Professional Documents
Culture Documents
Sensation: Hearing, Vision, Taste, Touch, and Smell
Sensation: Hearing, Vision, Taste, Touch, and Smell
Uploaded by
Michelle Lindsay0 ratings0% found this document useful (0 votes)
18 views99 pagesThis document discusses normal age-related changes to vision and hearing as well as common eye conditions like cataracts, macular degeneration, and glaucoma. It notes that intact senses are important for safety and involvement as people age but that natural changes can impair function. Common eye conditions are described along with risk factors, symptoms, treatments like surgery or medication, and ways to prevent or manage vision problems. Education is important so older adults understand their conditions and know when to seek help.
Original Description:
Nursing
Original Title
nur225chpt14
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses normal age-related changes to vision and hearing as well as common eye conditions like cataracts, macular degeneration, and glaucoma. It notes that intact senses are important for safety and involvement as people age but that natural changes can impair function. Common eye conditions are described along with risk factors, symptoms, treatments like surgery or medication, and ways to prevent or manage vision problems. Education is important so older adults understand their conditions and know when to seek help.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
18 views99 pagesSensation: Hearing, Vision, Taste, Touch, and Smell
Sensation: Hearing, Vision, Taste, Touch, and Smell
Uploaded by
Michelle LindsayThis document discusses normal age-related changes to vision and hearing as well as common eye conditions like cataracts, macular degeneration, and glaucoma. It notes that intact senses are important for safety and involvement as people age but that natural changes can impair function. Common eye conditions are described along with risk factors, symptoms, treatments like surgery or medication, and ways to prevent or manage vision problems. Education is important so older adults understand their conditions and know when to seek help.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 99
Chapter 14
Sensation: Hearing, Vision,
Taste, Touch, and Smell
Intact Senses
• Allows older adult to accurately perceive
the environment
• Remain involved with other people, places
and objects
• Helps keep older adult saft
Sensory Changes Occur
Naturally as Persons Age
• sensory dysfunction may suffer
– Functional impairment
– Injury
– Social isolation
– Depression
Normal Age-Related Changes of
the Eye
• Normal age-related changes in vision
occur gradually; however, over time
these changes can limit the functional
ability of the older adult
Normal Age-Related Changes of
the Eye
• External changes
• Graying and thinning of the
eyebrows and eyelashes
• Subcutaneous tissue atrophy
wrinkling of skin surrounding the
eyes
• Decreased orbital fat sunken
appearance of eye + sagging of
eyelids
FIGURE 14-2 Normal changes of aging in the eye include a thinning of skin surrounding the eye. Source: National
Eye Institute, National Institutes of Health, 2004.
Normal Age-Related Changes of
the Eye
• Internal changes
– Cornea and lens
• Less endothelial cells on cornea reduced ocular
sensitivity decreased pain response
• Lipid deposits around peripheral cornea arcus senilis
• Lenses thicken + harden
– Yellowish appearance + opacity
– Light to scatter interference with color discrimination
– Increase risk for falls and dangerous night driving
– Reduced space for drainage of aqueous humor
glaucoma
– Impedes accommodation presbyopia
Normal Age-Related Changes of
the Eye
• Internal changes
– Pupil
• Decreased dilation and constriction
• Delayed response difficulty responding to
changes in light
• INCREASED FALL RISK
• Diameter is decreased decreased light
reaching retina
– Iris
• Loses color eyes appear gray or light blue
Normal Age-Related Changes of
the Eye
• Visual acuity
– Diminishes gradually after age 50
– Decreases rapidly after age 70
• Light sensitivity declines with age
– Brightness contrast
– Dark adaptation
– Recovery from glare
Visual Impairment
• Linked with four causes
– Cataracts
– Macular degeneration
– Glaucoma
– Diabetic retinopahy
• Visual impairment = visual acuity 20/20 by
Snellen chart at 20 feet
– Increases with age
• Legal blindness = visual acuity 20/200 by
Snellen chart at 20 feet
– Increases with age
– Peaks at 85 years
FIGURE 14-1 The Snellen chart, used to measure visual acuity. Source: National Eye Institute, National Institutes of
Health, 2004.
Visual Impairment
• Personal cost for older person with
visual impairment
– Loss of independence
– Social isolation
– Depression
– Decreased quality of life
Visual Impairment
• Signs of difficulty with vision
– Squinting or tilting head to see
– Changes in ability to drive, read, watch television,
or write
– Holding objects closer to the face
– Difficulty with color discrimination and walking up
or down stairs
– Hesitation in reaching for objects
– Not being able to find something
(American Society on Aging, 2003)
Age-Related Macular
Degeneration (ARMD)
• Two types
1. Dry (atrophic form)- age related
– Gradual blocking of retinal capillaries
which leads to ischemia and necrotic
macula
– Rods and cones die
• Atrophy
• Retinal pigment degeneration
• Slow progression of visual loss
2. Exudative (wet)
– Serous detachment of pigment epithelium in
the macula occurs
– Fluid and blood collection under the macula
– Results in scar formation and visual distortion
Risk Factors for ARMD
• Age (above the age of 50)
• Cigarette smoking
• Family history of ARMD
• Increased exposure to ultraviolet light
• Caucasian race and light colored eyes
• Hypertension or cardiovascular disease
• Lack of dietary intake of antioxidants and
zinc
(Uphold, 2003; Fine, 2000)
FIGURE 14-3 A. Amsler grid as it appears to a person with normal vision. Source: National Eye Institute, National
Institutes of Health, 2004.
