Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
74 viewsCase Study NCM 118
Case Study NCM 118
Uploaded by
Romzy BasañesThis document provides information on emergency medications used to treat cardiac disorders. It discusses the actions, indications, dosages, and nursing considerations for lidocaine, magnesium sulfate, nitroglycerine, and amiodarone. Lidocaine is used to treat ventricular fibrillation and tachycardia. Magnesium sulfate corrects magnesium deficiencies and treats hypomagnesemia. Nitroglycerine provides acute relief of angina by relaxing blood vessels. Amiodarone is a class III antiarrhythmic that works by blocking potassium channels to treat arrhythmias. Close monitoring of patients is important when administering these cardiac medications.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You might also like
- PreviewpdfDocument145 pagesPreviewpdfTom100% (1)
- 1.5.2.3.00102 Reagent Insert Kit CRPDocument2 pages1.5.2.3.00102 Reagent Insert Kit CRPenoen_risa902883% (6)
- Darkness Visible: A Memoir of Madness IDocument4 pagesDarkness Visible: A Memoir of Madness ILucas ValdezNo ratings yet
- ANALYSIS OF LONGITUNIDAL CEPHALOMETRIC GROWTH DATA. Bhatia B.C. Leighton (1993) (01-17)Document17 pagesANALYSIS OF LONGITUNIDAL CEPHALOMETRIC GROWTH DATA. Bhatia B.C. Leighton (1993) (01-17)Nicolas StaffelbachNo ratings yet
- Severe Anxiety As Evidenced by Repetitive ActionDocument1 pageSevere Anxiety As Evidenced by Repetitive ActionRomzy Basañes100% (3)
- Nursing Care Plan 1Document3 pagesNursing Care Plan 1gagandipkS100% (1)
- 1.MOD On GERON (1) CommunicationDocument19 pages1.MOD On GERON (1) CommunicationPatricia VasquezNo ratings yet
- Nursing Care Plan: General: Goals Met GenreralDocument3 pagesNursing Care Plan: General: Goals Met GenreralRomzy BasañesNo ratings yet
- PediatricsDocument98 pagesPediatricsNicholas Field100% (1)
- LevofloxacinDocument15 pagesLevofloxacinsonal aranhaNo ratings yet
- Nursing Care of Clients in Emergency Situation 2Document108 pagesNursing Care of Clients in Emergency Situation 2Mary Joy FrancoNo ratings yet
- Kabiven: (Amino Acids, Electrolytes, Dextrose and Lipid Injectable Emulsion), For Intravenous UseDocument24 pagesKabiven: (Amino Acids, Electrolytes, Dextrose and Lipid Injectable Emulsion), For Intravenous UseDivine Mercy De JulianNo ratings yet
- NCP of Difficulty of BreathingDocument2 pagesNCP of Difficulty of BreathingMan GatuankoNo ratings yet
- Im Case Study 04Document49 pagesIm Case Study 04Shaine BalverdeNo ratings yet
- NCP For UDHDocument3 pagesNCP For UDHTomohiro HorieNo ratings yet
- Communicable Disease 2 AnswersDocument14 pagesCommunicable Disease 2 AnswersRika MaeNo ratings yet
- Checklist For Physical AssessmentDocument13 pagesChecklist For Physical AssessmentSharene Kate EribalNo ratings yet
- Bacillary DysenteryDocument32 pagesBacillary Dysenteryapi-199163990% (1)
- Cefixime: Suprax Class and CategoryDocument3 pagesCefixime: Suprax Class and CategoryArianne Joy SalvadorNo ratings yet
- Medical Surgical Nursing: By: Mr. Emerson AliswagDocument137 pagesMedical Surgical Nursing: By: Mr. Emerson AliswagMarie JhoanaNo ratings yet
- 01 NGT Procedure With RationaleDocument4 pages01 NGT Procedure With RationaleAryaj SulitNo ratings yet
- Write A If The Statement Is True and B If It Is FalseDocument1 pageWrite A If The Statement Is True and B If It Is FalseMemeeds ColangcagNo ratings yet
- Professional AdjustmentDocument22 pagesProfessional AdjustmentArgee Alonsabe100% (1)
- De Sagun, Leila Camille, A. NCMB312-RLE BSN3Y1-1B Course Task #1Document1 pageDe Sagun, Leila Camille, A. NCMB312-RLE BSN3Y1-1B Course Task #1Carl SantosNo ratings yet
- Discharge Plan: Patient'S Outcome Criteria Nursing OrderDocument1 pageDischarge Plan: Patient'S Outcome Criteria Nursing OrderCaroline AgbayNo ratings yet
- Example of Drug StudyDocument2 pagesExample of Drug Studydonna mae junioNo ratings yet
- Neuro - Sir Chavez - AS OF 12PMDocument5 pagesNeuro - Sir Chavez - AS OF 12PMCarl JustineNo ratings yet
- Potts DiseaseDocument8 pagesPotts Diseaseaimeeros0% (2)
- Case 1Document9 pagesCase 1Joselyn M. LachicaNo ratings yet
- Quiz 1Document5 pagesQuiz 1Francis Rafael PadillaNo ratings yet
- NCP Readiness UTI 1Document5 pagesNCP Readiness UTI 1Mary Grace AgataNo ratings yet
- November 2008 PreboardDocument84 pagesNovember 2008 PreboardYaj CruzadaNo ratings yet
- Funda Saved Ms2003Document103 pagesFunda Saved Ms2003June DumdumayaNo ratings yet
- 51 100Document18 pages51 100Jaessa Feliciano100% (1)
