Professional Documents
Culture Documents
Carcinoma of The Oesophagus
Carcinoma of The Oesophagus
Uploaded by
momodou s jallow0 ratings0% found this document useful (0 votes)
23 views27 pagesThe document discusses carcinoma of the esophagus, including its epidemiology, risk factors, clinical features, diagnostic evaluation, staging, and treatment options. The esophagus is approximately 25 cm long tube that extends from the cricopharyngeus to the gastroesophageal junction. Esophageal cancer is more common in males and risk increases with age. Symptoms often include dysphagia, weight loss, and pain. Diagnosis involves endoscopy with biopsy. Staging involves endoscopic ultrasound, CT, and PET scans. Treatment may include surgery, chemotherapy, radiation therapy, or a combination.
Original Description:
lecture powerpoint university of the Gambia
Original Title
Carcinoma of the Oesophagus
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses carcinoma of the esophagus, including its epidemiology, risk factors, clinical features, diagnostic evaluation, staging, and treatment options. The esophagus is approximately 25 cm long tube that extends from the cricopharyngeus to the gastroesophageal junction. Esophageal cancer is more common in males and risk increases with age. Symptoms often include dysphagia, weight loss, and pain. Diagnosis involves endoscopy with biopsy. Staging involves endoscopic ultrasound, CT, and PET scans. Treatment may include surgery, chemotherapy, radiation therapy, or a combination.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
23 views27 pagesCarcinoma of The Oesophagus
Carcinoma of The Oesophagus
Uploaded by
momodou s jallowThe document discusses carcinoma of the esophagus, including its epidemiology, risk factors, clinical features, diagnostic evaluation, staging, and treatment options. The esophagus is approximately 25 cm long tube that extends from the cricopharyngeus to the gastroesophageal junction. Esophageal cancer is more common in males and risk increases with age. Symptoms often include dysphagia, weight loss, and pain. Diagnosis involves endoscopy with biopsy. Staging involves endoscopic ultrasound, CT, and PET scans. Treatment may include surgery, chemotherapy, radiation therapy, or a combination.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 27
Carcinoma of the Oesophagus
Dr. Luis Vazquez Lopez
General Surgery Consultant
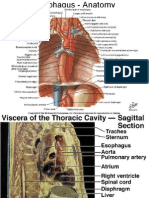
Clinical Anatomy
Hollow muscular tube 25 cm in length which spans from the
cricopharyngeus at the cricoid cartilage to gastroesophageal
junction (Extends from C7-T10).
Has 4 constrictions- At starting(cricophyrangeal
junction)
• crossed by aortic arch(9’inch)
• crossed by left bronchus(11’inch)
• Pierces the diaphragm(15’inch)
Histologically 4 layers:
• mucosa, submucosa, muscular &
fibrous layer.
Clinical Anatomy
Four regions of the esophagus:
• Cervical = cricoid cartilage to thoracic inlet (15–18 cm from the
incisor).
• Upper thoracic = thoracic inlet to tracheal bifurcation (18–24 cm).
• Midthoracic = tracheal bifurcation to just above the GE junction
(24–32 cm).
• Lower thoracic = GE junction (32–40 cm).
Lymphatic Drainage
Epidemiology
• Esophageal cancer is the 7th leading cause of cancer deaths.
• Accounts for 1% of all malignancy & 6% of all GI malignancy.
• Most common in China, Iran, South Africa, India and the former Soviet Union.
• The incidence rises steadily with age, reaching a peak in the 6th to 7th
decade of life.
• Male : Female = 3.5 : 1
• African-American males : White males = 5:1
Epidemiology
• Worldwide SCC responsible for most of the cases.
• Adenocarcinoma now accounts for over 50% of esophageal cancer in the
USA, due to association with GERD , Barretts’s esophagus & obesity.
• SCC usually occurs in the middle 3rd of the esophagus (the ratio of upper :
middle : lower is 15 : 50 : 35).
• Adenocarcinoma is most common in the lower 3rd of the esophagus,
accounting for over 65% of cases.
Risk Factors
Pathological Classification
Clinical Features
• It is commonly associated with the
symptoms of dysphagia, wt. loss, pain,
anorexia, and vomiting
• Symptoms often start 3 to 4 months
before diagnosis
• Dysphagia - in more than 90% pt.
• Odynophagia - in 50% of pt.
