Professional Documents
Culture Documents
Scholars Practicum Poster
Scholars Practicum Poster
Uploaded by
api-549309955Copyright:
Available Formats
You might also like
- 3 Free CelpipDocument20 pages3 Free CelpipMaDeline Rosario100% (3)
- Self - Care Deficit Theory of NursingDocument20 pagesSelf - Care Deficit Theory of NursingAudi Kyle Saydoven100% (2)
- Reflection Paper For Module 2Document2 pagesReflection Paper For Module 2Allan Jr Pancho100% (13)
- Levinas DissertationDocument299 pagesLevinas DissertationEmeth Cordovero100% (2)
- Spilker TaxIndivBusEnt2019 WMDocument1,276 pagesSpilker TaxIndivBusEnt2019 WMablay logeneNo ratings yet
- 2020 NBEC Respectful Maternity CareDocument20 pages2020 NBEC Respectful Maternity CareCece JohnsonNo ratings yet
- Week 10 Vulnerable PopulationsDocument44 pagesWeek 10 Vulnerable PopulationsMohd ArifNo ratings yet
- WGS.151 Gender, Health, & Society: Professor Brittany CharltonDocument22 pagesWGS.151 Gender, Health, & Society: Professor Brittany Charltongonzalezpedro774No ratings yet
- Symptom Management Guidelines: Care of Malignant WoundsDocument7 pagesSymptom Management Guidelines: Care of Malignant WoundsPatrico Rillah Setiawan100% (1)
- ID: Oral 045: Evidence of Less Blame and More Acceptance of Obesity As A Medical Condition Among U.S. AdultsDocument22 pagesID: Oral 045: Evidence of Less Blame and More Acceptance of Obesity As A Medical Condition Among U.S. AdultsCurso Completo AromaterapiaNo ratings yet
- Ortega - Implicit Bias in MedicineDocument4 pagesOrtega - Implicit Bias in Medicinepass4neilNo ratings yet
- Evaluating The Cosmetic PatientDocument71 pagesEvaluating The Cosmetic Patientdocrubes50No ratings yet
- Erik Erikson: - Virginia Johnson - December 16, 2020 - Psy 332 - Personality - Professor Shantelle JacobsDocument13 pagesErik Erikson: - Virginia Johnson - December 16, 2020 - Psy 332 - Personality - Professor Shantelle JacobsVirginia J.No ratings yet
- Considering Inclusion in Research: An Introduction To Scientific and Policy PerspectivesDocument17 pagesConsidering Inclusion in Research: An Introduction To Scientific and Policy Perspectivessaad nNo ratings yet
- Quantitative Research, MULTIDISCIPLINARYDocument25 pagesQuantitative Research, MULTIDISCIPLINARYSharlet BalacuitNo ratings yet
- In The Name of The Almighty: Epidemiology Definition Epidemiology DefinitionDocument13 pagesIn The Name of The Almighty: Epidemiology Definition Epidemiology DefinitionAliNo ratings yet
- Musser Guest Lecture PresentationDocument25 pagesMusser Guest Lecture Presentationapi-488924847No ratings yet
- Introduction To BioethicsDocument49 pagesIntroduction To BioethicsGlai zaNo ratings yet
- Fundamentals of Nursing Practice: de Jesus, M.BDocument12 pagesFundamentals of Nursing Practice: de Jesus, M.BBetina De Jesus0% (1)
- Infographic - Research EthicsDocument1 pageInfographic - Research EthicsScribdTranslationsNo ratings yet
- This Again - Managing The Weight of Moral Distress LGG JWDocument17 pagesThis Again - Managing The Weight of Moral Distress LGG JWapi-136237609No ratings yet
- Cornel 28 May 2017 Bioethics For Dummies NIPT Gene Editing ESHGDocument35 pagesCornel 28 May 2017 Bioethics For Dummies NIPT Gene Editing ESHGSyahputraWibowoNo ratings yet
- Bioethical IssuesDocument22 pagesBioethical IssuesALYSSA NICOLE GINESNo ratings yet
- Theory-Informed Interventions: University of Michigan School of Public HealthDocument16 pagesTheory-Informed Interventions: University of Michigan School of Public HealthRobinNo ratings yet
