Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
49 viewsLFTS - Types of Jaundice
LFTS - Types of Jaundice
Uploaded by
Sumaira JunaidThis document discusses various liver function tests (LFTs) and what they indicate about liver health and function. It explains that LFTs measure blood components like bilirubin, aminotransferases, alkaline phosphatase, albumin, GGT, and PT/INR to provide insight into liver damage, metabolism, and excretory function. Specific LFT abnormalities can suggest pre-hepatic, hepatic, or post-hepatic etiologies and whether the liver is experiencing damage, obstruction, or other issues. Chronic conditions like hepatitis or cirrhosis can also impact LFT results over time.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You might also like
- Pathophysiology LeptospirosisDocument1 pagePathophysiology Leptospirosisjeoffrey_castro100% (3)
- Differential Diagnosis of JaundiceDocument4 pagesDifferential Diagnosis of JaundiceVirag PatilNo ratings yet
- Organ Function Test: Assessment of Functions of The OrgansDocument39 pagesOrgan Function Test: Assessment of Functions of The OrgansSri Abinash MishraNo ratings yet
- Liver FunctionDocument90 pagesLiver Functionapi-19641337100% (1)
- Liver Function Test: Liver Hilang Bagian Masih Bisa KompensasiDocument53 pagesLiver Function Test: Liver Hilang Bagian Masih Bisa KompensasiKharisulNo ratings yet
- Liver MarkersDocument4 pagesLiver MarkerslucaNo ratings yet
- Liver PathologyDocument35 pagesLiver Pathologynhgwdwffp2No ratings yet
- 15 Coned CCRN GastrointestinalDocument21 pages15 Coned CCRN GastrointestinalAkbar TaufikNo ratings yet
- 1.1 Liver Function Tests 15.02.19Document39 pages1.1 Liver Function Tests 15.02.19Syed ArefinNo ratings yet
- Liver Function Test: Maimun ZA Lab Patologi Klinik Fkub-RssaDocument26 pagesLiver Function Test: Maimun ZA Lab Patologi Klinik Fkub-RssaSaifuddin BadarsyahNo ratings yet
- LFTSDocument34 pagesLFTSJoseline AliceNo ratings yet
- Liver DiseasesDocument24 pagesLiver DiseasesAbdo HaiderNo ratings yet
- Liver Panel: EM 6203 Dr. K. AikenheadDocument24 pagesLiver Panel: EM 6203 Dr. K. AikenheadCrystal Lynn Keener SciariniNo ratings yet
- A Case Oriented Approach To Liver Laboratory Profiling in Dogs and CatsDocument5 pagesA Case Oriented Approach To Liver Laboratory Profiling in Dogs and CatsAbelantonNo ratings yet
- Total Protein Albumin + Globulins (Ig, Complements, Fibrinogen, A1-Antrypsin Etc)Document4 pagesTotal Protein Albumin + Globulins (Ig, Complements, Fibrinogen, A1-Antrypsin Etc)bryan chan100% (1)
- Liver Function TesDocument58 pagesLiver Function TesnoffrizalNo ratings yet
- Molecular BiologyDocument17 pagesMolecular BiologyMzwandile NyawoseNo ratings yet
- Which of The Two Is More Liver Specific and Increases More During Liver DiseaseDocument8 pagesWhich of The Two Is More Liver Specific and Increases More During Liver DiseaseMariel AbatayoNo ratings yet
- Liver Function TestDocument25 pagesLiver Function Testnuradinman89No ratings yet
- Liver Function Tests InterpretationDocument2 pagesLiver Function Tests InterpretationdarrenkongNo ratings yet
- Liver Function Tests PDFDocument6 pagesLiver Function Tests PDFSubhash Digambar VisalNo ratings yet
- 07 Liver Tunction TestsDocument41 pages07 Liver Tunction TestsPaulina PaskeviciuteNo ratings yet
- Liver Function TestsDocument17 pagesLiver Function TestsHung Lam100% (1)
- JAUNDICE Internal Medicine PresentationDocument34 pagesJAUNDICE Internal Medicine PresentationNano BaddourNo ratings yet
