Professional Documents
Culture Documents
Journal Reading: Residen: Dr. Dewi S. Wahyuningtias Trainee: Dr. Abdul Haris M, SP.B Konsultan: Dr. Suwardjo, SP.B (Onk)
Journal Reading: Residen: Dr. Dewi S. Wahyuningtias Trainee: Dr. Abdul Haris M, SP.B Konsultan: Dr. Suwardjo, SP.B (Onk)
Uploaded by
dewiswahyu0 ratings0% found this document useful (0 votes)
29 views22 pagesThis study analyzed data from over 5,800 patients in Japan who underwent thyroidectomy for thyroid cancer between 2014-2017. The study aimed to investigate the risk of postoperative recurrent laryngeal nerve paralysis (RLNP) with and without the use of intraoperative nerve monitoring (IONM). The results showed that the overall incidence of postoperative RLNP was 2.2% and IONM use was not associated with RLNP in the primary multivariate analysis when adjusting for factors like age, tumor size, and surgery type. However, subgroup analyses found IONM was associated with higher RLNP rates for patients with more advanced T4 tumors or N1b nodal involvement.
Original Description:
Original Title
maju onko
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis study analyzed data from over 5,800 patients in Japan who underwent thyroidectomy for thyroid cancer between 2014-2017. The study aimed to investigate the risk of postoperative recurrent laryngeal nerve paralysis (RLNP) with and without the use of intraoperative nerve monitoring (IONM). The results showed that the overall incidence of postoperative RLNP was 2.2% and IONM use was not associated with RLNP in the primary multivariate analysis when adjusting for factors like age, tumor size, and surgery type. However, subgroup analyses found IONM was associated with higher RLNP rates for patients with more advanced T4 tumors or N1b nodal involvement.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
29 views22 pagesJournal Reading: Residen: Dr. Dewi S. Wahyuningtias Trainee: Dr. Abdul Haris M, SP.B Konsultan: Dr. Suwardjo, SP.B (Onk)
Journal Reading: Residen: Dr. Dewi S. Wahyuningtias Trainee: Dr. Abdul Haris M, SP.B Konsultan: Dr. Suwardjo, SP.B (Onk)
Uploaded by
dewiswahyuThis study analyzed data from over 5,800 patients in Japan who underwent thyroidectomy for thyroid cancer between 2014-2017. The study aimed to investigate the risk of postoperative recurrent laryngeal nerve paralysis (RLNP) with and without the use of intraoperative nerve monitoring (IONM). The results showed that the overall incidence of postoperative RLNP was 2.2% and IONM use was not associated with RLNP in the primary multivariate analysis when adjusting for factors like age, tumor size, and surgery type. However, subgroup analyses found IONM was associated with higher RLNP rates for patients with more advanced T4 tumors or N1b nodal involvement.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 22
Journal Reading
Residen: dr. Dewi S. Wahyuningtias
Trainee: dr. Abdul Haris M, Sp.B
Konsultan: dr. Suwardjo, Sp.B (onk)
• The recurrent laryngeal nerve (RLN) is located close to the thyroid gland
and is the main nerve that controls vocal-fold mobility.
• Recurrent laryngeal nerve paralysis (RLNP) is one of the major morbidities
following thyroidectomy; it results in dysphonia and dysphagia in cases of
• unilateral paralysis and can be associated with airway distress and require
tracheostomy in cases of bilateral RLNP.
• Permanent postoperative RLNP occurs in approximately 0.8% to 1.0% of
cases, whereas transient paralysis occurs in 2.2% to 8.0% of cases.
• It has also been reported that following surgeries for thyroid cancer in
particular, the RLNP rate (6.5%) was higher than the average rate (4.37%)
following surgeries for all kinds of thyroid disease.
• Intraoperative nerve monitoring (IONM) was introduced to assist with
identification of the RLN during thyroidectomy. it has been reported that
IONM is used during approximately 80% of thyroid surgeries performed by
head and neck surgeons and >50% of surgeries performed by general
surgeons.
• the utility of IONM is dependent on thyroid tumor size or the extent of
cancer invasion has not yet been determined.
• this study aimed to investigate the risk of postoperative RLNP with and
Data Source
• This retrospective cohort study utilized data from the Diagnosis Procedure
Combination inpatient database maintained by Medical Data Vision Co., Ltd. (Tokyo,
Japan).
• The database includes 297 facilities, which represent approximately 18% of the acute-
care hospitals in Japan. The database contains anonymous information from health
insurance claims submitted by approximately 18 million patients from April 2008 to
2017. It contains information pertaining to patient characteristics (e.g., age and sex),
diagnostic information (e.g., dates of diagnoses and disease codes, which were
recorded in accordance with the codes from the International Classification of
Diseases, Tenth Revision [ICD- 10]), and medical care provided (e.g., prescriptions,
laboratory tests, interventional procedures such as surgery, and dates of medical care).