- Examples of StressorsDocument1 pageExamples of StressorsOlivia SalvadorNo ratings yet
- Aging RehabilitationDocument35 pagesAging RehabilitationdrsonuchawlaNo ratings yet
- Ethics in Technical Communication PDFDocument28 pagesEthics in Technical Communication PDFPanasheNo ratings yet
- Illness Script Formation in Diagnostic Reasoning Within Advanced Practice Nursing EducationDocument28 pagesIllness Script Formation in Diagnostic Reasoning Within Advanced Practice Nursing EducationJOSE ALBERTO KENYO RIOFRIO PALACIOSNo ratings yet
- MITWGS 151S16 Week2Document61 pagesMITWGS 151S16 Week2gonzalezpedro774No ratings yet
- Nursing ProcessDocument70 pagesNursing Processsarhang talebaniNo ratings yet
- 9.1 - Dr. Tiar PIT IDIDocument40 pages9.1 - Dr. Tiar PIT IDINur RachmawatiNo ratings yet
- Dissecting Republic Act No. 10354: Medical & Public Health IssuesDocument50 pagesDissecting Republic Act No. 10354: Medical & Public Health IssuesaizaNo ratings yet
- TOK Ethics - Genetically Modified Babies (Designer BabiesDocument16 pagesTOK Ethics - Genetically Modified Babies (Designer Babiesiwolfie1050% (2)
- Integration of Kangaroo Mother Care in Health Systems: A Systematic Review of Barriers and EnablersDocument39 pagesIntegration of Kangaroo Mother Care in Health Systems: A Systematic Review of Barriers and EnablersNurafifah JackNo ratings yet
- Moral Distress LGGDocument17 pagesMoral Distress LGGapi-136237609No ratings yet
- Ethics of Genetics InaSHG MSHGDocument25 pagesEthics of Genetics InaSHG MSHGdesy armalinaNo ratings yet
- Literature Review PresentationDocument12 pagesLiterature Review PresentationTrinity HuttNo ratings yet
- Askep Remaja KOMUNITAS 2017Document32 pagesAskep Remaja KOMUNITAS 2017kholisNo ratings yet
- Consolidated RH Bill HB4244Document44 pagesConsolidated RH Bill HB4244Dr. Liza ManaloNo ratings yet
- E C: D H C D: Nsnared by Olorblindness Iscourse On Ealth Are IsparitiesDocument6 pagesE C: D H C D: Nsnared by Olorblindness Iscourse On Ealth Are IsparitiesOmar HassenNo ratings yet
- EthicsDocument2 pagesEthicsdaffny10No ratings yet
- Practice: Health Care Problems of Lesbian, Gay, Bisexual, and Transgender PatientsDocument6 pagesPractice: Health Care Problems of Lesbian, Gay, Bisexual, and Transgender PatientsAris DaooNo ratings yet
- NCM 117 - MidtermsDocument9 pagesNCM 117 - MidtermsSherlyn LopezNo ratings yet
- Pt BipolardisorderDocument24 pagesPt Bipolardisorderlove77lifeNo ratings yet
- Chapter - 1 - Cultural Competence in Health Care-Overview of IssuesDocument24 pagesChapter - 1 - Cultural Competence in Health Care-Overview of Issueskimberly barringerNo ratings yet
- Anorexia Nervosa Literature Review PosterDocument1 pageAnorexia Nervosa Literature Review Posterapi-664836263No ratings yet
- Part II. Chief Guide in Abnormal PsychologyDocument41 pagesPart II. Chief Guide in Abnormal PsychologyAvyNo ratings yet
- Week 3 - Preconception (Lecture1) - 4Document24 pagesWeek 3 - Preconception (Lecture1) - 4BoltNo ratings yet
- Chap 6 - Stereotyping, Prejudice and DiscriminationDocument71 pagesChap 6 - Stereotyping, Prejudice and DiscriminationAzra KhanNo ratings yet
- Concept MapDocument1 pageConcept MapSheryl Ann Barit PedinesNo ratings yet
- Module 4 Assignment PosterDocument1 pageModule 4 Assignment PosterChelsie Rachelle BrownNo ratings yet
- Module 5 Health Belief, Healing Trad.Document18 pagesModule 5 Health Belief, Healing Trad.samrasahluNo ratings yet
