Professional Documents
Culture Documents
Genetic Counselling
Genetic Counselling
Uploaded by
div100%(3)100% found this document useful (3 votes)
126 views23 pagesGenetic counseling is a process of communicating information about genetic conditions to help individuals understand implications, cope, and make informed decisions. Genetic counselors provide risk assessments, educate about inheritance patterns and testing, and support patients emotionally. The goals are to promote informed choices, clarify options and prognosis, and help reduce incidence and impact of genetic disorders. Genetic counseling involves gathering family history, assessing risks, discussing available options, and providing long-term support.
Original Description:
Original Title
GENETIC COUNSELLING
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentGenetic counseling is a process of communicating information about genetic conditions to help individuals understand implications, cope, and make informed decisions. Genetic counselors provide risk assessments, educate about inheritance patterns and testing, and support patients emotionally. The goals are to promote informed choices, clarify options and prognosis, and help reduce incidence and impact of genetic disorders. Genetic counseling involves gathering family history, assessing risks, discussing available options, and providing long-term support.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
100%(3)100% found this document useful (3 votes)
126 views23 pagesGenetic Counselling
Genetic Counselling
Uploaded by
divGenetic counseling is a process of communicating information about genetic conditions to help individuals understand implications, cope, and make informed decisions. Genetic counselors provide risk assessments, educate about inheritance patterns and testing, and support patients emotionally. The goals are to promote informed choices, clarify options and prognosis, and help reduce incidence and impact of genetic disorders. Genetic counseling involves gathering family history, assessing risks, discussing available options, and providing long-term support.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 23
GENETIC COUNSELLING
DEFINITION
• Genetic counseling is a communication process
whereby an individual or family obtains information
about a genetic condition, is helped to understand the
implications and significance of the condition, and is
given resources to help with coping and management
• It is a continuous process involving lasting supportive
relationships between the family and the genetic
professional.
• Genetic counselors are master’s level–trained health-
care professionals who work closely with
pediatricians and pediatric subspecialists alike.
• Genetic counselors can be a source of information
about genetic conditions, risk assessment for disease,
and genetic testing.
• Although most of a genetic counselor’s job is patient
care and education, genetic counselors also serve as
resources to educate health professionals about
genetics.
PURPOSES
• Inform and advice
on the consequences and nature of the disorder.
The probability of developing or transmitting it.
Options available in managing and planning in order
to
prevent, avoid or ameliorate that defect.
• Genetic counselling has supportive as well as
diagnostic aspects.
• Provide family with complete and accurate
information about genetic disorders.
GOALS
• Promoting informed decisions by involved family
members.
• Clarifying the family’s options , available treatments and
prognosis.
• Examining alternatives to reduce the risk of genetic
disorders.
• Decreasing the incidence of genetic disorder.
• Reducing the impact of the disorder.
Principles To Be Followed For Effective
Counselling
• Genetic counselling must include an accurate
diagnosis and non directive counselling
• Provides information in a nonthreatening ,un biased
manner
• Reserves related decisions for the family.
• Counselling must be confidential and completely
truthful, upholding the family’s right to know what to
expect.
• It must be timed appropriately , preferably before
pregnancy.
BENEFICIARIES
• Individuals and families with known hereditary conditions
or diseases thought to have a hereditary component
• Examples: Alzheimer's disease, cancer, cystic fibrosis,
diabetes, Down syndrome, hemophilia, Huntington’s
disease, Parkinson’s disease, Sickle Cell disease
• Anyone who is considering genetic testing
• Individuals and couples who are concerned with issues
related to pregnancy, such as birth defects, transmission of
genetic conditions, or effect of pregnancy on existing
genetic risk
• couples who have had multiple miscarriages
• couples who are related, such as first cousins
• healthcare providers who seek genetics consultations for
their patients
Time To Seek Genetic Counselling
• In a paediatric scenario , genetic counselling can occur
• Before conception , (as a part of planned parenthood)
when one or both of the parents are carriers of a certain
trait such as sickle cell trait.
• During pregnancy when an abnormality is detected on an
ultrasound scan , especially when the female is older than
35 years.
• After the birth if a birth defect is seen.
• During childhood if the child has developmental delay.
PROCESS OF GENETIC COUNSELLING
In general, a genetic counseling session aims to:
• Increase the family’s understanding of a genetic condition
• Discuss options regarding disease management and the
risks and benefits of further testing and other options
• Help the individual and family identify the psychosocial
tools required to cope with potential outcomes
• Reduce the family’s anxiety
During the initial genetic counseling visit,
• The genetic counselor will determine why the
patient/family is seeking genetic counseling,
• identify what information they wish to obtain from the
session, collect and record a family medical history, and
• assess and record the medical and psychosocial history of
the patient.