FIGURE 14-3 (continued) B. Amsler grid as it appears to a person with macular degeneration. Source: National
Eye Institute, National Institutes of Health, 2004.
FIGURE 14-4 A. Simulation of vision with macular degeneration. Source: National Eye Institute, National Institutes
of Health, 2004.
FIGURE 14-4 (continued) B. Normal vision. Source: National Eye Institute, National Institutes of Health, 2004.
Treatment for ARMD
• Steroid injections
• Plasmapheresis
• Radiation therapy
• No treatments for the dry form of ARMS
• Wet form may benefit from laser tx to stop
neovasularization and stop leaking blood
vessels
• Surgery- but benefits are limited
ARMD Preventive Measures
• Nurses should encourage
– Wearing ultraviolet protective lenses in sun
– Smoking cessation
– Exercising routinely
– Eating a healthy diet consisting of fruits and
vegetables
– Taking vitamins in divided doses twice a day to
delay progression
• Zinc oxide 80 mgm
• Cupric oxide 2 mg
• Beta carotene 15 mgm
• Vitamin C 500 mgm
• Vitamin E 400 IU
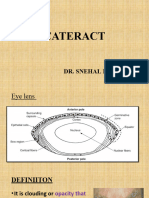
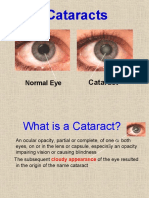
Cataracts
• Lens clouding decreased light to
retina limited vision
• Development is slow and painless
• Leading cause of blindness in the world
• > 50% of adults > 65 years have
cataracts visual problems
Cataracts
• Risk factors
– Increased age
– Smoking and alcohol
– Diabetes, hyperlipidemia
– Trauma to the eye
– Exposure to the sun and UVB rays
– Corticosteroid medications
Cataracts
• Symptoms
– Blurred vision
– Glare
– Halos around objects
– Double vision
– Lack of color contrast or faded colors
– Poor night vision
Education for Older Persons with
Cataracts
• Explanation about cataracts and their
causes
• Symptoms
• No medications available to treat
• Treatment options
– Surgery
Surgery recommended when:
• Visual acuity is 20/50 or less with symptoms of
loss of functional ability
• Visual acuity is 20/40 or better with disabling
glare or frequent exposure to low light situations
or occupational needs
• Cataract removal will treat another lens-induced
disease such as glaucoma
• Cataract exists with other diseases of the retina,
like diabetic retinopathy
Surgery
• Out patient surgical procedure
• Removal of affected lens and insertion of an
artificial lens or intraocular lens
• May do a partial iridectomy
• Usually nonemergency procedure
• Contraindicated when:
– Pt wishes to avoid surgery
– Glasses or visual aids provide satisfactory vision
– pt lifestyle is compromised
– Pt has been diagnosed with medical problems that
make surgery a high risk procedure
Post surgical procedure
• No lifting heavy objects
• No straining for bowel movements
• No bending at the waist
• Eye drops need to be done several times a day
• HOB 30-45 degrees
• Sleep on back or non operative side
• Eye patch
• Patient belongings on non operative side
Complications of Cataract
Surgery
• Infection
• Wound dehiscence
• Hemorrhage
• Severe pain
• Uncontrolled, elevated intraocular pressure
• Special concerns
– Patients with cognitive impairments careful
supervision for at least 24 hours after surgery
• Pt with cognitive impairment must be carefully
supervised for at least 24 hours after surgery to
ensure that they do not remove the protective
eye patch or rub their eye
• If both eyes need to be done, one is done first
and the next one after a month or later
• Adequate home care and support is needed
Education Regarding Cataract
Prevention
• Wearing hats and sunglasses when in
the sun
• Smoking cessation
• Eat a low-fat diet
• Avoid ocular injury
• Education regarding eye drop
administration
Glaucoma
• Increase in intraocular pressure (IOP)
optic nerve damage vision loss
• Open angle
– Slowed flow of aqueous humor through
trabecular meshwork build up
increased IOP damage to optic nerve
fiber loss of vision
– Painless vision loss
• Midperipheral visual field loss
Glaucoma
• Open angle “normal-tension”
– Normal IOP but still damaged optic nerve
visual changes
– Symptoms
• Enlargement of the optic cup
• Nicking of the neuroretinal rim
• Small hemorrhages near the optic disc
Glaucoma
• Angle-closure
– Angle of the iris obstructs drainage of
aqueous humor through trabecular
meshwork increased IOP visual
changes
– Symptoms
• Unilateral headache
• Visual blurring
• Nausea and vomiting
• Photophobia
Risk Factors for Glaucoma
• Increased intraocular pressure
• Normal 10-21 mm Hg
• 50-70 mmHg is very high
• Older than 60 years of age
• Family history of glaucoma
• Personal history of myopia, diabetes,
hypertension, or migraines
• African American ancestry
FIGURE 14-6 A. Simulated glaucoma vision. Source: National Eye Institute, National Institutes of Health, 2004.