- History NursingDocument31 pagesHistory Nursinganon_877103538No ratings yet
- GDR Gender Equity and Indigenous Women Health AmericasDocument31 pagesGDR Gender Equity and Indigenous Women Health Americasclaudia jocelyn velazquez ortegaNo ratings yet
- Maternal Health Programs: Monitoring and EvaluationDocument48 pagesMaternal Health Programs: Monitoring and Evaluationvikas takNo ratings yet
- Katharine KolcabaDocument4 pagesKatharine KolcabaimmajinbuxoxoNo ratings yet
- Justice, Ethnicity, and HealthcareDocument7 pagesJustice, Ethnicity, and HealthcareChristopherLeeNo ratings yet
- Session 7 - Ethical DilemmasDocument24 pagesSession 7 - Ethical DilemmasTRYPHONE zabronNo ratings yet
- Genetic Counselling: Lecturer Dept. of Psychiatric Nursing Sajjalashree Institute of Nursing Sciences, Navanagar-BagalkotDocument14 pagesGenetic Counselling: Lecturer Dept. of Psychiatric Nursing Sajjalashree Institute of Nursing Sciences, Navanagar-Bagalkottuppadb50% (2)
- EthicsDocument28 pagesEthicsabcdNo ratings yet
- Gene Editing: Bikash Gupta Shashwat Sinha Hul 371 - Science Technolgy & SocietyDocument20 pagesGene Editing: Bikash Gupta Shashwat Sinha Hul 371 - Science Technolgy & SocietyBikashGuptaNo ratings yet
- Late-Stage Dementia: Promoting Comfort, Compassion, and CareFrom EverandLate-Stage Dementia: Promoting Comfort, Compassion, and CareNo ratings yet
- Black Woman HEAL Thy Self: Obtain Your Ideal Level of Wellbeing Your WayFrom EverandBlack Woman HEAL Thy Self: Obtain Your Ideal Level of Wellbeing Your WayNo ratings yet
- Article Teyl Habiib MaulanaaDocument7 pagesArticle Teyl Habiib MaulanaaHabib Maulana OnceNo ratings yet
- Reporting Student LearningDocument6 pagesReporting Student LearningKip PygmanNo ratings yet
- Amendmentcircularr 201317Document77 pagesAmendmentcircularr 201317api-245897450No ratings yet
- Performance Testing of A Multi-Layer Biomass Briquette StoveDocument959 pagesPerformance Testing of A Multi-Layer Biomass Briquette StoveOBAJA GOBAINo ratings yet
- Huduma Namba Data Capture ToolsDocument2 pagesHuduma Namba Data Capture ToolsThe Star Kenya100% (4)
- Module 3 - RWS Patterns of DevelopmentDocument5 pagesModule 3 - RWS Patterns of DevelopmentJayya BaldoNo ratings yet
- SOLO Taxonomy: PrestructuralDocument3 pagesSOLO Taxonomy: PrestructuralDjelisa ArapaNo ratings yet
- GERIZALDocument6 pagesGERIZAL123r12f1No ratings yet
- Tpack Framework Challenges and Opportunities in Ef PDFDocument22 pagesTpack Framework Challenges and Opportunities in Ef PDFJojames GaddiNo ratings yet
- University of Santo Tomas Faculty of Arts and LettersDocument14 pagesUniversity of Santo Tomas Faculty of Arts and LettersKhaiye De Asis AggabaoNo ratings yet
- Unpacking of Competencies English 5 Quarter 2 Week 1 Content Retained Merged DroppedDocument2 pagesUnpacking of Competencies English 5 Quarter 2 Week 1 Content Retained Merged DroppedJoanne IcoNo ratings yet
- Losoff Haley Resume 2024Document2 pagesLosoff Haley Resume 2024api-736612890No ratings yet
- Eritrea Profile 05122018Document8 pagesEritrea Profile 05122018erimediaNo ratings yet
- Environmental Science PDFDocument2 pagesEnvironmental Science PDFEris OhNo ratings yet
- DLL Math 8Document5 pagesDLL Math 8Janet Aban Otana100% (1)
- FINAL PROJECT PolDocument18 pagesFINAL PROJECT PolmahuaNo ratings yet
- Description of The 4 Primary TemperamentsDocument1 pageDescription of The 4 Primary TemperamentshalyncaeonNo ratings yet