• Prenatal genetic counselling is usually given by a
counsellor at a high risk or specialty prenatal clinic
that offers prenatal diagnosis.
• Paediatric and adult genetic counselling is given at a
genetics centre by a genetic nurse or a genetic
counsellor.
• In certain places premarital genetic testing and
counselling is advised. (e.g. .West Africa for sickle cell
anaemia) .
• In certain communities, premarital genetic testing is
mandatory and a genetic requirement. (e.g.. Maine ).
• A team approach that involves physicians ,nurses and
social workers is essential.
• A pre-testing session are the clinical presentation of
the condition(s) the patient may be at risk for, pattern
of genetic inheritance of the condition, chance of
recurrence, available testing procedures and test
limitations, reproductive options, and follow-up
procedures, if needed.
• General questions relating to suggested treatment or
therapy are also addressed.
• If genetic testing performed, the genetic counselor
often acts as the point person to communicate the
results.
• The post-test session often focuses on helping families
cope with the emotional, psychological, medical, social,
and economic consequences of the test results.
• In particular, psychological issues such as denial, anxiety,
anger, grief, guilt, or blame are addressed, and,
• when necessary, referrals for in-depth psychosocial
counseling are offered.
• Information about community resources and support
groups can be provided to the patient/family.
• If the genetic test is positive, testing may be considered for
additional relatives of the individual.
• Genetic counseling referrals for other family members for
risk assessment may be discussed
• To decrease the risk of transmitting the disorder, a genetic
counsellor can discuss with the family an alternative
arrangement such as adoption , artificial insemination,
surrogate pregnancy, prenatal diagnosis with selective
abortion or prenatal treatment, curative treatment with
gene splicing or fetal surgery.
• The nurse plays an important role in follow up ,clarifying
information,providing continuous support to the family in
the grieving process as appropriate.
• At the conclusion of the final genetic counseling session,
the patient may receive a written summary of the major
topics discussed.
• The summary is often provided in the form of a letter,
which serves as a permanent record of the information
discussed and can include additional information that
became available after the final counseling session.
• The patient may choose to share the letter with other
family members or healthcare providers.
IMPORTANCE OF GENETIC COUNSELLING
• Genetic counselors help identify families at possible risk of a
genetic condition by gathering and analyzing family history and
inheritance patterns and calculating chances of recurrence.
• They provide information about genetic testing and related
procedures.
• They are trained to present complex and difficult-to-
comprehend information about genetic risks, testing, and
diagnosis to families and patients.
• Genetic counselors can help families understand the
significance of genetic conditions in relation to cultural,
personal, and familial contexts.
• They also discuss available options and can provide
referrals to educational services, advocacy and support
groups, other health professionals, and community or state
services.
• Genetic counselors can serve as a central resource of
information about genetic conditions for other healthcare
professionals, patients, and the general public.
NURSES ROLE
• A nurse who opts to be genetic counselor undergoes
training.
• Obtain a detailed family history and construct a
pedigree (family history diagram)
• Assess and analyze hereditary and nonhereditary
disease risk factors
• Identify potential genetic conditions or genetic
predisposition to disease
• Provide genetic information and psychosocial support to
individuals and families
• Provide nursing care for patients and families at risk for or
affected by diseases with a genetic component
• Provide genetic counseling
(Advanced Practice Nurses)
• Facilitate genetic testing and interpret genetic test results
and laboratory reports
(Advanced Practice Nurses)
• Paediatric nurse who work as a genetic counsellor
work as a member of a health care team ,
providing information and support to families who
have a member with birth defect or genetic disorder
and families with a risk for a variety of inherited
conditions.
• They identify families at risk,
• investigate problems present in the family ,
• interpret information about disorder,
• analyse inheritance patterns and
• risk of recurrences and
• review available options with the family
• Provide supportive counselling to families.
• Serve as patient advocates.
• Refer individuals and families to community or state
support services.
