii inhibitoare
Brain imaging in hypogonadal men before and after
treatment suggests that the left OFC might exert a
testosterone-dependent inhibitory tonic control on
sexual arousal and that this control decreases upon
visual sexual stimulation.
Also the response of the right anterior insula to visual
sexual stimulation was found to depend on the level of
plasma testosterone.
Neurotransmitters and Hormones
Involved in Sexual Desire and
Subjective Arousal
The role of testosterone in desire and arousal is
better documented in men than in women .
Serum levels of testosterone do not correlate with
womens sexual function according to large
epidemiologic studies
A link between low desire and low androgen activity as
reflected by serum testosterone levels or androgen
metabolites has not been identified to date
In animal models, steroid hormones modulate sexual
arousal by directing synthesis of the enzymes and the
receptors for a number of neurotransmitters, including
dopamine, noradrenalin, melanocortin, and
oxytocin.
Modele animale- cai stimulatorii si
inhibitorii
It is thought that dopamine transmission in the
medial preoptic area (MPOA) and the nucleus
accumbens focuses the persons attention on sexual
stimuli (the incentives or motivations for sexual activity) .
It is postulated that the behavioral pattern stimulated by
those systems and the subjective feelings that
accompany them constitute the phenomenon commonly
referred to assexual desire or arousal when genital
sensations triggered by these systems are subjectively
felt
Brain pathways for sexualinhibitioninclude opioid,
endocannabinoid, and serotonin neural transmissions
feeding back to various levels of the excitatory pathways.
It is thought that the behavioral pattern stimulated by
the inhibitory pathways includes both sexual reward
and satiety refractoriness.
Modele animale
Endogenous opioids modulate the feedback effects of sex
steroids on the hypothalamus and pituitary.-Endorphin is
synthesized in the anterior pituitary, the hypothalamus,
and the nucleus of the tractus solitarius in the brainstem.
The sexual inhibiting effects of opioids occur mainly
through their action in the MPOA and the amygdala.
Administration of melanocortin receptor agonists has
been associated with an increase in spontaneous
erections in healthy men and in men with ED, and with
increased desire, but not genital responses, in women.
Oxytocin levels increase close to orgasm. This hormone
is known to be involved in pair bonding in some animal
species, but its relevance in humans is unclear.
Rolul prolactinei
The physiologic role of prolactin in the human sexual
response remains uncertain.
Because a generalized reduction of dopamine activity
in the hypothalamus results in increased prolactin
secretion, it has been difficult to distinguish between
the effects of raised prolactin itself and the possible
effects of the reduced dopamine transmission.
High levels of prolactin are associated with
impaired sexual function in men and women
Genital Sexual Congestion and
Arousal
Men and women differ substantially with respect to the
correlation between genital congestion and subjective
sexual arousal (excitement). Whereas subjective
arousal is typically concordant with genital
congestion in men, there is a poor correlation
between subjective arousal and measures of
genital congestion in women.
There are some exceptions in men: sleep-related
erections are mostly dissociated from erotic dreams or
from subjective sexual arousal.
Also psychophysiologic studies have found that men
can get erections in response to films of assault or rape
while experiencing no subjective arousal.
Physiologic Mechanisms of Penile
Erection
The MPOA of the hypothalamus serves as the
integration site for the central nervous system
control of erections; it receives sensory input from the
amygdala and sends impulses to the paraventricular nuclei
of the hypothalamus and the periaqueductal gray matter.
Neurons in paraventricular nuclei project onto the
thoracolumbar and sacral nuclei associated with
erections.The parasympathetic input to the penis is
proerectile, and sympathetic input is mainly inhibitor
Penile erection results from a series of biochemical and
hemodynamic events that are associated with activation of
central nervous system sites involved in regulation of
erections, relaxation of cavernosal smooth muscle,
increased blood flow into cavernosal sinuses, and venous
occlusion resulting in penile engorgement and rigidity.
The Role of Testosterone in Regulating
Sexual Function in Men
Although androgen-deficient men can achieve penile erections in
response to visual erotic stimuli, their overall sexual activity is
decreased. Spontaneous but not stimulus-bound erections are
testosterone-responsive .Testosterone promotes sexual
thoughts and desire and increases sexual arousal and
attentiveness to erotic auditory and other stimuli . Nocturnal
erections, temporally related to peaks of nighttime testosterone
secretion, are of lower amplitude and duration in androgen-deficient
men, and testosterone therapy increases the frequency, fullness,
and duration of nocturnal penile tumescence. Maximum rigidity
may require a threshold level of androgen
activity.Testosterone regulates nitric oxide synthase (NOS) in the
cavernosal smooth muscle,exerts trophic effects on cavernosal
smooth muscle and ischiocavernosus and bulbospongiosus muscles,
and is necessary for the veno-occlusive response. Androgendeficient men show delayed orgasm and low ejaculatory
volume.