- TOK IntroductionDocument22 pagesTOK IntroductionAkweri OyunguNo ratings yet
- Lindsay Anderson-2Document3 pagesLindsay Anderson-2api-236365296No ratings yet
- CASTELÃO, Tereza. Kuhn-and-Bachelard PDFDocument9 pagesCASTELÃO, Tereza. Kuhn-and-Bachelard PDFDavid VelanesNo ratings yet
- Microcomputer Systems The 8086 8088 Family Architecture PDFDocument26 pagesMicrocomputer Systems The 8086 8088 Family Architecture PDFpalcon fury33% (3)
- IELTS Speaking Evaluation TemplateDocument4 pagesIELTS Speaking Evaluation TemplateruthNo ratings yet
- Faculty Development - EvaluationDocument1 pageFaculty Development - EvaluationEmi YunzalNo ratings yet
- 2011-Ross and Revilla-Minaya - Cognitive Studies in Ethnobiology What Can We Learn About The Mind As Well As Human Environmental InteractionDocument16 pages2011-Ross and Revilla-Minaya - Cognitive Studies in Ethnobiology What Can We Learn About The Mind As Well As Human Environmental InteractionwernerbhNo ratings yet
- Physical-Education-12 CBSEDocument381 pagesPhysical-Education-12 CBSEArnavNo ratings yet
- Course Outline in Assessment 1 and Principle 2Document14 pagesCourse Outline in Assessment 1 and Principle 2Benjie Moronia Jr.No ratings yet
Scholars Practicum Poster
Scholars Practicum Poster
Uploaded by
api-549309955Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Scholars Practicum Poster
Scholars Practicum Poster
Uploaded by
api-549309955Copyright:
Available Formats
Medical Racism: Tackling
Implicit Bias in Maternal Care
Kaelyn Carter
kcarter3@umd.edu
Global Public Health Scholars Program
Public Health Science
Introduction
Fieldwork Site
In maternal care, there seems to be dire problem.
41.7% (per 100,000 live births) of black women are
• CPSP359S (Research)
dying during maternity/labor. This is the highest race
• FMSC110S, SPHL260, CPGH classes (prior
of women with maternal morbidity.
Of these deaths, most of the causes are issues knowledge)
• UMD Counseling Center (interviews)
that could have been prevented (i.e., hemorrhage,
infection/sepsis). This raises the question of why is
this happening and why is the black women the
prime victim of this?
With this becoming an issue amongst celebrities
Public Health Implication
as well (i.e., Serena Williams), the most reasonable
cause seems to be implicit bias in the medical field. • Implicit bias in maternal care stems from racist
past
Picture of UMD’s Counseling Center. It is within the Shoemaker Building. • Marion J. Sims
• Idea of “pain”
Study Design Future Solutions to Explore • Invasive research of the black body
• Research • Difficult to determine due to racial history
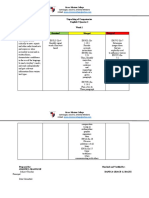
• Socio-economic model • Black women’s attitude towards physicians
• Expert’s work with implicit bias
• Organization level to target Physicians’ bias
• The past of medical advancements in
• Medical school curriculum, Workplace • Implicit bias is hard to distinguish among others
gynecology
• Black women’s perspective on doctors and yourself
• Unconsciously thinking and acting
• Extremely dangerous for physicians
Public Policy
• Federal and state non-
discriminatory laws
Community
• Built environment
• Cultural norms/values
Organizational
• College
• Medical School
• Workplace
Interpersonal
• Family showing bias
• Friends
• Environment of
upbringing
Individual
• attitudes or beliefs that
support bias
• History of showing bias
Figure 1. Socio-economic model.