• This study was approved by the Kyoto University Graduate School and Faculty of
Medicine Ethics Committee (R1261), following the STROBE statement guidelines.
• This need for obtaining individual informed patient consent was waived because this
study was a secondary analysis of an anonymous patient database.
Study Cohort
• We extracted data for patients age ≥20 years with thyroid
cancer who underwent thyroidectomy between April 1, 2014—
when use of IONM during thyroid cancer surgery initially began
being covered by health insurance in Japan—to May 31, 2017.
• These patients were identified by the Japanese procedure code
for thyroidectomy for malignant tumors (K463).
• We excluded patients with diagnostic codes indicating the
existence of RLNP before the index surgery (ICD-10: J380, G522,
or G978); those who underwent other head and neck surgeries,
radiation therapy, or parathyroid surgery before the index
surgery; and patients who had reoperations for thyroid cancer.
Independent Variables
• The primary exposure variable was the use of IONM (procedure code
K930) during thyroid cancer surgery.
• Additionally, we extracted the following patient data from the
database: sex, age, thyroid cancer tumor and nodal classifications
based on the seventh edition of the Union for International Cancer
Control–American Joint Committee on Cancer staging system,14 the
type of thyroid cancer surgery (lobectomy or total thyroidectomy),
performance of neck dissection (codes K000 and K469), presence of
underlying autoimmune thyroid disease (e.g., chronic thyroiditis or
Graves’ disease) defined as having the relevant diagnostic codes
before the day of the index surgery (ICD-10: E039, E050, E055, E059,
E063), the annual volume of thyroid cancer surgeries performed in
each facility, and the year in which the index surgery was performed.
Outcomes
• The primary outcome was the occurrence of
postoperative RLNP. We defined postoperative RLNP
as having the relevant diagnostic codes from the
day of the index surgery to 30 days after the index
surgery. To distinguish postoperative paralysis
• from paralysis caused by other surgery and
recurrence, the period was limited to 30 days
postoperatively.
Statistical Analysis
• The characteristics of the study population were summarized
using proportions for categorical variables and the median
and standard deviation for continuous variables.
• We compared relevant variables between patients who
underwent surgery with and without the use of IONM
• The Student t test and Fisher exact test were used for
continuous variables and categorical variables, respectively.
The variables compared included patient characteristics (age,
sex, and thyroid cancer tumor and nodal classifications),
procedural data (type of surgery and neck dissection),
postoperative outcomes (RLNP), the annual volume of thyroid
cancer surgeries performed in each facility, and the year in
which the index surgery was performed.
• We used the Fisher exact test to compare the rate of postoperative RLNP with IONM use, age,
sex, tumor classification, nodal classification, the type of surgery, neck dissection, surgery
volume of each facility, and the year in which the index surgery was performed.
• We performed multivariable logistic regression analyses to evaluate the association between
IONM use and postoperative RLNP, adjusting for potential confounders based on clinical
points of view (e.g., age, sex, tumor classification, nodal classification, the type of surgery,
and surgery volume of each facility).
• The results were expressed as odds ratios (OR) with 95% confidence intervals (CI).
• We conducted sensitivity analyses by changing one of the adjusting confounders of the
multivariable logistic regression analyses, nodal classification, to “neck dissection.”
• The neck dissection code in the database indicates that neck dissection was performed in
both the central and lateral compartments; however, neck dissection that was performed in
only the central compartment was not included due to the Japanese insurance system.
Moreover, we changed the period for including RLNP as having the relevant diagnostic codes
from 30 days after the index surgery to 60 days after the index surgery.
• Furthermore, we conducted subgroup analyses to investigate whether the utility of IONM
differed according to the tumor and nodal classifications.
• All statistical tests were two-sided; P < .05 was considered statistically significant. All data
analyses were performed using SAS for Windows (version 9.4; SAS Institute Inc., Cary, NC).
RESULTS
• From a multihospital claims database, we identified
6,359 patients who underwent thyroid cancer surgery
between April 1, 2014, and May 31, 2017. Of these, we
excluded 555 patients: 340 who were diagnosed with
RLNP before the index surgery, 59 who had undergone
thyroid cancer surgery before the index surgery, and
156 who had previously undergone other head and neck
cancer surgery, radiation therapy for head and neck
cancer, or parathyroid surgery (Fig. 1). Consequently,
5,804 patients were included in the study cohort.
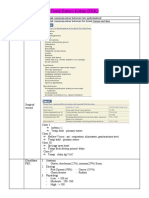
Univariate Comparison of Patient
• Characteristics and Postoperative RLNP
• Incidence
• Table I presents the demographic and baseline clinical
• characteristics of the study patients. IONM was used during thyroid
cancer surgery for 849 patients, accounting for 14.6% of the study
cohort.
