Professional Documents
Culture Documents
PHL 4201: Body Fluids & Blood: DR K.G. Ibrahim (Aka DR Ghandi)
PHL 4201: Body Fluids & Blood: DR K.G. Ibrahim (Aka DR Ghandi)
Uploaded by
SA Wakili0 ratings0% found this document useful (0 votes)
17 views34 pagesWhite blood cells
Original Title
Leucocytes
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentWhite blood cells
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
17 views34 pagesPHL 4201: Body Fluids & Blood: DR K.G. Ibrahim (Aka DR Ghandi)
PHL 4201: Body Fluids & Blood: DR K.G. Ibrahim (Aka DR Ghandi)
Uploaded by
SA WakiliWhite blood cells
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 34
PHL 4201: Body fluids & Blood
Leucocytes
Dr K.G. Ibrahim (aka Dr Ghandi)
Department of Physiology,
Faculty of Basic Medical Sciences,
College of Health Sciences,
Usmanu Danfodiyo University,
ghandi.kasimu@udusok.edu.ng
Sokoto.
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Defense Against Infection
• Our world is teeming with microorganisms, which
can be beneficial or harmful.
• Phagocytes can ingest and destroy invading
organisms, and participate in tissue reactions that
“wall off” infection.
• Other white cells mediate responses
(antibodies/sensitized lymphocytes) that destroy or
neutralize specific microorganisms.
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
White Blood Cells
• Mobile units of the body’s immune defence
system
• Immunity is the ability to eliminate potentially
harmful materials or abnormal cells
• Leucocytes and their derivatives together with
a variety of plasma proteins make up the
immune system
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
White Blood Cells
The immune system specifically:
• Defends against invading pathogens
• Functions as a clean up crew that removes
worn out cells paving way for wound healing
and tissue repair
• Identifies and destroys abnormal or mutant
cells that arise in the body.
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
White Blood Cells
• Circulate in blood and may enter the tissues
• Are of six types:
- Polymorphonuclear neutrophils
- “ eosinophils
- “ basophils
- Monocytes
- Lymphocytes (plasma cells)
- Platelets (from megakaryocytes)
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
White Blood Cell Counts
• Total WBC ~ 7,000 / mm3
(almost 1,000-fold fewer than RBCs)
• Proportions:
- Neutrophils 62%
- Eosinophils 2.3%
- Basophils 0.4%
- Monocytes 5.3%
- Lymphocytes 30%
• Platelets ~ 300,000 / mm3
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Leukopoiesis
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Genesis of White Blood Cells
• Granulocytes and monocytes develop in the bone
marrow, and most remain there until needed
peripherally (number in marrow ~3x blood; 6-day supply)
• Lymphocytes develop mostly in the peripheral
lymphoid organs (thymus, spleen, tonsils, lymph nodes,
Peyer’s patches)
• Megakaryocytes develop and reside in the marrow,
fragment to release platelets
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Life Span of White Blood Cells
• Granulocytes:
– Circulating, 4 – 8 hours
– In the tissues, 4 – 5 days
(shorter timelines with infection, inflammation)
• Monocytes / Macrophages:
– Circulating, 10 – 20 hours
– As tissue macrophages, months or longer
• Lymphocytes:
– Continuously re-circulate: lymph…nodes…blood
– Long-lived… weeks, months, longer
• Platelets: ~ Replaced every ten days
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Neutrophils and Macrophages
• Neutrophils are mature cells that can respond
immediately to infection
• Monocytes mature in the tissues to become macrophages
• Both exhibit motility:
– Diapedesis
– Ameboid motion
– Chemotaxis (Chemoattractants: bacterial or tissue degradation
products, complement fragments, other chemical mediators)
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Neutrophil Margination & Migration
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Phagocytosis
• “Phagocytosis” is the ingestion of particles
• Phagocytes must distinguish foreign particles from host
tissues
• Appropriate phagocytic targets:
– May have rough surfaces
– Lack protective protein coats
– May be immunologically marked for phagocytosis by
antibodies or complement components that are recognized by
receptors on the phagocytes
… this immunologic marking is called “opsonization”
