Professional Documents
Culture Documents
Anes Journal Appraisal
Anes Journal Appraisal
Uploaded by
Jade Monreal0 ratings0% found this document useful (0 votes)
20 views18 pagesThis journal appraises a study that compared norepinephrine and phenylephrine infusions for maintaining blood pressure during cesarean deliveries. The study found that both drugs effectively controlled blood pressure but norepinephrine was associated with fewer interventions needed. There were no significant differences in other outcomes like rates of hypotension. The results could apply to the local population but were limited by being a single-centered study that excluded patients with cardiac issues and only involved elective c-sections.
Original Description:
Original Title
ANES JOURNAL APPRAISAL
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis journal appraises a study that compared norepinephrine and phenylephrine infusions for maintaining blood pressure during cesarean deliveries. The study found that both drugs effectively controlled blood pressure but norepinephrine was associated with fewer interventions needed. There were no significant differences in other outcomes like rates of hypotension. The results could apply to the local population but were limited by being a single-centered study that excluded patients with cardiac issues and only involved elective c-sections.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
20 views18 pagesAnes Journal Appraisal
Anes Journal Appraisal
Uploaded by
Jade MonrealThis journal appraises a study that compared norepinephrine and phenylephrine infusions for maintaining blood pressure during cesarean deliveries. The study found that both drugs effectively controlled blood pressure but norepinephrine was associated with fewer interventions needed. There were no significant differences in other outcomes like rates of hypotension. The results could apply to the local population but were limited by being a single-centered study that excluded patients with cardiac issues and only involved elective c-sections.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 18
Journal Appraisal
By PGMI Jasleen Dennise V. Monreal
Team Bravo (11 – 20 June 2020)
Journal
Appraisal tool
• Appraised using Critical Appraisal Skills Program Checklist from
Oxford Center for Triple Value Healthcare Ltd www.casp-uk.net
Did the trial address a clearly focused
issue?
• Yes, the authors clearly stated that the aim of the study was to
compare Norepinephrine and Phenylephrine variable, manually
adjusted infusion for maintenance of maternal blood pressure
during caesarean delivery.
Was the assignment of patients to
treatments randomized?
• Yes, a computer-generated sequence was achieved by a statistician
using an online random number generator.
• Patient codes were placed into sequentially numbered sealed
opaque envelopes.
Were all the patients who entered the trial
properly accounted for?
• Yes, the authors set an eligibility criteria for the participants and the patient
who joined the trial was accounted for
• Eligibility Criteria
Inclusion Criteria Exclusion Criteria
Full-term singleton pregnant Patients with uncontrolled
women, admitted for elective cardiac morbidities, hypertensive
caesarean delivery, aged between disorders of pregnancy,
18 and 40 years. peripartum bleeding, coagulation
disorders, and baseline systolic
blood pressure (SBP) < 100
mmHg
Were the patients, health workers and
study personnel blind to the treatment?
• Yes, the study is a randomized, double blind, controlled trial and
was conducted in obstetric department in a single institution.
Were the group similar at the start of the
trial?
• Yes, patients’ characteristics were comparable in the two study
groups.
Aside from the experimental intervention,
were the groups treated equally?
• Yes, all of the study participant are treated equally.
o All of the patients were monitored using electrocardiography, pulse
oximetry, and non-invasive blood pressure monitor.
o Same pre-medication drugs were delivered (metoclopramide 10 mg, and
ranitidine 50 mg)
o Ten milligrams hyperbaric bupivacaine in addition to 20 mcg fentanyl
were injected in L3-L4 or L4-L5 interspace using 25 G spinal needle.
Were the groups treated equally?
After spinal block, patients received the vasopressor infusion according to
the allocated study group:
• NE group (n = 60): received NE infusion with a starting rate of 0.05
mcg/kg/min. Norepinephrine bitartrate (8 mg norepinephrine
bitartrate/4 mL, which is equivalent to 4 mg norepinephrine base/4 mL
produced by Alexandria Co. for pharmaceuticals and chemical industries,
Egypt) was diluted to reach a final concentration of 4 mcg/mL.
• PE group (n = 63): received PE infusion with a starting rate of 0.75
mcg/kg/min. Phenylephrine hydrochloride (10 mg/1 mL ampoule,
produced by Sterop Co. Belgium) was diluted to reach a final
concentration of 50 mcg/mL.
How large was the treatment effect?