Figure 2. Graph showing the discrepancy in maternal care.
Acknowledgments References
Bair, Barbara, and Susan E Cayleff. 1993. Wings of Gauze : Women of Color and the Experience of Health and Illness. Detroit: Wayne State University
A special thank you to Dr. Marring, Reva, Gislaine, Haley, and the Press.
“Pregnancy Mortality Surveillance System,” November 25, 2020. https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-
whole GPH Program!! surveillance-system.htm.
Sims, J. Marion, H Marion-Sims, and Joseph Meredith Toner Collection. The Story of My Life. New York, D. Appleton and company, 1884. Web..
https://lccn.loc.gov/13017881.
Washington, Harriet A. 2006. Medical Apartheid : The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present.
I also wanted to thank Professor Eubanks for helping me along my 1st ed. New York: Doubleday.
White, Augustus A, and David Chanoff. 2011. Seeing Patients : Unconscious Bias in Health Care. Cambridge, Massachusetts: Harvard University Press.
journey with this research!! https://umaryland.on.worldcat.org/search?databaseList=&queryString=seeing+unconscious&umdlib=#/oclc/726742563
You might also like
- 3 Free CelpipDocument20 pages3 Free CelpipMaDeline Rosario100% (3)
- Self - Care Deficit Theory of NursingDocument20 pagesSelf - Care Deficit Theory of NursingAudi Kyle Saydoven100% (2)
- Reflection Paper For Module 2Document2 pagesReflection Paper For Module 2Allan Jr Pancho100% (13)
- Levinas DissertationDocument299 pagesLevinas DissertationEmeth Cordovero100% (2)
- Spilker TaxIndivBusEnt2019 WMDocument1,276 pagesSpilker TaxIndivBusEnt2019 WMablay logeneNo ratings yet
- 2020 NBEC Respectful Maternity CareDocument20 pages2020 NBEC Respectful Maternity CareCece JohnsonNo ratings yet
- Week 10 Vulnerable PopulationsDocument44 pagesWeek 10 Vulnerable PopulationsMohd ArifNo ratings yet
- WGS.151 Gender, Health, & Society: Professor Brittany CharltonDocument22 pagesWGS.151 Gender, Health, & Society: Professor Brittany Charltongonzalezpedro774No ratings yet
- Symptom Management Guidelines: Care of Malignant WoundsDocument7 pagesSymptom Management Guidelines: Care of Malignant WoundsPatrico Rillah Setiawan100% (1)
- ID: Oral 045: Evidence of Less Blame and More Acceptance of Obesity As A Medical Condition Among U.S. AdultsDocument22 pagesID: Oral 045: Evidence of Less Blame and More Acceptance of Obesity As A Medical Condition Among U.S. AdultsCurso Completo AromaterapiaNo ratings yet
- Ortega - Implicit Bias in MedicineDocument4 pagesOrtega - Implicit Bias in Medicinepass4neilNo ratings yet
- Evaluating The Cosmetic PatientDocument71 pagesEvaluating The Cosmetic Patientdocrubes50No ratings yet
- Erik Erikson: - Virginia Johnson - December 16, 2020 - Psy 332 - Personality - Professor Shantelle JacobsDocument13 pagesErik Erikson: - Virginia Johnson - December 16, 2020 - Psy 332 - Personality - Professor Shantelle JacobsVirginia J.No ratings yet
- Considering Inclusion in Research: An Introduction To Scientific and Policy PerspectivesDocument17 pagesConsidering Inclusion in Research: An Introduction To Scientific and Policy Perspectivessaad nNo ratings yet
