Professional Documents
Culture Documents
CH 12 Health Transaction N Billing
CH 12 Health Transaction N Billing
Uploaded by
Mohammad IchsanCopyright:
Available Formats
You might also like
- 2024 Appropriation Bill - UpdatedDocument15 pages2024 Appropriation Bill - UpdatedifaloresimeonNo ratings yet
- NZ USAR Awareness ManualDocument87 pagesNZ USAR Awareness ManualShane Briggs100% (3)
- Ao2022-0006 HFEPDocument36 pagesAo2022-0006 HFEPDaryll DecanoNo ratings yet
- Audio TranscriptionDocument10 pagesAudio TranscriptionJohn PhilippNo ratings yet
- Billing Process ChecklistDocument2 pagesBilling Process ChecklistSandeep SharmaNo ratings yet
- ISDAPDocument5 pagesISDAPAlbert CongNo ratings yet
- Medical Billing Process: Naveen MajetyDocument21 pagesMedical Billing Process: Naveen MajetyNaveen KumarNo ratings yet
- Medical Billing - An OverviewDocument20 pagesMedical Billing - An OverviewRoaring King100% (1)
- Literature Review On Online Medical Billing SystemDocument6 pagesLiterature Review On Online Medical Billing Systemc5sd1aqjNo ratings yet
- OIG Compliance Program For Third-Party Medical Billing CompaniesDocument15 pagesOIG Compliance Program For Third-Party Medical Billing CompaniesaaronborosNo ratings yet
- Chapter2 - Billing 1Document33 pagesChapter2 - Billing 1Marivel Galviso BONIONo ratings yet
- Important Terms Used in Cash PostingDocument3 pagesImportant Terms Used in Cash PostingjamesNo ratings yet
- Medical Billing OutsourcingDocument9 pagesMedical Billing OutsourcingOutsource Strategies InternationalNo ratings yet
- Billing Documentation Software: For Slps AudiologistsDocument5 pagesBilling Documentation Software: For Slps AudiologistsHoàng Đức NhuậnNo ratings yet
- Chapter 3 Health Care Delivery Due 10Document3 pagesChapter 3 Health Care Delivery Due 10lisadhatchNo ratings yet
- MPRA Paper 70218Document231 pagesMPRA Paper 70218TRYVERN MAMIZANo ratings yet
- Medical Billing Resume ObjectiveDocument6 pagesMedical Billing Resume Objectivejhwwawrmd100% (2)
- Medicare Claims Processing Manual: Chapter 12 - Physicians/Nonphysician PractitionersDocument232 pagesMedicare Claims Processing Manual: Chapter 12 - Physicians/Nonphysician PractitionersAaron RasmussenNo ratings yet
- Coding Billing - PPSXDocument35 pagesCoding Billing - PPSXmanjuNo ratings yet
- Personal Details: Name Email Id Contact Number Address Date of Birth Gender Marital Status Languages KnownDocument4 pagesPersonal Details: Name Email Id Contact Number Address Date of Birth Gender Marital Status Languages KnownSacheen RathodNo ratings yet
- S. No Scenarios Check PointsDocument28 pagesS. No Scenarios Check PointsSuganthi LNo ratings yet
- Literature Review On e PaymentDocument7 pagesLiterature Review On e Paymentc5nr2r46100% (1)
- Cms 1500 Form Cms Manual Chapter 26Document114 pagesCms 1500 Form Cms Manual Chapter 26myousafkNo ratings yet
- Adb Ar CallerDocument2 pagesAdb Ar CallerRamesh MishraNo ratings yet
- Billing and Coding ResumeDocument7 pagesBilling and Coding Resumezehlobifg100% (2)
- Concierge RCM Implementation: DocumentsDocument5 pagesConcierge RCM Implementation: DocumentsSagardeep RoyNo ratings yet
- Healthcare Domain QuestionsDocument5 pagesHealthcare Domain QuestionsNikhil SatavNo ratings yet
- Billing and Invoicing - V3SCAPDocument59 pagesBilling and Invoicing - V3SCAPsonu singhNo ratings yet
- SHEARWATER ORIENTATION (Day 1)Document7 pagesSHEARWATER ORIENTATION (Day 1)Erica JoyNo ratings yet
- Curriculum Vitae: Omega Healthcare Solutions (Bangalore)Document3 pagesCurriculum Vitae: Omega Healthcare Solutions (Bangalore)mamatha mamtaNo ratings yet
- The Executive's Guide To Measuring Total Cost of Billing in The LaboratoryDocument12 pagesThe Executive's Guide To Measuring Total Cost of Billing in The Laboratoryranjith123No ratings yet
- Ecw EMR Workbook II - Updated - Portage Health PDFDocument63 pagesEcw EMR Workbook II - Updated - Portage Health PDFSyed Mudussir HusainNo ratings yet