Primary Outcome: Incidence of Post-spinal anesthesia hypotension (PSH)
Secondary Outcome: Incidence of severe PSH, incidence of post-delivery
hypotension, SBP (baseline reading and the subsequent 12 readings), heart
rate (baseline reading and the subsequent 12 readings), incidence of
intraoperative nausea and vomiting, incidence of reactive hypertension,
intraoperative requirements of phenylephrine, ephedrine and atropine,
number of physician interventions per mother (physician intervention was
defined as any of the following: vasopressor bolus, atropine bolus, cessation,
re-starting, and changing of the vasopressor infusion rate), intraoperative
fluid intake, umbilical blood gases (pH, PCO2, PO2, and HCO3), and Apgar
score for the neonate at 1 minute and 5 minutes post-delivery.
How large was the treatment effect?
• The incidence of PSH {NE group: 18/60 (30%), PE group: 20/63 (32%), P =
0.8}, severe PSH, nausea, vomiting and rescue vasopressor consumption were
not statistically different between the two groups
• Incidence of reactive hypertension was halved, and incidence of bradycardia
was also nearly halved in NE group compared to PE group, although these
differences did not reach statistical significance (respectively: 12% vs. 24%, P
= 0.1, and 13% vs. 21%, P = 0.3).
• NE group showed lower number of physician interventions per mother
compared to PE group with median (quartiles) number of interventions of 0
(0, 1) and 1(0, 3) respectively (P = 0.001). The number of mothers who
needed at least one physician intervention was lower in NE group compared
to PE group [26 (43%) versus 45 (71%), P = 0.002]
How large was the treatment effect?
• The neonatal outcomes were comparable between both groups.
Summary of Results
• The authors reported that NE and PE effectively controlled
maternal blood pressure during caesarean delivery; however, NE
infusion was associated with less number of physician
interventions.
• There was a potentially lower incidence of bradycardia and
reactive hypertension in NE group compared to PE group without
reaching statistical significance.
Can the results be applied to local
population?
• Yes, the study provides an evidence-based approach in choosing an
appropriate drug for an obstetric patient in preventing post-spinal
anesthesia hypotension, which can be used in the Philippine
setting.
Were all clinically important outcomes
considered?
• The primary and secondary outcomes included in the study are all
clinically relevant for an obstetric patient, however, some
limitations were seen such as it is a single-centered study, the
authors did not include mothers with cardiac morbidities, and all
of the participants were scheduled to elective caesarean delivery.
You might also like
- 18d Nls Use Manual EnglishDocument136 pages18d Nls Use Manual Englishneo carty100% (1)
- ABGC Practice Exam - No AnswersDocument32 pagesABGC Practice Exam - No AnswersSara WoffordNo ratings yet
- Department of Pathology, Dhanalakshmi Srinivasan Medical College and Hospital, Siruvachur, Perambalur, Tamil Nadu, IndiaDocument14 pagesDepartment of Pathology, Dhanalakshmi Srinivasan Medical College and Hospital, Siruvachur, Perambalur, Tamil Nadu, IndiaaishaNo ratings yet
- (Clinical Cases Uncovered) - CARDIOLOGY - (2010) - Halaman-202-207Document6 pages(Clinical Cases Uncovered) - CARDIOLOGY - (2010) - Halaman-202-207zizaNo ratings yet
- Genetics ReviewDocument80 pagesGenetics Reviewzubair sayedNo ratings yet
- Portfolio Pat 1Document18 pagesPortfolio Pat 1api-365835586No ratings yet
- Critical Appraisal: DR A C J Hutchesson Chair of Examiners' Panel, Frcpath (Clinical Biochemistry)Document10 pagesCritical Appraisal: DR A C J Hutchesson Chair of Examiners' Panel, Frcpath (Clinical Biochemistry)monday125No ratings yet
- Simulation StationDocument2 pagesSimulation Stationmonday125No ratings yet
