Professional Documents
Culture Documents
Inflammation and Healing (Revised/Reviewed)
Inflammation and Healing (Revised/Reviewed)
Uploaded by
Maria Margarita0 ratings0% found this document useful (0 votes)
46 views35 pagesOriginal Title
Chapter_005.Inflammation and Healing(2)
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
46 views35 pagesInflammation and Healing (Revised/Reviewed)
Inflammation and Healing (Revised/Reviewed)
Uploaded by
Maria MargaritaCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 35
Chapter 5
Inflammation and Healing
(Revised/Reviewed)
Review of Body Defenses
First line of defense (block entry of bacteria)
Nonspecific
Mechanical barrier
Unbroken skin and mucous membranes
Secretions such as tears and gastric juices
(enzymes and chemicals) inactivate/destroy
Second line of defense
Nonspecific processes
Phagocytosis (destruction of pathogens) –engulf
and destroy
Inflammation – sequence of events – limit impact
of injury
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •2
Review of Body Defenses
(Cont.)
Third line of defense
Specific defense
Production of specific antibodies or cell-mediated
immunity
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •3
Defense Mechanisms in the Body
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •4
Physiology of Inflammation
Inflammatory response
A protective defense mechanism and important basic
concept in pathophysiology
Disorders are named using the ending –itis.
Allergic reaction, insect bite
Signs and symptoms serve as warning for a
problem:
Problem may be hidden within the body.
It is not the same as infection. (no microbe)
Infection, however, is one cause of inflammation.
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •5
Causes of Inflammation
Direct physical damage –
cut, sprain
Caustic chemicals - acid, drain cleaner
Ischemia or infarction
Allergic reactions
Extremes of heat or cold
Foreign bodies - splinter, glass
Infection
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •6
Definition/Steps of Inflammation
INJURY (capillaries and tissue cells)
Release of bradykinin from injured cells
(stimulates pain receptors)
Pain causes release of histamine.
Bradykinin and histamine cause
capillary dilation.
Break in skin allows bacteria to enter tissue
Neutrophils phagocytize bacteria.
Macrophages (mature monocytes) leave the
bloodstream and phagocytose microbes.
Bradykinin – peptide that helps control inflammation
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •7
Acute Inflammation
Process of inflammation is the same, regardless of cause.
Timing varies with specific cause (immediate or delayed) –
sunburn (delayed)
Chemical mediators (released) affect blood
vessels and nerves in the damaged area:
Vasodilation
Hyperemia (excess of blood in the vessels)
Increase in capillary permeability
Leukocytes are attracted by chemotaxis
Chemotaxis – damaged cells release chemicals
Diapedesis – cells destroy foreign material, cell
debris (phagocytosis)
Chemotaxis – movement of a motile cell
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •8
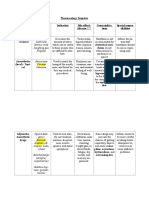
Chemical Mediators in the
Inflammatory Response
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •9
Local Effects of Inflammation
Redness and warmth
Caused by increased blood flow to damaged area
Swelling (edema)
Shift of protein and fluid into the interstitial space
Pain
Increased pressure of fluid on nerves; release of chemical
mediators (e.g., bradykinins)
Loss of function
May develop if cells lack nutrients; edema may interfere with
movement.
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •10
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •11
Exudate
Serous
Watery, consists primarily of fluid, some proteins, and white blood
cells
Fibrinous
Thick, sticky, high cell and fibrin content
Purulent
Thick, yellow-green, contains more leukocytes, cell debris, and
microorganisms (bacterial infection) “pus”
Abscess – pocket of purulent/pus in solid tissue
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •12
Systemic Effects of Inflammation
Mild fever (pyrexia)
Common if inflammation
is extensive
Release of pyrogens-
fever producing
substances
Impact of high fever
destroys pathogens
Malaise
Feeling unwell
Fatigue
Headache
Anorexia
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •13
Changes in the Blood
with Inflammation
Increased WBC –
leukocytosis
Differential count –
(neutrophils, lymphocytes,
eosinophils, monocytes, basophils)
Elevated Serum C-
reactive protein
Elevated erythrocyte
sedimentation rate
(ESR)
Helps identify viral from
bacterial etiology
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •14
Potential Complications of
Inflammation
Local – inflammation in lungs – reduce expansion,
decrease oxygen diffusion – joints – decreased ROM
Infection
Microorganisms can more easily penetrate
edematous tissues. (damaged tissue)
Some microbes resist phagocytosis.
