Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
51 viewsGlomerulonephritis: Nameesha Natasha Naidu 20130105
Glomerulonephritis: Nameesha Natasha Naidu 20130105
Uploaded by
AliMalikThis document provides information on glomerulonephritis (GN), including its presentation, causes, types, investigations, management, and details on specific types like minimal change disease, focal segmental glomerulosclerosis, membranous GN, and rapidly progressive GN. GN is inflammation of the glomeruli that can cause nephrotic or nephritic syndrome. It has primary and secondary causes and is investigated via blood tests, urine tests, imaging and renal biopsy. Management involves treating the underlying cause, controlling blood pressure and cholesterol, and immunosuppression.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You might also like
- Nephrotic Syndrome PathophysiologyDocument1 pageNephrotic Syndrome PathophysiologyKrisianne Mae Lorenzo FranciscoNo ratings yet
- Rheumatology Cases Fall Clinics 2019Document85 pagesRheumatology Cases Fall Clinics 2019NaziBrola TsivadzeNo ratings yet
- BloodDocument51 pagesBloodDrShahid Sahito100% (1)
- Malaria MEQDocument6 pagesMalaria MEQMuvenn KannanNo ratings yet
- GlomerulonephritisDocument58 pagesGlomerulonephritisJosa Anggi Pratama0% (1)
- Nephritic Syndrome - Armando HasudunganDocument14 pagesNephritic Syndrome - Armando HasudunganzahraaNo ratings yet
- Nephrotic and Nephritic Syndrome - 2008Document65 pagesNephrotic and Nephritic Syndrome - 2008rikasusanti101001201No ratings yet
- Anca VasculitisDocument12 pagesAnca Vasculitisatul_desai_3100% (2)
- Cirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDocument21 pagesCirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDan ChicinasNo ratings yet
- Glomerular DiseasesDocument37 pagesGlomerular DiseaseskiflomNo ratings yet
- Clinical Approach To RPRF PDFDocument6 pagesClinical Approach To RPRF PDFshankarNo ratings yet
- Pathogenesis of Micro and Macrovascular Complications of DiabetesDocument4 pagesPathogenesis of Micro and Macrovascular Complications of DiabetesFrancesca LiNo ratings yet
- Crush Injury and Crush Syndrome PDFDocument2 pagesCrush Injury and Crush Syndrome PDFMichael DrakeNo ratings yet
- Primary Cardiac LymphomaDocument3 pagesPrimary Cardiac LymphomaHan KethyanethNo ratings yet
- Click To Download E6Document2 pagesClick To Download E6Mona SahuNo ratings yet
- 4 Circulation Disorders PDFDocument69 pages4 Circulation Disorders PDFSetiawan SukmadjaNo ratings yet
- Management of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesDocument7 pagesManagement of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesdaypranitaNo ratings yet
- Nephrotic Syndrome 2016Document45 pagesNephrotic Syndrome 2016alaaNo ratings yet
- NEPHROTIC SYNDROME - HamidDocument20 pagesNEPHROTIC SYNDROME - HamidAbdul Hamid OmarNo ratings yet
- Antiphospholipid Antibody SyndromeDocument37 pagesAntiphospholipid Antibody SyndromeAhmad Reshad AslamNo ratings yet
- Glomerulonephritis Dwi Fin PDFDocument108 pagesGlomerulonephritis Dwi Fin PDFOvyanda Eka MItraNo ratings yet
- PATH - Acute Kidney InjuryDocument12 pagesPATH - Acute Kidney InjuryAyyaz HussainNo ratings yet
- ASCITESDocument25 pagesASCITESGanesh BabuNo ratings yet
- 04 NephrologyDocument19 pages04 NephrologyeuncieNo ratings yet
- Acute Glomerulonep Hritis: By: Edelrose D. Lapitan BSN Iii-CDocument29 pagesAcute Glomerulonep Hritis: By: Edelrose D. Lapitan BSN Iii-CEdelrose Lapitan100% (1)
- Diabetes MellitusDocument79 pagesDiabetes Mellituskhalid saifur rahman khanNo ratings yet
- By: DR Eyad Talal: Moderator: DR I - QudaisatDocument55 pagesBy: DR Eyad Talal: Moderator: DR I - QudaisatEyad AbdeljawadNo ratings yet
- Infective EndocarditisDocument68 pagesInfective EndocarditisDr. Rajesh PadhiNo ratings yet
- Nephrotic Syndrome in Children: January 2013Document7 pagesNephrotic Syndrome in Children: January 2013molenNo ratings yet
- Embryology and Development of KidneyDocument75 pagesEmbryology and Development of Kidneyranjitha sraateNo ratings yet
- EdemaDocument3 pagesEdemaUdaya SreeNo ratings yet
