Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
26 viewsLarge Intestine CA 2
Large Intestine CA 2
Uploaded by
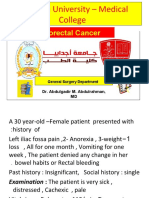
Worku Kifle1. The document summarizes the anatomy, blood supply, lymphatic drainage, staging, signs and symptoms, diagnosis, and treatment of the large intestine and colorectal cancer.
2. Key points include that the large intestine extends from the ileocecal valve to the anus and has distinct layers in its wall. Colorectal cancer most commonly presents after age 50 and symptoms vary depending on tumor location.
3. Staging is based on tumor invasion depth, lymph node involvement, and presence of metastases, and is important for determining prognosis and treatment. Surgery is the main treatment, and chemotherapy may be given post-operatively to reduce cancer recurrence.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You might also like
- Medical Terminology For Health Professions Spiral Bound Version Mindtap Course List 9Th Edition Ehrlich Full ChapterDocument68 pagesMedical Terminology For Health Professions Spiral Bound Version Mindtap Course List 9Th Edition Ehrlich Full Chapterjames.radford791100% (7)
- Colorectal CancerDocument39 pagesColorectal CancerMuvenn Kannan100% (2)
- Nervous System WorksheetDocument8 pagesNervous System WorksheetBeneNo ratings yet
- S6 - Q2 - DLPS - Week 1 To 5Document302 pagesS6 - Q2 - DLPS - Week 1 To 5Dom MartinezNo ratings yet
- Powerpoint: Colorectal Polyps and Colorectal CarcinomaDocument68 pagesPowerpoint: Colorectal Polyps and Colorectal Carcinomaj.doe.hex_87100% (5)
- Colorectal CancerDocument3 pagesColorectal CancerAriane May Rubio50% (2)
- Fast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeFrom EverandFast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeNo ratings yet
- Super SizeCrashCourseDocument61 pagesSuper SizeCrashCourseJitaru Wilkins100% (12)
- Plant Anatomy and Physiology 1Document60 pagesPlant Anatomy and Physiology 1keron100% (1)
- Biology 1: Learning Activity SheetDocument184 pagesBiology 1: Learning Activity SheetJohn joseph Ursulum100% (1)
- Colon: Malueth AbrahamDocument39 pagesColon: Malueth AbrahamMalueth AnguiNo ratings yet
- Colorectal CancerDocument39 pagesColorectal CancerFernando AnibanNo ratings yet
- Gastric CancerDocument126 pagesGastric Cancermwani775100% (1)
- CasediscussionDocument30 pagesCasediscussionFernando AnibanNo ratings yet
- Upper Git TumorsDocument51 pagesUpper Git TumorsIsaac MwangiNo ratings yet
- Colorectal CaDocument24 pagesColorectal CaSA NodeNo ratings yet
- Carcinomagallbladder PDFDocument61 pagesCarcinomagallbladder PDFZaki DhiifNo ratings yet
- Coloncancerlecturenice 170826084151Document81 pagesColoncancerlecturenice 170826084151ckyew64No ratings yet
- Colorectal Ca (CRC) .: Malueth Abraham, MBCHB ViDocument36 pagesColorectal Ca (CRC) .: Malueth Abraham, MBCHB ViMalueth AnguiNo ratings yet
- 9 Gastric NeoplasmsDocument40 pages9 Gastric NeoplasmselshadieNo ratings yet
- Esophageal CarcinomaDocument34 pagesEsophageal Carcinomaapi-19916399100% (1)
- 42 EsophagusDocument49 pages42 EsophagusShiva BhandariNo ratings yet
- Malignancy in GI Tract-DR AgungDocument69 pagesMalignancy in GI Tract-DR AgungwkwkwkhhhhNo ratings yet
- DysphagiaDocument40 pagesDysphagiamanabdebuNo ratings yet
- Ca Colon: Pembimbing Dr. Yanti, SP.B KBDDocument47 pagesCa Colon: Pembimbing Dr. Yanti, SP.B KBDRichard HadinataNo ratings yet
- Lower Gi Case Presentation PDFDocument35 pagesLower Gi Case Presentation PDFapi-448999672No ratings yet
- Colorectal TumoursDocument21 pagesColorectal TumoursRUDOLF YUSON BM20110052No ratings yet
- Esophageal CADocument56 pagesEsophageal CAEdwin OkonNo ratings yet
- SURG - Hepatobiliary, Pancreas, SpleenDocument230 pagesSURG - Hepatobiliary, Pancreas, SpleenJoan Timbol100% (1)
- Colon and Rectal CancerDocument62 pagesColon and Rectal CancerSK TalkNo ratings yet
- Colorectalcancer 200612134444Document80 pagesColorectalcancer 200612134444Elena CaterevNo ratings yet
- CA OesophagusDocument47 pagesCA OesophagusAnsif KNo ratings yet
- Carcinoma Gall BladderDocument25 pagesCarcinoma Gall Bladderrajan kumarNo ratings yet
- CA ColonDocument47 pagesCA ColonrahayuNo ratings yet
- Colorectal CADocument76 pagesColorectal CANur Insyirah100% (2)
- Squamous Cell CarcinomaDocument53 pagesSquamous Cell CarcinomaWacky BlankNo ratings yet
- Management of Colon Cancers-1Document110 pagesManagement of Colon Cancers-1Edwin OkonNo ratings yet
- Colorectal CancerDocument48 pagesColorectal CancerAndre F SusantioNo ratings yet