• Wt. loss – more than 5 % of total body
wt. in 40 – 70% pt. associated with
worst prognosis.
Complications
Cachexia, Malnutrition, dehydration, anaemia,.
Aspiration pneumonia.
Distant metastasis.
Invasion of near by structures: e.g.
• Recurrent laryngeal nerve → Hoarseness of voice
• Trachea: Stridor, cough, cyanosis
• Perforation into the pleural cavity → Empyema
• Back pain in celiac axis node involvement
Diagnostic
Detailed history & Physical examination: Dysphagia,
odynophagia, hoarseness, wt. loss, use of tobacco,
nitrosamines, history of GERD. Examine for cervical or
supraclavicular adenopathy.
Diagnostic
Confirmation of diagnosis:
EGD: allow direct visualization and biopsy, measure proximal &
distal distance of tumor from incisor, presence of Barrett’s
esophagus.
Diagnostic
Staging
CT chest and abdomen: Essential for staging because it can identify extension
beyond the esophageal wall, enlarged lymph nodes and visceral metastases.
Endoscopic Ultrasonography
EUS:
• Assess the depth of penetration and LN involvement. Limited by the degree of
obstruction.
• Compared with EUS, CT is not a reliable tool for evaluation of the
extent of tumor in the esophageal wall.
PET Scan
• most recently, proven to be valuable staging tool
• can detect up to 15–20% of metastases not seen on CT and EUS
• low accuracy in detecting local nodal disease compared to CT / EUS
• Value in evaluating response to Chemo Therapy & Radio Therapy
• addition of PET to CT can improve specificity and accuracy of non-invasive
staging
Barium swallow:
• can delineate proximal and distal margins as well as TEF
• Helpful for correlation with simulation film.
Bronchoscopy: rule-out fistula in midesophageal lesions.
Routine Investigations: CBC, chemistries, LFTs.
Evolution of treatment
Non surgical treatment
• Radiation therapy alone
• Combined modality therapy(CT+RT)
• Intensification of the radiation dose
Surgical treatment
• Sx alone
• Sx+adjuvant
• Preop CT + Sx
Surgery
Esophagectomy: Broad Principles
Depends on
• Site of disease
• Extent of disease involvement
• Co-morbid conditions
• Patient preference
• (May depend on) Histology
• Mainstay of treatment for all resectable disease
• T4b disease is non resectable disease.
Esophagectomy: Broad Principles
• A 5 cm margin cranio-caudally should be obtained to ensure negative final
microscopic margins.
• Thus not performed for cervical esophagus.
• May be performed for primaries of the upper-third thoracic esophagus
depending on location.
• The stomach is considered by the replacement conduit of choice for the
resected esophagus.
Types of Surgery
Transhiatal esophagectomy: for tumors anywhere in esophagus or
gastric cardia. No thoracotomy. Blunt dissection of the thoracic esophagus.
Left with cervical anastomosis. Limitations are lack of exposure of
midesophagus and direct visualization and dissection of the subcarinal LN
cannot be performed.
Right thoracotomy (Ivor-Lewis procedure): good for exposure of mid
to upper esophageal lesions. Left with thoracic or cervical anastomosis.
Left thoracotomy: appropriate for lower third of esophagus and gastric
cardia. Left with low-to-midthoracic anastomosis.