- RBC Disorder BcqsDocument68 pagesRBC Disorder BcqsMukhtiar AhmedNo ratings yet
- Introduction To Acid Base Metabolic AcidosisDocument12 pagesIntroduction To Acid Base Metabolic AcidosisKris Sharine Batalla OderoNo ratings yet
- Cirrhosis of LiverDocument106 pagesCirrhosis of LiveraahadNo ratings yet
- Lecture 10 - Hemolytic Anemias - Extracorpuscular DefectsDocument28 pagesLecture 10 - Hemolytic Anemias - Extracorpuscular DefectsArif MaulanaNo ratings yet
- Immune Thrombocytopenia (Second Option)Document16 pagesImmune Thrombocytopenia (Second Option)Fein MalricNo ratings yet
- Diagnostic Approach To The Adult With Jaundice or Asymptomatic Hyperbilirubinemia PDFDocument14 pagesDiagnostic Approach To The Adult With Jaundice or Asymptomatic Hyperbilirubinemia PDFSurat Saengjinda100% (1)
- HyphemaDocument19 pagesHyphemaLiyanti RinceNo ratings yet
- Diabetic Nephropathy: Assisstant Professor Dr. Mihaela-Dora DonciuDocument65 pagesDiabetic Nephropathy: Assisstant Professor Dr. Mihaela-Dora DonciuFloreaAndreiNo ratings yet
- Causes of HemoptysisDocument2 pagesCauses of HemoptysisAmira SaidinNo ratings yet
- Renal Tubular AcidosisDocument32 pagesRenal Tubular AcidosisSimon OnsongoNo ratings yet
- Atlas Urinary Sediments Renal BiopsiesDocument8 pagesAtlas Urinary Sediments Renal BiopsiesiruntoroNo ratings yet
- Renal Transplant: 1) Steps Involved in Kidney TransplantationDocument4 pagesRenal Transplant: 1) Steps Involved in Kidney TransplantationNadia SalwaniNo ratings yet
- Nephrotic SyndromeDocument34 pagesNephrotic SyndromeksanjdsaNo ratings yet
- Metabolic Syndrome DR - Yunus, SPPDDocument15 pagesMetabolic Syndrome DR - Yunus, SPPDMariaEllyNobetaHutabarat100% (1)
- Primary Glomerulonephritis UG LectureDocument50 pagesPrimary Glomerulonephritis UG LectureMalik Mohammad AzharuddinNo ratings yet
- Acute Renal FailureDocument6 pagesAcute Renal Failurearif kurnia timurNo ratings yet
- Learning Objectives:: Pathophysiology & Therapeutics, I (MSPR 521) Lecture No. 14Document9 pagesLearning Objectives:: Pathophysiology & Therapeutics, I (MSPR 521) Lecture No. 14adzhangNo ratings yet
- Essential Messages - 2023 DiabetesDocument13 pagesEssential Messages - 2023 Diabetesimran karimNo ratings yet
- Approach To Chronic DiarrheaDocument40 pagesApproach To Chronic DiarrheaJheng-Dao YangNo ratings yet
- Acute Kidney Injury-An UpdateDocument99 pagesAcute Kidney Injury-An UpdateProf Brigadier Mamun MostafiNo ratings yet
- Glycogen Storage Disease, Type II (Pompe Disease) : BackgroundDocument7 pagesGlycogen Storage Disease, Type II (Pompe Disease) : Background201111000No ratings yet
- Kidney Biopsy Finding of The Glomeruli - SUN 2019Document78 pagesKidney Biopsy Finding of The Glomeruli - SUN 2019Galih AryyagunawanNo ratings yet
- Aspirin OverdoseDocument3 pagesAspirin OverdoseSaputra BismaNo ratings yet
- GP Reg - Asthma and Spirometry 2011Document114 pagesGP Reg - Asthma and Spirometry 2011minerva_stanciuNo ratings yet
- Renal Tubular AcidosisDocument6 pagesRenal Tubular AcidosisRichella Khansa Lauditta100% (1)
- What Is Destroying This RBC?Document28 pagesWhat Is Destroying This RBC?Putri Azka RinandaNo ratings yet
- Hypernatremia From HarrisonDocument3 pagesHypernatremia From HarrisonNobel LaureateNo ratings yet
- The Liver: Dr. I Made Naris Pujawan, M.Biomed, SP - PADocument19 pagesThe Liver: Dr. I Made Naris Pujawan, M.Biomed, SP - PAAnonymous D29e00No ratings yet
- Upper GIT BleedingDocument69 pagesUpper GIT BleedingSoleh Ramly100% (1)
- Myasthenia GravisDocument24 pagesMyasthenia GravisAliMalikNo ratings yet
- 8 Tuberculosis Guidelines 2011Document63 pages8 Tuberculosis Guidelines 2011AliMalikNo ratings yet
- EpilepsyDocument21 pagesEpilepsyAliMalikNo ratings yet
- OrthopedicsDocument42 pagesOrthopedicsJubir Feat Divisi Operasional100% (1)
- Congenital Heart DiseasesDocument9 pagesCongenital Heart DiseasesAliMalikNo ratings yet
- Fiji DoctorsRecruitment March 2017Document4 pagesFiji DoctorsRecruitment March 2017AliMalikNo ratings yet
- A. Kumar, 2016 - Tia & StrokeDocument73 pagesA. Kumar, 2016 - Tia & StrokeAliMalikNo ratings yet
- Dr. Sultan Shah - Pre-Darwinian Islamic Evolution TheoriesDocument18 pagesDr. Sultan Shah - Pre-Darwinian Islamic Evolution TheoriesAliMalikNo ratings yet