Interventions
• Treat acute glaucoma as a medical
emergency
• Medications to lower intraocular pressure
• Peripheral iridectomy- allows aqueous
humor to flow from posterior to anterior
chamber
• Life long eye drops
• Client should wear a medical alert band
• Avoid anticholonergic medications
Interventions
• Client should report
– Eye pain
– Halos around the eyes
– Changes in vision
• If meds fail, need to have surgery
• Surgery is trabeculoplasty- to facilitate aqueous
humor drainage
• surgery is trabeculectomy-to drain into the
conjunctival space
Diabetic Retinopathy
• Microvascular disease of the eye
damage to the ocular microvascular
system impairing transportation of
oxygen and nutrients to the eye in
diabetics
• Two forms
• Nonproliferative
• proliferative
Diabetic Retinopathy
• Nonproliferative
– Endothelial layers of blood vessels in eye
are damaged + development of
microaneurysms leakage edema
near macula impaired vision
Diabetic Retinopathy
• Proliferative
– Damaged blood vessels retinal ischemia
decreased blood supply + nutrient supply to retina
neovascularization fragile blood vessels +
RBC leakage hemorrhage + vision obscured
– Tension exertion on retinal surface + vitreous
body retinal detachment + further damage to
surrounding blood vessels hemorrhage
– Neovascularization of the iris impaired drainage
of the aqueous humor Neovascular glaucoma
Diabetic Retinopathy
• Symptoms
– Gradual vision loss
– Generalized blurring
– Areas of focal vision loss
FIGURE 14-8 A. Simulated diabetic retinopathy vision. Source: National Eye Institute, National Institutes of Health,
2004.
Prevention of Diabetic
Retinopathy
• Tight glycemic control
– Average postparandial 80 to 120 mgm/dL
– Average bedtime capillary blood glucose
100 to 140 mgm/dL
– HbA1c < 7
• Manage hypertension
• Manage hyperlipidemia
Education of Patients with Diabetes
• Proper nutrition
– Low-carbohydrate diet
– Low-cholesterol diet
• Exercise
• Monitoring glucose
Nursing Diagnoses for Vision-
Impaired Older Patients
• Sensory/perceptual alterations: visual
– Encompasses a variety of nursing goals
and interventions communication
• Safety
• Mobility
• Self-care activities
• Mood assessment
Eye Examinations
• Healthy older adults
– Complete eye examination every year
• Visual acuity
• Retina
• Intraocular pressure
• Diabetics
– Complete eye examination every 6 -12
months
Assessment of Vision
• Observe appearance
– Clothing cleanliness
– Self-care
– Indications of bumps and bruises
Interview
• Adequacy of vision
• Recent changes in vision
• Visual problems
– Red eye
– Excessive tearing or discharge
– Headache or feeling of eyestrain when reading or doing close work
– Foreign body sensation in the eye
– New onset of double vision or rapid deterioration of visual acuity
– New onset of haziness, flashing lights, or moving spots
– Loss of central or peripheral vision
– Trauma or eye injury
– Date of last exam
– Inspection
– Movement of eyelids
– Abnormally colored sclera
– Abnormal or absent papillary response
Visual Aids
• Helpful aids for visually impaired
– Low-vision clinics for suggestions
– Telescopic lenses
– Books in Braille
– Computer scanners and readers
– Tinted glasses to reduce glare, large print books and
magazines
– Seeing eye dogs
– Canes
• Often rejected because of the stigma attached
• Very expensive and not covered by Medicare
• Register with Commission for the Blind
– Books on tape and tape player
– Telephones with large numbers
– High-intensity lights
Visual Difficulties May Limit
Independence
• Interference with ability to drive
• Trouble reading and writing
Identification of Safety Problems
at Home
• Provide adequate lighting in high-traffic areas
• Recommend motion sensors to turn on lights
when an older person walks into a room
• Look for areas where lighting is inconsistent;
use proper lampshades to prevent glare
• Use contrast when painting so that walls,
floors, and other structural elements of the
environment can be discriminated easily
• Avoid reflective floors
Identification of Safety
Problems at Home
• Use “hot” colors, such as red, orange, and yellow for
signage
• Urge the use of supplementary lamps near work and
reading areas
• Use red colored tape or paint on the edges of stairs
and in entryways to provide warning and signal the
need to step up or down
• Avoid complicated rug patterns that may overwhelm
the eye and obscure steps and ledges
• Teach the importance of walking slowly when
entering a room
Motor Vehicle Accidents and
Accidental Death
• Leading cause for persons > age 65
• Second leading cause after falls if >
age 75
• Accompany older person to assess
driving
• AARP offers 8-hour safe driving course
• Effects of aging on driving
• Unsafe drivers should be reported to
DMV for road test
Medications with Side Effects of
Visual Disturbance
• Hydroxychloroquine (Plaquenil)—retinopathy,