- Liver Function Tests (Sem)Document6 pagesLiver Function Tests (Sem)Francisco NiegasNo ratings yet
- Pemeriksaan Fungsi Hati, DR - DiahDocument42 pagesPemeriksaan Fungsi Hati, DR - DiahYuliana LatifNo ratings yet
- Approach To A Patient With JaundiceDocument33 pagesApproach To A Patient With JaundiceRahul Kumar VermaNo ratings yet
- Enzymes Liver Pancreas FCDocument10 pagesEnzymes Liver Pancreas FCLois Lipanovich100% (1)
- Professor Dr. Najat A. HasanDocument40 pagesProfessor Dr. Najat A. HasanPeter MungaiNo ratings yet
- Liver Function Test 2011Document26 pagesLiver Function Test 2011anisa rachmitaNo ratings yet
- Pathophysiology of Laboratory Abnormalities in Liver DisordersDocument55 pagesPathophysiology of Laboratory Abnormalities in Liver DisordersYudha fedrian AKNo ratings yet
- Lect. 8Document30 pagesLect. 8jayNo ratings yet
- Hepatobiliary Diseases 3Document28 pagesHepatobiliary Diseases 3AmirahNo ratings yet
- Liver Function Test by Alaa Abass PMDocument48 pagesLiver Function Test by Alaa Abass PMalaamabass93No ratings yet
- Liver Function Tests: Dr. ThomasDocument32 pagesLiver Function Tests: Dr. ThomasthomaskodiatteNo ratings yet
- Chem-Dr - Zainab-Bilirubin-Lab 2Document10 pagesChem-Dr - Zainab-Bilirubin-Lab 2gmpcbpzdysNo ratings yet
- 5 - JaundiceDocument16 pages5 - JaundiceHamzehNo ratings yet
- Obstructive Jaundice Group 6Document33 pagesObstructive Jaundice Group 6Qurbon AliNo ratings yet
- Hepatic Function TestsDocument12 pagesHepatic Function TestsalhassanmohamedNo ratings yet
- Liver Function Tests (LFTS) : Group TwoDocument12 pagesLiver Function Tests (LFTS) : Group TwoStanley KarugaNo ratings yet
- Liver Function TestsDocument48 pagesLiver Function TestsAli H. Sadiek أ.د. علي حسن صديق92% (13)
- Fisio 9Document9 pagesFisio 9anaNo ratings yet
- Organ Function TestDocument49 pagesOrgan Function TestmekuriawNo ratings yet
- Pemeriksaan Fungsi Hati .: Prof. Dr. Adi Koesoema Aman SPPK (KH)Document51 pagesPemeriksaan Fungsi Hati .: Prof. Dr. Adi Koesoema Aman SPPK (KH)kiki rawitriNo ratings yet
- Urea/ Ammonia Tests: Primary Liver Function TestsDocument6 pagesUrea/ Ammonia Tests: Primary Liver Function TestsMemory MahwendaNo ratings yet
- Liver (Hati) ZLDocument27 pagesLiver (Hati) ZLpafaniNo ratings yet
- Unit 8 - LIVER FUNCTION TESTSDocument93 pagesUnit 8 - LIVER FUNCTION TESTSRezan ThapaNo ratings yet
- Jaundice: Accumulation of Yellow Pigment in The Skin and Other Tissues (Bilirubin)Document65 pagesJaundice: Accumulation of Yellow Pigment in The Skin and Other Tissues (Bilirubin)qreenNo ratings yet
- Test LFTsDocument2 pagesTest LFTsostarburstoNo ratings yet
- Viral Hepatitis Diagnostic Test and Differential DiagnosisDocument21 pagesViral Hepatitis Diagnostic Test and Differential DiagnosisNedeln AudleyNo ratings yet
- Biochemistry - LG 1 (Liver Function Tests) - Dr. SalarDocument28 pagesBiochemistry - LG 1 (Liver Function Tests) - Dr. Salargabi.g.wahbeNo ratings yet
- Lucture 11functions of LiverDocument3 pagesLucture 11functions of Livermohammed jemalNo ratings yet
- Liver Function Tests: Shivansh Agarwal - 200201474Document16 pagesLiver Function Tests: Shivansh Agarwal - 200201474Shivansh AgarwalNo ratings yet
- Health Liver Interpretation and InterventionsDocument11 pagesHealth Liver Interpretation and InterventionsParas BansalNo ratings yet
- Approach To Jaundice (1) .PPT ALAWAJIDocument28 pagesApproach To Jaundice (1) .PPT ALAWAJIayuNo ratings yet
- Approach To The Patient With Abnormal Liver Tests: Alvaro Koch, M.DDocument47 pagesApproach To The Patient With Abnormal Liver Tests: Alvaro Koch, M.DTimotius Kevin NatanaelNo ratings yet