- The Surgical Patient Adult or Paediatric: Key PointsDocument16 pagesThe Surgical Patient Adult or Paediatric: Key PointsAliMalikNo ratings yet
- CKD AweDocument25 pagesCKD AweMunawwar AweNo ratings yet
- GlomerulonephritisDocument1 pageGlomerulonephritismaleskunNo ratings yet
- House of Assembly Renal Recalled MCQsDocument9 pagesHouse of Assembly Renal Recalled MCQsMUHAMMAD AHMAD HAMMANo ratings yet
- Atlas Urinary Sediments Renal BiopsiesDocument8 pagesAtlas Urinary Sediments Renal BiopsiesiruntoroNo ratings yet
- Nephritic SyndromeDocument23 pagesNephritic SyndromeLateefah TalalNo ratings yet
- Renal Pathology-1 (Glomerulonephritis) - 2021Document15 pagesRenal Pathology-1 (Glomerulonephritis) - 2021oziad4518No ratings yet
- Neild 2009Document7 pagesNeild 2009Putra nstNo ratings yet
- ICD 10 - Ginjal HipertensiDocument5 pagesICD 10 - Ginjal HipertensiAlexanderKamNo ratings yet
- Holly Sanusi, Adrian Umboh, Valentine UmbohDocument5 pagesHolly Sanusi, Adrian Umboh, Valentine UmbohTemiNo ratings yet
- NephroticDocument8 pagesNephroticsangheetaNo ratings yet
- LP CKD FiksDocument16 pagesLP CKD FiksWahyu7.8No ratings yet
- Kelompok 2 - Tugas TT PT 6 - KODEFIKASI.Document3 pagesKelompok 2 - Tugas TT PT 6 - KODEFIKASI.Nalisa JasrinNo ratings yet
- Nephrotic and Nephritic Syndrome - 2008Document65 pagesNephrotic and Nephritic Syndrome - 2008rikasusanti101001201No ratings yet
- 58 Iajps58122019 PDFDocument4 pages58 Iajps58122019 PDFiajpsNo ratings yet
- Glomerular Diseases: Ass - Prof. Rihab Al-Mudhaffer Kufa University Department of Pathology and Forensic MedicineDocument37 pagesGlomerular Diseases: Ass - Prof. Rihab Al-Mudhaffer Kufa University Department of Pathology and Forensic MedicineAli HusseinNo ratings yet
- Renal - Goljan SlidesDocument29 pagesRenal - Goljan SlidesJoan ChoiNo ratings yet
- Glomerular Diseases My NotesDocument5 pagesGlomerular Diseases My Notesmalar_km43No ratings yet
- Systemic Lupus Erythematosus AssignmentDocument6 pagesSystemic Lupus Erythematosus AssignmentnehaNo ratings yet
- Sindrom Hemolitik UremikDocument8 pagesSindrom Hemolitik UremikLidwina ElisabethNo ratings yet
- Glomerular Syndromes PKDocument33 pagesGlomerular Syndromes PKamalasywaq2771No ratings yet
- Skripsi Tanpa Bab PembahasanDocument67 pagesSkripsi Tanpa Bab PembahasanUpitFlowNo ratings yet
- KDIGO GD Membranous NephropathyDocument1 pageKDIGO GD Membranous NephropathyF AudreyNo ratings yet
- Mortality and Morbidity Conference: Service Census January 2019Document63 pagesMortality and Morbidity Conference: Service Census January 2019AnneCanapiNo ratings yet
- MCQDocument40 pagesMCQLuthie Singh100% (2)
- NephEasy-3 4 09Document181 pagesNephEasy-3 4 09mouhamedmaloulieNo ratings yet
- The Columbia Renal Biopsy Course: Live Zoom Session Dates: Friday, July 8, 15 & 22, 2022Document7 pagesThe Columbia Renal Biopsy Course: Live Zoom Session Dates: Friday, July 8, 15 & 22, 2022Freddy Shanner Chávez VásquezNo ratings yet
- Nephrotic Syndrome (Nephrosis)Document9 pagesNephrotic Syndrome (Nephrosis)Radit Radovzky MayangkaraNo ratings yet
- Lecture Note On Renal Diseases For Medical Students - GNDocument10 pagesLecture Note On Renal Diseases For Medical Students - GNEsayas KebedeNo ratings yet
- Renal MCQDocument6 pagesRenal MCQMikiyas Tefera100% (1)
Glomerulonephritis: Nameesha Natasha Naidu 20130105
Glomerulonephritis: Nameesha Natasha Naidu 20130105
Uploaded by
AliMalik0 ratings0% found this document useful (0 votes)
51 views26 pagesThis document provides information on glomerulonephritis (GN), including its presentation, causes, types, investigations, management, and details on specific types like minimal change disease, focal segmental glomerulosclerosis, membranous GN, and rapidly progressive GN. GN is inflammation of the glomeruli that can cause nephrotic or nephritic syndrome. It has primary and secondary causes and is investigated via blood tests, urine tests, imaging and renal biopsy. Management involves treating the underlying cause, controlling blood pressure and cholesterol, and immunosuppression.