• Postoperative RLNP was reported in 127 cases (2.2%); in most cases, it
was unclear whether the paralysis was unilateral or bilateral. Between
the patients who underwent surgery with and without the use of
IONM, the incidence of postoperative RLNP did not differ significantly
(Table II). In the patients with T4 tumor classification and N1b nodal
classification, postoperative RLNP occurred more frequently in the
patients who underwent IONM.
Multivariable Analyses
• Upon performing the multivariable logistic regression analysis,
we excluded 1,027 patients with missing tumor classification
data and 92 with missing nodal classification data.
• The multivariable analysis also indicated that use of IONM
during thyroid cancer surgery was not associated with
postoperative RLNP after adjusting for confounding factors
(OR: 1.13, 95% CI: 0.66-1.94; Table III).
• Meanwhile, advanced age (OR: 1.31 per 10 years, 95% CI:
1.12-1.51) and T4 tumor classification (OR: 2.31, 95% CI: 1.18-
4.52) were independently associated with higher incidences of
postoperative RLNP.
Sensitivity Analyses
• The subgroup analyses revealed that among patients
having T1, T2, or T3 tumor classifications, use of IONM
was not significantly associated with postoperative RLNP;
whereas among patients with tumors classified as T4, use
of IONM was associated with an increased incidence of
postoperative RLNP (Table IV). Subgroup analyses
stratified by nodal classification revealed that among
patients having N0 and N1a classifications, use of IONM
was not significantly associated with RLNP; but among
patients having an N1b classification, IONM use was
associated with an increased incidence of RLNP (Table V).
• In the multivariate model including neck dissection
(instead of nodal classification), the results were
similar to those of the primary analysis (Table VI) in
that use of IONM was not significantly associated
with postoperative RLNP.
• The factors that exhibited significant associations
with RLNP in the multivariate model included older
age, having had a total thyroidectomy, and having T4
tumor classification.
• Despite the change in the period for including RLNP
with the relevant diagnostic codes from 30 days after
the index surgery to 60 days after the index surgery,
the occurrence of RLNP did not change.
DISCUSSION
• In this observational cohort study, we investigated the association between
the use of IONM during thyroid cancer surgery and postoperative RLNP
using a nationwide claims database.
• We observed no significant association between IONM use and
postoperative RLNP. Our subgroup analyses demonstrated that among
patients with thyroid cancer classified as T4 or N1b, IONM use was
significantly associated with an increased incidence of postoperative RLNP.
• Many previous studies have examined the benefits of using IONM to reduce
the risk of postoperative RLNP; however, the results were inconsistent. Some
studies demonstrated a decreased risk of postoperative RLNP with the use
of IONM, and others observed a similar risk of RLNP regardless of IONM
use.2–5,8,9 In these previous studies, the patient populations included a
mixture of
• those having benign and malignant diseases. We hypothesized that the utility of IONM may
differ between cases of cancer and benign diseases; thus, we focused on patients with
thyroid cancer in the present study. In this regard, one recently conducted meta-analysis that
pooled the data of 595 patients with thyroid cancer from four different studies found that
there was no evidence to support IONM use to reduce postoperative RLNP. However, the
authors of this meta-analysis indicated that the sample size was small, suggesting the need
for a large-scalestudy. Furthermore, primary lesions and lymph node metastasis should be
considered risk factors for RLNP, because the completeness of surgical resection is an
important determinant of outcome in extracapsular thyroid cancer,15 and patients
undergoing central neck dissection have a significantly higher incidence of RLNP compared
with patients who do not undergo central neck dissection.16 Therefore, we hypothesized that
tumor size and the extent of invasion may affect the utility of IONM, and thereby performed
subgroup analyses according to tumor classification and the presence of lymph node
metastasis.
• Unexpectedly, in the subgroup analysis of the T4 and N1b groups, IONM use was significantly
associated with an increased incidence of postoperative RLNP. We assumed that IONM may
be used more frequently in difficult-to-manage cases, such as those in which the cancer had
invaded the recurrent laryngeal nerve, or by operators with less surgical experience. The
possibility of indication bias could be considered; however, such bias is difficult to measure,
and conducting a randomized controlled trial is the only way to control for this bias.
• We used a multihospital claims database to ensure that we obtained a large study sample.
