Professional Documents
Culture Documents
Dengue Hemorrhagic Fever III
Dengue Hemorrhagic Fever III
Uploaded by
Jehrisse L. Soriano-Ocampo0 ratings0% found this document useful (0 votes)
214 views28 pagesThe patient, a 6-year old Filipino male, presented with 6 days of intermittent undocumented fever, epigastric pain, and vomiting. His platelet count was decreasing and he developed hemoconcentration. He was diagnosed with dengue hemorrhagic fever based on his thrombocytopenia, hemoconcentration, and symptoms. DHF can progress to circulatory failure and shock without supportive treatment.
Original Description:
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe patient, a 6-year old Filipino male, presented with 6 days of intermittent undocumented fever, epigastric pain, and vomiting. His platelet count was decreasing and he developed hemoconcentration. He was diagnosed with dengue hemorrhagic fever based on his thrombocytopenia, hemoconcentration, and symptoms. DHF can progress to circulatory failure and shock without supportive treatment.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
214 views28 pagesDengue Hemorrhagic Fever III
Dengue Hemorrhagic Fever III
Uploaded by
Jehrisse L. Soriano-OcampoThe patient, a 6-year old Filipino male, presented with 6 days of intermittent undocumented fever, epigastric pain, and vomiting. His platelet count was decreasing and he developed hemoconcentration. He was diagnosed with dengue hemorrhagic fever based on his thrombocytopenia, hemoconcentration, and symptoms. DHF can progress to circulatory failure and shock without supportive treatment.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 28
Dengue Hemorrhagic Fever III
By: Katrina Tugado and Jehrisse Soriano
Identifying data:
D.A is a 6 year old Filipino male, Roman
Catholic born on September 2, 2003 from
Caloocan City admitted for the first time
on July 25, 2010
Source and Reliability
Parents, both with 85% reliability
Chief complaint:
Fever of six days duration
History of Present Illness
6 days PTA,
The patient had intermittent undocumented
moderate grade fever, the patient was given
Paracetamol syrup 250 mg/5 ml, 10 ml every four
hours (29 mkdose)
Accompanied by epigastric pain not relieved by
food intake
There were also five episodes of vomiting of
previously ingested food amounting to 2
tablespoons/episode
There were no cough, colds, abdominal
distention, diarrhea noted and no consult was done
History of Present Illness
5 days PTA,
There was persistence of undocumented moderate
grade fever
Epigastric pain decreased in frequency
Vomiting was also noted to decrease, 3 episodes were
noted, composed of previously ingested food
amounting to 2 tbsps./ episode
Paracetamol syrup 250 mg/5 ml, 10 ml every four
hours (29 mkdose) was continued
No changes in activity and appetite noted, no consult
was done
History of Present Illness
3 days PTA,
Intermittent undocumented moderate grade fever
persisted
Epigastric pain and vomiting with the same
characteristics as before persisted.
No cough, colds, bleeding and melena were
noted
Consult at Bermudez Polymedic Hospital was
done and the patient was admitted for 1 ½ days
CBC; PC was done which revealed:
History of Present Illness
7/23 (am) 7/23 (pm) 7/24 (am) 7/24 (pm)
Hgb 0.38 0.38 0.41 0.41
Hct 133 133 144 144
WBC 8.6
Segmenters 0.67
Lymphocytes 0.32
Monocytes 0.01
Eosinophils 0
Platelets 320 314 256 220
History of Present Illness
Urinalysis and serum electrolytes were done
but results were unrecalled
Impression was dengue fever and the patient
was advised transfer to a tertiary hospital for
further evaluation and management.
History of Present IIlness
1 day PTA,
The patient was transferred to Tala Hospital,
impression given was also Dengue fever.
CBC was done but with unrecalled results.
He was also given unrecalled medications for
abdominal pain and was advised transfer to a
tertiary hospital hence transfer to NCH
Past Health Maintenance History
(-) PTB
(-) pneumonia
(-) asthma
(-) chicken pox
(-) measles
Gestational History
The mother had no known feto-maternal complications
No intake of medications/ x-ray exposure
Regular PNCUs at 4 months until birth
With regular intake of multivitamins and ferrous
sulfate
Birth History
The patient was born full term via normal spontaneous
delivery at a lying-in clinic to a 26 year old G2P2
(2002) mother.
Neonatal history
(+) spontaneous respiration
(-) jaundice
(-) convulsions
(+) weight gain
Feeding History
Breastfed from 0-2 mos.
Formula fed from 2 mos-1 year old (Nestogen (1:1))
Started on solids at 7 mos.