Physiology of Physical Sexual Arousal in
Women: Genital Congestion
A number of physical changes accompany womens
sexual excitement (i.e., their subjective sexual arousal),
including genital swelling, increased vaginal lubrication,
breast engorgement, and nipple erection; increased skin
sensitivity to sexual stimulation; changes in heart rate,
blood pressure, muscle tone, breathing, and temperature;
and mottling of the skin with a sexual flush of
vasodilatation over the chest and face.
These changes are reflexive, mediated by the autonomic
nervous system.
As the clitoris becomes more swollen, it elevates to lie
nearer the symphysis pubis. The vagina lengthens and
dilates during arousal, elevating the uterus. The labia
become swollen and darker red, and the lower third of the
vagina swells.
Physiology of Physical Sexual Arousal in
Women: Genital Congestion
The correlation between genital congestion and
subjective arousal are found to be highly variable.This
is true in sexually healthy women and in women
reporting a lack of desire or arousal or sexual pain.
The physiology of nongenital physical changes and
their correlation with subjective excitement remain
poorly understood.
Physiology of Orgasm
Orgasm is a brain event, triggered typically by genital
stimulation but also by sleep, stimulation of other parts of the
body (including breast and nipple), fantasy, certain
medications, and in women with spinal cord injury,
vibrostimulation of the cervix.
Orgasm is a subjective experience in both men and women,
and it has been difficult to determine an objective marker. In
healthy men, there is the associated ejaculation and, in both
genders, involuntary (reflexive) muscular contractions of the
striated perineal muscles.
The role of oxytocin and prolactin in orgasm is unclear. Both
hormone levels increase at the time of orgasm: PET scanning
has confirmed increased pituitary blood flow in women, but
not in men, at the moment of orgasm. Both hormones can
cause uterine and vaginal smooth muscle contraction, which
may contribute to the sensations of orgasm.
The Revised Definitions of Sexual
Dysfunction in Men
a. Male hypoactive sexual desire disorder
b. ED
c. Premature ejaculation
d. Delayed ejaculation
Male Hypoactive Sexual Desire
Disorder
Androgen deficiency is an important, treatable cause
of HSDD and should be excluded by measuring serum
total testosterone levels.
Erectile Disorder
ED, previously referred to asimpotenceormale ED, is
the inability to attain or maintain an erection or to
achieve penile rigidity sufficient for satisfactory sexual
intercourse.
CVD and ED share common risk factors, such as
diabetes mellitus, obesity, hypertension, smoking, and
dyslipidemia
Recent surveys have revealed an association of lower
urinary tract symptoms (LUTS) with ED
Ejaculatory disorders
Ejaculatory disorders include premature ejaculation,
delayed ejaculation, retrograde ejaculation,
anejaculation/anorgasmia, and painful ejaculation.
Ejaculatory disorders are at least as prevalent and
may be even more prevalent than ED.
Premature ejaculation, defined as ejaculation
associated with lack of or poor ejaculatory control that
causes distress in one or both partners, is the most
prevalent sexual disorder in men 18 to 59 years of age.
Delayed ejaculation refers to inability to ejaculate in a
reasonable period that interferes with sexual or
emotional satisfaction and is associated with distress.
Current Definitions of Sexual
Disorders in Women
Sexual Interest/Arousal Disorder
Female Orgasmic Disorder
Genitopelvic Pain/Penetration Disorder
Persistent Genital Arousal Disorder
Sexual Dysfunction in the Context of
Endocrine Disease
In healthy women, factors such as attitudes toward
sex, feelings for the partner, past sexual experiences,
duration of relationship, and mental and emotional
health have been shown to more strongly modulate
desire and arousability than do biologic factors.
Contrary to gender stereotypes:
-mens physical sexual pleasure was more closely
linked to relational factors than was the case for
women.
-men rated the importance of sex for closeness and
intimacy to their partner more highly than did their
female partners
Androgen Deficiency Syndromes
The testosterone levels required to maintain sexual function
are close to the lower limit of the normal male range.
Androgen deficiency is an important treatable cause of male
HSDD. Therefore, the men diagnosed with HSDD should be
evaluated for androgen deficiency by measurement of
testosterone levels, preferably in an early morning fasting
blood sample.
