Professional Documents
Culture Documents
Safety: Falls: Impaired Mobility: Common Causes: Sensory Deficits, Parkinson, Diabetic Neuropathy
Safety: Falls: Impaired Mobility: Common Causes: Sensory Deficits, Parkinson, Diabetic Neuropathy
Uploaded by
Breeana MooreCopyright:
Available Formats
You might also like
- Sheehys Emergency Nursing Principles and Practice 7th EditionDocument61 pagesSheehys Emergency Nursing Principles and Practice 7th Editiontheresa.whitley25893% (56)
- Geriatric Nursing Review QuestionsDocument30 pagesGeriatric Nursing Review QuestionsPortia Dulce Toquero87% (93)
- Training ManualDocument41 pagesTraining Manualemiliow_1100% (3)
- Drug Information Tertiary Resources GameDocument46 pagesDrug Information Tertiary Resources Gameapi-661456802No ratings yet
- Case Study of DementiaDocument9 pagesCase Study of DementiaNsengimana Eric Maxigy50% (2)
- H06D Assignment 8Document4 pagesH06D Assignment 8Good ChannelNo ratings yet
- Cerebral PalsyDocument21 pagesCerebral PalsyEMily AbastaNo ratings yet
- NCLEX (Valerie) PDFDocument18 pagesNCLEX (Valerie) PDFValerie Orengo100% (1)
- Safety: Falls: Assessment: For Clients at Risk Repeat Risk Assessment Every 8hrs & Monitor More Freq. IdentifyDocument1 pageSafety: Falls: Assessment: For Clients at Risk Repeat Risk Assessment Every 8hrs & Monitor More Freq. IdentifyBreeana MooreNo ratings yet
- OrthosDocument6 pagesOrthosBatch V Med 2 SY 21-22No ratings yet
- Cerebral Palsy MXDocument34 pagesCerebral Palsy MXNeeraj VermaNo ratings yet
- Bullets in PsycheDocument115 pagesBullets in PsycheFEVIE ANNE BANATAONo ratings yet
- Value of Observations in Homoeopathic PracticeDocument6 pagesValue of Observations in Homoeopathic PracticeHomoeopathic Pulse100% (3)
- Physical AssessmentDocument20 pagesPhysical Assessmentkylemabanta123No ratings yet
- Health HistoryDocument7 pagesHealth HistoryAnnapurna DangetiNo ratings yet
- Group 1 - Alzheimers Disease Case StudyDocument34 pagesGroup 1 - Alzheimers Disease Case StudyMariah Ainna B. MatienzoNo ratings yet
- Neurological Disorder (Cerebral Palsy)Document2 pagesNeurological Disorder (Cerebral Palsy)Araw GabiNo ratings yet
- The Nervous System EditedDocument7 pagesThe Nervous System EditedFev BanataoNo ratings yet
- Feline Hyperesthesia Syndrome in Cats (Felis) - VetlexiconDocument5 pagesFeline Hyperesthesia Syndrome in Cats (Felis) - VetlexiconAna Clara SantosNo ratings yet
- Neuro Study GuideDocument19 pagesNeuro Study GuideMelissa SmirnowNo ratings yet
- CP Case PreDocument35 pagesCP Case PreCatherine CarmonaNo ratings yet
- Clinical Approach andDocument21 pagesClinical Approach andtavooppNo ratings yet
- Team 2 Case Study EpilepsyDocument15 pagesTeam 2 Case Study EpilepsytmgursalNo ratings yet
- Ataxia: Pediatric Neurology Quick TalksDocument18 pagesAtaxia: Pediatric Neurology Quick TalksAlex GasnasNo ratings yet
- Any Process That Can Disrupt Neuronal Function and ConnectivityDocument5 pagesAny Process That Can Disrupt Neuronal Function and ConnectivityElle RosalesNo ratings yet
- Motor Stereotypies PDFDocument5 pagesMotor Stereotypies PDFGiga Hasabi AlkaraniNo ratings yet
- Ad HD MSDocument16 pagesAd HD MSangelaNo ratings yet
- Congential 3 Musculoskeletal 3 Neurological 3 Abusive DisordersDocument7 pagesCongential 3 Musculoskeletal 3 Neurological 3 Abusive DisordersNichole CollinsNo ratings yet
- Case Study 3-ADocument4 pagesCase Study 3-AEsty NandoNo ratings yet