- FOCUS SAS Training Day Leeds Dr. Joanna Sheldon Protein Reference Unit, St. George'sDocument19 pagesFOCUS SAS Training Day Leeds Dr. Joanna Sheldon Protein Reference Unit, St. George'smonday125No ratings yet
- ICP-MS Talk ACBDocument31 pagesICP-MS Talk ACBmonday125No ratings yet
- DR Cole Storage Disorders Hand OutDocument3 pagesDR Cole Storage Disorders Hand Outmonday125No ratings yet
- Katherine Birch Specialist Testing of CSFDocument43 pagesKatherine Birch Specialist Testing of CSFmonday125No ratings yet
- Routine and Acute Clinical ChemistryDocument2 pagesRoutine and Acute Clinical ChemistryMohamed MounirNo ratings yet
- DR Moat Paediatric BochemistryDocument62 pagesDR Moat Paediatric Bochemistrymonday125No ratings yet
- Prof. Joy V. Lorin-Picar Davao Del Norte State College: New Visayas, Panabo CityDocument91 pagesProf. Joy V. Lorin-Picar Davao Del Norte State College: New Visayas, Panabo CityJeLo ReaNdelarNo ratings yet
- IFCC TF Ethics in Lab MedicineDocument16 pagesIFCC TF Ethics in Lab MedicineDr.Deepanshu SinghalNo ratings yet
- Scientist Viva AnswerDocument2 pagesScientist Viva Answermonday125No ratings yet
- Laboratory Tests For EndocrinologyDocument6 pagesLaboratory Tests For EndocrinologyAnastasia100% (1)
- Wet Practical Frcpath2014Document7 pagesWet Practical Frcpath2014monday125No ratings yet
- Chemical Pathology Job Description December 2011Document9 pagesChemical Pathology Job Description December 2011Chengyuan ZhangNo ratings yet
- EQASDocument23 pagesEQASSobha MatthewNo ratings yet
- Prenatal Diagnosis (Brynn Levy)Document357 pagesPrenatal Diagnosis (Brynn Levy)Pranali PatelNo ratings yet
- Microsoft Power Point - FRCPath Practical Exam 2009 WebsiteDocument20 pagesMicrosoft Power Point - FRCPath Practical Exam 2009 Websitesakai33100% (1)
- MayoTestCatalog Rochester SortedByTestName Duplex InterpretiveDocument2,763 pagesMayoTestCatalog Rochester SortedByTestName Duplex InterpretiveLaboratorium RS BELLANo ratings yet
- Alpha Fetoprotein (Afp)Document10 pagesAlpha Fetoprotein (Afp)Andi UkengNo ratings yet
- Chemical Pathology HODocument17 pagesChemical Pathology HOMurali TiarasanNo ratings yet
- Acid-Base MSC CasesDocument16 pagesAcid-Base MSC Casesmonday125No ratings yet
- Troubleshooting: - Sample Problems - Method/test Problems - Instrument ProblemsDocument6 pagesTroubleshooting: - Sample Problems - Method/test Problems - Instrument Problemsmonday125No ratings yet
- Chemical Pathology Reference Range 2017Document19 pagesChemical Pathology Reference Range 2017Shobana RaveendranNo ratings yet
- Chemical Pathology II HIV AIDSDocument33 pagesChemical Pathology II HIV AIDSSimeon AdebisiNo ratings yet
- Chapter 1 - Introduction: StudentDocument72 pagesChapter 1 - Introduction: Studentcloud_fantasyNo ratings yet
- Flow Cytometry, Immunohistochemistry, and Molecular Genetics For Hematologic Neoplasms (PDFDrive)Document450 pagesFlow Cytometry, Immunohistochemistry, and Molecular Genetics For Hematologic Neoplasms (PDFDrive)Mário da Costa PintoNo ratings yet
- Karen Smith Duty Biochemist ScenariosDocument43 pagesKaren Smith Duty Biochemist Scenariosmonday125100% (3)
- Predanalitika KoagulacijaDocument10 pagesPredanalitika KoagulacijaAnonymous w4qodCJNo ratings yet
- Endocrine QuizDocument34 pagesEndocrine Quizakash kondapalliNo ratings yet
- Classical Homocystinuria Disorder SummaryDocument5 pagesClassical Homocystinuria Disorder Summarymonday125No ratings yet
- Bloody Easy 4Document82 pagesBloody Easy 4dubblewalker100% (1)
- A Review of Medical Errors in Laboratory Diagnostics and Where We Are TodayDocument4 pagesA Review of Medical Errors in Laboratory Diagnostics and Where We Are TodaytaghamdNo ratings yet
- National Board of Examinations Dated: 19 April 2018: Question Paper For NEET-SSDocument6 pagesNational Board of Examinations Dated: 19 April 2018: Question Paper For NEET-SSrajvolgaNo ratings yet