blurred vision, and difficulty focusing
• Tamoxifen (Nolvadex)—decreased visual acuity
and blurred vision
• Thioridazine (Mellaril)—blurred vision, impaired
night vision, and color discrimination problems
• Levadopa—blurred vision
• Propranolol—dry eyes, visual disturbances
Ophthalmic Solutions with Potential
Adverse Effects
• Beta-blockers (Betagan, Timoptic, Ocupress) (blue or
yellow bottle caps)—bradycardia, congestive heart
failure, syncope, bronchospasm, depression, confusion,
sexual dysfunction
• Adrenergics (Lopidine, Alphagan, Epinal) (purple bottle
caps)—palpitation, hypertension, tremor, sweating
• Mitotics/cholinesterase inhibitors (pilocarpine, Humorsol)
(green bottle caps)—Bronchospasm, salivation, nausea,
vomiting, diarrhea, abdominal pain, lacrimation
Ophthalmic Solutions with Potential
Adverse Effects
• Carbonic anhydrase inhibitors (Trusopt,
Azopt) (orange bottle caps)—fatigue, renal
failure, hypokalemia, diarrhea, depression,
COPD exacerbation
• Prostaglandin analogues (Xalatan,
Lumigan) —changes in eye color and
periorbital tissues, itching
Hearing
• External ear
– Auricle wrinkles and sages
– Increased cerumen production
• Dry pruritis
• Hard
• Decreased apocrine gland activity accumulation
• Inner ear
– Atrophy of organ of Corti and cochlear neurons
– Loss of sensory hair cells
– Degeneration of the stria vascularis
Hearing Loss
• > 30% aged 65 to 76 years
• 50% >75 years
• Older men > older women
• Caucasian men and women > African
American men and women
Hearing Loss
• Risk Factors
– Long-term exposure to excessive noise
– Impacted cerumen (ear wax)
– Ototoxic medications (myosin medicatons
antibiotics)
– Tumors
– Diseases that affect sensorineural hearing
– Smoking
– History of middle ear infection
– Chemical exposure (e.g., long duration of
exposure to trichloroethylene)
Hearing Loss
• Temporary threshold shift (TTS)
– Sounds < 75 dB(A) temporary hearing
loss
– Sounds > 85 dB(A) for 8hrs/day + many
years permanent loss
Conductive Hearing Loss
• Sound unable to be transmitted poor
reception + amplification
– Site of problem
• External or middle ear
Conductive Hearing Loss
• Cause
– Otitis externa
– Impacted cerumen
• Most common and reversible
– Otitis media
– Benign tumors
– Tympanic membrane perforation
– Foreign bodies
– Otosclerosis
Sensorineural Hearing Loss
• Problems with cochlea + auditory nerve
sound distortion
• Causes
– Presbycusis
• Hearing impairment as a result of aging
• Bilateral
• Impaired ability to hear high pitches
• Rare, severe hearing loss or deafness
– Damage as a result of excessive noise exposure
– Meniere’s disease (Meniere's disease is an inner
ear disorder that affects balance and hearing.)
– Tumors
– Infection
Hearing Loss
• Assessment
– History
– Physical examination
• Inspection
• Examination of ear canal
– Childhood ear infections ruptured eardrum
jagged white scars on tympanic membrane in elderly
– Hearing Handicap Inventory for the Elderly
(HHIE-S)
• Talk with family members
Common Hearing Problems in
Older Persons
• Tinnitus
– Objective—pulsatile sounds with turbulent blood
flow through the ear
• Hypertension
• Anemia
• Hyperthyroidism
– Subjective—perception of sound without sound
stimulus
• Medications
• Infections
• Neurological conditions
• Disorders related to hearing loss
Nursing Diagnoses Associated
with Hearing Impairment
• Assessment
– Ability to perform activities of daily living
• Communication
• Driving or taking public transportation
• Safety awareness including the ability to hear
alarms, doorbells
• Engaging in leisure and recreational activities
Drugs with Risk of Hearing
Changes
• Aminoglycoside antibiotics (gentamycin)—
ototoxic
• Antineoplastics (cisplatinum)—ototoxic
• Loop diuretics (Furosemide)—ototoxic
• Baclofen—tinnitus
• Propranolol (Inderal)—tinnitus and hearing
loss
Nursing Diagnoses Associated
with Hearing Impairment
• Diagnosis
– Sensory/perceptual alterations: hearing
with a variety of nursing goals and
interventions
• Communication
• Safety
• Self-care activities
• Mood
• Recreation and leisure activities
Cerumen Impaction
• Hygiene
• Cerumen removal
– Currette
– Lavage or irrigation
FIGURE 14-10 The tip of a bulb irrigation syringe is placed into the external canal.
Hearing Aids
• Documentation on admission
– Type
– Model number
– Serial number
Hearing Aids
• Assessment
– Integrity of the ear mold: Are there cracks or rough
areas? Is there a good fit?
– Battery: Use a battery tester if you have one. Are the
contacts clean? Inserted correctly with + on battery
matched to + in compartment?
– Dials: Are they clean? Easily rotated? Does the
patient report variation of volume when the volume
dial is moved?
– Switches: Do they easily turn on and off? Is there
excessive static or feedback?
– Tubing for behind the ear aids: Are there cracks? Is
there good connection to the earpiece?