• They also serve as educators and resource people for other
health care professionals
THANK YOU
You might also like
- PALS Systematic Approach Summary: Initial ImpressionDocument2 pagesPALS Systematic Approach Summary: Initial ImpressionMark Vergel II100% (3)
- Private Health Institutions LawDocument22 pagesPrivate Health Institutions LawShankar Sanyal100% (1)
- Genetic Counselling: Submitted By: Jinson Raju 3 YearDocument6 pagesGenetic Counselling: Submitted By: Jinson Raju 3 YearJanet VargheseNo ratings yet
- School of Nursing Science and Research (Sharda University) : Assignment ON Nutritional Problems in CommunityDocument15 pagesSchool of Nursing Science and Research (Sharda University) : Assignment ON Nutritional Problems in CommunitySamjhana Neupane100% (2)
- Otc Advisor PainDocument24 pagesOtc Advisor Painfarzad100% (2)
- Genetic CounsellingDocument3 pagesGenetic Counsellingavinash dhameriyaNo ratings yet
- Ethical, Legal, Psychosocial Issues in GeneticDocument68 pagesEthical, Legal, Psychosocial Issues in GeneticShalini ChanduNo ratings yet
- Current StatusDocument14 pagesCurrent Statusthilaga88No ratings yet
- Genetics & Health: Alka Mishra M. Sc. Nursing 1 YearDocument63 pagesGenetics & Health: Alka Mishra M. Sc. Nursing 1 Yearpandem soniyaNo ratings yet
- Government College of Nursing, Jodhpur: Presentation ONDocument7 pagesGovernment College of Nursing, Jodhpur: Presentation ONpriyanka0% (1)
- Research in Continuing Education Seminar Typed ContentDocument31 pagesResearch in Continuing Education Seminar Typed Contentpravina praviNo ratings yet
- Teachers' Role in Procuring and Managing InstructionalDocument29 pagesTeachers' Role in Procuring and Managing InstructionalElsy MayjoNo ratings yet
- Journal PresentationDocument14 pagesJournal PresentationValarmathiNo ratings yet
- Prepared by Rita Yadav (Thakur) : M.SC Nursing First YearDocument34 pagesPrepared by Rita Yadav (Thakur) : M.SC Nursing First Yearreeta yadav100% (1)
- Application of Betty Neuman TheoryDocument44 pagesApplication of Betty Neuman TheorySimon JosanNo ratings yet
- Visit To PSG College of Nursing: Submitted To Submitted byDocument8 pagesVisit To PSG College of Nursing: Submitted To Submitted byShubha JeniferNo ratings yet
- Unit-6 Sampling: Ms - Samjhana Neupane MSC - Nursing 1 Year SNSRDocument67 pagesUnit-6 Sampling: Ms - Samjhana Neupane MSC - Nursing 1 Year SNSRSamjhana Neupane100% (2)
- Master Rotation Plan IDocument5 pagesMaster Rotation Plan IannuNo ratings yet
- Use of Computers in Teaching, Learning, Research & Nursing PracticeDocument24 pagesUse of Computers in Teaching, Learning, Research & Nursing PracticeStephy SojanNo ratings yet
- Assignment On Standardized and Non Standardized Tool 2s by Kamini c2Document11 pagesAssignment On Standardized and Non Standardized Tool 2s by Kamini c2kamini Choudhary100% (1)
- Unit 2 Teaching-Learning in Nursing Education: ObjectivesDocument28 pagesUnit 2 Teaching-Learning in Nursing Education: ObjectivesLALRINTLUANGI CHHAKCHHUAKNo ratings yet
- Historical Development of Pediatrics and Pediatric Nursing in IndiaDocument6 pagesHistorical Development of Pediatrics and Pediatric Nursing in Indiapreet.solankiNo ratings yet
- Formulation of NCPDocument8 pagesFormulation of NCPSandeep choudharyNo ratings yet
- A Study To Assess The Effectiveness of Video Assisted Teaching Programme On Toilet Training of Toddlers Among Parents in A Selected Rural Area at Mangalore, Dakshina Kannada, Karnataka StateDocument7 pagesA Study To Assess The Effectiveness of Video Assisted Teaching Programme On Toilet Training of Toddlers Among Parents in A Selected Rural Area at Mangalore, Dakshina Kannada, Karnataka StateInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Ppt-Journal ClubDocument50 pagesPpt-Journal Clubgao1989No ratings yet