- OSCE Must Knows For All SubjectsDocument8 pagesOSCE Must Knows For All SubjectsPrincess Jeanne Roque GairanodNo ratings yet
- CP CASE PRE FinalDocument35 pagesCP CASE PRE FinalCatherine CarmonaNo ratings yet
- Nurs 205 Concept MapDocument1 pageNurs 205 Concept MapJami SpearsNo ratings yet
- Comatose PatientDocument11 pagesComatose PatientUWIMANA Jean ClaudeNo ratings yet
- Cerebral PalsyDocument9 pagesCerebral PalsyAngy100% (2)
- Observation of The Patient When They Walk in - : HistoryDocument19 pagesObservation of The Patient When They Walk in - : Historyajaykumar soddalaNo ratings yet
- Chapter 5 PRT 1Document10 pagesChapter 5 PRT 1nayaddouaihyNo ratings yet
- Dizziness: Health Education Library For PeopleDocument2 pagesDizziness: Health Education Library For PeopleNaidu VegiNo ratings yet
- Cga 1Document37 pagesCga 1UDDE-E MARISABELNo ratings yet
- TLOY CLIN MED HEENT - Head Face NeckDocument11 pagesTLOY CLIN MED HEENT - Head Face NeckTRINIDAD, ALYANNA V.No ratings yet
- Anxiety DisorderDocument3 pagesAnxiety DisordergwenstacyNo ratings yet
- Cerebral PalsyDocument11 pagesCerebral PalsySanthosh.S.UNo ratings yet
- Genetic Disorders: U Me and SocietyDocument23 pagesGenetic Disorders: U Me and SocietyDeepansh GuptaNo ratings yet
- Status POMR LBPDocument4 pagesStatus POMR LBPGiovanno HermawanNo ratings yet
- Physiotherapy For Patients With Spina Bifida Cystica1Document11 pagesPhysiotherapy For Patients With Spina Bifida Cystica1Dimple GoyalNo ratings yet
- Checklist HEAD and NECKDocument8 pagesChecklist HEAD and NECKAezyreal Anne MirallesNo ratings yet
- Week 12 - Care of The Pediatric Client With Neurologic DisorderDocument66 pagesWeek 12 - Care of The Pediatric Client With Neurologic DisorderJaja ManezNo ratings yet
- Approach To Floppy Infant: LT Col (DR) Bindu T Nair Professor (Pediatrics)Document56 pagesApproach To Floppy Infant: LT Col (DR) Bindu T Nair Professor (Pediatrics)Dorjee SengeNo ratings yet
- Seizure Disorder Types: Partial - Local Onset May or May Not Impair Consciousness SimpleDocument4 pagesSeizure Disorder Types: Partial - Local Onset May or May Not Impair Consciousness Simpleampogison08No ratings yet
- Advanced Understanding of AutismDocument35 pagesAdvanced Understanding of AutismShanu JudNo ratings yet
- HA LEC Module 8 and 9 1Document30 pagesHA LEC Module 8 and 9 1Althea Sachi CruzNo ratings yet
- Case Study Activity 1-4Document7 pagesCase Study Activity 1-4kuma phNo ratings yet
- PemicuDocument34 pagesPemicuCindy SugandaNo ratings yet
- Neuro AssessmentDocument13 pagesNeuro Assessmentyassyrn100% (2)
- Approach To Loss of Counsciousness FinalDocument38 pagesApproach To Loss of Counsciousness FinalManish ShresthaNo ratings yet
- Care of Older Adult ReviewerDocument3 pagesCare of Older Adult ReviewerJennica BubanNo ratings yet
- Neurologic Disorder FinalDocument9 pagesNeurologic Disorder FinalMary Reigns BuhatNo ratings yet
- Practical NeuroDocument11 pagesPractical NeurokbaguyoNo ratings yet
- PHC Cold Weather Injury TrainingDocument41 pagesPHC Cold Weather Injury TrainingKolaNo ratings yet
- Back Pain in Children and AdolescentsDocument11 pagesBack Pain in Children and AdolescentsBariša KiršnerNo ratings yet
- Crib Sheet E4Document2 pagesCrib Sheet E4Anais Hall-GarrisonNo ratings yet
- Nursing Interview Guide To Collect Subjective Data From The Client Questions RationaleDocument19 pagesNursing Interview Guide To Collect Subjective Data From The Client Questions RationaleKent Rebong100% (1)