Original Description:
glomerulonephritis presentation
Original Title
Glomerulonephritis
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides information on glomerulonephritis (GN), including its presentation, causes, types, investigations, management, and details on specific types like minimal change disease, focal segmental glomerulosclerosis, membranous GN, and rapidly progressive GN. GN is inflammation of the glomeruli that can cause nephrotic or nephritic syndrome. It has primary and secondary causes and is investigated via blood tests, urine tests, imaging and renal biopsy. Management involves treating the underlying cause, controlling blood pressure and cholesterol, and immunosuppression.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
51 views26 pagesGlomerulonephritis: Nameesha Natasha Naidu 20130105
Glomerulonephritis: Nameesha Natasha Naidu 20130105
Uploaded by
AliMalikThis document provides information on glomerulonephritis (GN), including its presentation, causes, types, investigations, management, and details on specific types like minimal change disease, focal segmental glomerulosclerosis, membranous GN, and rapidly progressive GN. GN is inflammation of the glomeruli that can cause nephrotic or nephritic syndrome. It has primary and secondary causes and is investigated via blood tests, urine tests, imaging and renal biopsy. Management involves treating the underlying cause, controlling blood pressure and cholesterol, and immunosuppression.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 26
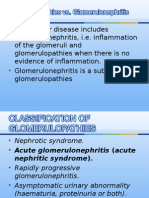
Glomerulonephritis
Nameesha Natasha Naidu
20130105
Reference
Davidson’s Principle and Practice of Medicine
Oxford Handbook of Clinical Medicine
Inflammation of the glomeruli
Presentation
Nephrotic Syndrome Nephritic Syndrome
1. Proteinuria >3.5g/24h 1. Hematuria
2. Hypoalbuminemia <25g/l 2. Oedma and generalized fluid
3. Oedema retention
Severe hyperlipidemia (TC 3. Hypertension
>10mmol/l) is often present 4. Oliguria
Causes
Primary Causes Secondary Causes
Nephrotic Sydrome: Nephrotic Sydrome:
Membranous nephropathy SLE(class V nephritis)
Minimal Change Diabetes
FSGS Amyloid
Mesangiocapillary GN Hepatitis B/C
Nephritic Syndrome: Nephritic Syndrome:
IgA nephropathy Post-streptococcal
Mesangiocapillary GN Vasculitis
SLE
Anti-GBM disease
cryoglobulinemia
Types
Minimal change nephropathy
Focal segmental glomerulosclerosis
Membranous glomerulonephritis
Mesangiocapillary glomerulonephritis
IgA nephropathy
Post-streptococcal glomerulonephritis
Henoch-Schonlein Purpura
Anti-glomerular basement membrane disease
Rapidly Progressive GN
Minimal Change Nephropathy
Reversible effacement of podocytes foot processes
Presents with proteinuria or nephrotic syndrome
Treatment: remits with high dose corticosteroid therapy (1mg/kg
prednisolone for 6 weeks)
Some patients who respond incompletely or relapse frequently
need maintenance corticosteroids, cytotoxic therapy or other
agents
Focal Segmental Glomerulosclerosis
Can occur in all age groups
Primary FSGS: cause unknown
Present with massive proteinuria and nephrotic syndrome
Sclerosis in segments of the glomeruli
Secondary FSGS:
Present with less proteinuria and sclerosis
The focal scarring may reflect healing of previous focal glomerular injury such
as HUS, cholesterol embolism or vasculitis. Other secondary causes-HIV,
podocyte toxins and massive obesity.