- Hepatocellular Carcinoma 05Document45 pagesHepatocellular Carcinoma 05tupagalhkya2000No ratings yet
- Hepatocellular Carcinoma and Other Hepatic MassesDocument59 pagesHepatocellular Carcinoma and Other Hepatic MassesIsaac MwangiNo ratings yet
- Lower GIT CancersDocument43 pagesLower GIT CancersIsaac MwangiNo ratings yet
- Carcinoma of ColonDocument39 pagesCarcinoma of ColonMuhammad DaniyalNo ratings yet
- Colon CancerDocument41 pagesColon Cancervaishali TayadeNo ratings yet
- CarcinomarectumDocument45 pagesCarcinomarectumHuzefa MemonNo ratings yet
- Emory Reynolds Program Colon Cancer Resource ModuleDocument45 pagesEmory Reynolds Program Colon Cancer Resource ModulealbertontaolaNo ratings yet
- Case Presentation: by DR SaleemDocument61 pagesCase Presentation: by DR SaleemsandeepNo ratings yet
- Pancreatic TumorDocument28 pagesPancreatic TumorAli AtiaNo ratings yet
- 3.radiation InjDocument9 pages3.radiation Injapi-3829364No ratings yet
- Colon Cancer Vail 2008Document63 pagesColon Cancer Vail 2008SamGoldsteinNo ratings yet
- DDX of RIF Mass (Syazwani)Document44 pagesDDX of RIF Mass (Syazwani)Nurul Syazwani RamliNo ratings yet
- Surgery: Crohn's DiseaseDocument9 pagesSurgery: Crohn's Diseaseapi-3829364No ratings yet
- Carcinoma OesophagusDocument27 pagesCarcinoma Oesophagussammykiilu3No ratings yet
- Paediatric Abdominal MassesDocument73 pagesPaediatric Abdominal Massesg1381821No ratings yet
- Esophageal CancerDocument42 pagesEsophageal Cancerapi-1964133750% (2)
- Small Intestine: Earle J. Niervo Medical ClerkDocument168 pagesSmall Intestine: Earle J. Niervo Medical ClerkEarle Jimenez Niervo RNNo ratings yet
- 8 28 12 R Schaffer MDDocument51 pages8 28 12 R Schaffer MDKay BristolNo ratings yet
- Colorectal CancersDocument162 pagesColorectal CancersSomto NwabuezeNo ratings yet
- Carcinoma Oesophagus: Dr. S. Ranita DeviDocument46 pagesCarcinoma Oesophagus: Dr. S. Ranita DeviVivek AhanthemNo ratings yet
- Rectum: Malueth AbrahamDocument19 pagesRectum: Malueth AbrahamMalueth AnguiNo ratings yet
- Colon CancerDocument5 pagesColon CancerPan Dong100% (1)
- Bladder TumorsDocument36 pagesBladder TumorsMohammad BelbahaithNo ratings yet
- 18 Colorectal Polyps and CarcinomaDocument89 pages18 Colorectal Polyps and Carcinomasuhaib ananzehNo ratings yet
- Malignant Neoplasm of Body of UterusDocument20 pagesMalignant Neoplasm of Body of UterusZahidul ZahidNo ratings yet
- Carcinoma Rectum - Janak - NEWDocument74 pagesCarcinoma Rectum - Janak - NEWTowhidulIslamNo ratings yet
- GIT, CorrectedDocument105 pagesGIT, Correctedali attiaNo ratings yet
- Home Cure for Colon Cancer with Best Natural RemediesFrom EverandHome Cure for Colon Cancer with Best Natural RemediesRating: 5 out of 5 stars5/5 (1)
- Lower Limb Fracture..MeDocument142 pagesLower Limb Fracture..MeWorku KifleNo ratings yet
- LaPlace's LawDocument2 pagesLaPlace's LawWorku KifleNo ratings yet
- Cast/Splint Choice and Application: Worku K. (MD)Document15 pagesCast/Splint Choice and Application: Worku K. (MD)Worku KifleNo ratings yet
- Orofacial CystsDocument84 pagesOrofacial CystsWorku KifleNo ratings yet
- Small Intestine MMCDocument65 pagesSmall Intestine MMCWorku KifleNo ratings yet
- Vitamins: Organic Compounds Required in Minute Quantities Specific Body FunctionsDocument57 pagesVitamins: Organic Compounds Required in Minute Quantities Specific Body FunctionsWorku KifleNo ratings yet
- Maxillary Sinus DR - AssefaDocument65 pagesMaxillary Sinus DR - AssefaWorku KifleNo ratings yet
- Arsi University College of Health Sciences Department of MedicineDocument127 pagesArsi University College of Health Sciences Department of MedicineWorku KifleNo ratings yet
- 6.1. Stool Specimen 6.1. Stool Specimen: 9/18/21 Tafeseb - Tufa 1Document67 pages6.1. Stool Specimen 6.1. Stool Specimen: 9/18/21 Tafeseb - Tufa 1Worku KifleNo ratings yet
- Dentistry HoDocument17 pagesDentistry HoWorku KifleNo ratings yet
- Aseptic Techniques: - Antiseptic or Antimicrobial AgentDocument17 pagesAseptic Techniques: - Antiseptic or Antimicrobial AgentWorku KifleNo ratings yet
- Ped SurgDocument11 pagesPed SurgWorku KifleNo ratings yet
- Ortho: - Orthopedic Instruments - Anatomy and Physiology - FractureDocument2 pagesOrtho: - Orthopedic Instruments - Anatomy and Physiology - FractureWorku KifleNo ratings yet
- Acute Abdomen: - DefinitionDocument27 pagesAcute Abdomen: - DefinitionWorku KifleNo ratings yet
- Neck Masses and FistulasDocument55 pagesNeck Masses and FistulasWorku KifleNo ratings yet
- NEUROFIBROMATOSISDocument11 pagesNEUROFIBROMATOSISWorku KifleNo ratings yet
- Melanoma Belay Z July, 6 2005Document20 pagesMelanoma Belay Z July, 6 2005Worku KifleNo ratings yet