- The Psychology of Hysteria - A Selection of Classic Articles on the Analysis and Symptoms of HysteriaFrom EverandThe Psychology of Hysteria - A Selection of Classic Articles on the Analysis and Symptoms of HysteriaNo ratings yet
- Med Surg 1 Exam 1Document23 pagesMed Surg 1 Exam 1Breeana MooreNo ratings yet
- Risk For Injury T1 MSDocument1 pageRisk For Injury T1 MSBreeana MooreNo ratings yet
- Dementia: Diagnosis Testing: CBC, Chemistry Profile, NM: Safe Environment, Watch For Sundowning, Risk For Falls, PromoteDocument1 pageDementia: Diagnosis Testing: CBC, Chemistry Profile, NM: Safe Environment, Watch For Sundowning, Risk For Falls, PromoteBreeana MooreNo ratings yet
- Safety: Falls: Assessment: For Clients at Risk Repeat Risk Assessment Every 8hrs & Monitor More Freq. IdentifyDocument1 pageSafety: Falls: Assessment: For Clients at Risk Repeat Risk Assessment Every 8hrs & Monitor More Freq. IdentifyBreeana MooreNo ratings yet
- This Study Resource Was: Mental Health Case: George PaloDocument2 pagesThis Study Resource Was: Mental Health Case: George PaloKyuSheenNo ratings yet
- Assessing Older DriversDocument5 pagesAssessing Older DriversArt SmithNo ratings yet
- Elderly Hip Fracture PatientsDocument7 pagesElderly Hip Fracture PatientspamancastroNo ratings yet
- Jgs 14518 PDFDocument8 pagesJgs 14518 PDFDes LastrianiNo ratings yet
- Introduction To Geriatric Medicine (Presentation) Author Edwin GomesDocument34 pagesIntroduction To Geriatric Medicine (Presentation) Author Edwin GomesSHERIF ZAHERNo ratings yet
- Comprehensive Geriatric Assessment A Summary (Article) Author Hamilton Southeastern SchoolsDocument6 pagesComprehensive Geriatric Assessment A Summary (Article) Author Hamilton Southeastern SchoolsSHERIF ZAHERNo ratings yet
- Tinetti Balance Scale InstrumentDocument2 pagesTinetti Balance Scale InstrumentInilah Namanya WestaNo ratings yet
- Ebook Ebook PDF Practice Guidelines For Family Nurse Practitioners 4th Edition PDFDocument41 pagesEbook Ebook PDF Practice Guidelines For Family Nurse Practitioners 4th Edition PDFbarbara.coakley466100% (34)
- Ags Panel On Persistent Pain in Older Persons PDFDocument20 pagesAgs Panel On Persistent Pain in Older Persons PDFHery SezanoNo ratings yet
- COVID 19 - Clinical Picture in The Elderly Population: A Qualitative Systematic ReviewDocument21 pagesCOVID 19 - Clinical Picture in The Elderly Population: A Qualitative Systematic ReviewRila RivandaNo ratings yet
- Aspen - EspenDocument38 pagesAspen - EspenJake BastoNo ratings yet
- 06 Chapter PDFDocument178 pages06 Chapter PDFanon_151515667No ratings yet
- Restraint Paper 3Document9 pagesRestraint Paper 3api-404185844No ratings yet
- Geriatric AssessmentDocument2 pagesGeriatric AssessmentAzubuike Ifejoku-ChukwukaNo ratings yet
- Senior Care CompettionDocument6 pagesSenior Care CompettionRafNo ratings yet
- Geria Session 1Document5 pagesGeria Session 1Cyril CayabyabNo ratings yet
- Geriatric Functional Rating Scale (GFRS)Document5 pagesGeriatric Functional Rating Scale (GFRS)Navina SureshNo ratings yet
- NSG 131.1 - DAY 2 Narrative ReportDocument1 pageNSG 131.1 - DAY 2 Narrative ReportNadja JamilahNo ratings yet
- Assessment of The Elderly Patient: Noel H. Ponce MDDocument33 pagesAssessment of The Elderly Patient: Noel H. Ponce MDlovelots1234No ratings yet
- Elderly Services in Health CentersDocument73 pagesElderly Services in Health CentersHsk MiaoNo ratings yet
- KWCCSP 02 PDFDocument156 pagesKWCCSP 02 PDFChung Pui SzeNo ratings yet