Previously with good appetite
Multivitamins started at birth until present (Tiki-tiki,
Ceelin)
Present diet: rice, fried chicken, pork
(-) vomiting
(-) food intolerance
Developmental History
Roll over at 6 mos.
Sat alone at 6 mos.
Stood alone at 12 mos.
Walk alone at 15 mos.
Talked at 2 y.o.
Immunization History
1 dose of BCG
3 doses of DPT
3 doses of OPV
3 doses of Hep B
1 dose of measles
Family History
Mother, 32 y/o apparently healthy
Father, 37 y/o apparently healthy
8 y/o male sibling, with dengue fever
(-) PTB
(-) DM
(-) Asthma
(-) Congenital defects
(-) Mental retardation
Physical examination
General survey: awake,afebrile, coherent, not in
cardiorespiratory distress
Vital signs: BP: 80/50 mmHg, CR: 118 bpm, RR: 30,
T: 36.6 C
Anthropometrics: Wt: 17 kgs. Ht: 103 cm
HEENT: Anictric sclerae, pink palpebral sclerae, no
tonsillopharyngeal congestion, no
cervicolymphadenopathies
Thorax and Lungs: Equal chest expansion, decreased
breath sounds at the lower lung fields
CVS: adynamic precordium, normal rate and rhythm,
no murmurs
Abdomen: flat, soft, tenderness on the epigastric area
and right flank, NABS
Extremities: poor pulses, CRT > 4 secs, cold
extremities
Rectal exam: no skin tags, no fissure, with good
sphincter tone, empty rectal vault with yellowish
material upon withdrawal of the examining finger
Abdomen: flat, soft, tenderness on the epigastric area
and right flank, NABS
Extremities: poor pulses, CRT > 4 secs, cold
extremities
Subjective data:
Moderate grade undocumented fever
Epigastric pain
Vomiting
A sibling with the same symptoms
Objective data:
Low Hgb
Low Hct
Decreasing platelet count (NV: 150-450 x 10 9 L)
Tenderness of the epigastric are upon palpation
Poor pulses, CRT > 4 secs, cold extremities
DHF vs. DF
Dengue fever Dengue Hemorrhagic fever
Symptoms: High fever, severe malaise, Same with DF in the early phase of
headache, retroorbital pain, myalgia, illness
lumbosacral pain, accompanied by sore Usually with high fever, hemorrhagic
throat, nausea, vomiting, epigastric pain phenomena, hepatomegaly, circulatory
and diarrhea failure
(in children: abdominal pain and sore
throat are predominant)
Defervescence: 3-8 days usually Defervescence: 2-5 days
followed by minor hemorrhagic
phenomena, others may progress to
severe GI bleeding and shock
Simultaneous or sequential introduction
of two or more serotypes,
Presents with thrombocytopenia (<100,
000) and hemoconcentration
Dengue Hemorrhagic fever
Hepatic enlargement and tenderness is a sign of bad
prognosis.
Other manifestations include pleural effusion and
hypoalbuminemia, encephalopathy with normal
cerebrospinal fluid.
Diffuse capillary leakage of plasma is responsible for
the hemoconcentration
Thrombocytpenia + hemoconcentration
Prognosis:
The case-fatality of DHF/DSS is 10% or higher if
untreated.
With supportive treatment, fewer than 1% of such
cases succumb.
Recovery is rapid and without sequelae
WHO classification:
Grade I - thrombocytopenia + hemoconcentration.
Absence of spontaneous bleeding.
Grade II - thrombocytopenia + hemoconcentration.
Presence of spontaneous bleeding.
Grade III - thrombocytopenia + hemoconcentration.
Hemodynamic instability: filiform pulse, narrowing of
the pulse pressure (< 20 mmHg), cold extremities,
mental confusion.
Grade IV - thrombocytopenia + hemoconcentration.
Declared shock, patient pulseless and with arterial blood
pressure = 0 mmHg (dengue shock syndrome - DSS).