- Literature Review Billing SystemDocument6 pagesLiterature Review Billing Systemchrvzyukg100% (1)
- CMS-855B - 04052021Document49 pagesCMS-855B - 04052021Sheldon GunbyNo ratings yet
- Resume Format 2015Document8 pagesResume Format 2015bcqta9j6100% (2)
- SITEL - Claims Reimbursement Form Rev.06 PDFDocument2 pagesSITEL - Claims Reimbursement Form Rev.06 PDFJoyce HerreraNo ratings yet
- Medical Billing ResumeDocument3 pagesMedical Billing ResumeK.Pavan Kalyan Reddy RAMBONo ratings yet
- Foundation Training To Medical BillingDocument23 pagesFoundation Training To Medical BillingHarry CanabaNo ratings yet
- Insurance: General Commercial Health Insurance Information 179Document22 pagesInsurance: General Commercial Health Insurance Information 179DeviselvamNo ratings yet
- Cc12 Coding Compliance PlanDocument5 pagesCc12 Coding Compliance PlanOppyNo ratings yet
- HL7Document13 pagesHL7sony100% (3)
- Medicare Denials How To HandleDocument6 pagesMedicare Denials How To Handlevikki soni100% (2)
- Denial Management White PaperDocument10 pagesDenial Management White PaperPraveen Shenoi100% (1)
- 15 Ways To Market Medical Billing BusinessDocument11 pages15 Ways To Market Medical Billing BusinessMuhammadSamran Zia100% (1)
- 2010-033 FS Rev Cycle White Paper FINALDocument56 pages2010-033 FS Rev Cycle White Paper FINALPraise Cabalum BuenaflorNo ratings yet
- Nithya ResumeDocument3 pagesNithya ResumeNithya NithuNo ratings yet
- Lecture 11 Adding Value To Core Products With Supplementary ServicesDocument7 pagesLecture 11 Adding Value To Core Products With Supplementary ServicesAditya VikramNo ratings yet
- ADT DFT ORU: The Most Commonly Used HL7 Message Types IncludeDocument1 pageADT DFT ORU: The Most Commonly Used HL7 Message Types IncludeRafi Uddin ShaikNo ratings yet
- Introduction To Electronic Medical Record - Non-CHKD Employees - August - 2023 V2Document56 pagesIntroduction To Electronic Medical Record - Non-CHKD Employees - August - 2023 V2Ahmad AhmadNo ratings yet
- Denials ImportantDocument7 pagesDenials ImportantAdityaNo ratings yet
- Literature Review On Online Billing SystemDocument4 pagesLiterature Review On Online Billing Systemfohudenyfeh2100% (1)
- Billing Process: Prioritize Larger COINSURANCE Values 2. Get Copy of Remittance AdviceDocument1 pageBilling Process: Prioritize Larger COINSURANCE Values 2. Get Copy of Remittance AdviceHaira Joyce E. PunoNo ratings yet
- ICD 10 Training Sessions Training AgendaDocument3 pagesICD 10 Training Sessions Training AgendaAntonSusanto100% (1)
- Patient Information SystemDocument5 pagesPatient Information SystemJignesh DesaiNo ratings yet
- Medical Billing Resume ExamplesDocument7 pagesMedical Billing Resume Examplesbcr7r579100% (2)
- 0 - Basic HealthcareDocument19 pages0 - Basic HealthcareMd SaifNo ratings yet
- Medical Transcription Practice Sample PagesDocument2 pagesMedical Transcription Practice Sample PagesAmeerah CabangalNo ratings yet
- DocumentationDocument27 pagesDocumentationanju kumawatNo ratings yet
- Codes - Ontario PDFDocument104 pagesCodes - Ontario PDFprabal rayNo ratings yet
- CPB Online Medical Billing Syllabus - 11th - 4!17!13Document2 pagesCPB Online Medical Billing Syllabus - 11th - 4!17!13Kian GonzagaNo ratings yet
- EHRA InteroperabilityRoadmap 20090310 v3Document40 pagesEHRA InteroperabilityRoadmap 20090310 v3Anonymous JE7uJR100% (1)
- Medical Transcription Industry FactsDocument2 pagesMedical Transcription Industry FactsSrinivas Pandian0% (1)
- Freelancing QuestionDocument8 pagesFreelancing QuestionImran AliNo ratings yet
- Utilization Review Coordinator: Passbooks Study GuideFrom EverandUtilization Review Coordinator: Passbooks Study GuideNo ratings yet
- Apa Yang Harus Dipersiapkan Rumah Sakit Untuk Meningkatkan Keamanan Fasilitasnya ?Document17 pagesApa Yang Harus Dipersiapkan Rumah Sakit Untuk Meningkatkan Keamanan Fasilitasnya ?Mohammad IchsanNo ratings yet
- 3.8 SPH Self-Assessment 508 PDFDocument2 pages3.8 SPH Self-Assessment 508 PDFMohammad IchsanNo ratings yet