Types of Surgery
Non-Surgical treatment
Radiotherapy and/or Chemotherapy
Chemotherapy
• Regimens
Radiotherapy (with or without chemotherapy)
• Neoadjuvant
• Postoperative
• Definitive
• Palliative
You might also like
- Medical-Surgical Questions With Rationale 70 QuestionsDocument59 pagesMedical-Surgical Questions With Rationale 70 QuestionsJam Torres100% (7)
- Casestudy Gastric CarcinomaDocument56 pagesCasestudy Gastric CarcinomaMJ Amarillo92% (12)
- Fast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeFrom EverandFast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeNo ratings yet
- HLTC 24Document5 pagesHLTC 24elmaNo ratings yet
- Acute Arterial OcclusionDocument44 pagesAcute Arterial OcclusionAlbertus Maria Henry SantosoNo ratings yet
- 42 EsophagusDocument49 pages42 EsophagusShiva BhandariNo ratings yet
- Colorectal Ca (CRC) .: Malueth Abraham, MBCHB ViDocument36 pagesColorectal Ca (CRC) .: Malueth Abraham, MBCHB ViMalueth AnguiNo ratings yet
- DysphagiaDocument40 pagesDysphagiamanabdebuNo ratings yet
- Esophageal CancerDocument42 pagesEsophageal Cancerapi-1964133750% (2)
- Colon and Rectal CancerDocument62 pagesColon and Rectal CancerSK TalkNo ratings yet
- Rectal Cancer OverviewDocument8 pagesRectal Cancer OverviewMihaela RosuNo ratings yet
- Esophageal CADocument56 pagesEsophageal CAEdwin OkonNo ratings yet
- Colorectal Carcinoma SurgeryDocument19 pagesColorectal Carcinoma SurgeryDaanishNo ratings yet
- Upper Git TumorsDocument51 pagesUpper Git TumorsIsaac MwangiNo ratings yet
- Faculty of Medicine NR - Ii Department of Surgery NR - Ii: Diseases of The Biliary TractDocument40 pagesFaculty of Medicine NR - Ii Department of Surgery NR - Ii: Diseases of The Biliary TractGalina LozovanuNo ratings yet
- CasediscussionDocument30 pagesCasediscussionFernando AnibanNo ratings yet
- CA OesophagusDocument47 pagesCA OesophagusAnsif KNo ratings yet
- Esophageal CarcinomaDocument34 pagesEsophageal Carcinomaapi-19916399100% (1)
- CarcinomarectumDocument45 pagesCarcinomarectumHuzefa MemonNo ratings yet
- Carcinoma Esophagus: Presented byDocument59 pagesCarcinoma Esophagus: Presented byBayarbaatar BoldNo ratings yet
- Case Presentation: by DR SaleemDocument61 pagesCase Presentation: by DR SaleemsandeepNo ratings yet
- Carcinomaoesophagus 120403111516 Phpapp02Document59 pagesCarcinomaoesophagus 120403111516 Phpapp02Koushik Reddy PodduturiNo ratings yet
- CA EsophagusDocument37 pagesCA EsophagusElandha PutriNo ratings yet
- GastriccancerDocument65 pagesGastriccancerSHIVAJINo ratings yet
- Management of Rectal Cancer... by DR Kassahun GirmaDocument50 pagesManagement of Rectal Cancer... by DR Kassahun GirmaKassahun Girma Gelaw100% (1)
- Gastric Carcinoma: H. Pylori InfectionDocument7 pagesGastric Carcinoma: H. Pylori InfectionMuvenn KannanNo ratings yet
- Colorectal CADocument76 pagesColorectal CANur Insyirah100% (2)
- Casestudy Gastric CarcinomaDocument53 pagesCasestudy Gastric CarcinomaAngelaTrinidadNo ratings yet
- Dr. E. J. Arteen F.R.C.S General & Colorectal Consultant Surgeon European-Gaza HospitalDocument83 pagesDr. E. J. Arteen F.R.C.S General & Colorectal Consultant Surgeon European-Gaza Hospitalpt.mahmoudNo ratings yet
- Carcinomagallbladder PDFDocument61 pagesCarcinomagallbladder PDFZaki DhiifNo ratings yet
- Management of Colon Cancers-1Document110 pagesManagement of Colon Cancers-1Edwin OkonNo ratings yet
- C4 A Rectal MassDocument2 pagesC4 A Rectal MassgeorgedejeuNo ratings yet
- Rectal Ca:: Malueth Abraham, MBCHB ViDocument32 pagesRectal Ca:: Malueth Abraham, MBCHB ViMalueth AnguiNo ratings yet
- CA Esophagus-Presentation and Its Diagnosis 1Document57 pagesCA Esophagus-Presentation and Its Diagnosis 1Usmle GuyNo ratings yet