- Liver Function Tests: Presented By-Dr. Arshiya Kaura (JR 1)Document50 pagesLiver Function Tests: Presented By-Dr. Arshiya Kaura (JR 1)vikasNo ratings yet
- Liver - Lecture 1 by Dr. Rehma Dar (14-03-2020)Document16 pagesLiver - Lecture 1 by Dr. Rehma Dar (14-03-2020)khadhiNo ratings yet
- Liver Function Test: DescriptionDocument3 pagesLiver Function Test: DescriptionOkura JoshuaNo ratings yet
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo ratings yet
- Indira National School: I. Give Reason For The FollowingDocument3 pagesIndira National School: I. Give Reason For The FollowingUPANSH SETHNo ratings yet
- Histology of The Respiratory System 20152016Document44 pagesHistology of The Respiratory System 20152016mugilanNo ratings yet
- Renal PhysiologyDocument193 pagesRenal Physiologyramadan100% (1)
- Medical Student Career Paths BookDocument124 pagesMedical Student Career Paths BookMindi WindmillNo ratings yet
- ReflexologyDocument4 pagesReflexologyphong duongNo ratings yet
- BIO270 Tuto 5Document3 pagesBIO270 Tuto 5Mirza KarmilaNo ratings yet
- Nervous System Grade 9 ??Document53 pagesNervous System Grade 9 ??Alia LauderNo ratings yet
- BSC 100 Midterm Questions For Oral ExamDocument20 pagesBSC 100 Midterm Questions For Oral ExamNovochino CastilloNo ratings yet
- Brain AnatomyDocument71 pagesBrain Anatomyhimani bansalNo ratings yet
- Chapter 9 - Endocrine SystemDocument9 pagesChapter 9 - Endocrine SystemrishellemaepilonesNo ratings yet
- Functions of Each Part of The Intergumentary System.1Document61 pagesFunctions of Each Part of The Intergumentary System.1Jane Ilagan VizcoNo ratings yet
- OralcholecystographyDocument13 pagesOralcholecystographySuman PokhrelNo ratings yet
- AbnormalL Liver Function Test 2012Document59 pagesAbnormalL Liver Function Test 2012Nayan MaharjanNo ratings yet
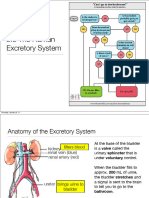
- SBI4U Unit 4 Homeostasis Excretory SystemDocument27 pagesSBI4U Unit 4 Homeostasis Excretory System전채연No ratings yet
- Harvade College of Science, Business and Management Studies Polt 1-12, Harvade Close, Off Obada Road Abeokuta Ogun StateDocument21 pagesHarvade College of Science, Business and Management Studies Polt 1-12, Harvade Close, Off Obada Road Abeokuta Ogun StateOluwaseun TosinNo ratings yet
- Guppy Brain Atlas SmallerDocument4 pagesGuppy Brain Atlas Smallerapi-394354061No ratings yet
- Introduction To Immunology, Lecture# 4 (Dr. Adeela Naureen)Document6 pagesIntroduction To Immunology, Lecture# 4 (Dr. Adeela Naureen)arissa noorNo ratings yet
- Intermediate Iridology Course TranscriptionDocument52 pagesIntermediate Iridology Course TranscriptionNireesh Gopalakrishnan100% (1)
- Laporan Kasus SMF/ Bagian Ilmu Bedah (Short Case 1)Document59 pagesLaporan Kasus SMF/ Bagian Ilmu Bedah (Short Case 1)Roby Aditya SuryaNo ratings yet
- Body Defence MechanismsDocument11 pagesBody Defence MechanismsJoyce TaiNo ratings yet
- Braak Et Al. - 2004 - Stages in The Development of Parkinson's Disease-Related PathologyDocument14 pagesBraak Et Al. - 2004 - Stages in The Development of Parkinson's Disease-Related PathologyAleja ToPaNo ratings yet
- BREAST - CARE FinalDocument5 pagesBREAST - CARE FinalSandhya GuptaNo ratings yet
- Xenotransplantation - An Option For Organ Transplants?Document1 pageXenotransplantation - An Option For Organ Transplants?udadNo ratings yet
- Thyrotoxicosis: Giridhar MF 9 TermDocument19 pagesThyrotoxicosis: Giridhar MF 9 TermGiridhar MFNo ratings yet
- Sistem RespirasiDocument1 pageSistem RespirasisyfaassyakwaNo ratings yet