Although ED and androgen deficiency in men are distinct
disorders with separate pathophysiologic mechanisms, the
two can coexist in the same patient. Testosterone levels
should be measured in men presenting with any form of
sexual dysfunction because androgen deficiency is treatable,
and furthermore, androgen deficiency may be a
manifestation of another underlying disease, such as a
pituitary tumor.
Diabetes and Sexual Dysfunction in
Men
The men with diabetes have significantly lower scores
for sexual desire, activity, arousal, and satisfaction,in
part due to the medical and psychological factors
associated with diabetes, such as the variations in
glycemic control, reduced energy, altered self-image,
and interpersonal difficulties regarding dietary
compliance, glucose monitoring, and medications.
Diabetes also is associated with increased risk of low
testosterone levels.
Endothelial and smooth muscle dysfunction, autonomic
neuropathy, and psychological and interpersonal issues
contribute to sexual dysfunction in men with diabetes
Sexual Dysfunction Associated with
Therapies for Benign Prostatic
Hypertrophy
Benign prostatic hypertrophy is frequently associated
with LUTS and sexual dysfunction
Hyperprolactinemia and Sexual
Dysfunction
Prolactin lowers testosterone levels through its
inhibitory effects on GnRH secretion and on the
pituitary response to GnRH. Most, but not all, men
with sexual dysfunction and hyperprolactinemia have
low testosterone levels.
Whether and how hyperprolactinemia directly affects
erectile function through target organ effects is not
well understood. Erectile function generally improves
in hyperprolactinemic men following treatment with
dopamine agonists.
Sexual Dysfunction in Patients with
Thyroid Disease
Hypothyroidism has been associated with increased
risk of hypoactive sexual desire and ED
Hyperthyroidism has been observed in a small fraction
of men with ED.
Natural Menopause
A majority of women who discontinue postmenopausal
estrogen supplementation develop signs of vulvovaginal
atrophy, which is a risk factor for sexual dysfunction
The traditional notion that maintaining sexual activity
will prevent symptomatic vulvovaginal atrophy has been
refuted. Subjective symptoms and objective signs of
vulvovaginal atrophy correlate poorly.
Epidemiologic studies have not shown an increase in the
prevalence of dyspareunia with age. Clearly not all
postmenopausal women develop sexual symptoms of
estrogen deficiency: of 1525 women followed from age
47 to 54 years, the vast majority were not affected by
the major hormonal shifts.
Natural Menopause
It is likely that multiple factors contribute to sexual symptoms,
including variations in the production of estrogen from adrenal
precursors, the number and sensitivity of estrogen receptors,
and the degree of sexual arousal or excitement at the time of
vulval stimulation and vaginal entry.
Psychological factors rather than estrogen levels were shown
to moderate symptoms when vulvovaginal atrophy is present.
Most studies report a decrease in sexual desire with advancing
age that is not easily explained by hormonal deficiency
The negative association between age and sexual desire was
particularly pronounced in women experiencing little intimacy.
Surgical Menopause
Surgical menopause is a state of both androgen and
estrogen depletion of sudden onset and has often been
viewed as a risk factor for sexual dysfunction. However,
most women undergoing bilateral BSO for benign clinical
indications do not develop sexual dysfunction. Three pro
spective studies found that women choosing BSO plus
hysterectomy for benign indications did not develop sexual
dysfunction over the next 1 to 3 years.
In women undergoing nonelective surgery, the thematic
context of bilateral oophorectomy may impair sexual desire
and function. For example, women who are treated for
malignant disease or those who desire to preserve their
fertility may experience greater distress about low sexual
desire after BSO than those who undergo BSO for benign
conditions.
Hormonal Contraceptives
The estrogen in combined systemic contraceptives
increases SHBG and thus decreases available free
testosterone. The decrease in sexual desire and
subjective arousability in some women receiving oral
contraceptives has been attributed to the decrease in
free testosterone levels.
Polycystic Ovary Syndrome
Limited research has shown that women with
polycystic ovary syndrome may be less sexually
satisfied and may regard themselves as less attractive
than control subjects.
The presumption is that obesity and androgen-related
symptoms may contribute to poor body image, which
may increase the risk of sexual dysfunction.