Differentials:
Leptospirosis:
Ruled in:
Fever, abdominal pain, vomiting of six days duration
Malaria
Ruled in:
Daily fever presentation
Ruled out:
Spleen enlargement
Jaundice
You might also like
- Functional Movement Disorder: Kathrin Lafaver Carine W. Maurer Timothy R. Nicholson David L. Perez EditorsDocument455 pagesFunctional Movement Disorder: Kathrin Lafaver Carine W. Maurer Timothy R. Nicholson David L. Perez Editors李世民100% (3)
- Case Presentation - Acute GlomerulonephritisDocument10 pagesCase Presentation - Acute GlomerulonephritisRold Brio Sos100% (1)
- Gaba Tryptophan: Amino Acid Solutions For Anxiety, Sugar CravingsDocument13 pagesGaba Tryptophan: Amino Acid Solutions For Anxiety, Sugar CravingsMirela Olarescu100% (1)
- Vollmer Et Al-1995-Journal of Applied Behavior AnalysisDocument16 pagesVollmer Et Al-1995-Journal of Applied Behavior AnalysisTimiNo ratings yet
- 1chief Complaint: FeverDocument10 pages1chief Complaint: FeverCarla Elize DerainNo ratings yet
- CPC-Patho Version 6Document20 pagesCPC-Patho Version 6Bea SamonteNo ratings yet
- Hemolytic Uremic Syndrome 8.13.18Document34 pagesHemolytic Uremic Syndrome 8.13.18Emily EresumaNo ratings yet
- DengueDocument38 pagesDengueadetiquezNo ratings yet
- Sickle CellDocument47 pagesSickle CellEmily EresumaNo ratings yet
- 'Batangas Medical Center Case Report by PGI Carlos H. AcuñaDocument7 pages'Batangas Medical Center Case Report by PGI Carlos H. AcuñaCarlos H. AcuñaNo ratings yet
- Dengue Hemorrhagic FeverDocument27 pagesDengue Hemorrhagic FeverTristiana DewiNo ratings yet
- IM Case ReportDocument5 pagesIM Case ReportGurungSurajNo ratings yet
- ASD Internship ReportingDocument14 pagesASD Internship ReportingPernel Jose Alam MicuboNo ratings yet
- Case Protocol M&MDocument5 pagesCase Protocol M&Mcharmaine BallanoNo ratings yet
- CPC CaseDocument8 pagesCPC CasePingky khingthongNo ratings yet
- Kavitha K C - A Case Presentation - Nephrotic SyndromeDocument27 pagesKavitha K C - A Case Presentation - Nephrotic SyndromeVishesh ParayilNo ratings yet
- LP DHFDocument14 pagesLP DHFyustiNo ratings yet
- University of The East Ramon Magsaysay Memorial Medical Center, IncDocument3 pagesUniversity of The East Ramon Magsaysay Memorial Medical Center, IncRejaelSenoroNo ratings yet
- Case Report Typhoid FeverDocument37 pagesCase Report Typhoid FeverAnonymous 0SYzMqje2No ratings yet
- Morning Report: Melissa Kleschen, MD, PGY3Document14 pagesMorning Report: Melissa Kleschen, MD, PGY3Emily EresumaNo ratings yet
- DUTY REPORT Igd Ecy AbeDocument21 pagesDUTY REPORT Igd Ecy AbeAsiah AbdillahNo ratings yet
- Imed Case 5Document11 pagesImed Case 5Shakshi RainaNo ratings yet
- Case History: Personal DataDocument5 pagesCase History: Personal DataMohammed AhmedNo ratings yet
- Typhoid FeverDocument68 pagesTyphoid FeverLd Rachel PableoNo ratings yet
- Morning Report 7/15/2015: Sydney Ryan PGY3Document23 pagesMorning Report 7/15/2015: Sydney Ryan PGY3Emily EresumaNo ratings yet
- Acute Abdominal PainDocument14 pagesAcute Abdominal PainTali SteedNo ratings yet
- DengueDocument13 pagesDengueHarshini ChandraboseNo ratings yet
- Hashimotos ThyroiditisDocument9 pagesHashimotos ThyroiditisKristiannlae DanoNo ratings yet
- Emergency Red Flags: DR - Magdy Khames AlyDocument58 pagesEmergency Red Flags: DR - Magdy Khames AlyJerry AbleNo ratings yet
- DENGUE Janice LouieDocument38 pagesDENGUE Janice LouieclikgoNo ratings yet
- Acute Glomerulonephritis GCDocument70 pagesAcute Glomerulonephritis GCMary Cruz100% (2)