- Endocrine System Anatomy and Physiology - NurseslabsDocument29 pagesEndocrine System Anatomy and Physiology - NurseslabsAlyssum Marie50% (2)
- Clinical EnzymologyDocument23 pagesClinical EnzymologyKishore KaranNo ratings yet
- Digestive Sysytem: Basic Health CareDocument50 pagesDigestive Sysytem: Basic Health CareBecky GalanoNo ratings yet
- Science10 q3 Mod2 Week2 Menstrual-Cycle-Version-3Document24 pagesScience10 q3 Mod2 Week2 Menstrual-Cycle-Version-3nadia doropanNo ratings yet
LFTS - Types of Jaundice
LFTS - Types of Jaundice
Uploaded by
Sumaira Junaid0 ratings0% found this document useful (0 votes)
49 views21 pagesThis document discusses various liver function tests (LFTs) and what they indicate about liver health and function. It explains that LFTs measure blood components like bilirubin, aminotransferases, alkaline phosphatase, albumin, GGT, and PT/INR to provide insight into liver damage, metabolism, and excretory function. Specific LFT abnormalities can suggest pre-hepatic, hepatic, or post-hepatic etiologies and whether the liver is experiencing damage, obstruction, or other issues. Chronic conditions like hepatitis or cirrhosis can also impact LFT results over time.
Original Description:
Liver function tests
Original Title
LFTS- TYPES OF JAUNDICE
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses various liver function tests (LFTs) and what they indicate about liver health and function. It explains that LFTs measure blood components like bilirubin, aminotransferases, alkaline phosphatase, albumin, GGT, and PT/INR to provide insight into liver damage, metabolism, and excretory function. Specific LFT abnormalities can suggest pre-hepatic, hepatic, or post-hepatic etiologies and whether the liver is experiencing damage, obstruction, or other issues. Chronic conditions like hepatitis or cirrhosis can also impact LFT results over time.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
49 views21 pagesLFTS - Types of Jaundice
LFTS - Types of Jaundice
Uploaded by
Sumaira JunaidThis document discusses various liver function tests (LFTs) and what they indicate about liver health and function. It explains that LFTs measure blood components like bilirubin, aminotransferases, alkaline phosphatase, albumin, GGT, and PT/INR to provide insight into liver damage, metabolism, and excretory function. Specific LFT abnormalities can suggest pre-hepatic, hepatic, or post-hepatic etiologies and whether the liver is experiencing damage, obstruction, or other issues. Chronic conditions like hepatitis or cirrhosis can also impact LFT results over time.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 21
Zoobia Zaheeruddin
Plays a major role in protein, CHO and Lipid metabolism
Metabolize, detoxify and excrete
Excretion of digestive aids (bile acids)
Why?
LFTs are measurements of blood components
which simply provide a lead to existence, the
extent and type of liver damage
Bilirubin – total and direct
Aminotransferases – ALT(SGPT) and AST(SGOT)
Alkaline Phosphatase
SERUM – RED TOP
Serum Albumin
GGT
PT
INVESTIGATION:
• Test for excretory function/ cholestasis:
• Total bilirubin, direct bilirubin
• Test for liver damage/ parenchymal injury:
•AST, ALT
• Synthetic Function:
•Total protein, Albumin
•Test for Obstruction:
•γGT, ALP
Pre-hepatic – Hemolysis -IB INCREASED
- Prematurity
- ALT/AST INCREASED
Hepatic
(acute hepatocellular damage)
Post-hepatic -DB INCREASED
(cholestasis, - ALP
- GGT
obstruction to bile flow)
Cholestasis is any condition in which the flow of bile from the liver
is blocked.