- Abdominal Wall DEFECTS: Omphalocele, Gastroschisis, Prune-BellyDocument38 pagesAbdominal Wall DEFECTS: Omphalocele, Gastroschisis, Prune-BellyWorku KifleNo ratings yet
- Acute Abdomen in ChildrenDocument61 pagesAcute Abdomen in ChildrenWorku KifleNo ratings yet
- Vascular Malformation and LymphoedemaDocument44 pagesVascular Malformation and LymphoedemaWorku KifleNo ratings yet
- Fluid and Electrolte Manageent in Paediatric Surgical PatientDocument29 pagesFluid and Electrolte Manageent in Paediatric Surgical PatientWorku KifleNo ratings yet
- Hypospadias Epispadias and Bladder Exstrophy: Khalid Abdella (MD) OCTOBER - 11 - 2006Document64 pagesHypospadias Epispadias and Bladder Exstrophy: Khalid Abdella (MD) OCTOBER - 11 - 2006Worku KifleNo ratings yet
- Obstruction of The Urinary TractDocument68 pagesObstruction of The Urinary TractWorku KifleNo ratings yet
- Colilithiasis 2Document53 pagesColilithiasis 2Worku KifleNo ratings yet
- Perioperative Care 2Document28 pagesPerioperative Care 2Worku KifleNo ratings yet
- Kaposi's Sarcoma: Patients Seen in The Past 8 Years: 83 CasesDocument12 pagesKaposi's Sarcoma: Patients Seen in The Past 8 Years: 83 CasesWorku KifleNo ratings yet
- Fluid & Electrolyte 2Document47 pagesFluid & Electrolyte 2Worku KifleNo ratings yet
- Melanoma: Meku Damtie (M.D.) July 18, 2006Document38 pagesMelanoma: Meku Damtie (M.D.) July 18, 2006Worku KifleNo ratings yet
- Gastrointestinal Hemorrhage2Document20 pagesGastrointestinal Hemorrhage2Worku KifleNo ratings yet
- Xylem - WikipediaDocument92 pagesXylem - WikipediaBashiir NuurNo ratings yet
- Life Processes - BIO - CLASS 10 - NOTESDocument10 pagesLife Processes - BIO - CLASS 10 - NOTESvaarunisaxenaNo ratings yet
- SBI3U Chapter 10 Self-QuizDocument6 pagesSBI3U Chapter 10 Self-QuizJannette JaneNo ratings yet
- Gynae FCPS 1 Guide-1Document24 pagesGynae FCPS 1 Guide-1Lubna MushtaqNo ratings yet
- SOX Science5 Q2 M2of7Document18 pagesSOX Science5 Q2 M2of7Neil Joy Felomino Basa-LepalemNo ratings yet
- TECH 614 Full Spine I (Castellucci)Document10 pagesTECH 614 Full Spine I (Castellucci)Robert StraubNo ratings yet
- Anti-Coagulant (Vte in Obstetrics) - Madam LiewDocument10 pagesAnti-Coagulant (Vte in Obstetrics) - Madam LiewNana YunusNo ratings yet
- Contoh Case ReportDocument4 pagesContoh Case ReportLyvia ChristieNo ratings yet
- Benign Gynecologic TumorsDocument57 pagesBenign Gynecologic TumorsDexter IanNo ratings yet
- Reflective Journal Mazatul AzrinDocument1 pageReflective Journal Mazatul AzrinNama Saya AtulNo ratings yet
- Feyer 2020 WvngoshawkDocument13 pagesFeyer 2020 WvngoshawkAgnieszka CzujkowskaNo ratings yet
- Developmental Biology of Frog: SpermDocument21 pagesDevelopmental Biology of Frog: SpermRavindra MadurNo ratings yet
- HemoperitoneumDocument36 pagesHemoperitoneumnovitafitri123No ratings yet
- ImmunohematologyDocument38 pagesImmunohematologyNoreenNo ratings yet
- 11th Bio Botany Book Back 1 Mark Questions With Answer Key English Medium - BakDocument6 pages11th Bio Botany Book Back 1 Mark Questions With Answer Key English Medium - BakShriya RameshNo ratings yet
- CS WTDocument5 pagesCS WTYeni PuspitasariNo ratings yet
- ATHENS: Class: 12, Topic: Human ReproductionDocument3 pagesATHENS: Class: 12, Topic: Human ReproductionATHENS MaterialNo ratings yet
- CH 10 Somatic and Special Senses Powerpoint 2006Document175 pagesCH 10 Somatic and Special Senses Powerpoint 2006Maikel PakageNo ratings yet
- Lesson 5. The Structure of The Human BodyDocument5 pagesLesson 5. The Structure of The Human BodyValeria BerzanNo ratings yet
- Test Bank For Advanced Nutrition and Human Metabolism 7th Edition Gropper Smith Carr 1305627857 9781305627857Document22 pagesTest Bank For Advanced Nutrition and Human Metabolism 7th Edition Gropper Smith Carr 1305627857 9781305627857francisNo ratings yet
- Tessa Thomas - The 10-Minute Facelift - Lessen The Signs of Ageing The Natural Way-Hamlyn (2001)Document132 pagesTessa Thomas - The 10-Minute Facelift - Lessen The Signs of Ageing The Natural Way-Hamlyn (2001)Defne Güller100% (1)
- Physical AssessmentDocument2 pagesPhysical AssessmentEdmar DalmacioNo ratings yet
- Pathophysiology of Pernicious AnemiaDocument1 pagePathophysiology of Pernicious AnemiaMikhael Anthony Medina50% (4)
Large Intestine CA 2
Large Intestine CA 2
Uploaded by
Worku Kifle0 ratings0% found this document useful (0 votes)
26 views21 pages1. The document summarizes the anatomy, blood supply, lymphatic drainage, staging, signs and symptoms, diagnosis, and treatment of the large intestine and colorectal cancer.