- Hand Book OshaDocument40 pagesHand Book OshaMohammad Ichsan100% (1)
- Kompetensi SDM Dan Kualitas Pelayanan Rumah Sakit: June 2012Document10 pagesKompetensi SDM Dan Kualitas Pelayanan Rumah Sakit: June 2012Mohammad IchsanNo ratings yet
- Agrarian Law and Social Legislation NotesDocument18 pagesAgrarian Law and Social Legislation Noteskenn1o1No ratings yet
- National Health Programs Final 150324130140 Conversion Gate01Document141 pagesNational Health Programs Final 150324130140 Conversion Gate01Manoj Garg100% (1)
- Request For Permit To Work (PTW) - Contactor Application: PLTG 75 MW Paya Pasir MedanDocument2 pagesRequest For Permit To Work (PTW) - Contactor Application: PLTG 75 MW Paya Pasir MedanDimas Dwi SwarnaNo ratings yet
- Deciding JCT Contract Practice GuideDocument43 pagesDeciding JCT Contract Practice GuideKajendra100% (2)
- CFR 2019 Title30 Vol1Document806 pagesCFR 2019 Title30 Vol1Carlos Ernesto Flores AlbinoNo ratings yet
- Leader Analysis-John MackeyDocument8 pagesLeader Analysis-John Mackeyapi-272623096No ratings yet
- Social Health Protection Toward UHC in Lao PDRDocument16 pagesSocial Health Protection Toward UHC in Lao PDRADBI EventsNo ratings yet
- Business Excellence AwardDocument18 pagesBusiness Excellence AwardKarthikeyan NatarajanNo ratings yet
- Maklumat Vaksinasi: Vaccination DetailsDocument2 pagesMaklumat Vaksinasi: Vaccination DetailsHakim FawwazNo ratings yet
- Health PDFDocument9 pagesHealth PDFAnshul SinghalNo ratings yet
- 2020 SK Accomplishment ReportDocument36 pages2020 SK Accomplishment ReportRegine Rosillo100% (2)
- 08-30-14 EditionDocument36 pages08-30-14 EditionSan Mateo Daily JournalNo ratings yet
- Know About United State Pharmacopoeia (Usp) by Dr.T.V.Vidyasagar Neuheit Pharma Technologies Private LimitedDocument13 pagesKnow About United State Pharmacopoeia (Usp) by Dr.T.V.Vidyasagar Neuheit Pharma Technologies Private LimitedtvvsagarNo ratings yet
- Chapter 1Document9 pagesChapter 1Antun RahmadiNo ratings yet
- The Inversion of Exceptionality: Foucault, Agamben, and "Reproductive Rights"Document17 pagesThe Inversion of Exceptionality: Foucault, Agamben, and "Reproductive Rights"HedvaNo ratings yet
- 2nd ARC Reports Unlocking Human CapitalDocument5 pages2nd ARC Reports Unlocking Human CapitalPrabhakar YadavNo ratings yet
- Aus Census Information 2016Document8 pagesAus Census Information 2016CaddlesmanNo ratings yet
- Medical EthicsDocument75 pagesMedical EthicsNenyAriyana100% (2)
- Irda Act & Types of InsuranceDocument19 pagesIrda Act & Types of InsuranceVinayak BhardwajNo ratings yet
- Article Ii Unlawful Acts and Penalties Section 11. Possession of Dangerous Drugs. - The Penalty of Life Imprisonment To Death and A FineDocument3 pagesArticle Ii Unlawful Acts and Penalties Section 11. Possession of Dangerous Drugs. - The Penalty of Life Imprisonment To Death and A FineCarol JacintoNo ratings yet
- Compendium-December, 2018Document61 pagesCompendium-December, 2018Shivam MishraNo ratings yet
- Rule 1010Document46 pagesRule 1010Kristel Gail BasilioNo ratings yet
- Federalism 101: Federalism Is A System of Government in Which Power Is Divided Between A NationalDocument1 pageFederalism 101: Federalism Is A System of Government in Which Power Is Divided Between A NationalJhoana Parica FranciscoNo ratings yet
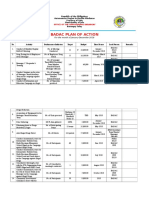
- Badac Plan of ActionDocument5 pagesBadac Plan of ActionTaz HalipaNo ratings yet
- NCQA PrimerDocument53 pagesNCQA Primerd_anto781063No ratings yet
CH 12 Health Transaction N Billing
CH 12 Health Transaction N Billing
Uploaded by
Mohammad IchsanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CH 12 Health Transaction N Billing
CH 12 Health Transaction N Billing
Uploaded by
Mohammad IchsanCopyright:
Available Formats
Health Information
Technology and Management
Health
Transactions and
Billing
Health Information Technology and Management
Figure 10-1 Billing wokflow.