- Quantitative Research, MULTIDISCIPLINARYDocument25 pagesQuantitative Research, MULTIDISCIPLINARYSharlet BalacuitNo ratings yet
- In The Name of The Almighty: Epidemiology Definition Epidemiology DefinitionDocument13 pagesIn The Name of The Almighty: Epidemiology Definition Epidemiology DefinitionAliNo ratings yet
- Musser Guest Lecture PresentationDocument25 pagesMusser Guest Lecture Presentationapi-488924847No ratings yet
- Introduction To BioethicsDocument49 pagesIntroduction To BioethicsGlai zaNo ratings yet
- Fundamentals of Nursing Practice: de Jesus, M.BDocument12 pagesFundamentals of Nursing Practice: de Jesus, M.BBetina De Jesus0% (1)
- Infographic - Research EthicsDocument1 pageInfographic - Research EthicsScribdTranslationsNo ratings yet
- This Again - Managing The Weight of Moral Distress LGG JWDocument17 pagesThis Again - Managing The Weight of Moral Distress LGG JWapi-136237609No ratings yet
- Cornel 28 May 2017 Bioethics For Dummies NIPT Gene Editing ESHGDocument35 pagesCornel 28 May 2017 Bioethics For Dummies NIPT Gene Editing ESHGSyahputraWibowoNo ratings yet
- Bioethical IssuesDocument22 pagesBioethical IssuesALYSSA NICOLE GINESNo ratings yet
- Theory-Informed Interventions: University of Michigan School of Public HealthDocument16 pagesTheory-Informed Interventions: University of Michigan School of Public HealthRobinNo ratings yet
- Examples of StressorsDocument1 pageExamples of StressorsOlivia SalvadorNo ratings yet
- Aging RehabilitationDocument35 pagesAging RehabilitationdrsonuchawlaNo ratings yet
- Ethics in Technical Communication PDFDocument28 pagesEthics in Technical Communication PDFPanasheNo ratings yet
- Illness Script Formation in Diagnostic Reasoning Within Advanced Practice Nursing EducationDocument28 pagesIllness Script Formation in Diagnostic Reasoning Within Advanced Practice Nursing EducationJOSE ALBERTO KENYO RIOFRIO PALACIOSNo ratings yet
- MITWGS 151S16 Week2Document61 pagesMITWGS 151S16 Week2gonzalezpedro774No ratings yet
- Nursing ProcessDocument70 pagesNursing Processsarhang talebaniNo ratings yet
- 9.1 - Dr. Tiar PIT IDIDocument40 pages9.1 - Dr. Tiar PIT IDINur RachmawatiNo ratings yet
- Dissecting Republic Act No. 10354: Medical & Public Health IssuesDocument50 pagesDissecting Republic Act No. 10354: Medical & Public Health IssuesaizaNo ratings yet
- TOK Ethics - Genetically Modified Babies (Designer BabiesDocument16 pagesTOK Ethics - Genetically Modified Babies (Designer Babiesiwolfie1050% (2)
- Integration of Kangaroo Mother Care in Health Systems: A Systematic Review of Barriers and EnablersDocument39 pagesIntegration of Kangaroo Mother Care in Health Systems: A Systematic Review of Barriers and EnablersNurafifah JackNo ratings yet
- Moral Distress LGGDocument17 pagesMoral Distress LGGapi-136237609No ratings yet
- Ethics of Genetics InaSHG MSHGDocument25 pagesEthics of Genetics InaSHG MSHGdesy armalinaNo ratings yet
- Literature Review PresentationDocument12 pagesLiterature Review PresentationTrinity HuttNo ratings yet
- Askep Remaja KOMUNITAS 2017Document32 pagesAskep Remaja KOMUNITAS 2017kholisNo ratings yet