- Obj Questions 19.03.2018Document2 pagesObj Questions 19.03.2018Eli Zza KoiralaNo ratings yet
- NCM 118 Medsurg EndtermDocument25 pagesNCM 118 Medsurg EndtermJmarie Brillantes PopiocoNo ratings yet
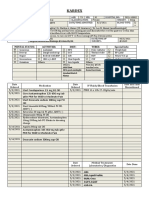
- Kardex: Mental Status: Activities: Diet: Tubes: Special InfoDocument3 pagesKardex: Mental Status: Activities: Diet: Tubes: Special InfoJanelle Cabida SupnadNo ratings yet
- Furosemide Drug StudyDocument2 pagesFurosemide Drug StudyNoah Kent MojicaNo ratings yet
- Drug StudyDocument17 pagesDrug StudyKenneth ManalangNo ratings yet
- Connie Mosuela MS FE 1Document3 pagesConnie Mosuela MS FE 1Tricia Jane OpinaldoNo ratings yet
- Evaluation Examination For Medicine WardDocument3 pagesEvaluation Examination For Medicine WardMarvick GalimaNo ratings yet
- Ateneo de Zamboanga University: Nursing Skills Output (Nso)Document9 pagesAteneo de Zamboanga University: Nursing Skills Output (Nso)Mitzi BelamideNo ratings yet
- TelmisartanDocument4 pagesTelmisartanHanniel MontecalboNo ratings yet
- P1 MS 3 Nur 200Document16 pagesP1 MS 3 Nur 200Xandra Joie Ondoy TabotaboNo ratings yet
- Post Op ThyroidectomyDocument1 pagePost Op Thyroidectomyzulkiflim88No ratings yet
- Therapeutic Communication Is A Collection ofDocument5 pagesTherapeutic Communication Is A Collection ofMadelaine EvangelioNo ratings yet
- PLAN OF ACTIVITIES 3 Days DRDocument5 pagesPLAN OF ACTIVITIES 3 Days DRKarl KiwisNo ratings yet
- NCPDocument3 pagesNCPErica Denice CastilloNo ratings yet
- Actual NCPDocument3 pagesActual NCPMabz BoholNo ratings yet
- NCLEX Questions PneumoniaDocument2 pagesNCLEX Questions PneumoniaLovely Laranjo100% (1)
- Hematologic ManagementDocument17 pagesHematologic ManagementAlyssa MontimorNo ratings yet
- Adult HealthDocument28 pagesAdult HealthL1NEDS DNo ratings yet
- Disaster Nursing NotesDocument4 pagesDisaster Nursing NotesChannelG100% (1)
- Case 3 Care of Client With GI, PUD, Cancer, Liver FailureDocument33 pagesCase 3 Care of Client With GI, PUD, Cancer, Liver FailureNyeam NyeamNo ratings yet
- A. Gestational Diabetes Mellitus B. Secondary Diabetes Mellitus D. Type II Diabetes MellitusDocument32 pagesA. Gestational Diabetes Mellitus B. Secondary Diabetes Mellitus D. Type II Diabetes MellitusNebawNo ratings yet
- GRP 3 2 Renal Nephrectomy NCPDocument6 pagesGRP 3 2 Renal Nephrectomy NCPPam RomeroNo ratings yet
- Ortho NCLEX Questions 1 PDFDocument39 pagesOrtho NCLEX Questions 1 PDFElizabella Henrietta TanaquilNo ratings yet
- Ob Ward Rle Drug StudyDocument3 pagesOb Ward Rle Drug StudyArisza Shane B.No ratings yet
- Case Study 1 PediaDocument7 pagesCase Study 1 PediaXeyanNo ratings yet
- Kardex: Mental Status - Conscious Activities Diet Tubes Special InfoDocument6 pagesKardex: Mental Status - Conscious Activities Diet Tubes Special InfoCaitlynNo ratings yet
- September 13 - NCM 112 (Mam G)Document2 pagesSeptember 13 - NCM 112 (Mam G)Aaron DayloNo ratings yet
- NVS Written ReportDocument20 pagesNVS Written ReportbabiNo ratings yet
- NCP - Impaired Gas Exchange (COPD)Document3 pagesNCP - Impaired Gas Exchange (COPD)Karen Joy ItoNo ratings yet
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDocument4 pagesTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestNo ratings yet
- Part 1 CD Mastery TestDocument15 pagesPart 1 CD Mastery TestRika MaeNo ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Chapter 4 - Health and Illness ReportDocument30 pagesChapter 4 - Health and Illness ReportRomzy BasañesNo ratings yet
- Nursing Care Plan: Subjective: "I Drink Alcohol and General: Independent: Independent: Goals Met GenreralDocument3 pagesNursing Care Plan: Subjective: "I Drink Alcohol and General: Independent: Independent: Goals Met GenreralRomzy BasañesNo ratings yet
- Nursing Care Plan: General: Goals Met GenreralDocument4 pagesNursing Care Plan: General: Goals Met GenreralRomzy Basañes100% (2)
- Movie Reflection Rain ManDocument1 pageMovie Reflection Rain ManRomzy Basañes100% (1)
- Week 1 RizalDocument2 pagesWeek 1 RizalRomzy BasañesNo ratings yet
- The Devil Wears Prada by Lauren Weisberger Is Classified As A Chick Lit Genre ofDocument3 pagesThe Devil Wears Prada by Lauren Weisberger Is Classified As A Chick Lit Genre ofRomzy BasañesNo ratings yet
- Hermeneutical PhenomenologyDocument12 pagesHermeneutical PhenomenologyRomzy Basañes50% (2)
- MammogramDocument2 pagesMammogramaideeh3110No ratings yet
- Folic Acid Deficiency AnemiaDocument8 pagesFolic Acid Deficiency AnemiaJon AbalosNo ratings yet