Recent studies show little evidence that polycystic
ovary syndrome (as opposed to obesity) is a risk
factor for sexual dysfunction.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Salama 1998 The Interproximal Height of Bone - A Guidepost To Predictable Aesthetic Strategies and Soft Tissue Contours in Anterior Tooth ReplacementDocument12 pagesSalama 1998 The Interproximal Height of Bone - A Guidepost To Predictable Aesthetic Strategies and Soft Tissue Contours in Anterior Tooth ReplacementFabiana VillarnoboNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Atlas de Anatomia Anthony B. OlingerDocument52 pagesAtlas de Anatomia Anthony B. OlingerKatia Roxana Quispe CondoriNo ratings yet
- Nursing Board Exam ReviewerDocument32 pagesNursing Board Exam ReviewerRose Anne Mückl100% (9)
- Nilsson 2017Document18 pagesNilsson 2017نذير الشرعبيNo ratings yet
- Angiology: Sanqiang Pan Department of Anatomy Medical College of Jinan UniversityDocument34 pagesAngiology: Sanqiang Pan Department of Anatomy Medical College of Jinan UniversityKw ChanNo ratings yet
- c17 Microbiology Tortora TestbankDocument18 pagesc17 Microbiology Tortora Testbankwhitewave25No ratings yet
- Long-Term Effects of Rapid Maxillary Expansion Followed by Fixed AppliancesDocument5 pagesLong-Term Effects of Rapid Maxillary Expansion Followed by Fixed AppliancesFourthMolar.comNo ratings yet
- BSN - 4C: PresentorsDocument52 pagesBSN - 4C: PresentorsHanya Bint Potawan100% (1)
- Neurosurgical EmergenciesDocument25 pagesNeurosurgical EmergenciesFarah Wahidah Abd RazakNo ratings yet
- Chapter 4 VGO-1 PDFDocument103 pagesChapter 4 VGO-1 PDFPankaj BeniwalNo ratings yet
- New Mbbs 16-05-2018 PDFDocument234 pagesNew Mbbs 16-05-2018 PDFAmoNo ratings yet
- Pituitary PathologyDocument5 pagesPituitary PathologyNada MuchNo ratings yet
- Space Maintainer KgaDocument13 pagesSpace Maintainer KgaSharon LawNo ratings yet
- Bio PoemDocument3 pagesBio Poemapi-4039173890% (1)
- Lab 6td5tbyyvtc1920 RevDocument15 pagesLab 6td5tbyyvtc1920 RevrinidinanNo ratings yet
- Genito Urinary SystemDocument10 pagesGenito Urinary SystemArul ValanNo ratings yet
- Parts of The Eye and FunctionDocument9 pagesParts of The Eye and FunctionEva May Flores-lugoNo ratings yet
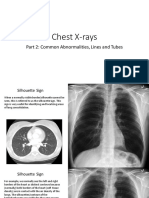
- Chest Xray PT 2Document41 pagesChest Xray PT 2pvs5155No ratings yet
- Diagnosis An Orthodontic CaseDocument126 pagesDiagnosis An Orthodontic Casethanhchon100% (28)
- Occlusion in FPDDocument108 pagesOcclusion in FPDVishal ReddyNo ratings yet
- Anatomy of The HeadDocument2 pagesAnatomy of The HeadVina EmpialesNo ratings yet
- CH 2 Quiz Results CPC AAPCDocument3 pagesCH 2 Quiz Results CPC AAPCBrenda MedinaNo ratings yet
- GAG ReflexDocument4 pagesGAG Reflexdrgayen6042No ratings yet
- Thesis ProtocolDocument11 pagesThesis ProtocolSuyajna JoshiNo ratings yet
- Description of Reproductive System of Indian Water Scorpion, Laccotrephes Maculatus Fabr. (Hemiptera, Heteroptera: Nepidae)Document13 pagesDescription of Reproductive System of Indian Water Scorpion, Laccotrephes Maculatus Fabr. (Hemiptera, Heteroptera: Nepidae)Kanhiya MahourNo ratings yet
- Development of Eye and EarDocument33 pagesDevelopment of Eye and Earkritimahajan1989100% (1)
- Management of Haemorrhage in Oral Surgery: V.K.VigneshDocument3 pagesManagement of Haemorrhage in Oral Surgery: V.K.VigneshadikaNo ratings yet
- 62-File Utama Naskah-253-1-10-20220416Document9 pages62-File Utama Naskah-253-1-10-20220416dw21541No ratings yet
- Physical & Chemical InjuriesDocument201 pagesPhysical & Chemical Injurieslifeinanutshell0000No ratings yet
- Endocrine System 1: Overview of The Endocrine System and HormonesDocument5 pagesEndocrine System 1: Overview of The Endocrine System and HormonesDance RangersNo ratings yet