- Consolidated RH Bill HB4244Document44 pagesConsolidated RH Bill HB4244Dr. Liza ManaloNo ratings yet
- E C: D H C D: Nsnared by Olorblindness Iscourse On Ealth Are IsparitiesDocument6 pagesE C: D H C D: Nsnared by Olorblindness Iscourse On Ealth Are IsparitiesOmar HassenNo ratings yet
- EthicsDocument2 pagesEthicsdaffny10No ratings yet
- Practice: Health Care Problems of Lesbian, Gay, Bisexual, and Transgender PatientsDocument6 pagesPractice: Health Care Problems of Lesbian, Gay, Bisexual, and Transgender PatientsAris DaooNo ratings yet
- NCM 117 - MidtermsDocument9 pagesNCM 117 - MidtermsSherlyn LopezNo ratings yet
- Pt BipolardisorderDocument24 pagesPt Bipolardisorderlove77lifeNo ratings yet
- Chapter - 1 - Cultural Competence in Health Care-Overview of IssuesDocument24 pagesChapter - 1 - Cultural Competence in Health Care-Overview of Issueskimberly barringerNo ratings yet
- Anorexia Nervosa Literature Review PosterDocument1 pageAnorexia Nervosa Literature Review Posterapi-664836263No ratings yet
- Part II. Chief Guide in Abnormal PsychologyDocument41 pagesPart II. Chief Guide in Abnormal PsychologyAvyNo ratings yet
- Week 3 - Preconception (Lecture1) - 4Document24 pagesWeek 3 - Preconception (Lecture1) - 4BoltNo ratings yet
- Chap 6 - Stereotyping, Prejudice and DiscriminationDocument71 pagesChap 6 - Stereotyping, Prejudice and DiscriminationAzra KhanNo ratings yet
- Concept MapDocument1 pageConcept MapSheryl Ann Barit PedinesNo ratings yet
- Module 4 Assignment PosterDocument1 pageModule 4 Assignment PosterChelsie Rachelle BrownNo ratings yet
- Module 5 Health Belief, Healing Trad.Document18 pagesModule 5 Health Belief, Healing Trad.samrasahluNo ratings yet
- History NursingDocument31 pagesHistory Nursinganon_877103538No ratings yet
- GDR Gender Equity and Indigenous Women Health AmericasDocument31 pagesGDR Gender Equity and Indigenous Women Health Americasclaudia jocelyn velazquez ortegaNo ratings yet
- Maternal Health Programs: Monitoring and EvaluationDocument48 pagesMaternal Health Programs: Monitoring and Evaluationvikas takNo ratings yet
- Katharine KolcabaDocument4 pagesKatharine KolcabaimmajinbuxoxoNo ratings yet
- Justice, Ethnicity, and HealthcareDocument7 pagesJustice, Ethnicity, and HealthcareChristopherLeeNo ratings yet
- Session 7 - Ethical DilemmasDocument24 pagesSession 7 - Ethical DilemmasTRYPHONE zabronNo ratings yet
- Genetic Counselling: Lecturer Dept. of Psychiatric Nursing Sajjalashree Institute of Nursing Sciences, Navanagar-BagalkotDocument14 pagesGenetic Counselling: Lecturer Dept. of Psychiatric Nursing Sajjalashree Institute of Nursing Sciences, Navanagar-Bagalkottuppadb50% (2)
- EthicsDocument28 pagesEthicsabcdNo ratings yet
- Gene Editing: Bikash Gupta Shashwat Sinha Hul 371 - Science Technolgy & SocietyDocument20 pagesGene Editing: Bikash Gupta Shashwat Sinha Hul 371 - Science Technolgy & SocietyBikashGuptaNo ratings yet
- Late-Stage Dementia: Promoting Comfort, Compassion, and CareFrom EverandLate-Stage Dementia: Promoting Comfort, Compassion, and CareNo ratings yet
- Black Woman HEAL Thy Self: Obtain Your Ideal Level of Wellbeing Your WayFrom EverandBlack Woman HEAL Thy Self: Obtain Your Ideal Level of Wellbeing Your WayNo ratings yet