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Phagocytosis
• Neutrophils: can ingest 3-20 bacteria
• Macrophages: After being activated in the tissues, are
extremely effective phagocytes (up to ~100 bacteria)
• Macrophages can ingest larger particles…
– Damaged RBCs
– Malarial parasites
• Macrophages can extrude digestion products and
survive and function for many months
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Digestion of Ingested Particles
• In both neutrophils and macrophages,
phagosomes fuse with lysosomes and other
granules to form phagolysosomes (digestive
vesicles)
• These contain proteolytic enzymes, and in
macrophages, lipases (important in killing
tuberculosis bacillus and some other bacteria)
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Bactericidal Agents
• Bacteria may be killed even if they are not digested
• Enzymes in the phagosome or in peroxisomes
generate strongly bactericidal reactive oxygen
species…
– Superoxide (O2-)
– Hydrogen peroxide (H2O2)
– Hydroxyl ions (OH-)
– Myeloperoxidase catalyzes H2O2 + 2 Cl- …
… 2 H+ + 2 ClO-
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
The Reticuloendothelial System
• After entering the tissues, macrophages become
fixed and may be resident for years
• When appropriately stimulated they can break
away and move to sites of inflammation
• Circulating monocytes, mobile macrophages, fixed
tissue macrophages, and some specialized
endothelial cells form the reticuloendothelial
system, almost all derived from monocytes,
comprising a phagocytic system located in all
tissues
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Specialized Macrophages
• Skin, subcutaneous (histiocytes)
• Lymph nodes
– Ingest / sample particles arriving through the lymph
• Alveolar macrophages
– Digest or entrap inhaled particles and
microorganisms
• Kupffer cells
– Surveillance of the portal circulation
• Macrophages in the spleen and bone marrow
– Surveillance of the general circulation
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Structure of a Lymph Node
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Kupffer Cells in the Liver
Sinusoids
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Structure of the Spleen
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Neutrophils, Macrophages &
Inflammation
• Inflammation is driven by chemical mediators and
characterized by heat, redness, swelling, and pain
• Physiologically, it involves…
– Vasodilatation and increased blood flow
– Increased capillary permeability
– Coagulation of interstitial fluids
– Accumulation of granulocytes and monocytes
– Swelling of tissue cells
• Mediators: histamine, bradykinin, serotonin,
prostaglandins, complement products, clotting
components, lymphokines
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
“Walling Off” Sites of Inflammation
• Fibrinogen clots minimize fluid flow in and out of
the inflamed area
• Staphylococci cause intense inflammation and are
effectively “walled off”
• Streptococci induce less intense inflammation and
may be more likely to spread than staphylococci
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Neutrophils and Macrophages in
Inflammation
• Tissue macrophages that encounter foreign particles
enlarge and become mobile to provide a first line of
defense
• Within an hour neutrophils migrate to the area in
response to inflammatory cytokines (TNF, IL-1)
• Upregulated selectins and ICAM-1 on endothelial cells
are bound by integrins on neutrophils, leading to
margination, followed by diapedesis, and chemotaxis
directing neutrophils into the inflamed tissues, to kill
bacteria and scavenge
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Neutrophil Migration to an Inflamed
Site
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Neutrophilia
• With intense inflammation neutrophil count
can increase dramatically…
4,000-5,000 15,000-25,000
• Results from mobilization of mature
neutrophils from the bone marrow by
inflammatory mediators
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Secondary Macrophage Invasion
• In response to chemoattractants, monocytes
gradually accumulate and become macrophages
(after ~ 8 hours)
• In part due to increased bone marrow
production, macrophages become the dominant
inflammatory cell over several weeks, cleaning
up remaining bacteria, necrotic tissue, and
directing tissue remodeling.