- School Health Examination Card: Republic of The Philippines Department of EducationDocument4 pagesSchool Health Examination Card: Republic of The Philippines Department of EducationDanny LineNo ratings yet
- Ait Nejm 2020Document9 pagesAit Nejm 2020Ahmed JallouliNo ratings yet
- Astm E2361 - 1 (En)Document5 pagesAstm E2361 - 1 (En)Sainath AmudaNo ratings yet
- 2022 Article 775Document17 pages2022 Article 775Felipe CortesNo ratings yet
- Outline For History TakingDocument2 pagesOutline For History TakingBlancheNo ratings yet
- Immune Thrombocytopenic Purpura in A Patient With Covid-19: CorrespondenceDocument2 pagesImmune Thrombocytopenic Purpura in A Patient With Covid-19: CorrespondencextineNo ratings yet
- Chemistry Analyzer: Chemistry Analyzers Can Be Benchtop Devices or Placed On A Cart Other Systems RequireDocument6 pagesChemistry Analyzer: Chemistry Analyzers Can Be Benchtop Devices or Placed On A Cart Other Systems RequireCalvin KleinNo ratings yet
- Assessment of Alveolar Bone Augmentation in Intrabony Defects Employing Platelet-Rich Fibrin (PRF) Membrane and Sticky Bone (Injectable-PRF & Demineralized Freeze-Dried Bone Graft) - A Case ReportDocument4 pagesAssessment of Alveolar Bone Augmentation in Intrabony Defects Employing Platelet-Rich Fibrin (PRF) Membrane and Sticky Bone (Injectable-PRF & Demineralized Freeze-Dried Bone Graft) - A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- What Happens During and After A ColonosDocument4 pagesWhat Happens During and After A ColonosAhmed Abd El AzizNo ratings yet
- Adenocarcinoma PulmonarDocument75 pagesAdenocarcinoma PulmonarLigia Micaela García XitamulNo ratings yet
- Matriks MCU Tangguh PreEmp 28 8 18 PDFDocument1 pageMatriks MCU Tangguh PreEmp 28 8 18 PDFDont All C SNo ratings yet
- NLE: Community Health Nursing Exam 1: Text ModeDocument33 pagesNLE: Community Health Nursing Exam 1: Text ModeAngelica SorianoNo ratings yet
- Pharmacology Questions CardiacDocument5 pagesPharmacology Questions CardiacAmanda SimpsonNo ratings yet
- SanaPro Individual Health Insurance Presentation - 2021 - Final ENDocument12 pagesSanaPro Individual Health Insurance Presentation - 2021 - Final ENGabriela GiurgiNo ratings yet
- NCP Acute Pain VaDocument3 pagesNCP Acute Pain VaKate ClarosNo ratings yet
- 35Document174 pages35sggdgdNo ratings yet
- Kolelitiasis in EnglishDocument18 pagesKolelitiasis in EnglishReza AkbarNo ratings yet
- Intravenous Thrombolysis For Acute Ischemic 2023Document19 pagesIntravenous Thrombolysis For Acute Ischemic 2023angieselene.telloNo ratings yet
- Vijaya DiagnosticDocument5 pagesVijaya Diagnosticuma reddyNo ratings yet
- White Blood Cells TugasDocument6 pagesWhite Blood Cells TugasanisaNo ratings yet
- Ingle's EndodonticsDocument50 pagesIngle's EndodonticsAndrei Antipin100% (1)
- Role of The Salivary Biomarkers in Oral Cancer Detection PDFDocument48 pagesRole of The Salivary Biomarkers in Oral Cancer Detection PDFBanditulNo ratings yet
- Arterial Blood GasDocument55 pagesArterial Blood GasDharlyn MungcalNo ratings yet
Case Study NCM 118
Case Study NCM 118
Uploaded by
Romzy Basañes0 ratings0% found this document useful (0 votes)
74 views14 pagesThis document provides information on emergency medications used to treat cardiac disorders. It discusses the actions, indications, dosages, and nursing considerations for lidocaine, magnesium sulfate, nitroglycerine, and amiodarone. Lidocaine is used to treat ventricular fibrillation and tachycardia. Magnesium sulfate corrects magnesium deficiencies and treats hypomagnesemia. Nitroglycerine provides acute relief of angina by relaxing blood vessels. Amiodarone is a class III antiarrhythmic that works by blocking potassium channels to treat arrhythmias. Close monitoring of patients is important when administering these cardiac medications.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides information on emergency medications used to treat cardiac disorders. It discusses the actions, indications, dosages, and nursing considerations for lidocaine, magnesium sulfate, nitroglycerine, and amiodarone. Lidocaine is used to treat ventricular fibrillation and tachycardia. Magnesium sulfate corrects magnesium deficiencies and treats hypomagnesemia. Nitroglycerine provides acute relief of angina by relaxing blood vessels. Amiodarone is a class III antiarrhythmic that works by blocking potassium channels to treat arrhythmias. Close monitoring of patients is important when administering these cardiac medications.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
74 views14 pagesCase Study NCM 118
Case Study NCM 118
Uploaded by