The inflammatory exudate also provides an
excellent medium for microorganisms.
Skeletal muscle spasm
May be initiated by inflammation
Protective response to pain
Bones/joints out of normal alignment
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •15
Chronic Inflammation
Follows acute episode of inflammation
Less swelling and exudate
Presence of more lymphocytes,
macrophages, and fibroblasts
Continued tissue destruction
More fibrous scar tissue
Granuloma may develop around foreign
object (small mass of cells with a necrotic center)
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •16
Potential Complications
Deep ulcers may result from severe or
prolonged inflammation
Caused by cell necrosis and lack of cell
regeneration that causes erosion of the tissue
• Can lead to complications such as perforation of viscera
• Extensive scar tissue formation
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •17
Treatment of Inflammation
Acetylsalicylic acid (ASA)
Aspirin (pain, inflammation, fever – irritation of GI, bleeding and ulcers)
Acetaminophen
Tylenol (fever, pain, not inflammation)
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Ibuprofen (inflammation, pain, fever – celecoxib (celebrex)
Glucocorticoids
Corticosteroids (anti inflammatory)
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •18
Anti-Inflammatory Effects of
Glucocorticoids (short term)
Decreased capillary permeability (stabilize
vascular system)
Reduced number of leukocytes and mast
cells
Reduces immune response
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •19
Adverse Effects of
Glucocorticoids (long term, high dose)
Atrophy of lymphoid tissue; reduced hemopoiesis
Increased risk of infection
Catabolic effects
Increased tissue breakdown; decreased protein
synthesis
Delayed healing
Delayed growth in children
Retention of sodium and water because of
aldosterone-like affect in the kidney (HTN,
edema) HTN and edema
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •20
“RICE” Therapy for Injuries (first aid)
Rest
Ice
Compression - stockings
Elevation - improve blood flow
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •21
Types of Healing
Resolution
Minimal tissue damage – return to normal short
period (sun burn)
Regeneration
Damaged tissue replaced with cells that are
functional (mitosis) – replicate (not all cells can do
this) – heart, liver
Replacement
Functional tissue replaced by scar tissue (fibrous)
Loss of function
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •22
The Healing Process
Healing of incised wound by first intention
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •23
The Healing Process (Cont.)
Healing by second intention
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •24
Scar Formation
Loss of function
Result of loss of normal cells and specialized
structures – lack of
• Hair follicles
• Nerves
• Receptors
Contractures and obstructions
Scar tissue is nonelastic. Shrinks over time
Can restrict range of movement
Adhesions
Bands of scar tissue joining two surfaces that are
normally separated (intestine) – distort and twist
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •25
Scar Formation
Hypertrophic scar tissue
Overgrowth of fibrous tissue
• Leads to hard ridges of scar tissue or
keloid formation
Ulceration
Blood supply may be impaired around
scar
• Results in further tissue breakdown
and ulceration at future time
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •26
Burns
Thermal—caused by flames or hot fluids
Chemical
Radiation
Electricity
Light
Friction
Cause an acute inflammatory response
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •27
Classification of Burns
Superficial partial-
thickness (first-degree)
burns
Involve epidermis and part
of dermis
Little, if any, blister
formation (sun burn, scald)
Deep partial-thickness
(second-degree) burns
Epidermis and part of
dermis
Blister formation – red and
edematous, pain
Become infected, scars
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •28
Full-thickness (third- and
fourth-degree) burns
Destruction of all skin
layers and often
underlying tissues
Charring – hard and dry
on the surface
Shrinking and tightening =
pressure
Treatment – escharotomy
– cutting through the crust
– relieve pressure and
allow circulation
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •29
Classification of Burn Injury
by Depth
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •30
Effects of Burn Injury
local and systemic Respiratory problems:
Dehydration and edema inhalation of toxic
no bleeding fumes
Shock (massive fluid Need high levels of
shift into tissues = oxygen
edema)
Damage to mucosal
Decreased circulating lining of trachea and
bronchi
blood volume – low Inflammation –
BP, hypovolemic obstruction
shock Wheezing, coughing
Sputum – black
Pneumonia
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •31
Continued
Very painful throughout Infection – microbes in
treatment process hair follicles and in
Body movements, tissues
grafts
Staphylococcus
Pain medications are aureus
Drug resistance
required Culture necessary for
treatment
Need for increased
dietary protein and
carbohydrates
Feel chilled
Anemia
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •32
Assessment of Burn Area Using
the Rule of Nines
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •33
Healing of Burns
Immediate covering of a clean wound is
needed to prevent infection.