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Bone Marrow Responses
• Growth factors produced in response to infection
and inflammation drive proliferation and
differentiation of leukocyte precursors in the
marrow
• First mature cells released after 3 – 4 days
• The bone marrow can increase production of
neutrophils and monocytes by 20 – 50- fold and
maintain this for months or years
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Bone Marrow Response to
Inflammation
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Formation of Pus
• Pus is composed of dead bacteria and neutrophils,
many dead macrophages, necrotic tissue that has
been degraded by proteases, and tissue fluid,
often in a cavity formed at the inflammatory site
• Over days and weeks it is absorbed into the
surrounding tissue and lymph and disappears
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Eosinophils
• Eosinophils are weak phagocytes and exhibit
chemotaxis
• Particularly important in defense against parasites
• Can adhere to parasites and release substances
that kill them (hydrolases, reactive oxygen
species, major basic protein)
• Also accumulate in tissues affected by allergies,
perhaps in response to eosinophil chemotactic
factor from basophils (eosinophils may detoxify
some products of basophils)
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Basophils
• Similar to mast cells adjacent to capillaries
– both cell types release heparin
• Basophils and mast cells both release histamine,
bradykinin, and serotonin
• When IgE bound to receptors on their surfaces is cross-
linked by its specific antigen, mast cells and basophils
degranulate, releasing…
– histamine, bradykinin, serotonin, heparin, leukotrienes, and
several lysosomal enzymes
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Leukopenia
• Leukopenia, or low white blood cell count, is usually the
result of reduced production of cells by the bone marrow
• It can allow clinically severe infections with organisms
that are not usually pathogenic
• Within two days of bone marrow shutdown mucous
membrane ulcers or respiratory infection may occur
• Causes: radiation, chemical toxins, some medicines
• In most cases marrow precursors can reconstitute normal
blood cell counts with proper support
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Leukemias
• Uncontrolled production of abnormal white blood cells
due to a genetic mutation
• Clonal, lineage-specific, often immature cells
• Leukemias are…
– Lymphocytic vs. myelogenous
– Acute vs. chronic (sometimes up to 10-20 years)
• Leukemias with partially differentiated cells may be
classified as neutrophilic, eosinophilic, basophilic, or
monocytic leukemias
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Clinical Effects of Leukemias
• Growth of leukemic cells in abnormal sites
• Invasion of bone from the marrow, with pathologic
fractures
• Eventually spreads to vascular and lymphatic
“filters”… spleen, lymph nodes, liver, other organs
• Replacement of normal bone marrow, resulting in
infection, and bleeding
• Wasting because of metabolic demands
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
You might also like
- 1Q Reviewer General Biology 1Document9 pages1Q Reviewer General Biology 1Ruby May Regala100% (9)
- Chapter 34 - HemaDocument32 pagesChapter 34 - HemaNicole Amado CabahugNo ratings yet