- Case Report Dengue Hemorrhagic Fever: Tutor, Dr. Leopold Simanjuntak, Sp.A Presented By, Martha Hapsari (04-066)Document43 pagesCase Report Dengue Hemorrhagic Fever: Tutor, Dr. Leopold Simanjuntak, Sp.A Presented By, Martha Hapsari (04-066)aryhehegaNo ratings yet
- Case Presentation: East Avenue Medical Center Female Surgical Ward Group DDocument32 pagesCase Presentation: East Avenue Medical Center Female Surgical Ward Group DKyle TampoyaNo ratings yet
- CSS DHFDocument40 pagesCSS DHFDina SofianaNo ratings yet
- Lascano, Joanne Alyssa - RheumatologyDocument13 pagesLascano, Joanne Alyssa - RheumatologyJoanne Alyssa Hernandez LascanoNo ratings yet
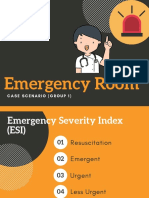
- Emergency Room: Case Scenario (Group 1)Document40 pagesEmergency Room: Case Scenario (Group 1)Victoria Castillo TamayoNo ratings yet
- Hema Case 2Document55 pagesHema Case 2jlcocm-2022-00028No ratings yet
- The Patient Is An Agitated 42Document25 pagesThe Patient Is An Agitated 42Johan Iswara SiagianNo ratings yet
- Case Presentation: Giorgi Kochiashvili, Rupesh Mohanadas, Mohammed Bilal, AbivarmaDocument29 pagesCase Presentation: Giorgi Kochiashvili, Rupesh Mohanadas, Mohammed Bilal, AbivarmaRupesh MohandasNo ratings yet
- Acute Rheumatic FeverDocument37 pagesAcute Rheumatic FeverQadriyah Ramadhani100% (1)
- Enteric Fever 3Document33 pagesEnteric Fever 3Grethel H SobrepeñaNo ratings yet
- Peds Case 3Document5 pagesPeds Case 3Mohammed AhmedNo ratings yet
- Group 2 - Case Child With Severe Measles Pneumonia - DDocument20 pagesGroup 2 - Case Child With Severe Measles Pneumonia - Dazzahra zahidaNo ratings yet
- Dengue Shock SyndromeDocument17 pagesDengue Shock SyndromehwelpNo ratings yet
- Medicine Common Condition Case FilesDocument3 pagesMedicine Common Condition Case Fileszezma GamingNo ratings yet
- CME DengueDocument37 pagesCME Dengueami5687No ratings yet
- PEDIA - TachypneaDocument12 pagesPEDIA - TachypneaAlvin Germo PasuquinNo ratings yet
- NC AninditaDocument20 pagesNC AninditaDodi DiNo ratings yet
- Case Presentation Febrile FitDocument33 pagesCase Presentation Febrile FitNurul Syazwani RamliNo ratings yet
- P Org 6 1Document37 pagesP Org 6 1melbourneichrcNo ratings yet
- Hypertensive Disorder in PregnancyDocument56 pagesHypertensive Disorder in PregnancyESCA Gabriel100% (1)
- Dengu Syndrome & Its Managment - Prof. Kaka1Document39 pagesDengu Syndrome & Its Managment - Prof. Kaka1Aditi SahaNo ratings yet
- WEEK4CASE4INTERNALMEDICINEDocument2 pagesWEEK4CASE4INTERNALMEDICINEINFO MANTICORE DUMMYNo ratings yet
- Sample Case Presentation - Occult BacteremiaDocument51 pagesSample Case Presentation - Occult BacteremiaPrecious Gutierrez BagazinNo ratings yet
- All Peads SEQsDocument14 pagesAll Peads SEQsShifa AminNo ratings yet
- Typhoid Fever: Dr. Dur Muhammad Khan (Mrcp. FRCP)Document52 pagesTyphoid Fever: Dr. Dur Muhammad Khan (Mrcp. FRCP)Osama HassanNo ratings yet
- Duty Report 16 December 2015: GP On Duty: Dr. Ike Dan Dr. Indri Coass On Duty: Dani & NitaDocument22 pagesDuty Report 16 December 2015: GP On Duty: Dr. Ike Dan Dr. Indri Coass On Duty: Dani & NitaNita Juliana AnggrainiNo ratings yet
- Morning Report: Rachel Laarman MD PGY-3Document18 pagesMorning Report: Rachel Laarman MD PGY-3Emily EresumaNo ratings yet
- Empyema ThoracisDocument14 pagesEmpyema ThoracisMara AbantoNo ratings yet
- Duty Report 27 AUGUST 2014: GP On Duty: Dr. Ananita Resident On Duty: Dr. Ardhestiro Co-Ass On Duty: Alvin & TedyDocument22 pagesDuty Report 27 AUGUST 2014: GP On Duty: Dr. Ananita Resident On Duty: Dr. Ardhestiro Co-Ass On Duty: Alvin & TedyAlvin BernardNo ratings yet
- CABRAL Diabetes Mellitus Case Presentation and DiscussionDocument9 pagesCABRAL Diabetes Mellitus Case Presentation and DiscussionCalingalan Hussin CaluangNo ratings yet