- Patient Fall - KKM Guideline 2019Document66 pagesPatient Fall - KKM Guideline 2019Nor Athirah HassanNo ratings yet
- Daftar Pustaka 13 Permasalahan Terkait Obat Antihipertensi Pada Pasien Usia Lanjut Di Poli Geriatri RSUD DR - Soetomo PDFDocument6 pagesDaftar Pustaka 13 Permasalahan Terkait Obat Antihipertensi Pada Pasien Usia Lanjut Di Poli Geriatri RSUD DR - Soetomo PDFDave AbrahamNo ratings yet
- Comprehensive Management SarcopeniaDocument25 pagesComprehensive Management SarcopeniaMardikaNo ratings yet
- Projecct Proposal PDFDocument20 pagesProjecct Proposal PDFMelbin BijuNo ratings yet
Safety: Falls: Impaired Mobility: Common Causes: Sensory Deficits, Parkinson, Diabetic Neuropathy
Safety: Falls: Impaired Mobility: Common Causes: Sensory Deficits, Parkinson, Diabetic Neuropathy
Uploaded by
Breeana MooreOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Safety: Falls: Impaired Mobility: Common Causes: Sensory Deficits, Parkinson, Diabetic Neuropathy
Safety: Falls: Impaired Mobility: Common Causes: Sensory Deficits, Parkinson, Diabetic Neuropathy
Uploaded by
Breeana MooreCopyright:
Available Formats
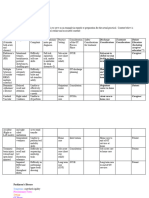
Assessment: For clients at risk repeat risk assessment every 8hrs
Safety: Falls RF: Sensory issues, hypotension, hx falls, pain, & monitor more freq. Identify meds that ^ risk for falling. Use
dizziness, etoh use, 80+, gait, infants Morse Fall scale, Get up & Go test, comprehensive fall evaluation
Causes: Footwear, postural hypotension, tripping hazards, poor
lighting, alcohol, polypharmacy, meds
More than ½ falls reserve in home, 80% 65+, 3rd injury related death.
Most common incident reported in hospitals and LTC. Interventions: Most important thing is to find out
Many cases involve falling from a bed, most likely at night, holidays, weekends. who is at risk for falls.
Ranks 7th cod for elderly, highest in 85+, usually cause hip fracture. Provide a safe environment: bed low, no clutter, lock
wheels/chairs/beds, call light close, nonskid socks –
brightly colored, orient to surroundings, assist when
needed. Assess, teach, support. Hourly rounding,
Geriatric triad: Changes in cognitive status, falls, incontinent (all 3)
surveillance of older adults. Document.
Geriatric syn.: # of problems-does not fit into discrete disease
categories requires a multidisciplinary + comprehensive assessment Dizziness: Older pts seek help often for dizziness.
to identify the underlying cause. *Skin impairment, poor nutrition, Hard to differentiate between true dizziness
falls, functional decline. May develop gradually but onset acute. (sensation of disorientation r/t position) vertigo
(spinning sensation). Similar sensations nearsyncope
+ disequilibrium – minor (built ear wax) Serve
(dysfunction of cerebral cortex, cerebellum, brain
Impaired mobility: Common causes: sensory deficits, parkinson, diabetic neuropathy, stem, proprioceptive receptors
cardiovascular comp, osteoarthritis
Older pts should remain active as much as poss. If bed rest cannot be avoided pts should
preform active rom + strengthening exercises w/the unaffected extremities – caregivers +
nurse should preform passive rom – freq position changes
You might also like
- Sheehys Emergency Nursing Principles and Practice 7th EditionDocument61 pagesSheehys Emergency Nursing Principles and Practice 7th Editiontheresa.whitley25893% (56)
- Geriatric Nursing Review QuestionsDocument30 pagesGeriatric Nursing Review QuestionsPortia Dulce Toquero87% (93)