- Resistance of The Body To Infection: Maria Verena R. Remudaro, MDDocument69 pagesResistance of The Body To Infection: Maria Verena R. Remudaro, MDRen AlvNo ratings yet
- Resistance To InfectionDocument94 pagesResistance To Infectionvergel john ErciaNo ratings yet
- Lecture 7-2Document33 pagesLecture 7-2Emmanuel Thon MadingNo ratings yet
- WBCs Chap 2Document119 pagesWBCs Chap 2Hoor ul Ain RamzanNo ratings yet
- WBCDocument25 pagesWBCcelecosibNo ratings yet
- 10.1 Lines of DefenseDocument17 pages10.1 Lines of DefenseMarites LammaoNo ratings yet
- Presentation 3Document24 pagesPresentation 3mahambadar786No ratings yet
- 16 Nonspecific Immune Response S17Document31 pages16 Nonspecific Immune Response S17Mohammed R.HusseinNo ratings yet
- ImmunologyDocument22 pagesImmunologynaumenabafukhaintsaNo ratings yet
- Leukocytes: (White Blood Cells)Document41 pagesLeukocytes: (White Blood Cells)syed nomanshahNo ratings yet
- UNIT 1 ImmunologyDocument82 pagesUNIT 1 ImmunologySivarama KrishnanNo ratings yet
- Innate ImmunityDocument32 pagesInnate ImmunityYik sNo ratings yet
- Lecture Note For Colleges of Health Technology by - M.A. JiyaDocument21 pagesLecture Note For Colleges of Health Technology by - M.A. JiyaDaniel DendaNo ratings yet
- Leukocytes, Granulocytes, The Monocyte-Macrophage System, and InflammationDocument10 pagesLeukocytes, Granulocytes, The Monocyte-Macrophage System, and InflammationShi no MeNo ratings yet
- Cells of The Immune SystemDocument28 pagesCells of The Immune SystemWei Zhu100% (3)
- DR - Gold Immunology NotesDocument11 pagesDR - Gold Immunology NotesAaron PhuaNo ratings yet
- Blood Composition and Plasma and Immune SystemDocument16 pagesBlood Composition and Plasma and Immune SystemFeranmi AkinboboyeNo ratings yet
- Innate ImmunityDocument29 pagesInnate ImmunityAsad MirzaNo ratings yet
- Imune System & Imune Response: Eka Yunita AmnaDocument67 pagesImune System & Imune Response: Eka Yunita AmnaVita R NatansNo ratings yet
- ImmunologyDocument7 pagesImmunologyMatsiri ImmanuelNo ratings yet
- PHS 221 Blood CellsDocument26 pagesPHS 221 Blood Cellsmetasynthronos748No ratings yet
- Immune System: Basic ImmunityDocument16 pagesImmune System: Basic ImmunityvicmomNo ratings yet
- Reticulo-Endothelial SystemDocument32 pagesReticulo-Endothelial Systemrabiatahir421No ratings yet
- Immune System: Basic ImmunityDocument14 pagesImmune System: Basic ImmunityPLANARIANo ratings yet
- B1. Cells OAA TrilogyDocument2 pagesB1. Cells OAA Trilogypixoxis263No ratings yet
- Biology Grade 9 and 10 Revision Short NotesDocument17 pagesBiology Grade 9 and 10 Revision Short Notesdawitdesta2022No ratings yet
- 3 LeukocytesDocument48 pages3 LeukocytesSabra MamjiNo ratings yet
- 3-17 Microbes Major GroupsDocument11 pages3-17 Microbes Major GroupsTanay PanjaNo ratings yet
- Inmunidad Innata ActorDocument50 pagesInmunidad Innata ActorBreen PhNo ratings yet
- Immune System PhysiologyDocument61 pagesImmune System PhysiologyBalasubramaniyan ReshmaNo ratings yet
- Blood: Types of Blood Cells and Their Average NumberDocument32 pagesBlood: Types of Blood Cells and Their Average NumberSumayya KabeerNo ratings yet
- Lecture 6 - MKDocument13 pagesLecture 6 - MKkaran hatkarNo ratings yet
- SME - 11 ImmunityDocument31 pagesSME - 11 Immunitykisepe6738No ratings yet
- 1 Introduction To Immunity and Overview of The Immune SystemDocument30 pages1 Introduction To Immunity and Overview of The Immune Systemshe.dil.oneNo ratings yet