2. Key points include that the large intestine extends from the ileocecal valve to the anus and has distinct layers in its wall. Colorectal cancer most commonly presents after age 50 and symptoms vary depending on tumor location.
3. Staging is based on tumor invasion depth, lymph node involvement, and presence of metastases, and is important for determining prognosis and treatment. Surgery is the main treatment, and chemotherapy may be given post-operatively to reduce cancer recurrence.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1. The document summarizes the anatomy, blood supply, lymphatic drainage, staging, signs and symptoms, diagnosis, and treatment of the large intestine and colorectal cancer.
2. Key points include that the large intestine extends from the ileocecal valve to the anus and has distinct layers in its wall. Colorectal cancer most commonly presents after age 50 and symptoms vary depending on tumor location.
3. Staging is based on tumor invasion depth, lymph node involvement, and presence of metastases, and is important for determining prognosis and treatment. Surgery is the main treatment, and chemotherapy may be given post-operatively to reduce cancer recurrence.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
26 views21 pagesLarge Intestine CA 2
Large Intestine CA 2
Uploaded by
Worku Kifle1. The document summarizes the anatomy, blood supply, lymphatic drainage, staging, signs and symptoms, diagnosis, and treatment of the large intestine and colorectal cancer.
2. Key points include that the large intestine extends from the ileocecal valve to the anus and has distinct layers in its wall. Colorectal cancer most commonly presents after age 50 and symptoms vary depending on tumor location.
3. Staging is based on tumor invasion depth, lymph node involvement, and presence of metastases, and is important for determining prognosis and treatment. Surgery is the main treatment, and chemotherapy may be given post-operatively to reduce cancer recurrence.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 21
Anatomy of large intestine
• Extends from ileo-caecal valve to the anus
• Divided anatomically & functionally into colon, rectum & anus
• The wall comprises 5 distinct layers-mucosa submucosa, inner
circular m.outer longitudinal m. & serosa
• Outer longitudinal m.separeted into 3 teniae coli
• The caecum is the widest & thinnest –vulnerable to perforation
• Mid gut- SI, ascending colon & proximal transverse colon—blood
supply by SMA
• Hind gut- distal transverse colon, descending ,rectum & proximal
anus –blood supply by IMA
Colon vascular supply
• SMA. –branches into
– Ileocolic a. which supply the terminal ileum &
proximal ascending colon
– Rt.colic a. supplies the ascending colon
– Middle colic a. supplies the transverse colon
• IMA--Lt.colic a. ,several sigmoidal a.& sup. Rectal a.
Colon lymphatic drainage
• Originate in a net work of lymphatics in the
muscularis mucosa
• LV & LN follow the regional arteries
• LN can be classified as –
.epi colic- on the bowel wall
.para colic – adj. to arterial arcades
.intermediate –named mesentric V.
.main – at the origin of SMA & IMA
SENTINEL LN –the 1st 1-4 LNS to drain the
specific segment of the colon
Colorectal Carcinoma
• Most common abdominal visceral malignancy
women- second to breast ca
men -third, Lung, prostate
• Sex -both sexes are affected
rectal ca- men
colonic -women
• Usually after sixth decade
_ Not strictly disease of old age
_ 10% occur before 40 years
_Familial and hereditary type-third decade
• Relatively un common in Africa&Asia
More common in Urban setup.
Distribution of CRC
Etiology( Risk factors)
• Environmental Factor
– Diet :High fiber diet with low fat diet is said to be more protective than fat
free diet
– Minor diet-Selenium, Vit A, Vit E , Caroteinoids
they decrease the free oxygen radicals at the mucosal surface and
decrease the risk of ca
– Other carcinogens Alcohol, Bile acid, Ionizing radiation
• Age –more than 50 years
• Pre malignant condition
Ulcerative colitis
Crohn’s disease
FAP
HNPCC
Previous hx of colonic polyp
• Family Hx of colorectal ca/polyp
• Long term immune suppression-small cell ca
Pathology and Path physiology
• Predominantly –mucosal adenocarcinoma
-Connective tissue sarcoma
-Carcinoid tumor
-Lymphoma
-M.melanoma
• Histologically- well ,moderately& poorly
differentiated
• Grossly –Annular _circumferential…left
• -Polyploidy ……right
• -ulcerative
Adenocarcinoma
Spread
• Arises in the colonic mucosa ` then invades the
muscularis mucosa…lymphatics in the submucosa …
regional LN….LN along the segmental arterial
supply and venous drainage
• Direct spread to adjacent structures (bladder,
ovaries,vagina)
• Transcelomic spread…cul de sac, blummer’s shelf
• Hematogenous spread…from the submucosal vein …
portal vein…liver
systemic vein….lung ,brain ,adrenal gland, kidneys.