Healing is a prolonged process.
Scar tissue develops, even with skin grafting.
Physiotherapy and occupational therapy may
be necessary.
Surgery may be necessary to release
restrictive scar tissue.
Biosynthetic skin substitutes – severe burns
May have living human cells
Strong and elastic - rapid healing
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •34
References
Vanmeter, K & Hubert, R (2014) Gould’s
Pathophysiology for the Health professions
(5th Ed) Elsevier
•Copyright © 2014, 2011, 2006 by Saunders, an imprint of Elsevier, Inc. •35
You might also like
- Gold Standard For NclexDocument113 pagesGold Standard For NclexMaria Margarita87% (30)
- Special Operations Forces Medical HandbookFrom EverandSpecial Operations Forces Medical HandbookRating: 4.5 out of 5 stars4.5/5 (2)
- U1L05 Activity Guide - Inputs and OutputsDocument4 pagesU1L05 Activity Guide - Inputs and OutputsGladis Stella Osorio GutierrezNo ratings yet
- Installation Method Statement (Scaffoldless)Document10 pagesInstallation Method Statement (Scaffoldless)faizbukhari100% (1)
- Mapiful - How To Make Your Home More YouDocument35 pagesMapiful - How To Make Your Home More YouElina100% (1)
- PHL 4201: Body Fluids & Blood: DR K.G. Ibrahim (Aka DR Ghandi)Document34 pagesPHL 4201: Body Fluids & Blood: DR K.G. Ibrahim (Aka DR Ghandi)SA WakiliNo ratings yet
- Chapter 34 - HemaDocument32 pagesChapter 34 - HemaNicole Amado CabahugNo ratings yet
- Exudate Management (Maserasi Dan HypergranulasiDocument48 pagesExudate Management (Maserasi Dan HypergranulasiEza R. KusumaNo ratings yet
- Innate Immunity Inflammation and Wound HealingDocument55 pagesInnate Immunity Inflammation and Wound HealingFrank AroniNo ratings yet
- InflammationDefinition, Symptoms, Treatment,&FactsBritannica 1710882912933Document6 pagesInflammationDefinition, Symptoms, Treatment,&FactsBritannica 1710882912933muhellen8No ratings yet
- Inflammation and Repair: 1 Elsevier Items and Derived Items © 2009 by Saunders, An Imprint of Elsevier IncDocument145 pagesInflammation and Repair: 1 Elsevier Items and Derived Items © 2009 by Saunders, An Imprint of Elsevier IncaqeelNo ratings yet
- Rheumatoid ArthritisDocument65 pagesRheumatoid ArthritisSiti AminahNo ratings yet
- Why Wounds Fail To HealDocument6 pagesWhy Wounds Fail To HealMsPocketbook HoarderNo ratings yet
- Clinical Features of Gingivitis & Gingival Inflammation: Pathogenesis.Document9 pagesClinical Features of Gingivitis & Gingival Inflammation: Pathogenesis.Prince AhmedNo ratings yet
- Aureus. It Can Be Either Acute or ChronicDocument7 pagesAureus. It Can Be Either Acute or ChronicfortunelobsterNo ratings yet
- Digestive System DisordersDocument58 pagesDigestive System Disorderskiemdinhit7No ratings yet
- Week 1. Introduction, Injury, Necrosis, Apoptosis - July 11, 2018 PDFDocument41 pagesWeek 1. Introduction, Injury, Necrosis, Apoptosis - July 11, 2018 PDFVincentNo ratings yet