- Dokumen PDF 4Document29 pagesDokumen PDF 4Arbella VeronickaNo ratings yet
- Blood Ii: Dr. Nindya Aryanty, M.Med - EdDocument31 pagesBlood Ii: Dr. Nindya Aryanty, M.Med - EdSiti RahmahNo ratings yet
- Introduction To ImmunologyDocument40 pagesIntroduction To ImmunologysylviahkamandaniNo ratings yet
- Leukocytes (WBCS) : Drsallama Hamid Consultant Lecturer DoctorDocument5 pagesLeukocytes (WBCS) : Drsallama Hamid Consultant Lecturer DoctorAhmed Ali AssafNo ratings yet
- Immunity NewDocument19 pagesImmunity NewdhahamnahNo ratings yet
- Chap1 Transport Form5Document107 pagesChap1 Transport Form5Nurul HusnaNo ratings yet
- Immune OrgansDocument49 pagesImmune OrgansdenyqueronoNo ratings yet
- General Anatomy of The Immune SystemDocument29 pagesGeneral Anatomy of The Immune Systemrambabs369100% (2)
- Hem QuizDocument38 pagesHem QuizRaneem AljuhaniNo ratings yet
- Biology Paper 1 Summary 2023Document108 pagesBiology Paper 1 Summary 2023Maria ThomasNo ratings yet
- 6 Connective TissueDocument109 pages6 Connective TissueAesthetics MinNo ratings yet
- Innate Immunity and Ocular Barrir DefenseDocument38 pagesInnate Immunity and Ocular Barrir DefenseJessica TieuNo ratings yet
- Medical Microbiology Anesthesia Lecture 2Document39 pagesMedical Microbiology Anesthesia Lecture 2Ubaid KhanNo ratings yet
- Medical Microbiology Anesthesia Lecture 2Document39 pagesMedical Microbiology Anesthesia Lecture 2Ubaid KhanNo ratings yet
- Connective TissueDocument109 pagesConnective TissueShin BoyceNo ratings yet
- Physiology Summary Chapter 33Document5 pagesPhysiology Summary Chapter 33gail018100% (1)
- 2.1 RESISTANCE OF THE BODY TO INFECTION I Leukocytes GranulocytesDocument40 pages2.1 RESISTANCE OF THE BODY TO INFECTION I Leukocytes GranulocytesGeevee Naganag VentulaNo ratings yet
- White Blood Cells (WBCS) : Total Leukocyte Count (TLC)Document7 pagesWhite Blood Cells (WBCS) : Total Leukocyte Count (TLC)Sharan MurugaboopathyNo ratings yet
- Inate or Natural ImmunityDocument18 pagesInate or Natural ImmunityYIKI ISAACNo ratings yet
- Circulatory System - Blood: Al-Farabi Kazakh National University Higher School of MedicineDocument35 pagesCirculatory System - Blood: Al-Farabi Kazakh National University Higher School of MedicineDevaDharshiniNo ratings yet
- LECTURE 1 HANDOUT Online ImmuneDocument28 pagesLECTURE 1 HANDOUT Online ImmuneFYMNo ratings yet
- Reticuloendothe Lial SystemDocument15 pagesReticuloendothe Lial Systemrekha dehariyaNo ratings yet
- Macrophage, Functions, Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandMacrophage, Functions, Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- (Class 8) MicroorganismsDocument3 pages(Class 8) MicroorganismsSnigdha GoelNo ratings yet
- Crop Diseases and Insect PestsDocument51 pagesCrop Diseases and Insect PestsChiamaka NwaguNo ratings yet
- Dna Repair: By:Saurabh Kumar Sharma M.SC Biotechnology 2 SemesterDocument17 pagesDna Repair: By:Saurabh Kumar Sharma M.SC Biotechnology 2 SemesterSaurabh SharmaNo ratings yet
- (The Multiple Choice Question in Psychiatry Series) Gin Malhi - MCQs For The MRCPsych - Part 2 - Basic Sciences-CRC Press (1999)Document108 pages(The Multiple Choice Question in Psychiatry Series) Gin Malhi - MCQs For The MRCPsych - Part 2 - Basic Sciences-CRC Press (1999)mubzNo ratings yet
- Obama's REAL Kenyan Birth Certificate SurfacedDocument32 pagesObama's REAL Kenyan Birth Certificate SurfacedPUNISHMENT POSSENo ratings yet