Hematogenous spread is generally associated with
poor prognosis.
Staging …..
• Duke's staging
– Duke`sA - tumor confined to bowel wall(T1-3)
– Duke`sB- tumor involving or through serosa,not extending
to LN(T4)
– Duke`sC –Lymph node involved
– Duke's D –Distant metastasis
TNM Staging System
• T1 - tumor invading the submucosa
• T2- tumor invading muscularis propria
• T3-tumor invades through muscularis propria in
to the serosa or nonperitonized pericolic or
perirectal tissue
• T4-tumor out side the serosa.
• N1 -1-3 pericolic or perirectal LN
• N2 ->4 pericolic or perirectal LN
• N3 -metastasis in any LN along the named
vascular trunk
Staging …..
• Mo –no distant metastasis
• M1 _distant metastasis
• Stage I –T1/No/Mo or T2/No/Mo
• Stage II –T3/No/Mo or T4/No/Mo
• Stage III _Any T/N1/Mo or Any T/N2 orN3/Mo
• Stage IV _Any T/Any N/M1
• This provides more detailed pathologic information, and can
be converted easily to the simpler Duke’s system.
– Stage I -----Duke’s A
– Stage II.----Duke’s B
– Stage III----Duke’s C
– Stage IV---Duke’s D
Prognosis
• Staging is most important for prognosis.
• Stage I disease has 95-100% five years survival
• Stage II---40-60% five years survival
• LN involvement ---30%
• Liver involvement ---5-10%
85% die within 1 year.
• Age -Those which occur <40 years have bad prognosis
• Poor histologic differentiation
Excessive mucin producing tumor
Signet ring cell tumor
• Venous or perineural invasion
• Bowel perforation
• Elevated CEA
Signs and Symptoms
• Has wide range of clinical presentation.
• Depends on the location of tumor
• 20% of the ca occur in the ceacum and Rt side
of colon
• 70% occur distal to splenic flexure
• -_45% occur at or below the rectosigmoid
level
• Change of bowel habit
• Abdominal pain
• Rectal bleeding
• Iron deficiency anemia
Sub acute presentations
• Rt side Usually silent, don't cause change in
bowel habit except those large mucin
producing tumor ,which may produce
diarrhea.
• Acute appendicitis in elderly
• Ileal obstruction
• Signs of Anemia ,fatigue ,palpitation
• intermittent
• Weight lose, Fever of unknown origin
• As lead point for intussusception in adult.
Left side colonic ca
• Lower abdominal pain---relieved by bowel
motion
• Change of bowel habit
• Passage of mucus
• Tenesmus
• Abdominal/ rectal pain
• ↓the caliber of stool
• Pass bright red blood per rectum
• Mass in the left iliac fossa
• Ascites. Jaundice,peruritis or chest x-ray
picture of lung lesion
Acute presentation
• Significant proportion of pt
• Obstruction
• Perforation
• Obstruction—complete obstruction occurs in 10% of
pts but it is real emergency
• If the obstruction is not relieved it leads to
perforation ---fecal peritonitis and sepsis
• Perforation can occur at site of tumor
• Some times it perforates to adjacent structures like
bladder,vagina or small bowel
• If it perforate posteriorly psoas abscess.
Diagnosis and Evaluation of Colorectal ca
• Hx and P/E are important tool for Dx.
• PDE
• Definitive Dx is usually made by
• flexible sigmoidoscope 60-75%
• colonoscopy 100%
• Important for Biopsy and to estimate distance
• Barium enema .synchronous lesions 3-5%
• Other tests are important to evaluate the
extent of the disease and to search for
metastasis.
Routine investigations
• Hct
• Chest x-ray
• U/S
• CT scan of the abdomen to assess the extent of primary
tumor and to search for metastasis to intra abdominal
organ.
• LFT Late event
• CEA -if the tumor does not penetrate the bowel wall its
level does not raise
-it is non specific lung ca,breast ca, pancreas and
stomach ca., Smokers, Cirrhosis, pancreatits and renal
failure.
- high correlation with tumor metastasis and
recurrence
• Transanal US to assess depth of rectal ca
• Imaging of the upper Urinary tract---IVP
Treatment Principle
Preoperative pt preparation
• Psychological preparation for
possibility of colostomy & site of colostomy
Rx complications…Impotency
• Bowel preparation
it decrease risk of wound infection and
intraabdomenal abscess.
by mechanical cleansing and antibiotics(E coli and
B fragilis)
• Heparin
The definitive management is surgery
• Adjuvant Chemotherapy
– Colorectal ca is said to be resistant to
Chemotherapy.