Health Information Technology and Management
Billing Workflow (continued)
• Providers verify patient insurance
eligibility; medical offices collect and post
copays
• The patient is treated and discharged or
checked out
• Procedure codes are assigned for services
rendered and supplies used; diagnosis
codes are assigned for disease or medical
condition
Health Information Technology and Management
Billing Workflow (continued)
• Computer program generates paper or
electronic claim to be sent to insurance
plan after its reviewed by insurance or
claim specialist
Health Information Technology and Management
Billing Workflow (continued)
• Insurance plan adjudicates claim and pays
provider (remittance); remittance advice or
EOB explaining payments generated
• Payment amount recorded in patient
accounts system; write-down adjustment,
if necessary, posted
Health Information Technology and Management
Billing Workflow (continued)
• If applicable, claim is next sent to patient’s
secondary plan; “piggyback” or COB claim
• Statement is sent to patient for any
amounts due that are patient’s
responsibility
• Patient payments received by medical
office or hospital are posted to patient’s
account
Health Information Technology and Management
Figure 10-2 Example of an open item patient statement.
Health Information Technology and Management
Real-Time Posting
• Occurs while patient still present
• Allows for collection of copay
• Shortens revenue cycle (charge posting
complete at day’s end)
• Most commonly used in medical offices
Health Information Technology and Management
Figure 10-3 Encounter form (also known as a superbill or charge ticket).
Health Information Technology and Management
Batch Posting
• Similar to real-time posting except
superbills are gathered into a batch for the
date and posted later
• Often handled by a billing service which
posts charges, generates insurance
claims, and sends patient statements
• Common method for hospital billing
Health Information Technology and Management
Payments
• Posted in both in batches and real time
• Patient payments, especially copays,
posted while patient is present to generate
receipt
• Insurance plan payments often posted in
batches
– May include lengthy EOB or ERA files
Health Information Technology and Management
Hospital Batch Posting
• Do not bill until patient is discharged and
all records completed
• Many hospitals do not begin coding and
charge capture until HIM department has
analyzed record and sent it for coding
Health Information Technology and Management
Hospital Batch Posting
(continued)
• Hospitals often use a bill-hold period to
ensure the hundreds of applicable charges
have been collected and coded
– Helps ensure use of accurate DRG and APC
codes
Health Information Technology and Management
Electronic Data Interchange (EDI)
• HIPAA standardized healthcare EDI by
requiring use of standard formats
developed and maintained by ANSI
• HIPAA requires specific transaction
standards for eight types of electronic data
interchange
Health Information Technology and Management
Eight Mandated
HIPAA Transactions
• Claims or equivalent encounters and
coordination of benefits (ANSI 837)
• Remittance and payment advice (ANSI
835)
• Claim status inquiry (ANSI 276) and
response (ANSI 277)
• Eligibility benefit inquiry (ANSI 270) and
response (ANSI 271)
Health Information Technology and Management
Eight Mandated
HIPAA Transactions (continued)
• Referral certification and authorization
(ANSI 278)
• Health plan premium payments (ANSI
820)
• Enrollment and de-enrollment in a health
plan (ANSI 834)
• Retail drug claims, coordination of drug
benefits and eligibility inquiry (NCPDP 5.1;
Version D.0)
Health Information Technology and Management
Additional Transactions
• Under development, not yet mandated by
HIPAA; include:
– Patient Information in Support of a Health
Claim or Encounter (ANSI 275)
– First Report of Injury transaction
Health Information Technology and Management
Professional Claims Billing
• Use either CMS-1500 form (paper) or
ANSI 837-P (electronic) transaction
– Medicare now requires most providers to
submit claims electronically
• CMS-1500 “fields” are numbered boxes
called form locators
• Form includes HCPCS/CPT-4 code;
associated with one or more diagnoses
that justify its medical necessity
Health Information Technology and Management
Professional Claims Billing
(continued)
• Charges for each item are typically
providers’ usual and customary rate for the
item, not the contractually allowed amount
they expect to be paid
• Electronic claims report the same
information, but are sent a batch file
containing many claims for same provider
or multiple claims for one or more patients
Health Information Technology and Management
Figure 10-4 Loop structure of ANSI 837-P electronic media claims.