CHRONIC LIVER DISEASE – ALBUMIN DECREASES
Results from excess production of bilirubin
(beyond the livers ability to conjugate it)
following hemolysis
High plasma concentrations of unconjugated
bilirubin
Impaired uptake, conjugation, or secretion of
bilirubin
Reflects a generalized liver (hepatocyte)
dysfunction
In this case, hyperbilirubinemia is usually
accompanied by other abnormalities in
biochemical markers of liver function
Caused by an obstruction of the biliary tree
Plasma bilirubin is conjugated, and other biliary
metabolites, such as bile acids accumulate in
the plasma
Characterized by pale colored stools (absence
of fecal bilirubin), and dark urine (increased
conjugated bilirubin)
Total
Direct ( conjugated )
Indirect ( unconjugated )
N/V: TB: 0.0-1.0 mg/dl
DB: 0.0-0.3 mg/dl
Benign liver disorder
½ of the affected individuals inherited it
Characterized by mild, fluctuating increases in
unconjugated bilirubin caused by decreased
ability of the liver to conjugate bilirubin
Onset of symptoms in teens, early 20’s or 30’s
Characterized by a complete absence or marked
reduction in bilirubin conjugation
Present with a severe unconjugated
hyperbilirubinemia that usually presents at birth
Condition is fatal when the enzyme is
completely absent
Characterized by impaired biliary secretion of
conjugated bilirubin
Present with a conjugated hyperbilirubinemia that is
usually mild
ALT / AST
Sensitive, acute damage to hapatocytes
Causes:
- Hepatitis
- Toxic injury
- Drug overdose
- Severe hypoxia
- Acute cardiac failure
N.V: ALT upto 31 U/L
AST in M upto 37 U/L , In F: upto31 U/L
Sources: - Bone (enzyme rich osteoblasts)
- Liver
Placenta – 3rd trimester
- Small Intestine
Kidney
Increase in ALP activity in liver disease due to extra
hepatic function of bile flow, usually in response to
cholestasis –> both intra and extra-hepatic
Also in Cirrhosis (b/c of obstruction)
N.V: Child: 117-390 U/L
Adult: 39-117 U/L
Microsomal enzyme, widely distributed in liver and
renal tubule
Activity increases in cholestasis
Very sensitive index of liver pathology
Induced by: ethanol, phenobarbitone, phenytoin
(even in the absence of recognizable liver disease)
Acute hepatic damage: changes in GGT activity
parallel those of aminotransferases
Pregnancy: GGT is inhibited by gestational
hormones so that it tends to remain normal despite
the presence of hepatic disease
N/V: In M: 11-50 U/L, In F: 5-50 U/L
Hepatic synthetic function
Albumin – major protein product of liver
Long biological half life in plasma, therefore,
significant falls in albumin concentration are slow to
occur if synthesis is suddenly reduced
Hypoalbuminemia is a feature of advanced chronic
liver disease
Can also occur in severe acute liver damage
N/V: TP: 6.6-8.7 gm/dl
Albumin: 3.8-4.4 gm/dl
Globulin: 1.9-2.8 gm/dl
You might also like
- Pathophysiology LeptospirosisDocument1 pagePathophysiology Leptospirosisjeoffrey_castro100% (3)
- Differential Diagnosis of JaundiceDocument4 pagesDifferential Diagnosis of JaundiceVirag PatilNo ratings yet
- Organ Function Test: Assessment of Functions of The OrgansDocument39 pagesOrgan Function Test: Assessment of Functions of The OrgansSri Abinash MishraNo ratings yet
- Liver FunctionDocument90 pagesLiver Functionapi-19641337100% (1)