- Advance Nursing Practice Presentation On Sensory DeprivationDocument22 pagesAdvance Nursing Practice Presentation On Sensory DeprivationLaveena Aswale67% (3)
- Rajiv Gandhi University of Health Sciences, Bangalore, Karnataka Synopsis Proforma For Registration of Subjects For DissertationDocument14 pagesRajiv Gandhi University of Health Sciences, Bangalore, Karnataka Synopsis Proforma For Registration of Subjects For Dissertationpavin0% (1)
- Impact of SocialDocument10 pagesImpact of SocialNeenu RajputNo ratings yet
- Assignment AV-Aids-File-Msc-Nursing-1st-year - MD - FinalDocument61 pagesAssignment AV-Aids-File-Msc-Nursing-1st-year - MD - Finalmohamad dildar100% (2)
- Subject: Advanced Nursing Practice Topic: Treatment Aspects: Pharmacological and Pre and Post Operative Care AspectsDocument44 pagesSubject: Advanced Nursing Practice Topic: Treatment Aspects: Pharmacological and Pre and Post Operative Care Aspectsankita100% (1)
- Cont EduDocument18 pagesCont EduShilu Mathai PappachanNo ratings yet
- Report On PanelDocument6 pagesReport On PanelBhawna PandhuNo ratings yet
- A Study To Evaluate The Effectiveness of Structured Teaching Program On Knowledge and Practice Regarding Kangaroo Mother Care Among Post Natal Mothers Having Low Birth Weight Babies 1Document9 pagesA Study To Evaluate The Effectiveness of Structured Teaching Program On Knowledge and Practice Regarding Kangaroo Mother Care Among Post Natal Mothers Having Low Birth Weight Babies 1Manisa ParidaNo ratings yet
- Programmes Related To Child Health and WelfareDocument40 pagesProgrammes Related To Child Health and WelfareAleena ShibuNo ratings yet
- Health Economics and TechnologyDocument20 pagesHealth Economics and TechnologyPriya ANo ratings yet
- MCH ProgrammeDocument14 pagesMCH ProgrammepriyankaNo ratings yet
- Final Synopsis PHD CorrectionDocument24 pagesFinal Synopsis PHD CorrectionshailaNo ratings yet
- A.V AidsDocument9 pagesA.V AidsshailaNo ratings yet
- Problem Solving PPT Neww2023Document33 pagesProblem Solving PPT Neww2023Seham AlyNo ratings yet
- Growth and DevelopmentDocument144 pagesGrowth and DevelopmentRanjana SharmaNo ratings yet
- Information Education CommunicationDocument53 pagesInformation Education Communicationvinnu kalyanNo ratings yet
- Fetal Therapy: Hyaline Membrane DiseaseDocument5 pagesFetal Therapy: Hyaline Membrane DiseaseDelphy VargheseNo ratings yet
- Post Mature Neonate, Infant of Diabetic and Substance Abuse MotherDocument14 pagesPost Mature Neonate, Infant of Diabetic and Substance Abuse MotherShilpa JoshiNo ratings yet
- Utilisation of Research FindingsDocument13 pagesUtilisation of Research Findingsshalini75No ratings yet
- 08 - Literature Search Using InternetDocument65 pages08 - Literature Search Using InternetFarhan KhanNo ratings yet
- Roles and Responsibilitis of Community Health NurseDocument22 pagesRoles and Responsibilitis of Community Health NurseAnusha AnishNo ratings yet
- Presentation On Pattern of Nursing Education andDocument7 pagesPresentation On Pattern of Nursing Education andnaga maniNo ratings yet
- Title Page: Title of The Article: "A Study To Assess The Effectiveness of Structured Teaching Programme OnDocument9 pagesTitle Page: Title of The Article: "A Study To Assess The Effectiveness of Structured Teaching Programme OnInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Health Education BureauDocument13 pagesHealth Education Bureauv_vijayakanth7656No ratings yet
- Scope of Nursing Research, EthicsDocument16 pagesScope of Nursing Research, EthicsAmanda ScarletNo ratings yet
- 1.clinical Teaching Methods MokshithaDocument23 pages1.clinical Teaching Methods MokshithaVeena DalmeidaNo ratings yet
- Seminar On Nurse PractitionerDocument13 pagesSeminar On Nurse PractitionerPriya A100% (1)
- Health BeliefDocument30 pagesHealth BeliefHemantNo ratings yet
- Infant of Diabetic MotherDocument16 pagesInfant of Diabetic MotherJOSLIN100% (1)