- Lupus Case PresentationDocument48 pagesLupus Case PresentationRoscelie KhoNo ratings yet
- Antidiabetic Potential of Acanthaceae Family: Review ArticleDocument8 pagesAntidiabetic Potential of Acanthaceae Family: Review ArticleWulan Klsb6No ratings yet
- CDC Mask MandateDocument3 pagesCDC Mask MandateFOX 17 NewsNo ratings yet
- WaPo 3005Document54 pagesWaPo 3005OrlandoRenzoNo ratings yet
- Dilg Doh Jao 2020 0001Document31 pagesDilg Doh Jao 2020 0001Novie FeneciosNo ratings yet
- HealthKartDocument8 pagesHealthKartSudhanshu GuptaNo ratings yet
- Teratogens: ND THDocument5 pagesTeratogens: ND THMinhwa KimNo ratings yet
- 9.social Health Class 10Document2 pages9.social Health Class 10Juned MulaniNo ratings yet
- Philosophy of SexualityDocument21 pagesPhilosophy of SexualityBrandon Toy100% (1)
- To Tbi 7Document6 pagesTo Tbi 7murtya aulifiaNo ratings yet
- 10 FinishingDocument59 pages10 FinishingMahesh ChanduNo ratings yet
- Personal Development: Quarter 1 Module 1Document31 pagesPersonal Development: Quarter 1 Module 1Earlimar Miechan Abriol100% (15)
- NCP Risk For Bleeding 3Document2 pagesNCP Risk For Bleeding 3Jayson Olile100% (2)
- 800 Ebook Dermatology and DiabetesDocument115 pages800 Ebook Dermatology and DiabetesAhmad ArifNo ratings yet
- HCP Lesson PlanDocument2 pagesHCP Lesson PlanDavid DvoskineNo ratings yet
- A.G Carsico Et Al 2019Document7 pagesA.G Carsico Et Al 2019reclinpharmaNo ratings yet
- Đề Chọn Đội Tuyển Anh 10 - date 4-12-2021Document16 pagesĐề Chọn Đội Tuyển Anh 10 - date 4-12-2021Minh HuyNo ratings yet
- The Relationship Between Liver Enzymes Aspartate Transaminase (AST) and Alanine Transaminase (ALT) With Hepatitis CDocument10 pagesThe Relationship Between Liver Enzymes Aspartate Transaminase (AST) and Alanine Transaminase (ALT) With Hepatitis Csajjad dheyabNo ratings yet
- Drug Resistance Pharmacology Lecture Lecture Series 2019Document23 pagesDrug Resistance Pharmacology Lecture Lecture Series 2019temitopeNo ratings yet
- Who To Complain To About VCU's Handling of COVIDDocument1 pageWho To Complain To About VCU's Handling of COVIDJ.R.R. BradenNo ratings yet
- Herbal Alternatives To Antibiotics From Stephen Harrod Buhner Book Herbal Antibiotics Storey Pub 2011.Document5 pagesHerbal Alternatives To Antibiotics From Stephen Harrod Buhner Book Herbal Antibiotics Storey Pub 2011.Dunat DobricaNo ratings yet
- The Persistent Stigma and Disregard For Mental Health in Sri LankaDocument3 pagesThe Persistent Stigma and Disregard For Mental Health in Sri Lankadevmini herathNo ratings yet
- Ayurvedic Management of Adhd (Attention Deficit Hyperactivity Disorder) - A Case StudyDocument5 pagesAyurvedic Management of Adhd (Attention Deficit Hyperactivity Disorder) - A Case StudyNatseenNo ratings yet
- Lesson Plan-PidDocument10 pagesLesson Plan-PidAmlan jyoti thanapatiNo ratings yet
- Parasitology Review Notes For Medical Technologists: Leishmania SPP)Document39 pagesParasitology Review Notes For Medical Technologists: Leishmania SPP)Kat Jornadal100% (2)
- HOMEWORK1Document9 pagesHOMEWORK1christinejoanNo ratings yet
- Severe Residual Pulmonary Stenosis After Surgical Repair of Tetralogy of Fallot: What's Our Next Strategy?Document11 pagesSevere Residual Pulmonary Stenosis After Surgical Repair of Tetralogy of Fallot: What's Our Next Strategy?International Journal of Innovative Science and Research TechnologyNo ratings yet
- Emotion and The Human Brain: Antonio R. DamasioDocument6 pagesEmotion and The Human Brain: Antonio R. DamasioBruno XavierNo ratings yet