– It is effective only,Post operatively when the
tumor burden is small
– 5 FU and Levamisole or
– 5 FU and Leucovorin
– Decreases cancer recurrence by 39% and cancer
related death by 32%
You might also like
- Medical Terminology For Health Professions Spiral Bound Version Mindtap Course List 9Th Edition Ehrlich Full ChapterDocument68 pagesMedical Terminology For Health Professions Spiral Bound Version Mindtap Course List 9Th Edition Ehrlich Full Chapterjames.radford791100% (7)
- Colorectal CancerDocument39 pagesColorectal CancerMuvenn Kannan100% (2)
- Nervous System WorksheetDocument8 pagesNervous System WorksheetBeneNo ratings yet
- S6 - Q2 - DLPS - Week 1 To 5Document302 pagesS6 - Q2 - DLPS - Week 1 To 5Dom MartinezNo ratings yet
- Powerpoint: Colorectal Polyps and Colorectal CarcinomaDocument68 pagesPowerpoint: Colorectal Polyps and Colorectal Carcinomaj.doe.hex_87100% (5)
- Colorectal CancerDocument3 pagesColorectal CancerAriane May Rubio50% (2)
- Fast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeFrom EverandFast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeNo ratings yet
- Super SizeCrashCourseDocument61 pagesSuper SizeCrashCourseJitaru Wilkins100% (12)
- Plant Anatomy and Physiology 1Document60 pagesPlant Anatomy and Physiology 1keron100% (1)
- Biology 1: Learning Activity SheetDocument184 pagesBiology 1: Learning Activity SheetJohn joseph Ursulum100% (1)
- Colon: Malueth AbrahamDocument39 pagesColon: Malueth AbrahamMalueth AnguiNo ratings yet
- Colorectal CancerDocument39 pagesColorectal CancerFernando AnibanNo ratings yet
- Gastric CancerDocument126 pagesGastric Cancermwani775100% (1)
- CasediscussionDocument30 pagesCasediscussionFernando AnibanNo ratings yet
- Upper Git TumorsDocument51 pagesUpper Git TumorsIsaac MwangiNo ratings yet
- Colorectal CaDocument24 pagesColorectal CaSA NodeNo ratings yet
- Carcinomagallbladder PDFDocument61 pagesCarcinomagallbladder PDFZaki DhiifNo ratings yet
- Coloncancerlecturenice 170826084151Document81 pagesColoncancerlecturenice 170826084151ckyew64No ratings yet
- Colorectal Ca (CRC) .: Malueth Abraham, MBCHB ViDocument36 pagesColorectal Ca (CRC) .: Malueth Abraham, MBCHB ViMalueth AnguiNo ratings yet
- 9 Gastric NeoplasmsDocument40 pages9 Gastric NeoplasmselshadieNo ratings yet
- Esophageal CarcinomaDocument34 pagesEsophageal Carcinomaapi-19916399100% (1)
- 42 EsophagusDocument49 pages42 EsophagusShiva BhandariNo ratings yet
- Malignancy in GI Tract-DR AgungDocument69 pagesMalignancy in GI Tract-DR AgungwkwkwkhhhhNo ratings yet
- DysphagiaDocument40 pagesDysphagiamanabdebuNo ratings yet
- Ca Colon: Pembimbing Dr. Yanti, SP.B KBDDocument47 pagesCa Colon: Pembimbing Dr. Yanti, SP.B KBDRichard HadinataNo ratings yet
- Lower Gi Case Presentation PDFDocument35 pagesLower Gi Case Presentation PDFapi-448999672No ratings yet
- Colorectal TumoursDocument21 pagesColorectal TumoursRUDOLF YUSON BM20110052No ratings yet
- Esophageal CADocument56 pagesEsophageal CAEdwin OkonNo ratings yet
- SURG - Hepatobiliary, Pancreas, SpleenDocument230 pagesSURG - Hepatobiliary, Pancreas, SpleenJoan Timbol100% (1)
- Colon and Rectal CancerDocument62 pagesColon and Rectal CancerSK TalkNo ratings yet
- Colorectalcancer 200612134444Document80 pagesColorectalcancer 200612134444Elena CaterevNo ratings yet
- CA OesophagusDocument47 pagesCA OesophagusAnsif KNo ratings yet
- Carcinoma Gall BladderDocument25 pagesCarcinoma Gall Bladderrajan kumarNo ratings yet
- CA ColonDocument47 pagesCA ColonrahayuNo ratings yet
- Colorectal CADocument76 pagesColorectal CANur Insyirah100% (2)
- Squamous Cell CarcinomaDocument53 pagesSquamous Cell CarcinomaWacky BlankNo ratings yet
- Management of Colon Cancers-1Document110 pagesManagement of Colon Cancers-1Edwin OkonNo ratings yet
- Colorectal CancerDocument48 pagesColorectal CancerAndre F SusantioNo ratings yet
- Hepatocellular Carcinoma 05Document45 pagesHepatocellular Carcinoma 05tupagalhkya2000No ratings yet
- Hepatocellular Carcinoma and Other Hepatic MassesDocument59 pagesHepatocellular Carcinoma and Other Hepatic MassesIsaac MwangiNo ratings yet
- Lower GIT CancersDocument43 pagesLower GIT CancersIsaac MwangiNo ratings yet
- Carcinoma of ColonDocument39 pagesCarcinoma of ColonMuhammad DaniyalNo ratings yet