- Gastric Cancer by BalaDocument17 pagesGastric Cancer by BalaArundeep AsaithambiNo ratings yet
- Anal CarcinomaDocument6 pagesAnal CarcinomaLouis FortunatoNo ratings yet
- Carcinoma EsophagusDocument47 pagesCarcinoma Esophagusyashwanth bNo ratings yet
- 04 Esophageal TumorsDocument36 pages04 Esophageal TumorsDetty NoviantyNo ratings yet
- Esmo Guidline: Presentasi Oleh: Dr.I Nyoman Dwija Putra SP.BDocument45 pagesEsmo Guidline: Presentasi Oleh: Dr.I Nyoman Dwija Putra SP.BIrbah NabilaNo ratings yet
- Gall Bladder CarcinomaDocument29 pagesGall Bladder CarcinomaUsman FarooqNo ratings yet
- General Consideration in EsophagectomyDocument4 pagesGeneral Consideration in EsophagectomyDabessa MosissaNo ratings yet
- Oesophageal Carcinoma: Dr. Malghalara Khan PGR, Surgical D Unit, KTHDocument50 pagesOesophageal Carcinoma: Dr. Malghalara Khan PGR, Surgical D Unit, KTHMalgh Kh100% (2)
- Common Bile Duct Stones StrictureDocument48 pagesCommon Bile Duct Stones StrictureSyarif MalawatNo ratings yet
- Neoplasmsofoesophagus 230619112311 Dfc34b23Document59 pagesNeoplasmsofoesophagus 230619112311 Dfc34b23Dharmdev YadavNo ratings yet
- Esophageal CancerDocument23 pagesEsophageal Cancerabhandlung100% (3)
- Gastric CancerDocument7 pagesGastric CancerMicah PingawanNo ratings yet
- Carcinoma Rectum - Janak - NEWDocument74 pagesCarcinoma Rectum - Janak - NEWTowhidulIslamNo ratings yet
- Colorectal CancerDocument7 pagesColorectal Cancerjames garciaNo ratings yet
- Esophageal CancerDocument66 pagesEsophageal Canceroezeamuzie100% (1)
- Appendicitis: Hamzeh Halawani M.D. American University of BeirutDocument17 pagesAppendicitis: Hamzeh Halawani M.D. American University of BeirutSilvana María Espinoza CuadrosNo ratings yet
- Journal Reading SurgeryDocument21 pagesJournal Reading Surgerydr.liraNo ratings yet
- Cholangiocarcinoma: R.KarthikeyanDocument49 pagesCholangiocarcinoma: R.KarthikeyanKarthikeyan R100% (2)
- Colon, Rectum and Anus-Dr. SigitDocument121 pagesColon, Rectum and Anus-Dr. SigitYuliana Latif100% (1)
- Gis 1 EnglishDocument85 pagesGis 1 Englishexand861No ratings yet
- Oesphageal Cancer: DR Ka NaiduDocument48 pagesOesphageal Cancer: DR Ka NaiduKISHAN NAIDUNo ratings yet
- Periampullary CarcinomaDocument35 pagesPeriampullary Carcinomaminnalesri100% (2)
- 17-09-2019 Lower GI FINALDocument32 pages17-09-2019 Lower GI FINALNaima HabibNo ratings yet
- Malignant Liver Tumors Undergrad 6th Year Students SharaanDocument56 pagesMalignant Liver Tumors Undergrad 6th Year Students SharaanMohamed AhmedNo ratings yet
- Pancreatic TumorDocument28 pagesPancreatic TumorAli AtiaNo ratings yet
- Surgery - Oral ExamDocument37 pagesSurgery - Oral ExamShidev100% (1)
- MalarDocument41 pagesMalarமணிகண்டன் ராஜேந்திரன்No ratings yet
- Dysphagia, Caustic Ingestion and Esophageal StricturesDocument86 pagesDysphagia, Caustic Ingestion and Esophageal Stricturesmomodou s jallow100% (1)
- Congenital Anorectal Anomalies: DR Jose Antonio Hernandez LivenDocument30 pagesCongenital Anorectal Anomalies: DR Jose Antonio Hernandez Livenmomodou s jallowNo ratings yet
- Dr. Lamin B.A Jaiteh General SurgeryDocument17 pagesDr. Lamin B.A Jaiteh General Surgerymomodou s jallowNo ratings yet
- Hirschsprung'S Disease: DR: Jose Antonio Hernandez LivenDocument32 pagesHirschsprung'S Disease: DR: Jose Antonio Hernandez Livenmomodou s jallowNo ratings yet
- Benign Prostatic HyperplasiaDocument36 pagesBenign Prostatic Hyperplasiamomodou s jallowNo ratings yet
- Efficient Osteoporosis and Skeletal Complications TreatmentDocument4 pagesEfficient Osteoporosis and Skeletal Complications TreatmentĐinh Hoàng Đoan NhãNo ratings yet