Romzy BasañesThis document provides information on emergency medications used to treat cardiac disorders. It discusses the actions, indications, dosages, and nursing considerations for lidocaine, magnesium sulfate, nitroglycerine, and amiodarone. Lidocaine is used to treat ventricular fibrillation and tachycardia. Magnesium sulfate corrects magnesium deficiencies and treats hypomagnesemia. Nitroglycerine provides acute relief of angina by relaxing blood vessels. Amiodarone is a class III antiarrhythmic that works by blocking potassium channels to treat arrhythmias. Close monitoring of patients is important when administering these cardiac medications.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 14
Emergency Medications for Cardiac Disorders
As presented by: Chery Lynn Arzaga & Romulo Basañes II
Client Background/History
Patient is a 30y/0 known case of epilepsy presented with
generalized tonic clonic seizures and got intubated in the emergency
department secondary to low GCS. Initially he was managed in line
with status epilepticus and kept on 4 antiepileptic drugs but EEG was
unremarkable. Later on found to have OTCs prolongation on digging
history, the patient’s family revealed use of loperamide tablets around
100-200 tablets per day. During stay he had recurrent VT and Vfib for
which a temporary pacemaker was applied and got reverted back.
Lidocaine
ACTION: Combines with fast sodium channels in myocardial cell membranes, which inhibits
sodium influx into cells and decreases ventricular depolarization, as well as automaticity and
excitability during diastole. Lidocaine also blocks nerve impulses by decreasing the
permeability of neuronal membranes to sodium, which produces local anesthesia.
INDICATION: To treat ventricular fibrillation or ventricular tachycardia
DOSAGE AND FORMS: Loading: 50 to 100 mg (or 1 to 1.5 mg/kg), given at 25 to 50 mg/min.
If desired response isn’t achieved after 5 to 10 min, second dose of 25 to 50 mg (or 0.5 to 0.75
mg/kg) given every 5 to 10 min until maximum loading dose (300 mg in 1 hr) has been given.
CONTRAINDICATIONS: Adams–Stokes syndrome; hypersensitivity to lidocaine, amide
anesthetics, or their components; severe heart block (without artificial pacemaker); Wolff–
Parkinson– White syndrome
Cont.
SPECIAL PRECAUTIONS:
Use caution when administering lidocaine to patients with compromised myocardial function
because of risk of electrolyte disturbances or fluid overload.
ADVERSE REACTIONS: CNS: Anxiety; apprehension; confusion; difficulty speaking;
dizziness; drowsiness; euphoria; hallucinations; lethargy; lightheadedness; malignant
hyperthermia; paresthesia; seizures; sensation of cold, heat, or numbness; tremors; twitching;
unconsciousness CV: Bradycardia, cardiac arrest, hypotension, new or worsening arrhythmias
EENT: Blurred vision, diplopia, tinnitus GI: Nausea, vomiting HEME: Methemoglobinemia
MS: Muscle weakness, myalgia RESP: Respiratory arrest or depression Other: Anaphylaxis,
other less severe hypersensitivity reactions; injection-site burning, irritation, petechiae, redness,
stinging, swelling, and tenderness; worsened pain
Cont.
NURSING CONSIDERATIONS:
Observe for respiratory depression after bolus injection and during I.V. infusion of lidocaine.
Keep life-support equipment and vasopressors nearby during I.V. use in case of respiratory depression or other
reactions.
Carefully check prefilled syringes before using. Use only syringes labeled “for cardiac arrhythmias” for I.V.
administration.
As ordered, titrate I.V. dose to minimum amount needed to prevent arrhythmias. If administration is controlled by a
pumping device, stop pump before container runs dry because an air embolism may result. Change intravenous
administration apparatus at least once every 24 hours.
During I.V. administration, place patient on cardiac monitor, as ordered, and closely observe her at all times. Monitor
for prolonged PR interval, widening QRS complex, or worsening arrhythmias— possible signs of drug toxicity. If
present, notify prescriber and expect to discontinue lidocaine therapy immediately. Although infrequent, also
monitor her for hypersensitivity reactions that can be as severe as anaphylaxis following lidocaine administration. If
anaphylaxis occurs, discontinue drug, notify prescriber, and provide supportive care.
If signs of toxicity, such as dizziness, occur, notify prescriber and expect to discontinue or slow infusion.
Monitor vital signs as well as BUN and serum creatinine and electrolyte levels during and after therapy.