- Training ManualDocument41 pagesTraining Manualemiliow_1100% (3)
- Drug Information Tertiary Resources GameDocument46 pagesDrug Information Tertiary Resources Gameapi-661456802No ratings yet
- Case Study of DementiaDocument9 pagesCase Study of DementiaNsengimana Eric Maxigy50% (2)
- H06D Assignment 8Document4 pagesH06D Assignment 8Good ChannelNo ratings yet
- Cerebral PalsyDocument21 pagesCerebral PalsyEMily AbastaNo ratings yet
- NCLEX (Valerie) PDFDocument18 pagesNCLEX (Valerie) PDFValerie Orengo100% (1)
- Safety: Falls: Assessment: For Clients at Risk Repeat Risk Assessment Every 8hrs & Monitor More Freq. IdentifyDocument1 pageSafety: Falls: Assessment: For Clients at Risk Repeat Risk Assessment Every 8hrs & Monitor More Freq. IdentifyBreeana MooreNo ratings yet
- OrthosDocument6 pagesOrthosBatch V Med 2 SY 21-22No ratings yet
- Cerebral Palsy MXDocument34 pagesCerebral Palsy MXNeeraj VermaNo ratings yet
- Bullets in PsycheDocument115 pagesBullets in PsycheFEVIE ANNE BANATAONo ratings yet
- Value of Observations in Homoeopathic PracticeDocument6 pagesValue of Observations in Homoeopathic PracticeHomoeopathic Pulse100% (3)
- Physical AssessmentDocument20 pagesPhysical Assessmentkylemabanta123No ratings yet
- Health HistoryDocument7 pagesHealth HistoryAnnapurna DangetiNo ratings yet
- Group 1 - Alzheimers Disease Case StudyDocument34 pagesGroup 1 - Alzheimers Disease Case StudyMariah Ainna B. MatienzoNo ratings yet
- Neurological Disorder (Cerebral Palsy)Document2 pagesNeurological Disorder (Cerebral Palsy)Araw GabiNo ratings yet
- The Nervous System EditedDocument7 pagesThe Nervous System EditedFev BanataoNo ratings yet
- Feline Hyperesthesia Syndrome in Cats (Felis) - VetlexiconDocument5 pagesFeline Hyperesthesia Syndrome in Cats (Felis) - VetlexiconAna Clara SantosNo ratings yet
- Neuro Study GuideDocument19 pagesNeuro Study GuideMelissa SmirnowNo ratings yet
- CP Case PreDocument35 pagesCP Case PreCatherine CarmonaNo ratings yet
- Clinical Approach andDocument21 pagesClinical Approach andtavooppNo ratings yet
- Team 2 Case Study EpilepsyDocument15 pagesTeam 2 Case Study EpilepsytmgursalNo ratings yet
- Ataxia: Pediatric Neurology Quick TalksDocument18 pagesAtaxia: Pediatric Neurology Quick TalksAlex GasnasNo ratings yet
- Any Process That Can Disrupt Neuronal Function and ConnectivityDocument5 pagesAny Process That Can Disrupt Neuronal Function and ConnectivityElle RosalesNo ratings yet
- Motor Stereotypies PDFDocument5 pagesMotor Stereotypies PDFGiga Hasabi AlkaraniNo ratings yet
- Ad HD MSDocument16 pagesAd HD MSangelaNo ratings yet
- Congential 3 Musculoskeletal 3 Neurological 3 Abusive DisordersDocument7 pagesCongential 3 Musculoskeletal 3 Neurological 3 Abusive DisordersNichole CollinsNo ratings yet
- Case Study 3-ADocument4 pagesCase Study 3-AEsty NandoNo ratings yet
- OSCE Must Knows For All SubjectsDocument8 pagesOSCE Must Knows For All SubjectsPrincess Jeanne Roque GairanodNo ratings yet
- CP CASE PRE FinalDocument35 pagesCP CASE PRE FinalCatherine CarmonaNo ratings yet
- Nurs 205 Concept MapDocument1 pageNurs 205 Concept MapJami SpearsNo ratings yet
- Comatose PatientDocument11 pagesComatose PatientUWIMANA Jean ClaudeNo ratings yet
- Cerebral PalsyDocument9 pagesCerebral PalsyAngy100% (2)
- Observation of The Patient When They Walk in - : HistoryDocument19 pagesObservation of The Patient When They Walk in - : Historyajaykumar soddalaNo ratings yet