- Physiology of Bone: Dr. Ross G. Cooper Senior Lecturer Division of Physiology School of Health & Policy StudiesDocument70 pagesPhysiology of Bone: Dr. Ross G. Cooper Senior Lecturer Division of Physiology School of Health & Policy StudiesnannaraNo ratings yet
- Acute Inflammation DrgayanaMDocument36 pagesAcute Inflammation DrgayanaMhenriettaobi128No ratings yet
- Inflammation 30.08.2022Document39 pagesInflammation 30.08.2022Abdur RaquibNo ratings yet
- 10.1 Lines of DefenseDocument17 pages10.1 Lines of DefenseMarites LammaoNo ratings yet
- Chapter 14: Inflammation, Tissue Repair, and Wound HealingDocument5 pagesChapter 14: Inflammation, Tissue Repair, and Wound Healingbdelvalle3100% (1)
- Power Point Week #4Document191 pagesPower Point Week #4Raelene MarceauNo ratings yet
- CHAPTER 5 InflammationDocument51 pagesCHAPTER 5 Inflammationyeshita yonasNo ratings yet
- Altered Cellular & Tissue Biology 2020Document24 pagesAltered Cellular & Tissue Biology 2020farzanamphNo ratings yet
- OsteomyelitisDocument26 pagesOsteomyelitisCxarina RamirezNo ratings yet
- The Immune System: Care of Clients With Altered ImmunityDocument87 pagesThe Immune System: Care of Clients With Altered ImmunityHanni Dayang PuspitasariNo ratings yet
- Pathology InflammationDocument111 pagesPathology InflammationAlyssa ArroyoNo ratings yet
- Acute Inflammation: DR - Djumadi Achmad, Sppa (K)Document46 pagesAcute Inflammation: DR - Djumadi Achmad, Sppa (K)Elearning FK UnhasNo ratings yet
- Lecture 3Document56 pagesLecture 3w2tz2qrqxdNo ratings yet
- Bed Sore (Pressure Ulcers)Document28 pagesBed Sore (Pressure Ulcers)Alma Susan100% (1)
- Osteomyelitis 130708212636 Phpapp01Document107 pagesOsteomyelitis 130708212636 Phpapp01merikasorNo ratings yet
- Osteomyelitis: ClassificationDocument5 pagesOsteomyelitis: Classificationthanuja mathewNo ratings yet
- Inflammation NotesDocument47 pagesInflammation Notespuji100% (2)
- Osteomyelitis 000Document43 pagesOsteomyelitis 000nurendah90No ratings yet
- CH17Document22 pagesCH17JoshMatthewsNo ratings yet
- Cell and Tissue InjuryDocument60 pagesCell and Tissue InjurydesiNo ratings yet
- Week 3Document107 pagesWeek 3wieka mawieNo ratings yet
- Inflammation For BDS StudentsDocument24 pagesInflammation For BDS StudentsMohan Prasad GuptaNo ratings yet
- L 3 Pathophysiology - 3Document37 pagesL 3 Pathophysiology - 3Fatimah FaqihiNo ratings yet
- Inflammation NotesDocument12 pagesInflammation NotesavidadarkestevillearnNo ratings yet
- Cell Injury Notes-1Document63 pagesCell Injury Notes-1Stefanie VirniaNo ratings yet
- Alterations in Body DefenseDocument45 pagesAlterations in Body DefenseAlfred NjeruNo ratings yet
- Hema Kini BASIC INFLAMMATION RECAP 2022Document49 pagesHema Kini BASIC INFLAMMATION RECAP 2022Shana ShirinNo ratings yet
- Compliment-Mediated Immune Responses: Response EffectsDocument12 pagesCompliment-Mediated Immune Responses: Response EffectsbiancameeNo ratings yet
- 5 Inflammation-1Document102 pages5 Inflammation-1Adil MusaddiqNo ratings yet
- 8 Gram Positive CocciDocument37 pages8 Gram Positive CocciSaleh AzizNo ratings yet
- Exp - No.5 Acute InflamationDocument22 pagesExp - No.5 Acute InflamationNatasha BalochNo ratings yet