Although we analyzed the data of 5,804 patients, the present study may still be
underpowered due to the low incidence of postoperative RLNP (n = 127).2–4,10 A meta-
analysis targeting both benign and malignant thyroid diseases that included
• 17,203 at-risk nerves demonstrated the benefits of using IONM to reduce the risk of RLNP,
but there was no statistical significance for persistent RLNP.5 Studies with larger sample sizes
may be needed to reflect a statistically significant difference for persistent RLNP, but it is
questionable whether such studies seeking “statistical significance” rather than “clinical
significance” will change the overall value of IONM.17
• There are three possible mechanisms of RLN injury that can occur during thyroidectomy:
excessive traction on the RLN; compression of the RLN by a ligature, clamp, pickup forceps,
retractor, or tissue band; or direct injury to the RLN by sharp transection or thermal injury.18
Excessive traction and compression are difficult to recognize intraoperatively by visual
identification alone. Recently, continuous IONM of the RLN has gained increasing interest as it
provides real-time feedback to surgeons to potentially avoid RLN injuries.
• Conventional IONM is intermittent and cannot provide continuous functional protection
during nonstimulation periods19; therefore, surgeons using intermittent IONM are not able
to detect excessive traction or compression during nonstimulation periods. This may be one
of the reasons why the protective effects of IONM against RLNP have not been observed in
some studies. In Japan, continuous IONM has been available since 2016; thus, in our study,
intermittent IONM probably accounted for the majority of cases wherein IONM was
performed.
• Further studies are needed to evaluate whether continuous IONM provides superior
protective effects compared with intermittent IONM or direct visualization alone.5 There
were several limitations of this study that should be considered. First, cases of RLNP without
diagnostic codes could not be identified. The accuracy of the diagnostic codes for RLNP in the
database was unknown; thus, it is possible that the occurrence of
• postoperative RLNP was underestimated. However, we anticipated that the degree of RLNP
underestimation was nondifferential between patients having had surgeries with and without
use of IONM. Thus, it is unlikely that our finding—the similar incidence of RLNP between the
two groups—was significantly affected by underestimation of RLNP. Second, it was unclear in
most cases whether RLNP had occurred bilaterally or unilaterally.
• Only 11% (14/127) of the postoperative RLNP cases could be differentiated as being bilateral or
unilateral. The clinical courses are considerably different for unilateral versus bilateral cases of
RLNP, and it may be important to distinguish between unilateral and bilateral cases, but this
could not be achieved in our study.
• Although our study did not observe any benefit of IONM use, the possibility remains that it may
prevent bilateral RLNP, a severe form of nerve palsy. Third, we could not determine whether
RLNP was transient or permanent in the included cases, as the database does not contain
information regarding the long-term outcomes of RLNP.
• Fourth, central neck dissection may be one of the factors associated with an increased risk of
RLNP, but we were unable to identify whether central neck dissection was performed for patients
with N0 nodal classification. Some N0 patients may have undergone prophylactic central neck
dissection, but not all. In the database, we could identify the code for “neck dissection,” but this
did not include cases of neck dissection performed only in the central compartment. Finally,
there were unmeasured confounding factors in this study, such as multiple operators and facility
traits, other than the hospitals’ annual surgery volumes. Surgical techniques may vary between
operators, which may affect the incidence of RLNP. Furthermore, the affordability and adaptation