- Colon CancerDocument41 pagesColon Cancervaishali TayadeNo ratings yet
- CarcinomarectumDocument45 pagesCarcinomarectumHuzefa MemonNo ratings yet
- Emory Reynolds Program Colon Cancer Resource ModuleDocument45 pagesEmory Reynolds Program Colon Cancer Resource ModulealbertontaolaNo ratings yet
- Case Presentation: by DR SaleemDocument61 pagesCase Presentation: by DR SaleemsandeepNo ratings yet
- Pancreatic TumorDocument28 pagesPancreatic TumorAli AtiaNo ratings yet
- 3.radiation InjDocument9 pages3.radiation Injapi-3829364No ratings yet
- Colon Cancer Vail 2008Document63 pagesColon Cancer Vail 2008SamGoldsteinNo ratings yet
- DDX of RIF Mass (Syazwani)Document44 pagesDDX of RIF Mass (Syazwani)Nurul Syazwani RamliNo ratings yet
- Surgery: Crohn's DiseaseDocument9 pagesSurgery: Crohn's Diseaseapi-3829364No ratings yet
- Carcinoma OesophagusDocument27 pagesCarcinoma Oesophagussammykiilu3No ratings yet
- Paediatric Abdominal MassesDocument73 pagesPaediatric Abdominal Massesg1381821No ratings yet
- Esophageal CancerDocument42 pagesEsophageal Cancerapi-1964133750% (2)
- Small Intestine: Earle J. Niervo Medical ClerkDocument168 pagesSmall Intestine: Earle J. Niervo Medical ClerkEarle Jimenez Niervo RNNo ratings yet
- 8 28 12 R Schaffer MDDocument51 pages8 28 12 R Schaffer MDKay BristolNo ratings yet
- Colorectal CancersDocument162 pagesColorectal CancersSomto NwabuezeNo ratings yet
- Carcinoma Oesophagus: Dr. S. Ranita DeviDocument46 pagesCarcinoma Oesophagus: Dr. S. Ranita DeviVivek AhanthemNo ratings yet
- Rectum: Malueth AbrahamDocument19 pagesRectum: Malueth AbrahamMalueth AnguiNo ratings yet
- Colon CancerDocument5 pagesColon CancerPan Dong100% (1)
- Bladder TumorsDocument36 pagesBladder TumorsMohammad BelbahaithNo ratings yet
- 18 Colorectal Polyps and CarcinomaDocument89 pages18 Colorectal Polyps and Carcinomasuhaib ananzehNo ratings yet
- Malignant Neoplasm of Body of UterusDocument20 pagesMalignant Neoplasm of Body of UterusZahidul ZahidNo ratings yet
- Carcinoma Rectum - Janak - NEWDocument74 pagesCarcinoma Rectum - Janak - NEWTowhidulIslamNo ratings yet
- GIT, CorrectedDocument105 pagesGIT, Correctedali attiaNo ratings yet
- Home Cure for Colon Cancer with Best Natural RemediesFrom EverandHome Cure for Colon Cancer with Best Natural RemediesRating: 5 out of 5 stars5/5 (1)
- Lower Limb Fracture..MeDocument142 pagesLower Limb Fracture..MeWorku KifleNo ratings yet
- LaPlace's LawDocument2 pagesLaPlace's LawWorku KifleNo ratings yet
- Cast/Splint Choice and Application: Worku K. (MD)Document15 pagesCast/Splint Choice and Application: Worku K. (MD)Worku KifleNo ratings yet
- Orofacial CystsDocument84 pagesOrofacial CystsWorku KifleNo ratings yet
- Small Intestine MMCDocument65 pagesSmall Intestine MMCWorku KifleNo ratings yet
- Vitamins: Organic Compounds Required in Minute Quantities Specific Body FunctionsDocument57 pagesVitamins: Organic Compounds Required in Minute Quantities Specific Body FunctionsWorku KifleNo ratings yet
- Maxillary Sinus DR - AssefaDocument65 pagesMaxillary Sinus DR - AssefaWorku KifleNo ratings yet
- Arsi University College of Health Sciences Department of MedicineDocument127 pagesArsi University College of Health Sciences Department of MedicineWorku KifleNo ratings yet
- 6.1. Stool Specimen 6.1. Stool Specimen: 9/18/21 Tafeseb - Tufa 1Document67 pages6.1. Stool Specimen 6.1. Stool Specimen: 9/18/21 Tafeseb - Tufa 1Worku KifleNo ratings yet
- Dentistry HoDocument17 pagesDentistry HoWorku KifleNo ratings yet
- Aseptic Techniques: - Antiseptic or Antimicrobial AgentDocument17 pagesAseptic Techniques: - Antiseptic or Antimicrobial AgentWorku KifleNo ratings yet
- Ped SurgDocument11 pagesPed SurgWorku KifleNo ratings yet
- Ortho: - Orthopedic Instruments - Anatomy and Physiology - FractureDocument2 pagesOrtho: - Orthopedic Instruments - Anatomy and Physiology - FractureWorku KifleNo ratings yet
- Acute Abdomen: - DefinitionDocument27 pagesAcute Abdomen: - DefinitionWorku KifleNo ratings yet
- Neck Masses and FistulasDocument55 pagesNeck Masses and FistulasWorku KifleNo ratings yet
- NEUROFIBROMATOSISDocument11 pagesNEUROFIBROMATOSISWorku KifleNo ratings yet
- Melanoma Belay Z July, 6 2005Document20 pagesMelanoma Belay Z July, 6 2005Worku KifleNo ratings yet