Treatment: high dose corticosteroid therapy(0.5-2mg/kg/day) but most patients
show little or no response
Immunosuppressive drugs e.g ciclosporin used but efficacy uncertain
Progression to CKD is common in patients who don’t respond to steroids and
the disease frequently recurs after renal transplantation
Membranous Glomerulonephritis
Most common cause of nephrotic syndrome in adults
Caused by autoantibodies directed at antigens expressed on the
surface of podocytes
Biopsy: diffusely thickened GBM with IgG and C3 deposits in
immunofluroscence
1/3 patients with idiopathic membranous glomerulonephritis undergo
spontaneous remission, 1/3 remain in a nephrotic state and 1/3 go on
to develop CKD
Treatment: treat underling cause
Give ACE-I and diuretics
Short-term treatment with high dose corticosteroids and
cyclophosphamide may improve the nephrotic syndrome and long
term prognosis
Mesangiocapillary Glomerulonephritis
Two types: immune complex mediated and complement mediated
Increase in mesangial cellularity with thickening of glomerular
capillary walls and subendothelial deposition of immune complexes
and complements
Causes: hepatitis C, SLE, monoclonal gammopathy and
abnormalities in complement pathway
Presents with proteinuria and hematuria
Biopsy: double contouring of the capillary walls(tram-tracks) and
thickened capillary basement membrane
Treatment: treat underlying cause. Give ACEI/ARB to all.
Immunosuppression with steroids and cyclophosphamide if rapid
progression of disease
IgA Nephropathy
One of the most common types of GN
Presents with hematuria, hypertension and proteinuria
In many cases there is slowly progressive loss of renal function leading to ESRD
A particular hallmark in some individuals is acute self-limiting exacerbations, often
with gross haematuria, in association with minor respiratory infections.
There is increased IgA which forms immune complexes and deposits in mesangial
cells
IF shows IgA and C3 deposits and mesangial proliferation in renal biopsy
The latency from clinical infection to nephritis is short
Treatment: BP control with ACE-I
Immunosuppressant may slow decline in renal function in those with nephritic
presentation
The management of less acute disease is largely directed towards the control of
BP in an attempt to prevent or retard progressive renal disease
Henoch-Schonlein Purpura
Characterised by systemic vasculitis that often arises in response to an
infectious trigger.
Presents with purpuric rash on extensor surfaces(mostly legs), flitting
polyarthritis, abdominal pain and nephritis
GN is usually indicated by hematuria
Diagnosis is confirmed with + IF for IgA and C3 in skin/renal biopsy
Treatment: same as IgA nephropathy
Prognosis is good with spontaneous resolution but some develop ESRD
Systemic Lupus Erythematous
1/3 patients with SLE will have evidence of renal disease with
vascular, glomerular and tubulointerstitial damage
Requires early treatment
Antiglomerular Basement Membrane
Disease(Goodpasture’s disease)
Caused by autoantibodies(IgG) to type IV collagen, an essential
component of GBM.
Type IV collagen is also found in lungs and pulmonary hemorrhage
can occur especially in smokers.
Present with hematuria/nephritic syndrome
AKI may occur within days of onset of symptoms
Treatment: plasma exchange, steroids and cytotoxics
If started early, full recovery is possible and relapses are rare
Case
20year old male presents with
hematuria and puffiness of face, eyes
and trunk. On examination he was
found to be hypertensive(170/100)
with scrotal swelling. The patient gives
a history of pyoderma 5 weeks ago.
Post-streptococcal GN
More common in children than adults
Occurs 1-12 weeks after a sore throat or skin infection.
A streptococcal antigen is deposited on the glomerulus, causing a
host reaction and immune complex formation
Molecular mimicry also occurs
Presents as nephritic syndrome(↓ GFR, proteinuria, hematuria and
oliguria)
Treatment: improves spontaneously within 10-14days
supportive (>95% patients renal function recovers)-fluid and salt
restriction with hypotensive agents.
Rapidly progressive glomerulonephritis
Also known as crescentic glomerulonephritis
Rapid loss of renal function over days to weeks.
Most aggressive GN, potential to cause ESRD over days.