of IONM may vary between facilities. Therefore, these factors could affect the frequency of use
of IONM and the occurrence of RLNP.
You might also like
- Step 2 CK BibleDocument435 pagesStep 2 CK Biblewilksebas100% (13)
- DD-110 110HFDocument290 pagesDD-110 110HFsergioNo ratings yet
- New American Paintings - December-January, 2019Document180 pagesNew American Paintings - December-January, 2019Fabio Nagual100% (2)
- Cho Et Al., 2014Document8 pagesCho Et Al., 2014NyomantrianaNo ratings yet
- Completion Thyroidectomy: Predicting Bilateral Disease: Originalresearcharticle Open AccessDocument7 pagesCompletion Thyroidectomy: Predicting Bilateral Disease: Originalresearcharticle Open AccessRadita Dwihaning PutriNo ratings yet
- K. Ueta Et Al.2019Document6 pagesK. Ueta Et Al.2019Mai M. AlshalNo ratings yet
- Bongiolatti 2019Document10 pagesBongiolatti 2019Alin Ionut BurlacuNo ratings yet
- Oncologic Outcomes of Robotic Thyroidectomy: 5-Year Experience With Propensity Score MatchingDocument8 pagesOncologic Outcomes of Robotic Thyroidectomy: 5-Year Experience With Propensity Score MatchingmawarmelatiNo ratings yet
- Presenter: DR Muthulingesh, SR-RO Moderator: DR Shyama Prem, ProfessorDocument51 pagesPresenter: DR Muthulingesh, SR-RO Moderator: DR Shyama Prem, ProfessorGousalyaNo ratings yet
- Clinical StudyDocument7 pagesClinical StudyMeriam MalindaNo ratings yet
- Predictive Value of Nodal Metastases On Local Recurrence in The Management of Differentiated Thyroid Cancer. Retrospective Clinical StudyDocument6 pagesPredictive Value of Nodal Metastases On Local Recurrence in The Management of Differentiated Thyroid Cancer. Retrospective Clinical StudyuqbaNo ratings yet
- Delta Neutrophil Index and Neutrophil-to-Lymphocyte Ratio in The Differentiation of Thyroid Malignancy and Nodular GoiterDocument8 pagesDelta Neutrophil Index and Neutrophil-to-Lymphocyte Ratio in The Differentiation of Thyroid Malignancy and Nodular GoiteragusNo ratings yet
- 2017 Article 1126Document6 pages2017 Article 1126roel_04No ratings yet
- Nej Mo A 1414882Document9 pagesNej Mo A 1414882Corina Hagiu-RaduNo ratings yet
- Needle Tract Implantation Following Fine-Needle Aspiration of Thyroid CancerDocument7 pagesNeedle Tract Implantation Following Fine-Needle Aspiration of Thyroid Cancersalman khanNo ratings yet
- In - Vivo 35 3483Document6 pagesIn - Vivo 35 3483juan uribeNo ratings yet
- Readmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsDocument9 pagesReadmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsbobNo ratings yet
- Thyroid Cancer-Full Article Corrected 'Discussion' Part. (1417)Document8 pagesThyroid Cancer-Full Article Corrected 'Discussion' Part. (1417)PARVEZ AHMEDNo ratings yet
- Tiefeng Cao 2015Document9 pagesTiefeng Cao 2015elenamihaelavrabieNo ratings yet
- Otolaryngology ComplicacionDocument7 pagesOtolaryngology ComplicacionYuriko Castro SanchezNo ratings yet
- Kanker ParuDocument10 pagesKanker Parunovi hidayahNo ratings yet
- RAZOR TrialDocument35 pagesRAZOR TrialankitNo ratings yet
- Maju Jurnal Onko 2Document34 pagesMaju Jurnal Onko 2Yunita SaraswatiNo ratings yet
- s10147 020 01632 XDocument7 pagess10147 020 01632 X363331272No ratings yet
- Current Practice of Surgery For Benign GoitreDocument10 pagesCurrent Practice of Surgery For Benign GoitreazharbattooNo ratings yet
- Laparoscopic-Assisted Versus Open Surgery For Colorectal Cancer: Short-And Long-Term Outcomes ComparisonDocument7 pagesLaparoscopic-Assisted Versus Open Surgery For Colorectal Cancer: Short-And Long-Term Outcomes ComparisonRegina SeptianiNo ratings yet
- Significance of Nuclear Morphometry in Cytological Aspirates of Breast MassesDocument48 pagesSignificance of Nuclear Morphometry in Cytological Aspirates of Breast MassesRajni ChattarajNo ratings yet
- Erectile Function After Partial Penectomy For Penile CancerDocument8 pagesErectile Function After Partial Penectomy For Penile CancerTai rascunhos TaiNo ratings yet