Hearing Aids
• Care of hearing aids
– Remove and clean at bedtime
• Warm water or saline
– NO alcohol or harsh soaps
• Use cotton pad
• Carefully remove cerumen
– Disengage battery
– Store in safe place
Hearing Aids
• Other devices
– Cochlear implants
– Assistive listening devices
• Amplifiers in theaters
• Telephone device for the deaf (TDD)
Taste
• Normal changes associated with aging
– Diminished sense of taste
– Thresholds are ~2.5 to 5 times higher in older adults
» Protein
» Salt
» Sweetness
Taste
• Contributing factors to taste alterations
– Oral condition
– Olfactory function
– Medications
– Diseases
– Surgical interventions
– Environmental exposure
– Medical conditions
Taste
• Oral status can affect gustatory function
– Poor dentition improper chewing less
flavor release
– Improperly fitting dentures obstruction
of palate decreased taste perception
– Oral infections release of acidic
substances altered taste + impaired
salivary stimulations decreased ability
for food to dissolve diminished flavor
Taste
• Medications can alter taste sensation by
affecting peripheral receptors and
chemosensory pathways
• Focused assessment for taste disturbances
– Head and neck
– Mucous membranes
– Interview with focus on past dietary habits
Taste
• Education
– Implications of inability to distinguished
between salt and sugar
– Decreased taste lack of motivation to
prepare + eat malnutrition
Xerostomia
• Cause
– Systemic diseases
– Radiation
– Medications
– Sjogren’s syndrome
• Implications
– Altered taste
– Difficulty swallowing Risk for aspiration pneumonia
– Periodontal disease
– Speech difficulties embarrassment social isolation
– Dry lips + dry mucosa increased infection + dental caries
– Halitosis
– Sleeping problems
Nursing Diagnoses Associated
with Taste Impairment
• Sensory/perceptual alterations:
gustatory
• Intake less than necessary for caloric
requirements
Smell
• Thresholds for common odors ~11
times higher for older people
• Structural alterations contribute to loss
of sense of smell
– Upper airway
– Olfactory tract and bulb
– Hippocampus
– Amygdaloid complex
– Hypothalamus
Olfactory Dysfunction
• Statistics
– Males > females
• Causes
– Nasal and sinus disease
– Upper respiratory infection
– Head trauma
– Secondary
• Chemotherapy or other medications
• Radiation
• Current or past use of cocaine or tobacco
• Poor dentition
Olfactory Dysfunction
• Special concerns
– Safety related to smoke and fire
• Malnourishment
• Sense of smell fails to be detected because it
is not adequately tested
– Use three familiar smells
– Repeat with both nostrils, in different orders
• Nursing diagnoses associated with hyposmia
– Sensory/perceptual alterations: olfactory
Nursing Assessment
• Assess safety and preventive measures
• Some medications affect the sense of smell.
• Additional assessment
– Nutrition
– Patient safety
• Date and label all foods
• Place natural gas detectors in the home (for gas heat)
• Place smoke detectors in strategic locations
• Establish schedules for personal hygiene and house
cleaning
• Remove kitchen waste every evening
Strategies to Relieve Xerostomia
• Nonpharmacological
– Diet low in sugar
– Sugar-free candies
– OTC artificial saliva
– Drinking fluids, especially with meals
– Humidifiers
• Pharmacological
– Anticholinergics during the day
– Dividing doses from once a day to twice a day
Appetite Enhancement Strategies
• Coffee stimulates the appetite
• Add flavors
• Check dentures for fit and cleanliness
• Inspect mouth for ulcers or gingivitis
• Review medications
• Encourage fluids
• Maintain bowel records
• Assess palatability of food
Appetite Enhancement Strategies
• Provide a pleasant environment in which
to eat
• Seat residents with others of similar
functional and cognitive levels
• Provide pleasant background music
• Allow for appetizing smells
• Provide clean table settings
• Position small bunch of flowers here and
there
Tactile Sensation
• Diminishes with age
• Decreased ability to detect temperature
extremes
Nursing diagnosis for changes in physical sensations
Sensory/perceptual alterations: tactile
Need for Touch
• Tactile sense interpretation
• Environmental orientation
• Psychological benefits
– Comfort
– Love
• Communication
• Protective by stimulating withdrawal
• Touch can decrease dementia-associated
problems
Nursing Interventions for Older
Persons with Tactile Impairment
• Continuous monitoring of the intactness of the
skin,
– Diabetics should place a mirror on a wall close to floor
examine the bottom of their feet
• Assessment of safety risks
• Development of a safety plan with instructions to
minimize injury
• Water heaters turned down to 110° F.