Magnesium Sulfate
• ACTION: Assists all enzymes involved in phosphate transfer reactions that use adenosine triphosphate
(ATP). Magnesium is required for normal function of the ATP-dependent sodium–potassium pump in
muscle membranes. It may effectively treat digitalis glycoside–induced arrhythmias because correction of
hypomagnesemia improves the sodium–potassium pump’s ability to distribute potassium into intracellular
spaces and because magnesium decreases calcium uptake and potassium outflow through myocardial cell
membranes
• INDICATION: To correct magnesium deficiency and to treat severe hypomagnesemia
• DOSAGE AND FORMS: 5 g diluted in 1 L I.V. solution and infused over 3 hr.
• CONTRAINDICATIONS: Hypersensitivity to magnesium salts or any component of magnesium-
containing preparations For magnesium chloride: Coma, heart disease, renal impairment For magnesium
sulfate: Heart block, MI, preeclampsia 2 hours or less before delivery (I.V. form) For use as laxative: Acute
abdominal problem (as indicated by abdominal pain, nausea, or vomiting), diverticulitis, fecal impaction,
intestinal obstruction or perforation, colostomy or ileostomy, severe renal impairment, ulcerative colitis
Cont.
SPECIAL PRECAUTIONS:
warning Observe for and report early evidence of hypermagnesemia: bradycardia, depressed
deep tendon reflexes, diplopia, dyspnea, flushing, hypotension, nausea, slurred speech,
vomiting, and weakness.
warning Be aware that magnesium may precipitate myasthenic crisis by decreasing patient’s
sensitivity to acetylcholine.
ADVERSE REACTIONS: CNS: Confusion, decreased reflexes, dizziness, syncope CV:
Arrhythmias, hypotension GI: Flatulence, vomiting MS: Muscle cramps RESP: Dyspnea,
respiratory depression or paralysis SKIN: Diaphoresis Other: Allergic reaction,
hypermagnesemia, injection-site pain or irritation (I.M. form), laxative dependence, magnesium
toxicity.
Cont.
NURSING CONSIDERATIONS:
Always consider the 5 rights: right patient, right drugs, right dose, right time and right route
Frequently assess cardiac status of patient taking drugs that lower heart rate, such as beta
blockers, because magnesium may aggravate symptoms of heart block.
Monitor serum electrolyte levels in patients with renal insufficiency because they’re at risk for
magnesium toxicity.
Monitor v/s
Nitroglycerine
Action:Nitroglycerin is converted by mitochondrial aldehyde dehydrogenase (mtALDH) to nitric oxide
(NO), an active substance which then activates the enzyme guanylate cyclase.The activation of this
enzyme is followed by the synthesis of cyclic guanosine 3',5'-monophosphate (cGMP), activating a
cascade of protein kinase-dependent phosphorylation events in smooth muscles. This process eventually
leads to the dephosphorylation of the myosin light chain of smooth muscles, causing relaxation and
increased blood flow in veins, arteries and cardiac tissue.. The above processes lead to decreased work of
the heart decreased blood pressure, relief of anginal symptoms, and increased blood flow to the
myocardium.
Indications: indicated for the acute relief of an attack or acute prophylaxis of angina pectoris due to
coronary artery disease.
Dosage and Forms: Sublingual. Administer one tablet under the tongue or in the buccal pouch at the first
sign of an acute anginal attack. Allow tablet to dissolve without swallowing. One additional tablet may
be administered every 5 minutes until relief is obtained. No more than three tablets are recommended
within a 15-minute period.
Cont.
Contraindications: Known history of increased intracranial pressure, severe anemia, right-
sided myocardial infarction, or hypersensitivity to nitroglycerin are contraindications to
nitroglycerin therapy.
Special Precautions:
i. Excessive use may lead to the development of tolerance. Only the smallest dose required for
effective relief of the acute angina attack should be used.
ii. Severe hypotension, particularly with upright posture, may occur with small doses of
nitroglycerin particularly in patients with constrictive pericarditis, aortic or mitral stenosis,
patients who may be volume-depleted, or are already hypotensive
iii. Nitroglycerin produces dose-related headaches, especially at the start of nitroglycerin therapy,
which may be severe and persist but usually subside with continued use.
Cont.
Adverse Reactions: severe or throbbing headaches, pounding heartbeats,
fluttering in your chest, slow heart rate, lightheadedness, blurred vision, dry
mouth, chest pain or pressure, pain spreading to your jaw or shoulder, nausea,
and sweating
Nursing Considerations:
i. Check blood pressure and pulse before each administration of NTG–blood
pressure can drop precipitously after a single dose. Hold dose if systolic BP <
90 mm Hg or more than 30 mm Hg below baseline.
ii. NTG is highly unstable and should be stored in light resistant container in cool
environment
Amiodarone
Action: Amiodarone is primarily a class III antiarrhythmic. Like other antiarrhythmic drugs of this class,
amiodarone works primarily by blocking potassium rectifier currents responsible for the repolarization of
the heart during phase 3 of the cardiac action potential. This potassium channel-blocking effect results in
increased action potential duration and a prolonged effective refractory period in cardiac myocytes.
Myocyte excitability is decreased, preventing reentry mechanisms and ectopic foci from perpetuating
tachyarrhythmias.