- Liver Function Test: Liver Hilang Bagian Masih Bisa KompensasiDocument53 pagesLiver Function Test: Liver Hilang Bagian Masih Bisa KompensasiKharisulNo ratings yet
- Liver MarkersDocument4 pagesLiver MarkerslucaNo ratings yet
- Liver PathologyDocument35 pagesLiver Pathologynhgwdwffp2No ratings yet
- 15 Coned CCRN GastrointestinalDocument21 pages15 Coned CCRN GastrointestinalAkbar TaufikNo ratings yet
- 1.1 Liver Function Tests 15.02.19Document39 pages1.1 Liver Function Tests 15.02.19Syed ArefinNo ratings yet
- Liver Function Test: Maimun ZA Lab Patologi Klinik Fkub-RssaDocument26 pagesLiver Function Test: Maimun ZA Lab Patologi Klinik Fkub-RssaSaifuddin BadarsyahNo ratings yet
- LFTSDocument34 pagesLFTSJoseline AliceNo ratings yet
- Liver DiseasesDocument24 pagesLiver DiseasesAbdo HaiderNo ratings yet
- Liver Panel: EM 6203 Dr. K. AikenheadDocument24 pagesLiver Panel: EM 6203 Dr. K. AikenheadCrystal Lynn Keener SciariniNo ratings yet
- A Case Oriented Approach To Liver Laboratory Profiling in Dogs and CatsDocument5 pagesA Case Oriented Approach To Liver Laboratory Profiling in Dogs and CatsAbelantonNo ratings yet
- Total Protein Albumin + Globulins (Ig, Complements, Fibrinogen, A1-Antrypsin Etc)Document4 pagesTotal Protein Albumin + Globulins (Ig, Complements, Fibrinogen, A1-Antrypsin Etc)bryan chan100% (1)
- Liver Function TesDocument58 pagesLiver Function TesnoffrizalNo ratings yet
- Molecular BiologyDocument17 pagesMolecular BiologyMzwandile NyawoseNo ratings yet
- Which of The Two Is More Liver Specific and Increases More During Liver DiseaseDocument8 pagesWhich of The Two Is More Liver Specific and Increases More During Liver DiseaseMariel AbatayoNo ratings yet
- Liver Function TestDocument25 pagesLiver Function Testnuradinman89No ratings yet
- Liver Function Tests InterpretationDocument2 pagesLiver Function Tests InterpretationdarrenkongNo ratings yet
- Liver Function Tests PDFDocument6 pagesLiver Function Tests PDFSubhash Digambar VisalNo ratings yet
- 07 Liver Tunction TestsDocument41 pages07 Liver Tunction TestsPaulina PaskeviciuteNo ratings yet
- Liver Function TestsDocument17 pagesLiver Function TestsHung Lam100% (1)
- JAUNDICE Internal Medicine PresentationDocument34 pagesJAUNDICE Internal Medicine PresentationNano BaddourNo ratings yet
- Liver Function Tests (Sem)Document6 pagesLiver Function Tests (Sem)Francisco NiegasNo ratings yet
- Pemeriksaan Fungsi Hati, DR - DiahDocument42 pagesPemeriksaan Fungsi Hati, DR - DiahYuliana LatifNo ratings yet
- Approach To A Patient With JaundiceDocument33 pagesApproach To A Patient With JaundiceRahul Kumar VermaNo ratings yet
- Enzymes Liver Pancreas FCDocument10 pagesEnzymes Liver Pancreas FCLois Lipanovich100% (1)
- Professor Dr. Najat A. HasanDocument40 pagesProfessor Dr. Najat A. HasanPeter MungaiNo ratings yet
- Liver Function Test 2011Document26 pagesLiver Function Test 2011anisa rachmitaNo ratings yet
- Pathophysiology of Laboratory Abnormalities in Liver DisordersDocument55 pagesPathophysiology of Laboratory Abnormalities in Liver DisordersYudha fedrian AKNo ratings yet
- Lect. 8Document30 pagesLect. 8jayNo ratings yet
- Hepatobiliary Diseases 3Document28 pagesHepatobiliary Diseases 3AmirahNo ratings yet
- Liver Function Test by Alaa Abass PMDocument48 pagesLiver Function Test by Alaa Abass PMalaamabass93No ratings yet