- Seminar On Hospitalized ChildDocument29 pagesSeminar On Hospitalized ChildArchanaNo ratings yet
- State Nursing Council1Document3 pagesState Nursing Council1suman gupta100% (1)
- Research Problem: Mr. Jayesh Patidar WWW - Drjayeshpatidar.blogspot.c OmDocument42 pagesResearch Problem: Mr. Jayesh Patidar WWW - Drjayeshpatidar.blogspot.c OmKrishnaveni MurugeshNo ratings yet
- Report of Inservice EducationDocument35 pagesReport of Inservice EducationAkansha JohnNo ratings yet
- Legal Aspects and EthicsDocument18 pagesLegal Aspects and EthicsBuyung Tegar AribowoNo ratings yet
- Assertiveness: Presented by Maj Mercy Jacob 1 Year M SC Trainee OfficerDocument24 pagesAssertiveness: Presented by Maj Mercy Jacob 1 Year M SC Trainee OfficerMercy JacobNo ratings yet
- Genetic CounselingDocument26 pagesGenetic CounselingJEEJANo ratings yet
- Genetic CounsellingDocument23 pagesGenetic Counsellingleih jsNo ratings yet
- Counselling and Practical Application of Genetic in NursingDocument30 pagesCounselling and Practical Application of Genetic in NursingBhawna JoshiNo ratings yet
- Scientific Programme PDFDocument20 pagesScientific Programme PDFChockalingam R MNo ratings yet
- Superficial Femoral Artery InjuryDocument3 pagesSuperficial Femoral Artery InjuryErlin EsauNo ratings yet
- Duloxetine PDFDocument4 pagesDuloxetine PDFscribdseewalNo ratings yet
- نموذج الامتيازات السريريةDocument67 pagesنموذج الامتيازات السريريةSAFA ALYNo ratings yet
- Bronze Sponsors - ECVIM-CA CONGRESSDocument5 pagesBronze Sponsors - ECVIM-CA CONGRESSLaia GardanNo ratings yet
- Diagnostic Radiology - New Cover2021Document154 pagesDiagnostic Radiology - New Cover2021fouzi bentayebNo ratings yet
- Seminar On FibroadenosisDocument23 pagesSeminar On FibroadenosisSk Saklin MustakNo ratings yet
- Staff List As On 01072017 PDFDocument58 pagesStaff List As On 01072017 PDFVocxx PopluNo ratings yet
- Roula Choueiri CDC Act Early Ambassador To Ma - Ma Act Early Updates April 2017Document33 pagesRoula Choueiri CDC Act Early Ambassador To Ma - Ma Act Early Updates April 2017Paola BGNo ratings yet
- Biology Jan 2020 1BRDocument32 pagesBiology Jan 2020 1BRMohamedNo ratings yet
- Insulin in DMDocument46 pagesInsulin in DMask1400No ratings yet
- Planning and Design 1 - Breathing RateDocument3 pagesPlanning and Design 1 - Breathing RateNelson LongsworthNo ratings yet
- Afib Protocol Exclusion CriteriaDocument3 pagesAfib Protocol Exclusion CriteriaJesse M. MassieNo ratings yet
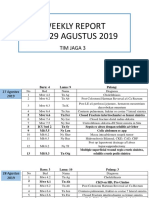
- WR Tim Jaga 3Document285 pagesWR Tim Jaga 3VincentiusNo ratings yet
- Resume - Hamid Kermani MoakharDocument2 pagesResume - Hamid Kermani Moakharmohammadrezahajian12191No ratings yet
- H N O S CH N: Indication DosageDocument2 pagesH N O S CH N: Indication DosagehelloaNo ratings yet
- Peptic Ulcer - Naitik Trivedi PDFDocument72 pagesPeptic Ulcer - Naitik Trivedi PDFSuraj PatilNo ratings yet
- Pemanfaatan Epas Pada LBPDocument134 pagesPemanfaatan Epas Pada LBPBesa Erlin PukaNo ratings yet
- Eaton County Apparent Drowning Death UnidentifiedDocument5 pagesEaton County Apparent Drowning Death UnidentifiedFergus BurnsNo ratings yet
- Health MateDocument3 pagesHealth MateAnisah AquilaNo ratings yet
- 01 What Economics Is AboutDocument1 page01 What Economics Is AboutcarloNo ratings yet
- 7th of OctoberDocument19 pages7th of OctoberOthman AldhewaileNo ratings yet
- Glucose Control in Acute Brain InjuryDocument8 pagesGlucose Control in Acute Brain InjurymohamedNo ratings yet
- Bls Study GuideDocument2 pagesBls Study GuideJohnNo ratings yet
- UntitledDocument8 pagesUntitledAman KhanNo ratings yet
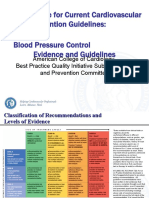
- 3 ACC Prevention Blood PressureDocument69 pages3 ACC Prevention Blood PressureMelissa Delgado100% (1)
- 2020 Pre-Operative Diagnosis of A Primary Uterine Mature TeratomaDocument4 pages2020 Pre-Operative Diagnosis of A Primary Uterine Mature Teratomapaula rangelNo ratings yet