Indications: commonly used off-label to treat supraventricular tachyarrhythmias such as atrial fibrillation
as well as for the prevention of ventricular tachyarrhythmias (VTs) in high-risk patients.
Dosage and forms: Injectable solution. 50mg/ml, 150mg/100ml, 360mg/200ml
Contraindications:
i. Hypersensitivity
ii. Severe sinus node dysfunction, 2°/3° AV block or bradycardia causing syncope (except with functioning
artificial pacemaker), cardiogenic shock
iii. Avoid during breastfeeding
Cont.
Special Precautions:
i. Indicated only for life-threatening arrhythmias because of risk for substantial toxicity; poses
major management problems that could be life-threatening in patients at risk of sudden death;
therefore, make every effort to utilize alternative agents first
ii. amiodarone may remain in your body for several months after you stop taking it. You may
continue to experience side effects of amiodarone during this time. Be sure to tell every
health care provider who treats you or prescribes any medication for you during this time that
you have recently stopped taking amiodarone.
Adverse Reactions: constipation loss of appetite headache, decreased sex drive, difficulty
falling asleep or staying asleep, flushing, changes in ability to taste and smell, changes in
amount of saliva
Cont.
Nursing Responsibilities:
i. Monitor blood pressure and apical pulse prior to administration.
ii. Cardiac monitor should be used on patients receiving amiodarone therapy.
iii. Baseline assessments should be checked of liver function and thyroid function.
iv. Monitor serum level frequently.
You might also like
- PreviewpdfDocument145 pagesPreviewpdfTom100% (1)
- 1.5.2.3.00102 Reagent Insert Kit CRPDocument2 pages1.5.2.3.00102 Reagent Insert Kit CRPenoen_risa902883% (6)
- Darkness Visible: A Memoir of Madness IDocument4 pagesDarkness Visible: A Memoir of Madness ILucas ValdezNo ratings yet
- ANALYSIS OF LONGITUNIDAL CEPHALOMETRIC GROWTH DATA. Bhatia B.C. Leighton (1993) (01-17)Document17 pagesANALYSIS OF LONGITUNIDAL CEPHALOMETRIC GROWTH DATA. Bhatia B.C. Leighton (1993) (01-17)Nicolas StaffelbachNo ratings yet
- Severe Anxiety As Evidenced by Repetitive ActionDocument1 pageSevere Anxiety As Evidenced by Repetitive ActionRomzy Basañes100% (3)
- Nursing Care Plan 1Document3 pagesNursing Care Plan 1gagandipkS100% (1)
- 1.MOD On GERON (1) CommunicationDocument19 pages1.MOD On GERON (1) CommunicationPatricia VasquezNo ratings yet
- Nursing Care Plan: General: Goals Met GenreralDocument3 pagesNursing Care Plan: General: Goals Met GenreralRomzy BasañesNo ratings yet
- PediatricsDocument98 pagesPediatricsNicholas Field100% (1)
- LevofloxacinDocument15 pagesLevofloxacinsonal aranhaNo ratings yet
- Nursing Care of Clients in Emergency Situation 2Document108 pagesNursing Care of Clients in Emergency Situation 2Mary Joy FrancoNo ratings yet
- Kabiven: (Amino Acids, Electrolytes, Dextrose and Lipid Injectable Emulsion), For Intravenous UseDocument24 pagesKabiven: (Amino Acids, Electrolytes, Dextrose and Lipid Injectable Emulsion), For Intravenous UseDivine Mercy De JulianNo ratings yet
- NCP of Difficulty of BreathingDocument2 pagesNCP of Difficulty of BreathingMan GatuankoNo ratings yet
- Im Case Study 04Document49 pagesIm Case Study 04Shaine BalverdeNo ratings yet
- NCP For UDHDocument3 pagesNCP For UDHTomohiro HorieNo ratings yet
- Communicable Disease 2 AnswersDocument14 pagesCommunicable Disease 2 AnswersRika MaeNo ratings yet
- Checklist For Physical AssessmentDocument13 pagesChecklist For Physical AssessmentSharene Kate EribalNo ratings yet
- Bacillary DysenteryDocument32 pagesBacillary Dysenteryapi-199163990% (1)
- Cefixime: Suprax Class and CategoryDocument3 pagesCefixime: Suprax Class and CategoryArianne Joy SalvadorNo ratings yet
- Medical Surgical Nursing: By: Mr. Emerson AliswagDocument137 pagesMedical Surgical Nursing: By: Mr. Emerson AliswagMarie JhoanaNo ratings yet
- 01 NGT Procedure With RationaleDocument4 pages01 NGT Procedure With RationaleAryaj SulitNo ratings yet
- Write A If The Statement Is True and B If It Is FalseDocument1 pageWrite A If The Statement Is True and B If It Is FalseMemeeds ColangcagNo ratings yet
- Professional AdjustmentDocument22 pagesProfessional AdjustmentArgee Alonsabe100% (1)