- Drummelsmith - Laboratory Diagnosis and Bacterial Identification - Study GuideDocument19 pagesDrummelsmith - Laboratory Diagnosis and Bacterial Identification - Study GuideTom TsouNo ratings yet
- Automated Versus Manual Platelet Count in Aden 2161 0681-3-149Document4 pagesAutomated Versus Manual Platelet Count in Aden 2161 0681-3-149Jeffry MaglalangNo ratings yet
- Chemical Pathology Workshop II - Diagnostic Theory in Chemical Pathology (2017.11.14)Document57 pagesChemical Pathology Workshop II - Diagnostic Theory in Chemical Pathology (2017.11.14)Arthur Chang100% (1)
- 5527 and AmendmentsDocument18 pages5527 and AmendmentsMica BernardoNo ratings yet
- CLIAbrochure8 PDFDocument12 pagesCLIAbrochure8 PDFAlexandr Chuvakov100% (1)
- Ovarian Reserve Testing and Follicular MonitoringDocument35 pagesOvarian Reserve Testing and Follicular Monitoringjindal clinicsNo ratings yet
- Quality Control in A Clinical LaboratoryDocument9 pagesQuality Control in A Clinical LaboratoryHenry OseiNo ratings yet
- Cast in Urine SedimentDocument3 pagesCast in Urine Sedimentfirie100% (1)
- Pathology 9Document34 pagesPathology 9Lorenzo FrancisNo ratings yet
- Sp0005. Platelet Antibody Direct - Pakplus (Elisa)Document7 pagesSp0005. Platelet Antibody Direct - Pakplus (Elisa)yennieyenfulNo ratings yet
- Objectives:: Enzymes - Prelims Lesson 04Document13 pagesObjectives:: Enzymes - Prelims Lesson 04Louise BandalaNo ratings yet
- Inborn Errors of Metabolism - Basics For Students (Iver Andreas Norbergs Kopi Som Er I Konflikt 2016-01-24)Document4 pagesInborn Errors of Metabolism - Basics For Students (Iver Andreas Norbergs Kopi Som Er I Konflikt 2016-01-24)Wen Jie LauNo ratings yet
- Clinical Lab TechnqDocument67 pagesClinical Lab TechnqRatnamala SarmaNo ratings yet
- Platelet Storage Pool Disorders PDFDocument4 pagesPlatelet Storage Pool Disorders PDFMano CempakaNo ratings yet
- Rules of 3 Jeri Walters Knoxville 2015Document26 pagesRules of 3 Jeri Walters Knoxville 2015pieterinpretoria391No ratings yet
- The Significance of The Hemoglobin A2Document18 pagesThe Significance of The Hemoglobin A2Paula MadureuraNo ratings yet
- Mock Board Review 3Document5 pagesMock Board Review 3billNo ratings yet
- Toxicology and TDMDocument121 pagesToxicology and TDMteppie0917No ratings yet
- Criteria For Specimen AcceptabilityDocument3 pagesCriteria For Specimen AcceptabilityFatwa100% (1)
- 2.5 Antibody ScreeningDocument5 pages2.5 Antibody ScreeningBALAJINo ratings yet
- Mls Imls Reading ListDocument3 pagesMls Imls Reading ListPeng KwanNo ratings yet
- Opioids: General Trans FormatDocument2 pagesOpioids: General Trans FormatJade Monreal100% (1)
- Revised FIGO Staging For Carcinoma of The Cervix Uteri - Bhatla - 2019 - International Journal of Gynecology & Obstetrics - Wiley Online LibraryDocument19 pagesRevised FIGO Staging For Carcinoma of The Cervix Uteri - Bhatla - 2019 - International Journal of Gynecology & Obstetrics - Wiley Online LibraryJade MonrealNo ratings yet
- Katzung Summary of DrugsDocument45 pagesKatzung Summary of DrugsJade MonrealNo ratings yet
- Conjunctivitis: by PGMI Jasleen MonrealDocument77 pagesConjunctivitis: by PGMI Jasleen MonrealJade MonrealNo ratings yet
- Course in The Wards FormatDocument2 pagesCourse in The Wards FormatJade MonrealNo ratings yet
- 4th Shifting Micro Lab ReviewerDocument154 pages4th Shifting Micro Lab ReviewerJade MonrealNo ratings yet
- Breast Reviewer (2014)Document7 pagesBreast Reviewer (2014)Jade Monreal0% (1)
- Burkitt's Lymphoma in HIV-Positive Child: Diagnostic Ascitic Fluid CytologyDocument2 pagesBurkitt's Lymphoma in HIV-Positive Child: Diagnostic Ascitic Fluid CytologyJade MonrealNo ratings yet
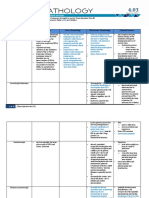
- General Pathology 4.03 Endocrine System Super SummaryDocument15 pagesGeneral Pathology 4.03 Endocrine System Super SummaryJade MonrealNo ratings yet