Classified into 3 categories:
1. Immune complex disease e.g post-infections, SLE, IgA/HSP
2. Pauci-immune disease
3. Anti GBM disease e.g Goodpasture’s disease
Clinical presentation: AKI with systemic features(fever, myalgia, weight loss,
hemoptysis). Pulmonary hemorrahge is the commonest cause of death
Renal biopsy shows crescentric lesions
Treatment: aggressive immunesuppression with high dose IV steroids and
cyclophosphamide + plasma exchange
Investigations for GN Management
Blood: FBC, U&E, LFT, ESR, ACE-I or ARB
immunoglobulins, autoantibodies,
ANA, anti-dsDNA, blood culture Frusemide
Urine: RBC cast Statin to reduce cholesterol
Dipstick urinalysis to check for ACR Treat underlying cause
or PCR(ACR for men is <2.5 and High dose steroids
for women <3.5)
Supportive treatment
Imaging: renal ultrasound, CXR
Renal Biopsy
You might also like
- Nephrotic Syndrome PathophysiologyDocument1 pageNephrotic Syndrome PathophysiologyKrisianne Mae Lorenzo FranciscoNo ratings yet
- Rheumatology Cases Fall Clinics 2019Document85 pagesRheumatology Cases Fall Clinics 2019NaziBrola TsivadzeNo ratings yet
- BloodDocument51 pagesBloodDrShahid Sahito100% (1)
- Malaria MEQDocument6 pagesMalaria MEQMuvenn KannanNo ratings yet
- GlomerulonephritisDocument58 pagesGlomerulonephritisJosa Anggi Pratama0% (1)
- Nephritic Syndrome - Armando HasudunganDocument14 pagesNephritic Syndrome - Armando HasudunganzahraaNo ratings yet
- Nephrotic and Nephritic Syndrome - 2008Document65 pagesNephrotic and Nephritic Syndrome - 2008rikasusanti101001201No ratings yet
- Anca VasculitisDocument12 pagesAnca Vasculitisatul_desai_3100% (2)
- Cirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDocument21 pagesCirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDan ChicinasNo ratings yet
- Glomerular DiseasesDocument37 pagesGlomerular DiseaseskiflomNo ratings yet
- Clinical Approach To RPRF PDFDocument6 pagesClinical Approach To RPRF PDFshankarNo ratings yet
- Pathogenesis of Micro and Macrovascular Complications of DiabetesDocument4 pagesPathogenesis of Micro and Macrovascular Complications of DiabetesFrancesca LiNo ratings yet
- Crush Injury and Crush Syndrome PDFDocument2 pagesCrush Injury and Crush Syndrome PDFMichael DrakeNo ratings yet
- Primary Cardiac LymphomaDocument3 pagesPrimary Cardiac LymphomaHan KethyanethNo ratings yet
- Click To Download E6Document2 pagesClick To Download E6Mona SahuNo ratings yet
- 4 Circulation Disorders PDFDocument69 pages4 Circulation Disorders PDFSetiawan SukmadjaNo ratings yet
- Management of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesDocument7 pagesManagement of Acute Glomerulonephritis in Children: Children's Services Medical GuidelinesdaypranitaNo ratings yet
- Nephrotic Syndrome 2016Document45 pagesNephrotic Syndrome 2016alaaNo ratings yet
- NEPHROTIC SYNDROME - HamidDocument20 pagesNEPHROTIC SYNDROME - HamidAbdul Hamid OmarNo ratings yet
- Antiphospholipid Antibody SyndromeDocument37 pagesAntiphospholipid Antibody SyndromeAhmad Reshad AslamNo ratings yet
- Glomerulonephritis Dwi Fin PDFDocument108 pagesGlomerulonephritis Dwi Fin PDFOvyanda Eka MItraNo ratings yet
- PATH - Acute Kidney InjuryDocument12 pagesPATH - Acute Kidney InjuryAyyaz HussainNo ratings yet
- ASCITESDocument25 pagesASCITESGanesh BabuNo ratings yet
- 04 NephrologyDocument19 pages04 NephrologyeuncieNo ratings yet
- Acute Glomerulonep Hritis: By: Edelrose D. Lapitan BSN Iii-CDocument29 pagesAcute Glomerulonep Hritis: By: Edelrose D. Lapitan BSN Iii-CEdelrose Lapitan100% (1)
- Diabetes MellitusDocument79 pagesDiabetes Mellituskhalid saifur rahman khanNo ratings yet
- By: DR Eyad Talal: Moderator: DR I - QudaisatDocument55 pagesBy: DR Eyad Talal: Moderator: DR I - QudaisatEyad AbdeljawadNo ratings yet
- Infective EndocarditisDocument68 pagesInfective EndocarditisDr. Rajesh PadhiNo ratings yet