- De Sagun, Leila Camille, A. NCMB312-RLE BSN3Y1-1B Course Task #1Document1 pageDe Sagun, Leila Camille, A. NCMB312-RLE BSN3Y1-1B Course Task #1Carl SantosNo ratings yet
- Discharge Plan: Patient'S Outcome Criteria Nursing OrderDocument1 pageDischarge Plan: Patient'S Outcome Criteria Nursing OrderCaroline AgbayNo ratings yet
- Example of Drug StudyDocument2 pagesExample of Drug Studydonna mae junioNo ratings yet
- Neuro - Sir Chavez - AS OF 12PMDocument5 pagesNeuro - Sir Chavez - AS OF 12PMCarl JustineNo ratings yet
- Potts DiseaseDocument8 pagesPotts Diseaseaimeeros0% (2)
- Case 1Document9 pagesCase 1Joselyn M. LachicaNo ratings yet
- Quiz 1Document5 pagesQuiz 1Francis Rafael PadillaNo ratings yet
- NCP Readiness UTI 1Document5 pagesNCP Readiness UTI 1Mary Grace AgataNo ratings yet
- November 2008 PreboardDocument84 pagesNovember 2008 PreboardYaj CruzadaNo ratings yet
- Funda Saved Ms2003Document103 pagesFunda Saved Ms2003June DumdumayaNo ratings yet
- 51 100Document18 pages51 100Jaessa Feliciano100% (1)
- Obj Questions 19.03.2018Document2 pagesObj Questions 19.03.2018Eli Zza KoiralaNo ratings yet
- NCM 118 Medsurg EndtermDocument25 pagesNCM 118 Medsurg EndtermJmarie Brillantes PopiocoNo ratings yet
- Kardex: Mental Status: Activities: Diet: Tubes: Special InfoDocument3 pagesKardex: Mental Status: Activities: Diet: Tubes: Special InfoJanelle Cabida SupnadNo ratings yet
- Furosemide Drug StudyDocument2 pagesFurosemide Drug StudyNoah Kent MojicaNo ratings yet
- Drug StudyDocument17 pagesDrug StudyKenneth ManalangNo ratings yet
- Connie Mosuela MS FE 1Document3 pagesConnie Mosuela MS FE 1Tricia Jane OpinaldoNo ratings yet
- Evaluation Examination For Medicine WardDocument3 pagesEvaluation Examination For Medicine WardMarvick GalimaNo ratings yet
- Ateneo de Zamboanga University: Nursing Skills Output (Nso)Document9 pagesAteneo de Zamboanga University: Nursing Skills Output (Nso)Mitzi BelamideNo ratings yet
- TelmisartanDocument4 pagesTelmisartanHanniel MontecalboNo ratings yet
- P1 MS 3 Nur 200Document16 pagesP1 MS 3 Nur 200Xandra Joie Ondoy TabotaboNo ratings yet
- Post Op ThyroidectomyDocument1 pagePost Op Thyroidectomyzulkiflim88No ratings yet
- Therapeutic Communication Is A Collection ofDocument5 pagesTherapeutic Communication Is A Collection ofMadelaine EvangelioNo ratings yet
- PLAN OF ACTIVITIES 3 Days DRDocument5 pagesPLAN OF ACTIVITIES 3 Days DRKarl KiwisNo ratings yet
- NCPDocument3 pagesNCPErica Denice CastilloNo ratings yet
- Actual NCPDocument3 pagesActual NCPMabz BoholNo ratings yet
- NCLEX Questions PneumoniaDocument2 pagesNCLEX Questions PneumoniaLovely Laranjo100% (1)
- Hematologic ManagementDocument17 pagesHematologic ManagementAlyssa MontimorNo ratings yet
- Adult HealthDocument28 pagesAdult HealthL1NEDS DNo ratings yet
- Disaster Nursing NotesDocument4 pagesDisaster Nursing NotesChannelG100% (1)
- Case 3 Care of Client With GI, PUD, Cancer, Liver FailureDocument33 pagesCase 3 Care of Client With GI, PUD, Cancer, Liver FailureNyeam NyeamNo ratings yet
- A. Gestational Diabetes Mellitus B. Secondary Diabetes Mellitus D. Type II Diabetes MellitusDocument32 pagesA. Gestational Diabetes Mellitus B. Secondary Diabetes Mellitus D. Type II Diabetes MellitusNebawNo ratings yet
- GRP 3 2 Renal Nephrectomy NCPDocument6 pagesGRP 3 2 Renal Nephrectomy NCPPam RomeroNo ratings yet
- Ortho NCLEX Questions 1 PDFDocument39 pagesOrtho NCLEX Questions 1 PDFElizabella Henrietta TanaquilNo ratings yet
- Ob Ward Rle Drug StudyDocument3 pagesOb Ward Rle Drug StudyArisza Shane B.No ratings yet
- Case Study 1 PediaDocument7 pagesCase Study 1 PediaXeyanNo ratings yet
- Kardex: Mental Status - Conscious Activities Diet Tubes Special InfoDocument6 pagesKardex: Mental Status - Conscious Activities Diet Tubes Special InfoCaitlynNo ratings yet
- September 13 - NCM 112 (Mam G)Document2 pagesSeptember 13 - NCM 112 (Mam G)Aaron DayloNo ratings yet
- NVS Written ReportDocument20 pagesNVS Written ReportbabiNo ratings yet
- NCP - Impaired Gas Exchange (COPD)Document3 pagesNCP - Impaired Gas Exchange (COPD)Karen Joy ItoNo ratings yet
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDocument4 pagesTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestNo ratings yet