- Full Ebook of Tumor Board Review Evidence Based Case Reviews and Questions Francis P Worden Martha P Mims Helen K Chew Online PDF All ChapterDocument69 pagesFull Ebook of Tumor Board Review Evidence Based Case Reviews and Questions Francis P Worden Martha P Mims Helen K Chew Online PDF All Chapterfrancespool751681100% (5)
- Du 9Document1 pageDu 9BDI92No ratings yet
- Hardness in Drinking-Water: Background Document For Development of WHO Guidelines For Drinking-Water QualityDocument9 pagesHardness in Drinking-Water: Background Document For Development of WHO Guidelines For Drinking-Water QualityLionel TaneoNo ratings yet
- Investigation For Hoarseness and StridorDocument30 pagesInvestigation For Hoarseness and Stridormohd-khairil-anwar-ramli-2048No ratings yet
- Accordion Sign-Appearance (C. Difficile)Document41 pagesAccordion Sign-Appearance (C. Difficile)Andra HijratulNo ratings yet
- 2013 Mets Media GuideDocument564 pages2013 Mets Media Guidejen_rogers295No ratings yet
- AmoebiasisDocument5 pagesAmoebiasisyondaime268875No ratings yet
- Neuro-Oncology AdvancesDocument8 pagesNeuro-Oncology AdvancesYESSELYS SILVERANo ratings yet
- Multimedia Presentation Breast FeedingDocument58 pagesMultimedia Presentation Breast Feedingsusie eusebius mudiNo ratings yet
- Trematodes and Their Intermediate HostDocument1 pageTrematodes and Their Intermediate HostKriziaoumo P. OrpiaNo ratings yet
- Intestinal Obstruction: Dr. Mohammad Jamil AlhashlamonDocument19 pagesIntestinal Obstruction: Dr. Mohammad Jamil AlhashlamonBheru LalNo ratings yet
- Chemistry Investigatory Project ABSDocument18 pagesChemistry Investigatory Project ABS11th Batch LegendzNo ratings yet
- AMSOIL Material Safety Data Sheet: Component Cas Number % by WTDocument6 pagesAMSOIL Material Safety Data Sheet: Component Cas Number % by WTapi-19921780No ratings yet
- Radiation ApplicationAERBausOct2010Document94 pagesRadiation ApplicationAERBausOct2010Vallabh SinghNo ratings yet
- The Scalp and Skin of The FaceDocument31 pagesThe Scalp and Skin of The FacewillyoueverlovemenkNo ratings yet
- Veterans Hearing Loss Physician EvaluationDocument5 pagesVeterans Hearing Loss Physician Evaluationjim912No ratings yet
- Serrapeptase Book Edition 4 WebDocument358 pagesSerrapeptase Book Edition 4 WebIvan Curcio100% (2)
- Spherocytosis AyurvedaDocument4 pagesSpherocytosis AyurvedaSameer HusainNo ratings yet
- BM 8-9 OncogenesisDocument139 pagesBM 8-9 OncogenesisabdullahshiddiqadamNo ratings yet
- Philippines - Bridging Care To The Barangay-1Document2 pagesPhilippines - Bridging Care To The Barangay-1Richard ErickNo ratings yet
- FC Urol (SA) Final Past Papers - 2011 Mar 26-3-2014Document3 pagesFC Urol (SA) Final Past Papers - 2011 Mar 26-3-2014matentenNo ratings yet
- Renal Cell Carcinoma: DR Kalyan K Sarkar Ms FrcsedDocument38 pagesRenal Cell Carcinoma: DR Kalyan K Sarkar Ms FrcsedMichael ParkNo ratings yet
- British Association of Dermatologists and British Photodermatology Group Guidelines For Narrowband Ultraviolet B Phototherapy 2022Document14 pagesBritish Association of Dermatologists and British Photodermatology Group Guidelines For Narrowband Ultraviolet B Phototherapy 2022Pietro PensoNo ratings yet
- Daftar PustakaDocument3 pagesDaftar Pustakanurul ayu pratiwiNo ratings yet
- Diagnostic Imaging Chest 3Rd Edition Melissa L Martinez Jimenez Santiago Rosado de Christenson Full ChapterDocument67 pagesDiagnostic Imaging Chest 3Rd Edition Melissa L Martinez Jimenez Santiago Rosado de Christenson Full Chapterbenito.burnett216100% (17)
- Answers To Virology MCQ Paper 3Document7 pagesAnswers To Virology MCQ Paper 3bmhsh100% (6)