- Nephrotic Syndrome in Children: January 2013Document7 pagesNephrotic Syndrome in Children: January 2013molenNo ratings yet
- Embryology and Development of KidneyDocument75 pagesEmbryology and Development of Kidneyranjitha sraateNo ratings yet
- EdemaDocument3 pagesEdemaUdaya SreeNo ratings yet
- RBC Disorder BcqsDocument68 pagesRBC Disorder BcqsMukhtiar AhmedNo ratings yet
- Introduction To Acid Base Metabolic AcidosisDocument12 pagesIntroduction To Acid Base Metabolic AcidosisKris Sharine Batalla OderoNo ratings yet
- Cirrhosis of LiverDocument106 pagesCirrhosis of LiveraahadNo ratings yet
- Lecture 10 - Hemolytic Anemias - Extracorpuscular DefectsDocument28 pagesLecture 10 - Hemolytic Anemias - Extracorpuscular DefectsArif MaulanaNo ratings yet
- Immune Thrombocytopenia (Second Option)Document16 pagesImmune Thrombocytopenia (Second Option)Fein MalricNo ratings yet
- Diagnostic Approach To The Adult With Jaundice or Asymptomatic Hyperbilirubinemia PDFDocument14 pagesDiagnostic Approach To The Adult With Jaundice or Asymptomatic Hyperbilirubinemia PDFSurat Saengjinda100% (1)
- HyphemaDocument19 pagesHyphemaLiyanti RinceNo ratings yet
- Diabetic Nephropathy: Assisstant Professor Dr. Mihaela-Dora DonciuDocument65 pagesDiabetic Nephropathy: Assisstant Professor Dr. Mihaela-Dora DonciuFloreaAndreiNo ratings yet
- Causes of HemoptysisDocument2 pagesCauses of HemoptysisAmira SaidinNo ratings yet
- Renal Tubular AcidosisDocument32 pagesRenal Tubular AcidosisSimon OnsongoNo ratings yet
- Atlas Urinary Sediments Renal BiopsiesDocument8 pagesAtlas Urinary Sediments Renal BiopsiesiruntoroNo ratings yet
- Renal Transplant: 1) Steps Involved in Kidney TransplantationDocument4 pagesRenal Transplant: 1) Steps Involved in Kidney TransplantationNadia SalwaniNo ratings yet
- Nephrotic SyndromeDocument34 pagesNephrotic SyndromeksanjdsaNo ratings yet
- Metabolic Syndrome DR - Yunus, SPPDDocument15 pagesMetabolic Syndrome DR - Yunus, SPPDMariaEllyNobetaHutabarat100% (1)
- Primary Glomerulonephritis UG LectureDocument50 pagesPrimary Glomerulonephritis UG LectureMalik Mohammad AzharuddinNo ratings yet
- Acute Renal FailureDocument6 pagesAcute Renal Failurearif kurnia timurNo ratings yet
- Learning Objectives:: Pathophysiology & Therapeutics, I (MSPR 521) Lecture No. 14Document9 pagesLearning Objectives:: Pathophysiology & Therapeutics, I (MSPR 521) Lecture No. 14adzhangNo ratings yet
- Essential Messages - 2023 DiabetesDocument13 pagesEssential Messages - 2023 Diabetesimran karimNo ratings yet
- Approach To Chronic DiarrheaDocument40 pagesApproach To Chronic DiarrheaJheng-Dao YangNo ratings yet
- Acute Kidney Injury-An UpdateDocument99 pagesAcute Kidney Injury-An UpdateProf Brigadier Mamun MostafiNo ratings yet
- Glycogen Storage Disease, Type II (Pompe Disease) : BackgroundDocument7 pagesGlycogen Storage Disease, Type II (Pompe Disease) : Background201111000No ratings yet
- Kidney Biopsy Finding of The Glomeruli - SUN 2019Document78 pagesKidney Biopsy Finding of The Glomeruli - SUN 2019Galih AryyagunawanNo ratings yet
- Aspirin OverdoseDocument3 pagesAspirin OverdoseSaputra BismaNo ratings yet
- GP Reg - Asthma and Spirometry 2011Document114 pagesGP Reg - Asthma and Spirometry 2011minerva_stanciuNo ratings yet
- Renal Tubular AcidosisDocument6 pagesRenal Tubular AcidosisRichella Khansa Lauditta100% (1)
- What Is Destroying This RBC?Document28 pagesWhat Is Destroying This RBC?Putri Azka RinandaNo ratings yet
- Hypernatremia From HarrisonDocument3 pagesHypernatremia From HarrisonNobel LaureateNo ratings yet
- The Liver: Dr. I Made Naris Pujawan, M.Biomed, SP - PADocument19 pagesThe Liver: Dr. I Made Naris Pujawan, M.Biomed, SP - PAAnonymous D29e00No ratings yet
- Upper GIT BleedingDocument69 pagesUpper GIT BleedingSoleh Ramly100% (1)
- Myasthenia GravisDocument24 pagesMyasthenia GravisAliMalikNo ratings yet
- 8 Tuberculosis Guidelines 2011Document63 pages8 Tuberculosis Guidelines 2011AliMalikNo ratings yet