• Implement teaching guidelines for patients and
families with sensory impairments
You might also like
- Answering NCLEX QuestionsDocument19 pagesAnswering NCLEX QuestionsNorma Zamudio92% (24)
- BCPS Study 10monthDocument5 pagesBCPS Study 10monthMagdy Ali ELsherbenyNo ratings yet
- Clinical Case Report Powerpoint PresentationDocument24 pagesClinical Case Report Powerpoint Presentationapi-354139540100% (1)
- VI Psa Pres Common Eye Conditions2Document58 pagesVI Psa Pres Common Eye Conditions2PopeyeNo ratings yet
- Vi Psa Pres Common Eye Conditions Aug10 3.08.29 PMDocument58 pagesVi Psa Pres Common Eye Conditions Aug10 3.08.29 PMSarthak KabiNo ratings yet
- Chapter 11 Eye & Vision DisordersDocument72 pagesChapter 11 Eye & Vision DisordersMYLENE GRACE ELARCOSANo ratings yet
- Gradual Loss of Vision-Nurses - 065937Document73 pagesGradual Loss of Vision-Nurses - 065937CosbyNo ratings yet
- AMETROPIADocument48 pagesAMETROPIARahul KirkNo ratings yet
- OT 677 Conditions Lecture 3Document66 pagesOT 677 Conditions Lecture 3Yuvaraaj NavaneethakrishnanNo ratings yet
- Age-Related Macular Degeneration: by Lohit Valleru Course - Rehabilitation Engineering Professor - Joel MyklebustDocument34 pagesAge-Related Macular Degeneration: by Lohit Valleru Course - Rehabilitation Engineering Professor - Joel Myklebustlohitv9No ratings yet
- Retina - 4Th SemiDocument14 pagesRetina - 4Th SemiBob BinNo ratings yet
- Dr. Ashraf Sayeed: Department of OphthalmologyDocument49 pagesDr. Ashraf Sayeed: Department of Ophthalmologysaiful haque100% (1)
- Group 9 Mathematics Year Today School YearDocument44 pagesGroup 9 Mathematics Year Today School YearElsie GumocNo ratings yet
- Approach To A Case of CataractDocument18 pagesApproach To A Case of CataractVineet GuptaNo ratings yet
- Lecture 11 Special Senses Part 6-VisionDocument48 pagesLecture 11 Special Senses Part 6-VisionMoses Jr KazevuNo ratings yet
- 1 CataractDocument31 pages1 CataractsnehalNo ratings yet
- Blackboard1 150313105122 Conversion Gate01Document45 pagesBlackboard1 150313105122 Conversion Gate01jessajoy deslateNo ratings yet
- Impaired Vision and BlindnessDocument44 pagesImpaired Vision and BlindnessYujenNo ratings yet
- Cataract: Zarka Wahid Bux Nursing Instructor Siut School of NursingDocument14 pagesCataract: Zarka Wahid Bux Nursing Instructor Siut School of NursingZarka InqlabiNo ratings yet
- Cataract InformationDocument25 pagesCataract Informationvasanth_1515No ratings yet
- Mishermaliyani I11105026Document49 pagesMishermaliyani I11105026Dewi rafikaNo ratings yet
- Ophthalmology Clerks: Alea, Denz Marc Custodio, Audreyfil Perez, Francis MiguelDocument14 pagesOphthalmology Clerks: Alea, Denz Marc Custodio, Audreyfil Perez, Francis MiguelDenz Marc AleaNo ratings yet
- Cataract 3Document11 pagesCataract 3Ravi KushwahaNo ratings yet
- Cataract SenilisDocument54 pagesCataract Senilismayo djitroNo ratings yet
- Cataracts 1Document18 pagesCataracts 1Hno Joseph MulahNo ratings yet
- About 70% of All Sensory Information Reaches The Brain Through The EyesDocument127 pagesAbout 70% of All Sensory Information Reaches The Brain Through The Eyesjoan olanteNo ratings yet
- CataractsDocument47 pagesCataractsNrs Sani Sule MashiNo ratings yet
- Advance Trends in Eye Care: DR Divya Kesarwani Consultant Cataract and Glaucoma ServicesDocument42 pagesAdvance Trends in Eye Care: DR Divya Kesarwani Consultant Cataract and Glaucoma ServicesdrdivyakesarwaniNo ratings yet
- Eye Department Queen Elizabeth HospitalDocument43 pagesEye Department Queen Elizabeth Hospitalarnol3090No ratings yet
- Blindness: Introduction:-Low Vision Is A General Term Describing Visual Impairment That Requires Patients To UseDocument12 pagesBlindness: Introduction:-Low Vision Is A General Term Describing Visual Impairment That Requires Patients To UseaparnaNo ratings yet
- Blindness in The Elderly: - Prevalence Increases Exponentially With Advancing Age - One of The Most Common DisabilitiesDocument72 pagesBlindness in The Elderly: - Prevalence Increases Exponentially With Advancing Age - One of The Most Common DisabilitiesfanyazharNo ratings yet
- Glaukoma Dan KonjungtivitisDocument24 pagesGlaukoma Dan KonjungtivitisAnnisa DeasyNo ratings yet
- 5 Cataract-200605111818Document55 pages5 Cataract-200605111818Ashok TawadeNo ratings yet
- Objective - Subjective Eye Examination-Referral System and When To ReferDocument56 pagesObjective - Subjective Eye Examination-Referral System and When To ReferClara Sainuka100% (1)