Health Information Technology and Management
Figure 10-5 CMS-1500 paper form for professional claims.
Health Information Technology and Management
Institutional Claims Billing
• Hospitals use different claim form for
paper and electronic billing, necessitated
by reimbursement system based on
principal diagnosis and DRG
Health Information Technology and Management
Institutional Claims Billing
• UB-04 form (paper) and ANSI 837-I
(electronic) format differ substantially from
professional claim forms
– Has coded fields instead of “yes/no” boxes
– Has condition, occurrence, and value codes
to communicate special information
– May be nine pages long to accommodate 450
line items
Health Information Technology and Management
Figure 10-6 Sample electronic media claim file (ANSI 837-I).
Health Information Technology and Management
Electronic Media Claims (EMCs)
• HIPAA requires most health plans to
receive claims electronically in ANSI 837
format and permits all types of providers to
send them
• Medicare also requires nearly all providers
to submit claims electronically
• EMC files are typically batches of claims
sent in one large file
Health Information Technology and Management
Clearinghouses
• Act as transaction intermediaries between
providers and health plans
• Receive claims from provider, send them
to plans, receive responses from plans,
and send responses to provider (functions
as a switch)
Health Information Technology and Management
Clearinghouses (continued)
• May transmit PHI because they are one of
the three covered entities defined by
HIPAA
– Clearinghouse function is to convert data
arriving in a noncompliant format into a
HIPAA-compliant format
Health Information Technology and Management
Claim Scrubbers
• Special software that examines claim data
before it is sent to eliminate preventable
billing errors
• May be component of billing system and
thus help prevent claims from being
created until errors corrected
Health Information Technology and Management
Claim Scrubbers (continued)
• Or, may examine batch of claims and
report errors prior to sending
• Follow same logic as payer’s claim edits
Health Information Technology and Management
Provider Payment Delays
• Caused by:
– Bill-hold period
– Payment floor
14-day delay (electronic claims) and 29-day delay
(paper claims) imposed by Medicare intermediaries
and other health plans
Health Information Technology and Management
Provider Payment Delays
(continued)
• Caused by:
– Secondary insurance plan billing
– Payment from patient
– Accounts receivable is uncollected money
owed
Health Information Technology and Management
Two Types of Patient Statements
• Balance forward
– Begins with previous month’s balance and
shows only charges or payments posted in
current period
• Open item
– Shows all unpaid items with payment,
adjustments, and balance for each item
Health Information Technology and Management
ERA Systems
• Receive remittance information
electronically from payer in ANSI 835
transaction
– Special segments carry codified information
about how claim was adjudicated and any
adjustments made to the payment
• Save information from ANSI 835
transaction in database and report claim
electronically to secondary payer
Health Information Technology and Management
ERA Systems (continued)
• Create report of what has been sent and
how it has been applied to patient
accounts
• Reconciles checks to totals on report or
verifies EFT
• ERA not sent to bank due to PHI
Health Information Technology and Management
Figure 10-8 Sample paper EOB remittance advice.