- Primary Surgery Versus Chemoradiotherapy For Advanced Oropharyngeal Cancers: A Longitudinal Population StudyDocument7 pagesPrimary Surgery Versus Chemoradiotherapy For Advanced Oropharyngeal Cancers: A Longitudinal Population StudyLuvita Amallia SyadhatinNo ratings yet
- Neutrophil-To-Lymphocyte Ratio Is A Prognostic Factor For Colon Cancer: A Propensity Score AnalysisDocument8 pagesNeutrophil-To-Lymphocyte Ratio Is A Prognostic Factor For Colon Cancer: A Propensity Score AnalysisDini AuliaNo ratings yet
- Clinical Neurology and Neurosurgery: Preservation of Olfaction in Surgery of Olfactory Groove MeningiomasDocument5 pagesClinical Neurology and Neurosurgery: Preservation of Olfaction in Surgery of Olfactory Groove MeningiomasBhayu RizallinoorNo ratings yet
- Dream 2020Document4 pagesDream 2020Karlito Dela CruzNo ratings yet
- Risk Factors and Prognosis of IB IIB Cervical Carcinoma With Common Iliac Lymph Node MetastasisDocument5 pagesRisk Factors and Prognosis of IB IIB Cervical Carcinoma With Common Iliac Lymph Node MetastasisGrace Noviyanthi SinambelaNo ratings yet
- P. Wang Et Al.2019Document6 pagesP. Wang Et Al.2019Mai M. AlshalNo ratings yet
- Bacciu 2013Document10 pagesBacciu 2013AshokNo ratings yet
- P1 Functional Outcomes and Health-Related QualityDocument11 pagesP1 Functional Outcomes and Health-Related Qualityernitaranterupang79No ratings yet
- JR Onkologi Bedah Kepala LeherDocument21 pagesJR Onkologi Bedah Kepala LeherRina DesdwiNo ratings yet
- Prognostic Significance of Neutrophil-to-Lymphocyte Ratio and PLRDocument9 pagesPrognostic Significance of Neutrophil-to-Lymphocyte Ratio and PLRdominguezmariela465No ratings yet
- Jurnal CNFDocument36 pagesJurnal CNFAndrianorMuhammadNo ratings yet
- Medicina: Hemithyroidectomy For Thyroid Cancer: A ReviewDocument12 pagesMedicina: Hemithyroidectomy For Thyroid Cancer: A ReviewaisyahNo ratings yet
- Long-Term Outcomes of Primary Endoscopic Resection Vs Surgery For T1Document16 pagesLong-Term Outcomes of Primary Endoscopic Resection Vs Surgery For T1ellya zalfaNo ratings yet
- 2018 Article 6554Document8 pages2018 Article 6554Raíla SoaresNo ratings yet
- Ajr 05 0936Document7 pagesAjr 05 0936ChavdarNo ratings yet
- Journal CaDocument7 pagesJournal CaNiniek Putri SujiwaNo ratings yet
- The Effect of Season of Operation On The Survival of Patients With Resected Non-Small Cell Lung CancerDocument5 pagesThe Effect of Season of Operation On The Survival of Patients With Resected Non-Small Cell Lung CancerDaniel AriasNo ratings yet
- Hta Versus IncidentalomaDocument10 pagesHta Versus IncidentalomaClaudia IrimieNo ratings yet
- International Ovarian Tumor Analysis (IOTA)Document19 pagesInternational Ovarian Tumor Analysis (IOTA)VeerSidhuNo ratings yet
- Active Surveillance For Adult Low-Risk Papillary ThyroidDocument15 pagesActive Surveillance For Adult Low-Risk Papillary ThyroidmiguelalmenarezNo ratings yet
- Prognostic Model For Survival of Local Recurrent Nasopharyngeal Carcinoma With Intensity-Modulated RadiotherapyDocument7 pagesPrognostic Model For Survival of Local Recurrent Nasopharyngeal Carcinoma With Intensity-Modulated Radiotherapypp kabsemarangNo ratings yet
- Atm 07 14 323Document9 pagesAtm 07 14 323Ethel GeanNo ratings yet
- Amaros TrialDocument43 pagesAmaros TrialnitinNo ratings yet
- Lectura 2Document10 pagesLectura 2Ricardo Huaman QuirozNo ratings yet
- JURNALDocument6 pagesJURNALPutu erwanNo ratings yet
- UTD 28 11 1634 1640hemaDocument7 pagesUTD 28 11 1634 1640hemappdspkjuli23No ratings yet
- Radiation Oncology: Organizing Pneumonia After Stereotactic Ablative Radiotherapy of The LungDocument19 pagesRadiation Oncology: Organizing Pneumonia After Stereotactic Ablative Radiotherapy of The LungjaccovanmeelNo ratings yet
- Efficacy and Safety of Vismodegib in Patients With Advanced Basal Cell Carcinoma (BCC) : 12-Month Update of The ERIVANCE BCC StudyDocument1 pageEfficacy and Safety of Vismodegib in Patients With Advanced Basal Cell Carcinoma (BCC) : 12-Month Update of The ERIVANCE BCC Studyjuloc34No ratings yet