- Chapter 5 PRT 1Document10 pagesChapter 5 PRT 1nayaddouaihyNo ratings yet
- Dizziness: Health Education Library For PeopleDocument2 pagesDizziness: Health Education Library For PeopleNaidu VegiNo ratings yet
- Cga 1Document37 pagesCga 1UDDE-E MARISABELNo ratings yet
- TLOY CLIN MED HEENT - Head Face NeckDocument11 pagesTLOY CLIN MED HEENT - Head Face NeckTRINIDAD, ALYANNA V.No ratings yet
- Anxiety DisorderDocument3 pagesAnxiety DisordergwenstacyNo ratings yet
- Cerebral PalsyDocument11 pagesCerebral PalsySanthosh.S.UNo ratings yet
- Genetic Disorders: U Me and SocietyDocument23 pagesGenetic Disorders: U Me and SocietyDeepansh GuptaNo ratings yet
- Status POMR LBPDocument4 pagesStatus POMR LBPGiovanno HermawanNo ratings yet
- Physiotherapy For Patients With Spina Bifida Cystica1Document11 pagesPhysiotherapy For Patients With Spina Bifida Cystica1Dimple GoyalNo ratings yet
- Checklist HEAD and NECKDocument8 pagesChecklist HEAD and NECKAezyreal Anne MirallesNo ratings yet
- Week 12 - Care of The Pediatric Client With Neurologic DisorderDocument66 pagesWeek 12 - Care of The Pediatric Client With Neurologic DisorderJaja ManezNo ratings yet
- Approach To Floppy Infant: LT Col (DR) Bindu T Nair Professor (Pediatrics)Document56 pagesApproach To Floppy Infant: LT Col (DR) Bindu T Nair Professor (Pediatrics)Dorjee SengeNo ratings yet
- Seizure Disorder Types: Partial - Local Onset May or May Not Impair Consciousness SimpleDocument4 pagesSeizure Disorder Types: Partial - Local Onset May or May Not Impair Consciousness Simpleampogison08No ratings yet
- Advanced Understanding of AutismDocument35 pagesAdvanced Understanding of AutismShanu JudNo ratings yet
- HA LEC Module 8 and 9 1Document30 pagesHA LEC Module 8 and 9 1Althea Sachi CruzNo ratings yet
- Case Study Activity 1-4Document7 pagesCase Study Activity 1-4kuma phNo ratings yet
- PemicuDocument34 pagesPemicuCindy SugandaNo ratings yet
- Neuro AssessmentDocument13 pagesNeuro Assessmentyassyrn100% (2)
- Approach To Loss of Counsciousness FinalDocument38 pagesApproach To Loss of Counsciousness FinalManish ShresthaNo ratings yet
- Care of Older Adult ReviewerDocument3 pagesCare of Older Adult ReviewerJennica BubanNo ratings yet
- Neurologic Disorder FinalDocument9 pagesNeurologic Disorder FinalMary Reigns BuhatNo ratings yet
- Practical NeuroDocument11 pagesPractical NeurokbaguyoNo ratings yet
- PHC Cold Weather Injury TrainingDocument41 pagesPHC Cold Weather Injury TrainingKolaNo ratings yet
- Back Pain in Children and AdolescentsDocument11 pagesBack Pain in Children and AdolescentsBariša KiršnerNo ratings yet
- Crib Sheet E4Document2 pagesCrib Sheet E4Anais Hall-GarrisonNo ratings yet
- Nursing Interview Guide To Collect Subjective Data From The Client Questions RationaleDocument19 pagesNursing Interview Guide To Collect Subjective Data From The Client Questions RationaleKent Rebong100% (1)
- The Psychology of Hysteria - A Selection of Classic Articles on the Analysis and Symptoms of HysteriaFrom EverandThe Psychology of Hysteria - A Selection of Classic Articles on the Analysis and Symptoms of HysteriaNo ratings yet
- Med Surg 1 Exam 1Document23 pagesMed Surg 1 Exam 1Breeana MooreNo ratings yet
- Risk For Injury T1 MSDocument1 pageRisk For Injury T1 MSBreeana MooreNo ratings yet
- Dementia: Diagnosis Testing: CBC, Chemistry Profile, NM: Safe Environment, Watch For Sundowning, Risk For Falls, PromoteDocument1 pageDementia: Diagnosis Testing: CBC, Chemistry Profile, NM: Safe Environment, Watch For Sundowning, Risk For Falls, PromoteBreeana MooreNo ratings yet