- Ent Lesson 8Document45 pagesEnt Lesson 8favourednancie9No ratings yet
- Glaucoma: Diska Astarini I11109083Document49 pagesGlaucoma: Diska Astarini I11109083Nauli PanjaitanNo ratings yet
- Nursing Gerontology: Mrs. Sheryll Liz B. Regis, RN, RM College of Nursing St. Paul University DumagueteDocument170 pagesNursing Gerontology: Mrs. Sheryll Liz B. Regis, RN, RM College of Nursing St. Paul University Dumaguetepetite_chien15No ratings yet
- Examination of EyeDocument39 pagesExamination of EyeDr Sravya M VNo ratings yet
- Glaucoma: Zarieh Dawn Novela Medicine 2Document41 pagesGlaucoma: Zarieh Dawn Novela Medicine 2Zari NovelaNo ratings yet
- L6 Refractive Errors and PaedsDocument37 pagesL6 Refractive Errors and PaedsSofíaGriggsNo ratings yet
- Eyes and Ears DisordersDocument36 pagesEyes and Ears Disordersjeshema100% (4)
- CataractDocument11 pagesCataractFSO MedicNo ratings yet
- Blurred VisionDocument14 pagesBlurred VisionpreezaNo ratings yet
- Opthalmic Emergencies PresentationDocument85 pagesOpthalmic Emergencies PresentationvictoreffiomNo ratings yet
- Cataract: Done by Mo3taz Abu Rabiah A7mad LubaniDocument46 pagesCataract: Done by Mo3taz Abu Rabiah A7mad LubaniMaxwell C Jay KafwaniNo ratings yet
- Visual Impairment SimplifiedDocument2 pagesVisual Impairment SimplifiedJustine Joy SabalboroNo ratings yet
- Cataract: Done by Jony MallikDocument46 pagesCataract: Done by Jony MallikAlfa Suryani ArdliNo ratings yet
- Glaucoma and CataractDocument30 pagesGlaucoma and CataractJayselle ArvieNo ratings yet
- Glaucoma & CataractDocument53 pagesGlaucoma & CataractBenita100% (1)
- HYPERMETROPIA and Myopia PDFDocument55 pagesHYPERMETROPIA and Myopia PDFDrashti ChudasamaNo ratings yet
- Case ReportDocument29 pagesCase ReportRaisa AriesthaNo ratings yet
- Eye Disorders: Structure of The EyeDocument13 pagesEye Disorders: Structure of The Eyeapi-3822433No ratings yet
- Glaucoma 191024141130Document25 pagesGlaucoma 191024141130Broz100% (1)
- Lay Forum NotesDocument7 pagesLay Forum NotesCleoGomezNo ratings yet
- Refractive ErrorsDocument33 pagesRefractive ErrorsMathew Sebastian100% (3)
- CataractDocument11 pagesCataractSubha MaheswariNo ratings yet
- BlindessDocument6 pagesBlindessapi-355019671No ratings yet
- BlindessDocument6 pagesBlindessapi-344623337No ratings yet
- Glaucoma: Defitaria Permatasari I11109005Document46 pagesGlaucoma: Defitaria Permatasari I11109005yusufharkianNo ratings yet
- Retina Nss2013Document46 pagesRetina Nss2013proluvieslacusNo ratings yet
- Common Causes of BlindnessDocument58 pagesCommon Causes of BlindnesskaunaNo ratings yet
- Low Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsFrom EverandLow Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsNo ratings yet
- CRNA Board Preparation ProductsDocument1 pageCRNA Board Preparation ProductsMichelle LindsayNo ratings yet
- Nunsr: ArursrhestaDocument29 pagesNunsr: ArursrhestaMichelle Lindsay100% (1)
- Bacterionomicon Digital PDFDocument77 pagesBacterionomicon Digital PDFMichelle LindsayNo ratings yet
- A Brief Look at Nurse Anesthesia History. Text To Accompany The Aana History Powerpoint PresentationDocument3 pagesA Brief Look at Nurse Anesthesia History. Text To Accompany The Aana History Powerpoint PresentationMichelle LindsayNo ratings yet
- Flowmeters Prodigy AnesthesiaDocument2 pagesFlowmeters Prodigy AnesthesiaMichelle LindsayNo ratings yet
- Anesthesia Machine Self-Study TopicsDocument22 pagesAnesthesia Machine Self-Study TopicsMichelle LindsayNo ratings yet
- The University of Akron Nurse Anesthesia Program: Anesthesia Techniques, Procedures, & Simulation LabDocument2 pagesThe University of Akron Nurse Anesthesia Program: Anesthesia Techniques, Procedures, & Simulation LabMichelle LindsayNo ratings yet
- Anesthetic Delivery SystemsDocument10 pagesAnesthetic Delivery SystemsMichelle LindsayNo ratings yet
- The University of Akron Nurse Anesthesia Program: Anesthesia Techniques, Procedures, & Simulation LabDocument1 pageThe University of Akron Nurse Anesthesia Program: Anesthesia Techniques, Procedures, & Simulation LabMichelle LindsayNo ratings yet
- The University of Akron Nurse Anesthesia Program: Anesthesia Techniques, Procedures, & Simulation LabDocument2 pagesThe University of Akron Nurse Anesthesia Program: Anesthesia Techniques, Procedures, & Simulation LabMichelle LindsayNo ratings yet