- Annals Case Reports PDF Final Final.25.05.l22.Document13 pagesAnnals Case Reports PDF Final Final.25.05.l22.rossbar13No ratings yet
- qt5kh1c39r NosplashDocument12 pagesqt5kh1c39r NosplashSusieNo ratings yet
- A Profile of Cervical Cancer Cases in A Government Medical College HospitalDocument6 pagesA Profile of Cervical Cancer Cases in A Government Medical College HospitalIOSRjournalNo ratings yet
- 10 1097@PRS 0000000000002165Document8 pages10 1097@PRS 0000000000002165Rina DelgadoNo ratings yet
- Recurrence Rate of Endometriomas Following A Laparoscopic CystectomyDocument5 pagesRecurrence Rate of Endometriomas Following A Laparoscopic CystectomyPutri Tamara DasantosNo ratings yet
- Therapy Response Imaging in OncologyFrom EverandTherapy Response Imaging in OncologyMizuki NishinoNo ratings yet
- Technical Aspects of Focal Therapy in Localized Prostate CancerFrom EverandTechnical Aspects of Focal Therapy in Localized Prostate CancerEric BarretNo ratings yet
- Kuliah Class Inter IDocument59 pagesKuliah Class Inter IdewiswahyuNo ratings yet
- Dr. Teguh Marfen Djadjakusumah, SP.B, SubspBVE (K) AAA Pit IKABIDocument19 pagesDr. Teguh Marfen Djadjakusumah, SP.B, SubspBVE (K) AAA Pit IKABIdewiswahyuNo ratings yet
- Kuliah Kelainan PayudaraDocument44 pagesKuliah Kelainan PayudaradewiswahyuNo ratings yet
- Kuliah Class Inter 2Document39 pagesKuliah Class Inter 2dewiswahyuNo ratings yet
- Current Concepts of Damage Control Resuscitation and Damage Control SurgeryDocument52 pagesCurrent Concepts of Damage Control Resuscitation and Damage Control SurgerydewiswahyuNo ratings yet
- Callosities, Corns, and Calluses: BMJ Clinical Research July 1996Document5 pagesCallosities, Corns, and Calluses: BMJ Clinical Research July 1996dewiswahyu100% (1)
- 5 DR Nico PPt. PIT IKABI 2022Document45 pages5 DR Nico PPt. PIT IKABI 2022dewiswahyuNo ratings yet
- Breast Recosntruction Flap ProcedureDocument41 pagesBreast Recosntruction Flap ProceduredewiswahyuNo ratings yet
- Grynfeltt-Lesshaft Lumbar Hernia: Sebuah Kasus Wanita 57 Tahun Dengan Benjolan Di Sisi Kanan AbdomenDocument11 pagesGrynfeltt-Lesshaft Lumbar Hernia: Sebuah Kasus Wanita 57 Tahun Dengan Benjolan Di Sisi Kanan AbdomendewiswahyuNo ratings yet
- MATERI SESI 1.3 Dr. Risal Wintoko, SPBDocument36 pagesMATERI SESI 1.3 Dr. Risal Wintoko, SPBdewiswahyuNo ratings yet
- Dr. Warsinggih, SP.B-KBD (SLIDE ERAS in Digestive Surgery)Document34 pagesDr. Warsinggih, SP.B-KBD (SLIDE ERAS in Digestive Surgery)dewiswahyuNo ratings yet
- MATERI SESI 4.1 - MAR DR - HeryDocument9 pagesMATERI SESI 4.1 - MAR DR - HerydewiswahyuNo ratings yet
- DD Billous VomittingDocument2 pagesDD Billous VomittingdewiswahyuNo ratings yet
- Dr. Kuman EARLY TOTAL CARE (ETC) - DAMAGEDocument22 pagesDr. Kuman EARLY TOTAL CARE (ETC) - DAMAGEdewiswahyuNo ratings yet
- Dr. Dedy Pratama, SPB, SubspBVE (K) (Management of Varicose Vein and Chronic Venous Disorders PIT IKABI Lampung 2022 FINAL)Document63 pagesDr. Dedy Pratama, SPB, SubspBVE (K) (Management of Varicose Vein and Chronic Venous Disorders PIT IKABI Lampung 2022 FINAL)dewiswahyuNo ratings yet
- Fistul Entero Kutan (FEK)Document4 pagesFistul Entero Kutan (FEK)dewiswahyuNo ratings yet
- Endoscopic Thyroidectomy IKABIDocument28 pagesEndoscopic Thyroidectomy IKABIdewiswahyu100% (1)
- Dr. Tondi Maspian Tjili, SPBS (K), M.Kes (Advanced Techniques For Minimallu Invasive in Hemorhagic Stroke)Document22 pagesDr. Tondi Maspian Tjili, SPBS (K), M.Kes (Advanced Techniques For Minimallu Invasive in Hemorhagic Stroke)dewiswahyuNo ratings yet
- Truncal Vagotomy - StatPearls - NCBI BookshelfDocument6 pagesTruncal Vagotomy - StatPearls - NCBI BookshelfdewiswahyuNo ratings yet
- CEDERA KEPALA - Bencana - Wawan - PIT IKABI LAMPUNG1Document20 pagesCEDERA KEPALA - Bencana - Wawan - PIT IKABI LAMPUNG1dewiswahyuNo ratings yet
- Neonatal Necrotizing Enterocolitis: Research and Reports in Neonatology DoveDocument15 pagesNeonatal Necrotizing Enterocolitis: Research and Reports in Neonatology DovedewiswahyuNo ratings yet
- Complications After Hemorrhoid surgery-UGMDocument38 pagesComplications After Hemorrhoid surgery-UGMdewiswahyuNo ratings yet