- Safety: Falls: Assessment: For Clients at Risk Repeat Risk Assessment Every 8hrs & Monitor More Freq. IdentifyDocument1 pageSafety: Falls: Assessment: For Clients at Risk Repeat Risk Assessment Every 8hrs & Monitor More Freq. IdentifyBreeana MooreNo ratings yet
- This Study Resource Was: Mental Health Case: George PaloDocument2 pagesThis Study Resource Was: Mental Health Case: George PaloKyuSheenNo ratings yet
- Assessing Older DriversDocument5 pagesAssessing Older DriversArt SmithNo ratings yet
- Elderly Hip Fracture PatientsDocument7 pagesElderly Hip Fracture PatientspamancastroNo ratings yet
- Jgs 14518 PDFDocument8 pagesJgs 14518 PDFDes LastrianiNo ratings yet
- Introduction To Geriatric Medicine (Presentation) Author Edwin GomesDocument34 pagesIntroduction To Geriatric Medicine (Presentation) Author Edwin GomesSHERIF ZAHERNo ratings yet
- Comprehensive Geriatric Assessment A Summary (Article) Author Hamilton Southeastern SchoolsDocument6 pagesComprehensive Geriatric Assessment A Summary (Article) Author Hamilton Southeastern SchoolsSHERIF ZAHERNo ratings yet
- Tinetti Balance Scale InstrumentDocument2 pagesTinetti Balance Scale InstrumentInilah Namanya WestaNo ratings yet
- Ebook Ebook PDF Practice Guidelines For Family Nurse Practitioners 4th Edition PDFDocument41 pagesEbook Ebook PDF Practice Guidelines For Family Nurse Practitioners 4th Edition PDFbarbara.coakley466100% (34)
- Ags Panel On Persistent Pain in Older Persons PDFDocument20 pagesAgs Panel On Persistent Pain in Older Persons PDFHery SezanoNo ratings yet
- COVID 19 - Clinical Picture in The Elderly Population: A Qualitative Systematic ReviewDocument21 pagesCOVID 19 - Clinical Picture in The Elderly Population: A Qualitative Systematic ReviewRila RivandaNo ratings yet
- Aspen - EspenDocument38 pagesAspen - EspenJake BastoNo ratings yet
- 06 Chapter PDFDocument178 pages06 Chapter PDFanon_151515667No ratings yet
- Restraint Paper 3Document9 pagesRestraint Paper 3api-404185844No ratings yet
- Geriatric AssessmentDocument2 pagesGeriatric AssessmentAzubuike Ifejoku-ChukwukaNo ratings yet
- Senior Care CompettionDocument6 pagesSenior Care CompettionRafNo ratings yet
- Geria Session 1Document5 pagesGeria Session 1Cyril CayabyabNo ratings yet
- Geriatric Functional Rating Scale (GFRS)Document5 pagesGeriatric Functional Rating Scale (GFRS)Navina SureshNo ratings yet
- NSG 131.1 - DAY 2 Narrative ReportDocument1 pageNSG 131.1 - DAY 2 Narrative ReportNadja JamilahNo ratings yet
- Assessment of The Elderly Patient: Noel H. Ponce MDDocument33 pagesAssessment of The Elderly Patient: Noel H. Ponce MDlovelots1234No ratings yet
- Elderly Services in Health CentersDocument73 pagesElderly Services in Health CentersHsk MiaoNo ratings yet
- KWCCSP 02 PDFDocument156 pagesKWCCSP 02 PDFChung Pui SzeNo ratings yet
- Patient Fall - KKM Guideline 2019Document66 pagesPatient Fall - KKM Guideline 2019Nor Athirah HassanNo ratings yet
- Daftar Pustaka 13 Permasalahan Terkait Obat Antihipertensi Pada Pasien Usia Lanjut Di Poli Geriatri RSUD DR - Soetomo PDFDocument6 pagesDaftar Pustaka 13 Permasalahan Terkait Obat Antihipertensi Pada Pasien Usia Lanjut Di Poli Geriatri RSUD DR - Soetomo PDFDave AbrahamNo ratings yet
- Comprehensive Management SarcopeniaDocument25 pagesComprehensive Management SarcopeniaMardikaNo ratings yet
- Projecct Proposal PDFDocument20 pagesProjecct Proposal PDFMelbin BijuNo ratings yet