- EpilepsyDocument21 pagesEpilepsyAliMalikNo ratings yet
- OrthopedicsDocument42 pagesOrthopedicsJubir Feat Divisi Operasional100% (1)
- Congenital Heart DiseasesDocument9 pagesCongenital Heart DiseasesAliMalikNo ratings yet
- Fiji DoctorsRecruitment March 2017Document4 pagesFiji DoctorsRecruitment March 2017AliMalikNo ratings yet
- A. Kumar, 2016 - Tia & StrokeDocument73 pagesA. Kumar, 2016 - Tia & StrokeAliMalikNo ratings yet
- Dr. Sultan Shah - Pre-Darwinian Islamic Evolution TheoriesDocument18 pagesDr. Sultan Shah - Pre-Darwinian Islamic Evolution TheoriesAliMalikNo ratings yet
- The Surgical Patient Adult or Paediatric: Key PointsDocument16 pagesThe Surgical Patient Adult or Paediatric: Key PointsAliMalikNo ratings yet
- CKD AweDocument25 pagesCKD AweMunawwar AweNo ratings yet
- GlomerulonephritisDocument1 pageGlomerulonephritismaleskunNo ratings yet
- House of Assembly Renal Recalled MCQsDocument9 pagesHouse of Assembly Renal Recalled MCQsMUHAMMAD AHMAD HAMMANo ratings yet
- Atlas Urinary Sediments Renal BiopsiesDocument8 pagesAtlas Urinary Sediments Renal BiopsiesiruntoroNo ratings yet
- Nephritic SyndromeDocument23 pagesNephritic SyndromeLateefah TalalNo ratings yet
- Renal Pathology-1 (Glomerulonephritis) - 2021Document15 pagesRenal Pathology-1 (Glomerulonephritis) - 2021oziad4518No ratings yet
- Neild 2009Document7 pagesNeild 2009Putra nstNo ratings yet
- ICD 10 - Ginjal HipertensiDocument5 pagesICD 10 - Ginjal HipertensiAlexanderKamNo ratings yet
- Holly Sanusi, Adrian Umboh, Valentine UmbohDocument5 pagesHolly Sanusi, Adrian Umboh, Valentine UmbohTemiNo ratings yet
- NephroticDocument8 pagesNephroticsangheetaNo ratings yet
- LP CKD FiksDocument16 pagesLP CKD FiksWahyu7.8No ratings yet
- Kelompok 2 - Tugas TT PT 6 - KODEFIKASI.Document3 pagesKelompok 2 - Tugas TT PT 6 - KODEFIKASI.Nalisa JasrinNo ratings yet
- Nephrotic and Nephritic Syndrome - 2008Document65 pagesNephrotic and Nephritic Syndrome - 2008rikasusanti101001201No ratings yet
- 58 Iajps58122019 PDFDocument4 pages58 Iajps58122019 PDFiajpsNo ratings yet
- Glomerular Diseases: Ass - Prof. Rihab Al-Mudhaffer Kufa University Department of Pathology and Forensic MedicineDocument37 pagesGlomerular Diseases: Ass - Prof. Rihab Al-Mudhaffer Kufa University Department of Pathology and Forensic MedicineAli HusseinNo ratings yet
- Renal - Goljan SlidesDocument29 pagesRenal - Goljan SlidesJoan ChoiNo ratings yet
- Glomerular Diseases My NotesDocument5 pagesGlomerular Diseases My Notesmalar_km43No ratings yet
- Systemic Lupus Erythematosus AssignmentDocument6 pagesSystemic Lupus Erythematosus AssignmentnehaNo ratings yet
- Sindrom Hemolitik UremikDocument8 pagesSindrom Hemolitik UremikLidwina ElisabethNo ratings yet
- Glomerular Syndromes PKDocument33 pagesGlomerular Syndromes PKamalasywaq2771No ratings yet
- Skripsi Tanpa Bab PembahasanDocument67 pagesSkripsi Tanpa Bab PembahasanUpitFlowNo ratings yet
- KDIGO GD Membranous NephropathyDocument1 pageKDIGO GD Membranous NephropathyF AudreyNo ratings yet
- Mortality and Morbidity Conference: Service Census January 2019Document63 pagesMortality and Morbidity Conference: Service Census January 2019AnneCanapiNo ratings yet
- MCQDocument40 pagesMCQLuthie Singh100% (2)
- NephEasy-3 4 09Document181 pagesNephEasy-3 4 09mouhamedmaloulieNo ratings yet
- The Columbia Renal Biopsy Course: Live Zoom Session Dates: Friday, July 8, 15 & 22, 2022Document7 pagesThe Columbia Renal Biopsy Course: Live Zoom Session Dates: Friday, July 8, 15 & 22, 2022Freddy Shanner Chávez VásquezNo ratings yet
- Nephrotic Syndrome (Nephrosis)Document9 pagesNephrotic Syndrome (Nephrosis)Radit Radovzky MayangkaraNo ratings yet
- Lecture Note On Renal Diseases For Medical Students - GNDocument10 pagesLecture Note On Renal Diseases For Medical Students - GNEsayas KebedeNo ratings yet
- Renal MCQDocument6 pagesRenal MCQMikiyas Tefera100% (1)