- Part 1 CD Mastery TestDocument15 pagesPart 1 CD Mastery TestRika MaeNo ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Chapter 4 - Health and Illness ReportDocument30 pagesChapter 4 - Health and Illness ReportRomzy BasañesNo ratings yet
- Nursing Care Plan: Subjective: "I Drink Alcohol and General: Independent: Independent: Goals Met GenreralDocument3 pagesNursing Care Plan: Subjective: "I Drink Alcohol and General: Independent: Independent: Goals Met GenreralRomzy BasañesNo ratings yet
- Nursing Care Plan: General: Goals Met GenreralDocument4 pagesNursing Care Plan: General: Goals Met GenreralRomzy Basañes100% (2)
- Movie Reflection Rain ManDocument1 pageMovie Reflection Rain ManRomzy Basañes100% (1)
- Week 1 RizalDocument2 pagesWeek 1 RizalRomzy BasañesNo ratings yet
- The Devil Wears Prada by Lauren Weisberger Is Classified As A Chick Lit Genre ofDocument3 pagesThe Devil Wears Prada by Lauren Weisberger Is Classified As A Chick Lit Genre ofRomzy BasañesNo ratings yet
- Hermeneutical PhenomenologyDocument12 pagesHermeneutical PhenomenologyRomzy Basañes50% (2)
- MammogramDocument2 pagesMammogramaideeh3110No ratings yet
- Folic Acid Deficiency AnemiaDocument8 pagesFolic Acid Deficiency AnemiaJon AbalosNo ratings yet
- School Health Examination Card: Republic of The Philippines Department of EducationDocument4 pagesSchool Health Examination Card: Republic of The Philippines Department of EducationDanny LineNo ratings yet
- Ait Nejm 2020Document9 pagesAit Nejm 2020Ahmed JallouliNo ratings yet
- Astm E2361 - 1 (En)Document5 pagesAstm E2361 - 1 (En)Sainath AmudaNo ratings yet
- 2022 Article 775Document17 pages2022 Article 775Felipe CortesNo ratings yet
- Outline For History TakingDocument2 pagesOutline For History TakingBlancheNo ratings yet
- Immune Thrombocytopenic Purpura in A Patient With Covid-19: CorrespondenceDocument2 pagesImmune Thrombocytopenic Purpura in A Patient With Covid-19: CorrespondencextineNo ratings yet
- Chemistry Analyzer: Chemistry Analyzers Can Be Benchtop Devices or Placed On A Cart Other Systems RequireDocument6 pagesChemistry Analyzer: Chemistry Analyzers Can Be Benchtop Devices or Placed On A Cart Other Systems RequireCalvin KleinNo ratings yet
- Assessment of Alveolar Bone Augmentation in Intrabony Defects Employing Platelet-Rich Fibrin (PRF) Membrane and Sticky Bone (Injectable-PRF & Demineralized Freeze-Dried Bone Graft) - A Case ReportDocument4 pagesAssessment of Alveolar Bone Augmentation in Intrabony Defects Employing Platelet-Rich Fibrin (PRF) Membrane and Sticky Bone (Injectable-PRF & Demineralized Freeze-Dried Bone Graft) - A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- What Happens During and After A ColonosDocument4 pagesWhat Happens During and After A ColonosAhmed Abd El AzizNo ratings yet
- Adenocarcinoma PulmonarDocument75 pagesAdenocarcinoma PulmonarLigia Micaela García XitamulNo ratings yet
- Matriks MCU Tangguh PreEmp 28 8 18 PDFDocument1 pageMatriks MCU Tangguh PreEmp 28 8 18 PDFDont All C SNo ratings yet
- NLE: Community Health Nursing Exam 1: Text ModeDocument33 pagesNLE: Community Health Nursing Exam 1: Text ModeAngelica SorianoNo ratings yet
- Pharmacology Questions CardiacDocument5 pagesPharmacology Questions CardiacAmanda SimpsonNo ratings yet
- SanaPro Individual Health Insurance Presentation - 2021 - Final ENDocument12 pagesSanaPro Individual Health Insurance Presentation - 2021 - Final ENGabriela GiurgiNo ratings yet
- NCP Acute Pain VaDocument3 pagesNCP Acute Pain VaKate ClarosNo ratings yet
- 35Document174 pages35sggdgdNo ratings yet
- Kolelitiasis in EnglishDocument18 pagesKolelitiasis in EnglishReza AkbarNo ratings yet
- Intravenous Thrombolysis For Acute Ischemic 2023Document19 pagesIntravenous Thrombolysis For Acute Ischemic 2023angieselene.telloNo ratings yet
- Vijaya DiagnosticDocument5 pagesVijaya Diagnosticuma reddyNo ratings yet
- White Blood Cells TugasDocument6 pagesWhite Blood Cells TugasanisaNo ratings yet
- Ingle's EndodonticsDocument50 pagesIngle's EndodonticsAndrei Antipin100% (1)
- Role of The Salivary Biomarkers in Oral Cancer Detection PDFDocument48 pagesRole of The Salivary Biomarkers in Oral Cancer Detection PDFBanditulNo ratings yet
- Arterial Blood GasDocument55 pagesArterial Blood GasDharlyn MungcalNo ratings yet