- Fundamentals of Wound Management 2014Document37 pagesFundamentals of Wound Management 2014anjelopaul2017No ratings yet
- Osteomyelitis Report Orthopedic NursingDocument15 pagesOsteomyelitis Report Orthopedic NursingSienaNo ratings yet
- Leg Ulcers: Dr. RaghunandanDocument53 pagesLeg Ulcers: Dr. RaghunandansorinmoroNo ratings yet
- Inflamation: Drh. M. Arfan Lesmana, M.Sc. Fakultas Kedokteran Hewan, Universitas Brawijaya EmailDocument55 pagesInflamation: Drh. M. Arfan Lesmana, M.Sc. Fakultas Kedokteran Hewan, Universitas Brawijaya EmailalrezaNo ratings yet
- Biocompatibility: Biological Response Biocompatibility Tests Sterilization IssuesDocument41 pagesBiocompatibility: Biological Response Biocompatibility Tests Sterilization Issuesbagus3869No ratings yet
- InflammationDocument8 pagesInflammationGhazi Uddin AhmedNo ratings yet
- Clinical Signs of GingivitisDocument58 pagesClinical Signs of GingivitisNishtha BaralNo ratings yet
- Inflammation and Repair: Definition of Inflammation Acute Inflammation Vascular Events in InflammationDocument35 pagesInflammation and Repair: Definition of Inflammation Acute Inflammation Vascular Events in InflammationSoji AdimulaNo ratings yet
- 01.inflammation 1Document30 pages01.inflammation 1Shameena KnNo ratings yet
- Principles of Plastic Surgery ForDocument54 pagesPrinciples of Plastic Surgery ForStevysNo ratings yet
- 9th Seminar - Diseases of Pulp Part IIDocument54 pages9th Seminar - Diseases of Pulp Part IISriya Saatwika ReddyNo ratings yet
- Introduction, Cell & Tissue Damage: by Hermizan HalihanafiahDocument41 pagesIntroduction, Cell & Tissue Damage: by Hermizan HalihanafiahSebghat Ullah BalochNo ratings yet
- Group 7 - OsteomyelitisDocument35 pagesGroup 7 - Osteomyelitismercygreat2014No ratings yet
- Paper 2Document71 pagesPaper 2Edward AngimoyNo ratings yet
- Vascular Access and Infusion TherapyDocument47 pagesVascular Access and Infusion TherapyMaria Margarita100% (1)
- 2.4 165880-2011-League - of - Cities - of - The - Phils. - v. - Commission20180914-5466-UtnhegDocument27 pages2.4 165880-2011-League - of - Cities - of - The - Phils. - v. - Commission20180914-5466-UtnhegBiancaDiwaraNo ratings yet
- Urinary Elimination and CatheterizationDocument41 pagesUrinary Elimination and CatheterizationMaria Margarita100% (1)
- Route/Dosage: Concentration: Not To Exceed 10 Mg/ml. Do NotDocument2 pagesRoute/Dosage: Concentration: Not To Exceed 10 Mg/ml. Do NotMaria MargaritaNo ratings yet
- Nursing From Conception To AdolescenceDocument24 pagesNursing From Conception To AdolescenceMaria MargaritaNo ratings yet
- CLIN 1330 Week 7 Complex Wound Care Spring 2018Document26 pagesCLIN 1330 Week 7 Complex Wound Care Spring 2018Maria MargaritaNo ratings yet
- Respiratory SystemDocument90 pagesRespiratory SystemMaria MargaritaNo ratings yet
- Pharmacology Template Classification Examples Indication Side Effects Adverse Contraindica-Tions Special Respon - SibilitiesDocument3 pagesPharmacology Template Classification Examples Indication Side Effects Adverse Contraindica-Tions Special Respon - SibilitiesMaria MargaritaNo ratings yet