Health Information Technology and Management
Determining Insurance Eligibility
• Provider sends eligibility inquiry to payer in
ANSI 270 format
• Payer responds with requested
information using ANSI 271 transaction
• Payer can also send ANSI 271
transactions to communicate information
Health Information Technology and Management
Referrals and Authorizations
• Use ANSI 278 transaction, Health Care
Services Request for Review and
Response, to:
– Send request for authorization
– Return information about authorization,
certification, or referral to provider by plan
Health Information Technology and Management
Claim Status
• Suspended claims may have not been
adjudicated due to:
– Need for further information, supporting
documentation, or test
– Loss of requests for missing information
• Unpaid claims must be investigated after
reasonable amount of time
– By phone
– Electronically using ANSI 276 transaction
Health Information Technology and Management
Claim Attachments
• Supplemental documents providing
additional medical information to claims
processor
• Include information that cannot be
accommodated within claim format
Health Information Technology and Management
Claim Attachments (continued)
• Examples include:
– certificates of medical necessity (CMNs),
discharge summaries, operative reports
• Main reason claims are suspended
Health Information Technology and Management
Notice of Proposed Rule Making
• Identifies six types of electronic claims
attachments:
– Clinical reports
– Laboratory reports
– Emergency department reports
– Rehabilitative services
– Ambulance services
– Medications (during treatment, upon
discharge)
Health Information Technology and Management
You might also like
- 2024 Appropriation Bill - UpdatedDocument15 pages2024 Appropriation Bill - UpdatedifaloresimeonNo ratings yet
- NZ USAR Awareness ManualDocument87 pagesNZ USAR Awareness ManualShane Briggs100% (3)
- Ao2022-0006 HFEPDocument36 pagesAo2022-0006 HFEPDaryll DecanoNo ratings yet
- Audio TranscriptionDocument10 pagesAudio TranscriptionJohn PhilippNo ratings yet
- Billing Process ChecklistDocument2 pagesBilling Process ChecklistSandeep SharmaNo ratings yet
- ISDAPDocument5 pagesISDAPAlbert CongNo ratings yet
- Medical Billing Process: Naveen MajetyDocument21 pagesMedical Billing Process: Naveen MajetyNaveen KumarNo ratings yet
- Medical Billing - An OverviewDocument20 pagesMedical Billing - An OverviewRoaring King100% (1)
- Literature Review On Online Medical Billing SystemDocument6 pagesLiterature Review On Online Medical Billing Systemc5sd1aqjNo ratings yet
- OIG Compliance Program For Third-Party Medical Billing CompaniesDocument15 pagesOIG Compliance Program For Third-Party Medical Billing CompaniesaaronborosNo ratings yet
- Chapter2 - Billing 1Document33 pagesChapter2 - Billing 1Marivel Galviso BONIONo ratings yet
- Important Terms Used in Cash PostingDocument3 pagesImportant Terms Used in Cash PostingjamesNo ratings yet
- Medical Billing OutsourcingDocument9 pagesMedical Billing OutsourcingOutsource Strategies InternationalNo ratings yet
- Billing Documentation Software: For Slps AudiologistsDocument5 pagesBilling Documentation Software: For Slps AudiologistsHoàng Đức NhuậnNo ratings yet
- Chapter 3 Health Care Delivery Due 10Document3 pagesChapter 3 Health Care Delivery Due 10lisadhatchNo ratings yet
- MPRA Paper 70218Document231 pagesMPRA Paper 70218TRYVERN MAMIZANo ratings yet
- Medical Billing Resume ObjectiveDocument6 pagesMedical Billing Resume Objectivejhwwawrmd100% (2)
- Medicare Claims Processing Manual: Chapter 12 - Physicians/Nonphysician PractitionersDocument232 pagesMedicare Claims Processing Manual: Chapter 12 - Physicians/Nonphysician PractitionersAaron RasmussenNo ratings yet
- Coding Billing - PPSXDocument35 pagesCoding Billing - PPSXmanjuNo ratings yet
- Personal Details: Name Email Id Contact Number Address Date of Birth Gender Marital Status Languages KnownDocument4 pagesPersonal Details: Name Email Id Contact Number Address Date of Birth Gender Marital Status Languages KnownSacheen RathodNo ratings yet
- S. No Scenarios Check PointsDocument28 pagesS. No Scenarios Check PointsSuganthi LNo ratings yet
- Literature Review On e PaymentDocument7 pagesLiterature Review On e Paymentc5nr2r46100% (1)