- Liver Function Tests: Dr. ThomasDocument32 pagesLiver Function Tests: Dr. ThomasthomaskodiatteNo ratings yet
- Chem-Dr - Zainab-Bilirubin-Lab 2Document10 pagesChem-Dr - Zainab-Bilirubin-Lab 2gmpcbpzdysNo ratings yet
- 5 - JaundiceDocument16 pages5 - JaundiceHamzehNo ratings yet
- Obstructive Jaundice Group 6Document33 pagesObstructive Jaundice Group 6Qurbon AliNo ratings yet
- Hepatic Function TestsDocument12 pagesHepatic Function TestsalhassanmohamedNo ratings yet
- Liver Function Tests (LFTS) : Group TwoDocument12 pagesLiver Function Tests (LFTS) : Group TwoStanley KarugaNo ratings yet
- Liver Function TestsDocument48 pagesLiver Function TestsAli H. Sadiek أ.د. علي حسن صديق92% (13)
- Fisio 9Document9 pagesFisio 9anaNo ratings yet
- Organ Function TestDocument49 pagesOrgan Function TestmekuriawNo ratings yet
- Pemeriksaan Fungsi Hati .: Prof. Dr. Adi Koesoema Aman SPPK (KH)Document51 pagesPemeriksaan Fungsi Hati .: Prof. Dr. Adi Koesoema Aman SPPK (KH)kiki rawitriNo ratings yet
- Urea/ Ammonia Tests: Primary Liver Function TestsDocument6 pagesUrea/ Ammonia Tests: Primary Liver Function TestsMemory MahwendaNo ratings yet
- Liver (Hati) ZLDocument27 pagesLiver (Hati) ZLpafaniNo ratings yet
- Unit 8 - LIVER FUNCTION TESTSDocument93 pagesUnit 8 - LIVER FUNCTION TESTSRezan ThapaNo ratings yet
- Jaundice: Accumulation of Yellow Pigment in The Skin and Other Tissues (Bilirubin)Document65 pagesJaundice: Accumulation of Yellow Pigment in The Skin and Other Tissues (Bilirubin)qreenNo ratings yet
- Test LFTsDocument2 pagesTest LFTsostarburstoNo ratings yet
- Viral Hepatitis Diagnostic Test and Differential DiagnosisDocument21 pagesViral Hepatitis Diagnostic Test and Differential DiagnosisNedeln AudleyNo ratings yet
- Biochemistry - LG 1 (Liver Function Tests) - Dr. SalarDocument28 pagesBiochemistry - LG 1 (Liver Function Tests) - Dr. Salargabi.g.wahbeNo ratings yet
- Lucture 11functions of LiverDocument3 pagesLucture 11functions of Livermohammed jemalNo ratings yet
- Liver Function Tests: Shivansh Agarwal - 200201474Document16 pagesLiver Function Tests: Shivansh Agarwal - 200201474Shivansh AgarwalNo ratings yet
- Health Liver Interpretation and InterventionsDocument11 pagesHealth Liver Interpretation and InterventionsParas BansalNo ratings yet
- Approach To Jaundice (1) .PPT ALAWAJIDocument28 pagesApproach To Jaundice (1) .PPT ALAWAJIayuNo ratings yet
- Approach To The Patient With Abnormal Liver Tests: Alvaro Koch, M.DDocument47 pagesApproach To The Patient With Abnormal Liver Tests: Alvaro Koch, M.DTimotius Kevin NatanaelNo ratings yet
- Liver Function Tests: Presented By-Dr. Arshiya Kaura (JR 1)Document50 pagesLiver Function Tests: Presented By-Dr. Arshiya Kaura (JR 1)vikasNo ratings yet
- Liver - Lecture 1 by Dr. Rehma Dar (14-03-2020)Document16 pagesLiver - Lecture 1 by Dr. Rehma Dar (14-03-2020)khadhiNo ratings yet
- Liver Function Test: DescriptionDocument3 pagesLiver Function Test: DescriptionOkura JoshuaNo ratings yet
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo ratings yet
- Indira National School: I. Give Reason For The FollowingDocument3 pagesIndira National School: I. Give Reason For The FollowingUPANSH SETHNo ratings yet
- Histology of The Respiratory System 20152016Document44 pagesHistology of The Respiratory System 20152016mugilanNo ratings yet