- DPP-01 - Cell The Unit of Life CORRECTEDDocument3 pagesDPP-01 - Cell The Unit of Life CORRECTEDSiazzzNo ratings yet
- Immunology ExamDocument9 pagesImmunology ExamNICHOLAS KAUMBANo ratings yet
- Recent Progress in The Regeneration of Spinal Cord Injuries by Induced Pluripotent Stem CellsDocument13 pagesRecent Progress in The Regeneration of Spinal Cord Injuries by Induced Pluripotent Stem CellsEdison HernandezNo ratings yet
- Introduction To CytogeneticsDocument31 pagesIntroduction To CytogeneticsVia Gail CanlasNo ratings yet
- Chapter 2 History of MicrobiologyDocument39 pagesChapter 2 History of MicrobiologyChristian AbordoNo ratings yet
- Assignment-1 Genetics 341Document4 pagesAssignment-1 Genetics 341damionsimmons10No ratings yet
- Nature of Symbiosis in Oral DiseaseDocument4 pagesNature of Symbiosis in Oral DiseaseDavid NohNo ratings yet
- Caracterização Da Enzima Bifuncional BioDA Envolvida Na Síntese de Biotina e Patogenicidade em Aspergillus FlavusDocument11 pagesCaracterização Da Enzima Bifuncional BioDA Envolvida Na Síntese de Biotina e Patogenicidade em Aspergillus FlavusRenan Guilherme de Oliveira GuihNo ratings yet
- Septic Arthritis - 2 Main Groups of Septic: Gonoccocal and Non Gonocca: NO BACK PAIN, AND HLA B27 (REACTING ARTHRITIS)Document3 pagesSeptic Arthritis - 2 Main Groups of Septic: Gonoccocal and Non Gonocca: NO BACK PAIN, AND HLA B27 (REACTING ARTHRITIS)raNo ratings yet
- Polyethylene Glycol Precipitation For Recovery of Pathogenic VirusDocument6 pagesPolyethylene Glycol Precipitation For Recovery of Pathogenic VirusYoNo ratings yet
- Exam in Microbiology and Parasitology I CDocument3 pagesExam in Microbiology and Parasitology I CJoycee Bo100% (2)
- Physiology of LiverDocument97 pagesPhysiology of LiverRatna Praveen100% (1)
- Pharmacologyonline 3: 107-117 (2009) Alang Et AlDocument53 pagesPharmacologyonline 3: 107-117 (2009) Alang Et Almaia halleNo ratings yet
- Management of Bleeding in Dentistry NewDocument59 pagesManagement of Bleeding in Dentistry NewAnushriya DuttaNo ratings yet
- Para QuizDocument5 pagesPara QuizEricsson CarabbacanNo ratings yet
- NCM 112-Mod5Document6 pagesNCM 112-Mod5Samantha BolanteNo ratings yet
- Blood Tube Collection GuideDocument365 pagesBlood Tube Collection GuideFeliciadlT100% (1)
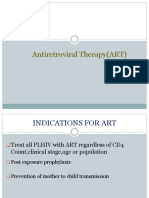
- Antiretroviral Therapy (ART)Document41 pagesAntiretroviral Therapy (ART)Ashik Jithu JohnNo ratings yet
- Microbial Diseases of The Respiratory SystemDocument6 pagesMicrobial Diseases of The Respiratory SystemJohn Daemer Halasan KinocNo ratings yet
- Almustaqbal University Collage Department Semester Exam./ 1 Attempt Sample: Subject: Human Biology Code: Max. Time: 2 H. Class: First DateDocument3 pagesAlmustaqbal University Collage Department Semester Exam./ 1 Attempt Sample: Subject: Human Biology Code: Max. Time: 2 H. Class: First DateZainab HasanNo ratings yet
- 1.1 Mrs Gren and ClassificationDocument3 pages1.1 Mrs Gren and ClassificationsamNo ratings yet
- Ceftriaxone SodiumDocument3 pagesCeftriaxone SodiumjohannakatebellyNo ratings yet
- Catalase TestDocument2 pagesCatalase TestsekaralingamNo ratings yet
- Spontaneous Mutation: Genetically Modified OrganismsDocument7 pagesSpontaneous Mutation: Genetically Modified OrganismsYE Wondwossen ANo ratings yet
- CFTDocument9 pagesCFTWad Kafouri100% (1)