- Maxillofacial TraumaDocument15 pagesMaxillofacial TraumadewiswahyuNo ratings yet
- Trauma Tumpul AbdomenDocument30 pagesTrauma Tumpul AbdomendewiswahyuNo ratings yet
- Current Concept Inguinal Hernia RepairDocument6 pagesCurrent Concept Inguinal Hernia RepairdewiswahyuNo ratings yet
- Indication 4 Wiring RIB FRACTUREDocument13 pagesIndication 4 Wiring RIB FRACTUREdewiswahyuNo ratings yet
- Vascular Injury: Book Reading Dr. RonaldDocument24 pagesVascular Injury: Book Reading Dr. RonalddewiswahyuNo ratings yet
- RES Thoracic Trauma + Pulmonary ContusionDocument33 pagesRES Thoracic Trauma + Pulmonary ContusiondewiswahyuNo ratings yet
- Batu Patofisiologi - Dr. IDWDocument24 pagesBatu Patofisiologi - Dr. IDWdewiswahyuNo ratings yet
- Clubfoot (Congenital Talipes Equinovarus) - Pediatrics - OrthobulletsDocument8 pagesClubfoot (Congenital Talipes Equinovarus) - Pediatrics - OrthobulletsdewiswahyuNo ratings yet
- Vocabulary HSC 22 PDFDocument28 pagesVocabulary HSC 22 PDFMadara Uchiha83% (6)
- Guida Busplan 2003Document31 pagesGuida Busplan 2003cajun28No ratings yet
- 2-1 Basic CT EquipmentDocument35 pages2-1 Basic CT EquipmentAnthony LakpahNo ratings yet
- PosterDocument1 pagePosterSaad Ullah100% (2)
- M.H. Saboo Siddik College of Engineering: CertificateDocument55 pagesM.H. Saboo Siddik College of Engineering: Certificatebhanu jammu100% (1)
- KS3 Africa 5ghanafactsheetDocument3 pagesKS3 Africa 5ghanafactsheetSandy SaddlerNo ratings yet
- Worksheet 1Document7 pagesWorksheet 1ndtitcNo ratings yet
- Picking Manten Tebu' in The Syncretism of The Cembengan Tradition Perspective of Value Education and Urf'-Lila, Siti, Ning FikDocument10 pagesPicking Manten Tebu' in The Syncretism of The Cembengan Tradition Perspective of Value Education and Urf'-Lila, Siti, Ning FiklilaNo ratings yet
- RB Cba Executive Summary 0405Document24 pagesRB Cba Executive Summary 0405pepegrillo891No ratings yet
- Position, Leverage and Opportunity: A Typology of Strategic Logics Linking Resources With Competitive AdvantageDocument16 pagesPosition, Leverage and Opportunity: A Typology of Strategic Logics Linking Resources With Competitive AdvantageEdgar LL.CNo ratings yet
- CH # 4 AudioDocument55 pagesCH # 4 AudioHamza Nazir Hamza NazirNo ratings yet
- Math 241 Section 2.1 (3-2-2021)Document20 pagesMath 241 Section 2.1 (3-2-2021)H ANo ratings yet
- SOLUTION VECTOR ANALYSIS BY S M YUSUF PDF - Are You Looking For Solution VectorDocument6 pagesSOLUTION VECTOR ANALYSIS BY S M YUSUF PDF - Are You Looking For Solution VectorZara Malik67% (3)
- 100 Korean Proverbs With Meanings For TOPIK 2Document19 pages100 Korean Proverbs With Meanings For TOPIK 2Rumah Sakit Bhakti NugrahaNo ratings yet
- Achasta Bear Paw RidgeDocument1 pageAchasta Bear Paw RidgeC Bombin'No ratings yet
- 14386l Camu 11670 Rev34 IngleseDocument253 pages14386l Camu 11670 Rev34 Inglesejohnysonycum0% (1)
- TECHNOLOGY1 Answer-1Document6 pagesTECHNOLOGY1 Answer-1JlkKumarNo ratings yet
- 5070 s17 Ms 31 PDFDocument4 pages5070 s17 Ms 31 PDFAl-Qayyuum T.G1753No ratings yet
- Hughes2007 PDFDocument21 pagesHughes2007 PDFThiago CancianNo ratings yet
- Advanced 250 V Three-Phase BLDC Controller With Embedded STM32 MCUDocument32 pagesAdvanced 250 V Three-Phase BLDC Controller With Embedded STM32 MCUOne SpringNo ratings yet
- JMA-7100 Instruction ManualDocument560 pagesJMA-7100 Instruction ManualViliame D RoqicaNo ratings yet
- Statistical PackagesDocument18 pagesStatistical Packagesannie naeemNo ratings yet
- BURETI - 2016 (RK) Form 4 - Chemistry - 3Document4 pagesBURETI - 2016 (RK) Form 4 - Chemistry - 3Martin KariukiNo ratings yet
- LeeBoy Tack Tank Manual 8 21 06 PDFDocument40 pagesLeeBoy Tack Tank Manual 8 21 06 PDFLuis Miguel Mamani CastroNo ratings yet
- Report Project 2Document12 pagesReport Project 2Fiq IFTNo ratings yet
- Lab 5 - Ring AC DistributorDocument6 pagesLab 5 - Ring AC DistributorMuhammad AnasNo ratings yet
- EgyptDocument5 pagesEgyptLorenz Jedd GuañizoNo ratings yet