- Cms 1500 Form Cms Manual Chapter 26Document114 pagesCms 1500 Form Cms Manual Chapter 26myousafkNo ratings yet
- Adb Ar CallerDocument2 pagesAdb Ar CallerRamesh MishraNo ratings yet
- Billing and Coding ResumeDocument7 pagesBilling and Coding Resumezehlobifg100% (2)
- Concierge RCM Implementation: DocumentsDocument5 pagesConcierge RCM Implementation: DocumentsSagardeep RoyNo ratings yet
- Healthcare Domain QuestionsDocument5 pagesHealthcare Domain QuestionsNikhil SatavNo ratings yet
- Billing and Invoicing - V3SCAPDocument59 pagesBilling and Invoicing - V3SCAPsonu singhNo ratings yet
- SHEARWATER ORIENTATION (Day 1)Document7 pagesSHEARWATER ORIENTATION (Day 1)Erica JoyNo ratings yet
- Curriculum Vitae: Omega Healthcare Solutions (Bangalore)Document3 pagesCurriculum Vitae: Omega Healthcare Solutions (Bangalore)mamatha mamtaNo ratings yet
- The Executive's Guide To Measuring Total Cost of Billing in The LaboratoryDocument12 pagesThe Executive's Guide To Measuring Total Cost of Billing in The Laboratoryranjith123No ratings yet
- Ecw EMR Workbook II - Updated - Portage Health PDFDocument63 pagesEcw EMR Workbook II - Updated - Portage Health PDFSyed Mudussir HusainNo ratings yet
- Literature Review Billing SystemDocument6 pagesLiterature Review Billing Systemchrvzyukg100% (1)
- CMS-855B - 04052021Document49 pagesCMS-855B - 04052021Sheldon GunbyNo ratings yet
- Resume Format 2015Document8 pagesResume Format 2015bcqta9j6100% (2)
- SITEL - Claims Reimbursement Form Rev.06 PDFDocument2 pagesSITEL - Claims Reimbursement Form Rev.06 PDFJoyce HerreraNo ratings yet
- Medical Billing ResumeDocument3 pagesMedical Billing ResumeK.Pavan Kalyan Reddy RAMBONo ratings yet
- Foundation Training To Medical BillingDocument23 pagesFoundation Training To Medical BillingHarry CanabaNo ratings yet
- Insurance: General Commercial Health Insurance Information 179Document22 pagesInsurance: General Commercial Health Insurance Information 179DeviselvamNo ratings yet
- Cc12 Coding Compliance PlanDocument5 pagesCc12 Coding Compliance PlanOppyNo ratings yet
- HL7Document13 pagesHL7sony100% (3)
- Medicare Denials How To HandleDocument6 pagesMedicare Denials How To Handlevikki soni100% (2)
- Denial Management White PaperDocument10 pagesDenial Management White PaperPraveen Shenoi100% (1)
- 15 Ways To Market Medical Billing BusinessDocument11 pages15 Ways To Market Medical Billing BusinessMuhammadSamran Zia100% (1)
- 2010-033 FS Rev Cycle White Paper FINALDocument56 pages2010-033 FS Rev Cycle White Paper FINALPraise Cabalum BuenaflorNo ratings yet
- Nithya ResumeDocument3 pagesNithya ResumeNithya NithuNo ratings yet
- Lecture 11 Adding Value To Core Products With Supplementary ServicesDocument7 pagesLecture 11 Adding Value To Core Products With Supplementary ServicesAditya VikramNo ratings yet
- ADT DFT ORU: The Most Commonly Used HL7 Message Types IncludeDocument1 pageADT DFT ORU: The Most Commonly Used HL7 Message Types IncludeRafi Uddin ShaikNo ratings yet
- Introduction To Electronic Medical Record - Non-CHKD Employees - August - 2023 V2Document56 pagesIntroduction To Electronic Medical Record - Non-CHKD Employees - August - 2023 V2Ahmad AhmadNo ratings yet
- Denials ImportantDocument7 pagesDenials ImportantAdityaNo ratings yet
- Literature Review On Online Billing SystemDocument4 pagesLiterature Review On Online Billing Systemfohudenyfeh2100% (1)
- Billing Process: Prioritize Larger COINSURANCE Values 2. Get Copy of Remittance AdviceDocument1 pageBilling Process: Prioritize Larger COINSURANCE Values 2. Get Copy of Remittance AdviceHaira Joyce E. PunoNo ratings yet
- ICD 10 Training Sessions Training AgendaDocument3 pagesICD 10 Training Sessions Training AgendaAntonSusanto100% (1)
- Patient Information SystemDocument5 pagesPatient Information SystemJignesh DesaiNo ratings yet
- Medical Billing Resume ExamplesDocument7 pagesMedical Billing Resume Examplesbcr7r579100% (2)
- 0 - Basic HealthcareDocument19 pages0 - Basic HealthcareMd SaifNo ratings yet
- Medical Transcription Practice Sample PagesDocument2 pagesMedical Transcription Practice Sample PagesAmeerah CabangalNo ratings yet
- DocumentationDocument27 pagesDocumentationanju kumawatNo ratings yet
- Codes - Ontario PDFDocument104 pagesCodes - Ontario PDFprabal rayNo ratings yet