- Interspecific Competition Can Limit The Number of Species That Can Coexist in A Community and Affect TheDocument10 pagesInterspecific Competition Can Limit The Number of Species That Can Coexist in A Community and Affect TheJade MonrealNo ratings yet
- KRAS G12D MutationsDocument13 pagesKRAS G12D Mutationslol pookNo ratings yet
- Stroke (Bisaya and English)Document4 pagesStroke (Bisaya and English)AnaNo ratings yet
- Outpatient Art Therapy With A Suicidal AdolDocument16 pagesOutpatient Art Therapy With A Suicidal AdolEsteban Ferrandez MirallesNo ratings yet
- Fundamentals of Nursing TestDocument78 pagesFundamentals of Nursing TestNicomille T. Caliging80% (5)
- Pengaruh Derajat Kelainan Refraksi Dan Penggunaan Kacamata Koreksi Terhadap Ketajaman Stereopsis Pada AnakDocument8 pagesPengaruh Derajat Kelainan Refraksi Dan Penggunaan Kacamata Koreksi Terhadap Ketajaman Stereopsis Pada AnakAndi Adam Jr.No ratings yet
- Actual NCPDocument10 pagesActual NCPRouie Björn ABrianNo ratings yet
- Immunology Summit UCBDocument2 pagesImmunology Summit UCBJuan G. Ovalles B.No ratings yet
- ICU AlgorithmsDocument45 pagesICU AlgorithmsHashimIdreesNo ratings yet
- Food Poisoning Treatment What To ExpectDocument3 pagesFood Poisoning Treatment What To ExpectPrian Estrella ClaudioNo ratings yet
- PneumothoraxDocument3 pagesPneumothoraxYara YousefNo ratings yet
- تجميعات شهر مارس EmsDocument11 pagesتجميعات شهر مارس EmsMohamed MahmoudNo ratings yet
- Clinicopathological Profile and Outcome of Infection-Related Glomerulonephritis (Irgn) :a Single Center ExperienceDocument7 pagesClinicopathological Profile and Outcome of Infection-Related Glomerulonephritis (Irgn) :a Single Center ExperienceIJAR JOURNALNo ratings yet
- Amali DarahDocument31 pagesAmali DarahMhd Shazly FahmiNo ratings yet
- Fracture Colles Rehabilitation Advice Following WristDocument4 pagesFracture Colles Rehabilitation Advice Following WristfaprilisaNo ratings yet
- Pain Management NCLEXDocument5 pagesPain Management NCLEXPotchiee PfizerNo ratings yet
- Depression PDFDocument54 pagesDepression PDFAndrew FongNo ratings yet
- Understanding Ventilator Waveforms-And How To Use Them in Pa... - Nursing2020 Critical CareDocument19 pagesUnderstanding Ventilator Waveforms-And How To Use Them in Pa... - Nursing2020 Critical Caremahbub alamNo ratings yet
- Borges, K. Et Al. (2018)Document7 pagesBorges, K. Et Al. (2018)Paulina Bermudez ValenzuelaNo ratings yet
- (Kannan Et Al., 2012) Thermal Burn of Palate in An Elderly Diabetic PatientDocument4 pages(Kannan Et Al., 2012) Thermal Burn of Palate in An Elderly Diabetic PatientAFINA MUTIAH TUHEPALYNo ratings yet
- Cases in Medical EthicsDocument8 pagesCases in Medical EthicsOmarNo ratings yet
- Ipsen Announces FDA Approval of A New Delivery Device For Somatuline® Depot® (Lanreotide) PFS InjectionDocument6 pagesIpsen Announces FDA Approval of A New Delivery Device For Somatuline® Depot® (Lanreotide) PFS Injectionraju1559405No ratings yet
- Text Extraction Engine To Upgrade Clinical Decision Support SystemDocument4 pagesText Extraction Engine To Upgrade Clinical Decision Support SystemjournalNo ratings yet
- Oil and Natural Gas Corporation LTD Self Declaration On Medical StatusDocument4 pagesOil and Natural Gas Corporation LTD Self Declaration On Medical StatusDodiya NikunjNo ratings yet
- GINA Under5 Pocket 20091 1Document0 pagesGINA Under5 Pocket 20091 1Boby ShéNo ratings yet
- Bihar HospitalDocument4 pagesBihar Hospitalmahwish khanNo ratings yet
- Andrew Austin - IEMT & Long Term Anxiety - DVD Cover PDFDocument2 pagesAndrew Austin - IEMT & Long Term Anxiety - DVD Cover PDFMichael CliftonNo ratings yet
- WM9 3 Chronic Lymphocytic Leukemia CLLDocument6 pagesWM9 3 Chronic Lymphocytic Leukemia CLLyorghiLNo ratings yet
- MHS 6401Document5 pagesMHS 6401Delelegn EmwodewNo ratings yet
- Summary of Intestinal and Luminal ProtozoaDocument3 pagesSummary of Intestinal and Luminal ProtozoaMegh Raj BhattNo ratings yet