- Article Teyl Habiib MaulanaaDocument7 pagesArticle Teyl Habiib MaulanaaHabib Maulana OnceNo ratings yet
- Reporting Student LearningDocument6 pagesReporting Student LearningKip PygmanNo ratings yet
- Amendmentcircularr 201317Document77 pagesAmendmentcircularr 201317api-245897450No ratings yet
- Performance Testing of A Multi-Layer Biomass Briquette StoveDocument959 pagesPerformance Testing of A Multi-Layer Biomass Briquette StoveOBAJA GOBAINo ratings yet
- Huduma Namba Data Capture ToolsDocument2 pagesHuduma Namba Data Capture ToolsThe Star Kenya100% (4)
- Module 3 - RWS Patterns of DevelopmentDocument5 pagesModule 3 - RWS Patterns of DevelopmentJayya BaldoNo ratings yet
- SOLO Taxonomy: PrestructuralDocument3 pagesSOLO Taxonomy: PrestructuralDjelisa ArapaNo ratings yet
- GERIZALDocument6 pagesGERIZAL123r12f1No ratings yet
- Tpack Framework Challenges and Opportunities in Ef PDFDocument22 pagesTpack Framework Challenges and Opportunities in Ef PDFJojames GaddiNo ratings yet
- University of Santo Tomas Faculty of Arts and LettersDocument14 pagesUniversity of Santo Tomas Faculty of Arts and LettersKhaiye De Asis AggabaoNo ratings yet
- Unpacking of Competencies English 5 Quarter 2 Week 1 Content Retained Merged DroppedDocument2 pagesUnpacking of Competencies English 5 Quarter 2 Week 1 Content Retained Merged DroppedJoanne IcoNo ratings yet
- Losoff Haley Resume 2024Document2 pagesLosoff Haley Resume 2024api-736612890No ratings yet
- Eritrea Profile 05122018Document8 pagesEritrea Profile 05122018erimediaNo ratings yet
- Environmental Science PDFDocument2 pagesEnvironmental Science PDFEris OhNo ratings yet
- DLL Math 8Document5 pagesDLL Math 8Janet Aban Otana100% (1)
- FINAL PROJECT PolDocument18 pagesFINAL PROJECT PolmahuaNo ratings yet
- Description of The 4 Primary TemperamentsDocument1 pageDescription of The 4 Primary TemperamentshalyncaeonNo ratings yet
- TOK IntroductionDocument22 pagesTOK IntroductionAkweri OyunguNo ratings yet
- Lindsay Anderson-2Document3 pagesLindsay Anderson-2api-236365296No ratings yet
- CASTELÃO, Tereza. Kuhn-and-Bachelard PDFDocument9 pagesCASTELÃO, Tereza. Kuhn-and-Bachelard PDFDavid VelanesNo ratings yet
- Microcomputer Systems The 8086 8088 Family Architecture PDFDocument26 pagesMicrocomputer Systems The 8086 8088 Family Architecture PDFpalcon fury33% (3)
- IELTS Speaking Evaluation TemplateDocument4 pagesIELTS Speaking Evaluation TemplateruthNo ratings yet
- Faculty Development - EvaluationDocument1 pageFaculty Development - EvaluationEmi YunzalNo ratings yet
- 2011-Ross and Revilla-Minaya - Cognitive Studies in Ethnobiology What Can We Learn About The Mind As Well As Human Environmental InteractionDocument16 pages2011-Ross and Revilla-Minaya - Cognitive Studies in Ethnobiology What Can We Learn About The Mind As Well As Human Environmental InteractionwernerbhNo ratings yet
- Physical-Education-12 CBSEDocument381 pagesPhysical-Education-12 CBSEArnavNo ratings yet
- Course Outline in Assessment 1 and Principle 2Document14 pagesCourse Outline in Assessment 1 and Principle 2Benjie Moronia Jr.No ratings yet