- The University of Akron Nurse Anesthesia Program: Anesthesia Techniques, Procedures, & Simulation LabDocument1 pageThe University of Akron Nurse Anesthesia Program: Anesthesia Techniques, Procedures, & Simulation LabMichelle LindsayNo ratings yet
- Airway Management: Airway Suctioning Artificial AirwaysDocument25 pagesAirway Management: Airway Suctioning Artificial AirwaysMichelle LindsayNo ratings yet
- 2019-20 Ohio Hunting & Trapping RegulationsDocument44 pages2019-20 Ohio Hunting & Trapping RegulationsMichelle LindsayNo ratings yet
- YNHH CLABSI.v4Document1 pageYNHH CLABSI.v4Michelle LindsayNo ratings yet
- The University of Akron Nurse Anesthesia Program: Anesthesia Techniques, Procedures, & Simulation LabDocument1 pageThe University of Akron Nurse Anesthesia Program: Anesthesia Techniques, Procedures, & Simulation LabMichelle LindsayNo ratings yet
- Ladue Public LandDocument2 pagesLadue Public LandMichelle LindsayNo ratings yet
- Gerontological Nursing IssuesDocument39 pagesGerontological Nursing IssuesMichelle LindsayNo ratings yet
- CCRN Review Course 2015Document81 pagesCCRN Review Course 2015Michelle LindsayNo ratings yet
- 3.levels of Health CareDocument43 pages3.levels of Health CareNamrah AfzalNo ratings yet
- Case 1Document7 pagesCase 1bsc.clinicalnutrition2018No ratings yet
- Schizophrenia Case StudyDocument14 pagesSchizophrenia Case Studyapi-593859653No ratings yet
- Daftar PustakaDocument6 pagesDaftar Pustakarifa salsabilahNo ratings yet
- Clostridium Difficile InfectionDocument20 pagesClostridium Difficile InfectionTony ZhangNo ratings yet
- Ela Writing Extended Matching Questions FormatDocument9 pagesEla Writing Extended Matching Questions FormatRuth MungaiNo ratings yet
- Management of Acute Chemotherapy-Related Diarrhea - UpToDateDocument19 pagesManagement of Acute Chemotherapy-Related Diarrhea - UpToDateMarius PapuricaNo ratings yet
- Introduction of CytopathologyDocument41 pagesIntroduction of CytopathologyNurul Laili Nahlia86% (7)
- Tetanus, Analysis of 29 Cases - ScienceDirectDocument1 pageTetanus, Analysis of 29 Cases - ScienceDirectNikkole VelascoNo ratings yet
- Therapeutic Drug MonitoringDocument10 pagesTherapeutic Drug MonitoringAnnie SethiNo ratings yet
- Capstone - Tissue EngineeringDocument10 pagesCapstone - Tissue Engineeringapi-373339200No ratings yet
- Definition, Classification, Etiology, and Pathophysiology of Shock in Adults - UpToDateDocument18 pagesDefinition, Classification, Etiology, and Pathophysiology of Shock in Adults - UpToDatePaloma GBNo ratings yet
- Clinical Pharmacy FinalDocument83 pagesClinical Pharmacy FinalAbin ChandrakumarNo ratings yet
- 7 5 16 Physiology of Red Blood CellsDocument72 pages7 5 16 Physiology of Red Blood CellsJoshua NyazonNo ratings yet
- List of Must Read Books and Journals For DNB AnaesthesiaDocument2 pagesList of Must Read Books and Journals For DNB AnaesthesiaSirisha CkvNo ratings yet
- OliclinomelDocument11 pagesOliclinomelDevarajan Melpanaiyur SowmyanarayananNo ratings yet
- Bempedoic Acid: 06-Feb-2020 CreatedDocument56 pagesBempedoic Acid: 06-Feb-2020 CreatedLuis Carlos MillánNo ratings yet
- Comprehensive Report On Rapid Plasma Reagin Test (RPR)Document3 pagesComprehensive Report On Rapid Plasma Reagin Test (RPR)Kim RuizNo ratings yet
- Grade 10 PE DLP 11Document3 pagesGrade 10 PE DLP 11Charles Norman Amparado RodriguezNo ratings yet
- Maste Med SheetDocument78 pagesMaste Med SheetBarbie Wiggers100% (1)
- Bates Chapter 7 - HEENTDocument87 pagesBates Chapter 7 - HEENTGuia De GuzmanNo ratings yet
- The Disabilities of The Arm, Shoulder and Hand (DASH) ScoreDocument2 pagesThe Disabilities of The Arm, Shoulder and Hand (DASH) ScoreMuh RasyidNo ratings yet
- BVAS WG Instructions ManualDocument7 pagesBVAS WG Instructions ManualAbdirahmanNo ratings yet
- New Thesis With Corrections Grad School CorrectionsDocument62 pagesNew Thesis With Corrections Grad School Correctionsapi-535934790No ratings yet
- Nama Prinsipal Kode Produk Nama Produk Unit Stok HNAPPNDocument19 pagesNama Prinsipal Kode Produk Nama Produk Unit Stok HNAPPNTrie WahyuningsihNo ratings yet
- Intoduction To Assistive TechnologyDocument20 pagesIntoduction To Assistive TechnologyMaraka MartinNo ratings yet
- Otitis Media - Pediatrics in Review 2010Document17 pagesOtitis Media - Pediatrics in Review 2010cristobal_daniel_3No ratings yet
- Pharmacotherapeutics For Advanced Practice A Practical Approach Ebook PDFDocument62 pagesPharmacotherapeutics For Advanced Practice A Practical Approach Ebook PDFrosanne.hahn846100% (46)