- CPB Online Medical Billing Syllabus - 11th - 4!17!13Document2 pagesCPB Online Medical Billing Syllabus - 11th - 4!17!13Kian GonzagaNo ratings yet
- EHRA InteroperabilityRoadmap 20090310 v3Document40 pagesEHRA InteroperabilityRoadmap 20090310 v3Anonymous JE7uJR100% (1)
- Medical Transcription Industry FactsDocument2 pagesMedical Transcription Industry FactsSrinivas Pandian0% (1)
- Freelancing QuestionDocument8 pagesFreelancing QuestionImran AliNo ratings yet
- Utilization Review Coordinator: Passbooks Study GuideFrom EverandUtilization Review Coordinator: Passbooks Study GuideNo ratings yet
- Apa Yang Harus Dipersiapkan Rumah Sakit Untuk Meningkatkan Keamanan Fasilitasnya ?Document17 pagesApa Yang Harus Dipersiapkan Rumah Sakit Untuk Meningkatkan Keamanan Fasilitasnya ?Mohammad IchsanNo ratings yet
- 3.8 SPH Self-Assessment 508 PDFDocument2 pages3.8 SPH Self-Assessment 508 PDFMohammad IchsanNo ratings yet
- Hand Book OshaDocument40 pagesHand Book OshaMohammad Ichsan100% (1)
- Kompetensi SDM Dan Kualitas Pelayanan Rumah Sakit: June 2012Document10 pagesKompetensi SDM Dan Kualitas Pelayanan Rumah Sakit: June 2012Mohammad IchsanNo ratings yet
- Agrarian Law and Social Legislation NotesDocument18 pagesAgrarian Law and Social Legislation Noteskenn1o1No ratings yet
- National Health Programs Final 150324130140 Conversion Gate01Document141 pagesNational Health Programs Final 150324130140 Conversion Gate01Manoj Garg100% (1)
- Request For Permit To Work (PTW) - Contactor Application: PLTG 75 MW Paya Pasir MedanDocument2 pagesRequest For Permit To Work (PTW) - Contactor Application: PLTG 75 MW Paya Pasir MedanDimas Dwi SwarnaNo ratings yet
- Deciding JCT Contract Practice GuideDocument43 pagesDeciding JCT Contract Practice GuideKajendra100% (2)
- CFR 2019 Title30 Vol1Document806 pagesCFR 2019 Title30 Vol1Carlos Ernesto Flores AlbinoNo ratings yet
- Leader Analysis-John MackeyDocument8 pagesLeader Analysis-John Mackeyapi-272623096No ratings yet
- Social Health Protection Toward UHC in Lao PDRDocument16 pagesSocial Health Protection Toward UHC in Lao PDRADBI EventsNo ratings yet
- Business Excellence AwardDocument18 pagesBusiness Excellence AwardKarthikeyan NatarajanNo ratings yet
- Maklumat Vaksinasi: Vaccination DetailsDocument2 pagesMaklumat Vaksinasi: Vaccination DetailsHakim FawwazNo ratings yet
- Health PDFDocument9 pagesHealth PDFAnshul SinghalNo ratings yet
- 2020 SK Accomplishment ReportDocument36 pages2020 SK Accomplishment ReportRegine Rosillo100% (2)
- 08-30-14 EditionDocument36 pages08-30-14 EditionSan Mateo Daily JournalNo ratings yet
- Know About United State Pharmacopoeia (Usp) by Dr.T.V.Vidyasagar Neuheit Pharma Technologies Private LimitedDocument13 pagesKnow About United State Pharmacopoeia (Usp) by Dr.T.V.Vidyasagar Neuheit Pharma Technologies Private LimitedtvvsagarNo ratings yet
- Chapter 1Document9 pagesChapter 1Antun RahmadiNo ratings yet
- The Inversion of Exceptionality: Foucault, Agamben, and "Reproductive Rights"Document17 pagesThe Inversion of Exceptionality: Foucault, Agamben, and "Reproductive Rights"HedvaNo ratings yet
- 2nd ARC Reports Unlocking Human CapitalDocument5 pages2nd ARC Reports Unlocking Human CapitalPrabhakar YadavNo ratings yet
- Aus Census Information 2016Document8 pagesAus Census Information 2016CaddlesmanNo ratings yet
- Medical EthicsDocument75 pagesMedical EthicsNenyAriyana100% (2)
- Irda Act & Types of InsuranceDocument19 pagesIrda Act & Types of InsuranceVinayak BhardwajNo ratings yet
- Article Ii Unlawful Acts and Penalties Section 11. Possession of Dangerous Drugs. - The Penalty of Life Imprisonment To Death and A FineDocument3 pagesArticle Ii Unlawful Acts and Penalties Section 11. Possession of Dangerous Drugs. - The Penalty of Life Imprisonment To Death and A FineCarol JacintoNo ratings yet
- Compendium-December, 2018Document61 pagesCompendium-December, 2018Shivam MishraNo ratings yet
- Rule 1010Document46 pagesRule 1010Kristel Gail BasilioNo ratings yet
- Federalism 101: Federalism Is A System of Government in Which Power Is Divided Between A NationalDocument1 pageFederalism 101: Federalism Is A System of Government in Which Power Is Divided Between A NationalJhoana Parica FranciscoNo ratings yet
- Badac Plan of ActionDocument5 pagesBadac Plan of ActionTaz HalipaNo ratings yet
- NCQA PrimerDocument53 pagesNCQA Primerd_anto781063No ratings yet