- Renal PhysiologyDocument193 pagesRenal Physiologyramadan100% (1)
- Medical Student Career Paths BookDocument124 pagesMedical Student Career Paths BookMindi WindmillNo ratings yet
- ReflexologyDocument4 pagesReflexologyphong duongNo ratings yet
- BIO270 Tuto 5Document3 pagesBIO270 Tuto 5Mirza KarmilaNo ratings yet
- Nervous System Grade 9 ??Document53 pagesNervous System Grade 9 ??Alia LauderNo ratings yet
- BSC 100 Midterm Questions For Oral ExamDocument20 pagesBSC 100 Midterm Questions For Oral ExamNovochino CastilloNo ratings yet
- Brain AnatomyDocument71 pagesBrain Anatomyhimani bansalNo ratings yet
- Chapter 9 - Endocrine SystemDocument9 pagesChapter 9 - Endocrine SystemrishellemaepilonesNo ratings yet
- Functions of Each Part of The Intergumentary System.1Document61 pagesFunctions of Each Part of The Intergumentary System.1Jane Ilagan VizcoNo ratings yet
- OralcholecystographyDocument13 pagesOralcholecystographySuman PokhrelNo ratings yet
- AbnormalL Liver Function Test 2012Document59 pagesAbnormalL Liver Function Test 2012Nayan MaharjanNo ratings yet
- SBI4U Unit 4 Homeostasis Excretory SystemDocument27 pagesSBI4U Unit 4 Homeostasis Excretory System전채연No ratings yet
- Harvade College of Science, Business and Management Studies Polt 1-12, Harvade Close, Off Obada Road Abeokuta Ogun StateDocument21 pagesHarvade College of Science, Business and Management Studies Polt 1-12, Harvade Close, Off Obada Road Abeokuta Ogun StateOluwaseun TosinNo ratings yet
- Guppy Brain Atlas SmallerDocument4 pagesGuppy Brain Atlas Smallerapi-394354061No ratings yet
- Introduction To Immunology, Lecture# 4 (Dr. Adeela Naureen)Document6 pagesIntroduction To Immunology, Lecture# 4 (Dr. Adeela Naureen)arissa noorNo ratings yet
- Intermediate Iridology Course TranscriptionDocument52 pagesIntermediate Iridology Course TranscriptionNireesh Gopalakrishnan100% (1)
- Laporan Kasus SMF/ Bagian Ilmu Bedah (Short Case 1)Document59 pagesLaporan Kasus SMF/ Bagian Ilmu Bedah (Short Case 1)Roby Aditya SuryaNo ratings yet
- Body Defence MechanismsDocument11 pagesBody Defence MechanismsJoyce TaiNo ratings yet
- Braak Et Al. - 2004 - Stages in The Development of Parkinson's Disease-Related PathologyDocument14 pagesBraak Et Al. - 2004 - Stages in The Development of Parkinson's Disease-Related PathologyAleja ToPaNo ratings yet
- BREAST - CARE FinalDocument5 pagesBREAST - CARE FinalSandhya GuptaNo ratings yet
- Xenotransplantation - An Option For Organ Transplants?Document1 pageXenotransplantation - An Option For Organ Transplants?udadNo ratings yet
- Thyrotoxicosis: Giridhar MF 9 TermDocument19 pagesThyrotoxicosis: Giridhar MF 9 TermGiridhar MFNo ratings yet
- Sistem RespirasiDocument1 pageSistem RespirasisyfaassyakwaNo ratings yet
- Endocrine System Anatomy and Physiology - NurseslabsDocument29 pagesEndocrine System Anatomy and Physiology - NurseslabsAlyssum Marie50% (2)
- Clinical EnzymologyDocument23 pagesClinical EnzymologyKishore KaranNo ratings yet
- Digestive Sysytem: Basic Health CareDocument50 pagesDigestive Sysytem: Basic Health CareBecky GalanoNo ratings yet
- Science10 q3 Mod2 Week2 Menstrual-Cycle-Version-3Document24 pagesScience10 q3 Mod2 Week2 Menstrual-Cycle-Version-3nadia doropanNo ratings yet