- Abdominal Wall DEFECTS: Omphalocele, Gastroschisis, Prune-BellyDocument38 pagesAbdominal Wall DEFECTS: Omphalocele, Gastroschisis, Prune-BellyWorku KifleNo ratings yet
- Acute Abdomen in ChildrenDocument61 pagesAcute Abdomen in ChildrenWorku KifleNo ratings yet
- Vascular Malformation and LymphoedemaDocument44 pagesVascular Malformation and LymphoedemaWorku KifleNo ratings yet
- Fluid and Electrolte Manageent in Paediatric Surgical PatientDocument29 pagesFluid and Electrolte Manageent in Paediatric Surgical PatientWorku KifleNo ratings yet
- Hypospadias Epispadias and Bladder Exstrophy: Khalid Abdella (MD) OCTOBER - 11 - 2006Document64 pagesHypospadias Epispadias and Bladder Exstrophy: Khalid Abdella (MD) OCTOBER - 11 - 2006Worku KifleNo ratings yet
- Obstruction of The Urinary TractDocument68 pagesObstruction of The Urinary TractWorku KifleNo ratings yet
- Colilithiasis 2Document53 pagesColilithiasis 2Worku KifleNo ratings yet
- Perioperative Care 2Document28 pagesPerioperative Care 2Worku KifleNo ratings yet
- Kaposi's Sarcoma: Patients Seen in The Past 8 Years: 83 CasesDocument12 pagesKaposi's Sarcoma: Patients Seen in The Past 8 Years: 83 CasesWorku KifleNo ratings yet
- Fluid & Electrolyte 2Document47 pagesFluid & Electrolyte 2Worku KifleNo ratings yet
- Melanoma: Meku Damtie (M.D.) July 18, 2006Document38 pagesMelanoma: Meku Damtie (M.D.) July 18, 2006Worku KifleNo ratings yet
- Gastrointestinal Hemorrhage2Document20 pagesGastrointestinal Hemorrhage2Worku KifleNo ratings yet
- Xylem - WikipediaDocument92 pagesXylem - WikipediaBashiir NuurNo ratings yet
- Life Processes - BIO - CLASS 10 - NOTESDocument10 pagesLife Processes - BIO - CLASS 10 - NOTESvaarunisaxenaNo ratings yet
- SBI3U Chapter 10 Self-QuizDocument6 pagesSBI3U Chapter 10 Self-QuizJannette JaneNo ratings yet
- Gynae FCPS 1 Guide-1Document24 pagesGynae FCPS 1 Guide-1Lubna MushtaqNo ratings yet
- SOX Science5 Q2 M2of7Document18 pagesSOX Science5 Q2 M2of7Neil Joy Felomino Basa-LepalemNo ratings yet
- TECH 614 Full Spine I (Castellucci)Document10 pagesTECH 614 Full Spine I (Castellucci)Robert StraubNo ratings yet
- Anti-Coagulant (Vte in Obstetrics) - Madam LiewDocument10 pagesAnti-Coagulant (Vte in Obstetrics) - Madam LiewNana YunusNo ratings yet
- Contoh Case ReportDocument4 pagesContoh Case ReportLyvia ChristieNo ratings yet
- Benign Gynecologic TumorsDocument57 pagesBenign Gynecologic TumorsDexter IanNo ratings yet
- Reflective Journal Mazatul AzrinDocument1 pageReflective Journal Mazatul AzrinNama Saya AtulNo ratings yet
- Feyer 2020 WvngoshawkDocument13 pagesFeyer 2020 WvngoshawkAgnieszka CzujkowskaNo ratings yet
- Developmental Biology of Frog: SpermDocument21 pagesDevelopmental Biology of Frog: SpermRavindra MadurNo ratings yet
- HemoperitoneumDocument36 pagesHemoperitoneumnovitafitri123No ratings yet
- ImmunohematologyDocument38 pagesImmunohematologyNoreenNo ratings yet
- 11th Bio Botany Book Back 1 Mark Questions With Answer Key English Medium - BakDocument6 pages11th Bio Botany Book Back 1 Mark Questions With Answer Key English Medium - BakShriya RameshNo ratings yet
- CS WTDocument5 pagesCS WTYeni PuspitasariNo ratings yet
- ATHENS: Class: 12, Topic: Human ReproductionDocument3 pagesATHENS: Class: 12, Topic: Human ReproductionATHENS MaterialNo ratings yet
- CH 10 Somatic and Special Senses Powerpoint 2006Document175 pagesCH 10 Somatic and Special Senses Powerpoint 2006Maikel PakageNo ratings yet
- Lesson 5. The Structure of The Human BodyDocument5 pagesLesson 5. The Structure of The Human BodyValeria BerzanNo ratings yet
- Test Bank For Advanced Nutrition and Human Metabolism 7th Edition Gropper Smith Carr 1305627857 9781305627857Document22 pagesTest Bank For Advanced Nutrition and Human Metabolism 7th Edition Gropper Smith Carr 1305627857 9781305627857francisNo ratings yet
- Tessa Thomas - The 10-Minute Facelift - Lessen The Signs of Ageing The Natural Way-Hamlyn (2001)Document132 pagesTessa Thomas - The 10-Minute Facelift - Lessen The Signs of Ageing The Natural Way-Hamlyn (2001)Defne Güller100% (1)
- Physical AssessmentDocument2 pagesPhysical AssessmentEdmar DalmacioNo ratings yet
- Pathophysiology of Pernicious AnemiaDocument1 pagePathophysiology of Pernicious AnemiaMikhael Anthony Medina50% (4)