- Solved AnswersDocument11 pagesSolved AnswersChandrilNo ratings yet
- PS-MM IntegrationDocument2 pagesPS-MM IntegrationmohammedraulmadridNo ratings yet
- Lesson PlanDocument2 pagesLesson PlanLUZ SELENE OLIVARES BONILLANo ratings yet
- Form 49 B (TAN)Document4 pagesForm 49 B (TAN)Mohan NaiduNo ratings yet
- Assessment-2: Sithind002 Source and Use Information On The Hospitality IndustryDocument19 pagesAssessment-2: Sithind002 Source and Use Information On The Hospitality IndustryNidhi GuptaNo ratings yet
- #SyallabusDocument33 pages#SyallabusSandeep B MNo ratings yet
- PHP Security CPanelDocument5 pagesPHP Security CPanelManiMegalaiNo ratings yet
- Metal Joining (Fasteners)Document11 pagesMetal Joining (Fasteners)ganeshNo ratings yet
- Manual Del Gemcom Surpac - Underground Ring DesignDocument43 pagesManual Del Gemcom Surpac - Underground Ring DesignDavid GarciaNo ratings yet
- © The Institute of Chartered Accountants of IndiaDocument154 pages© The Institute of Chartered Accountants of IndiaJattu TatiNo ratings yet
- MBA Global Management Technische Hochschule Ingolstadt - IngolstadtDocument7 pagesMBA Global Management Technische Hochschule Ingolstadt - IngolstadtHieu NguyenNo ratings yet
- 55 Selection of Appropriate Internal Process Challenge Devices PCDsDocument4 pages55 Selection of Appropriate Internal Process Challenge Devices PCDsRakeshNo ratings yet
- 17.0 DistillationDocument73 pages17.0 DistillationcheesewizzNo ratings yet
- Cash Flow TemplateDocument9 pagesCash Flow Templatealdi ruNo ratings yet
- Catalog - Tesys Essential Guide - 2012 - (En)Document54 pagesCatalog - Tesys Essential Guide - 2012 - (En)Anonymous FTBYfqkNo ratings yet
- Singles NumericDocument27 pagesSingles Numericestevaocanan85No ratings yet
- Gloss 1Document8 pagesGloss 1api-3723109No ratings yet
- BPO - Bank Payment ObligationDocument2 pagesBPO - Bank Payment ObligationshreyaNo ratings yet
- EMTECH DLP Week3Document5 pagesEMTECH DLP Week3Joanne GuevarraNo ratings yet
- Activity 3.module 1Document4 pagesActivity 3.module 1Juedy Lala PostreroNo ratings yet
- 460 Protective Clear Coat MSDS TDSDocument4 pages460 Protective Clear Coat MSDS TDSFrancesco VignaliNo ratings yet
- TedDocument93 pagesTedanvignesh18No ratings yet
- SHC English BulletinDocument1 pageSHC English BulletinMarcus Yee XiangNo ratings yet
- Executing / Implementing Agency: Financial Management Assessment Questionnaire Topic ResponseDocument6 pagesExecuting / Implementing Agency: Financial Management Assessment Questionnaire Topic ResponseBelle CartagenaNo ratings yet
- Epoxy Curing Agents and Modifiers: Ancamide® 260A Curing AgentDocument1 pageEpoxy Curing Agents and Modifiers: Ancamide® 260A Curing AgentNissim Hazar CasanovaNo ratings yet
- Math Solo Plan NewDocument15 pagesMath Solo Plan NewMicah David SmithNo ratings yet
- Almario, Rich L. - InvestmentDocument6 pagesAlmario, Rich L. - InvestmentRich Lopez AlmarioNo ratings yet