Professional Documents
Culture Documents
Food (Seafood) Borne Outbreaks: R.Varidianto Yudo T., dr.,M.Kes
Food (Seafood) Borne Outbreaks: R.Varidianto Yudo T., dr.,M.Kes
Uploaded by
Akasorachi0 ratings0% found this document useful (0 votes)
9 views21 pagesThis document discusses several pathogens that can cause foodborne illness from seafood, including Vibrio species, Salmonella, Shigella, and Clostridium botulinum. It provides details on the clinical features of infections, modes of transmission, laboratory diagnosis, and prevention strategies. Contamination of seafood can occur during harvest from polluted waters or during processing, storage, and handling. Thorough cooking and proper handling/processing of seafood can reduce the risk of illness.
Original Description:
Outbreak disease should hve been concerned
Original Title
128708_Outbreak Disease
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses several pathogens that can cause foodborne illness from seafood, including Vibrio species, Salmonella, Shigella, and Clostridium botulinum. It provides details on the clinical features of infections, modes of transmission, laboratory diagnosis, and prevention strategies. Contamination of seafood can occur during harvest from polluted waters or during processing, storage, and handling. Thorough cooking and proper handling/processing of seafood can reduce the risk of illness.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
9 views21 pagesFood (Seafood) Borne Outbreaks: R.Varidianto Yudo T., dr.,M.Kes
Food (Seafood) Borne Outbreaks: R.Varidianto Yudo T., dr.,M.Kes
Uploaded by
AkasorachiThis document discusses several pathogens that can cause foodborne illness from seafood, including Vibrio species, Salmonella, Shigella, and Clostridium botulinum. It provides details on the clinical features of infections, modes of transmission, laboratory diagnosis, and prevention strategies. Contamination of seafood can occur during harvest from polluted waters or during processing, storage, and handling. Thorough cooking and proper handling/processing of seafood can reduce the risk of illness.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 21
R.Varidianto Yudo T., dr.,M.Kes.
Departemen Mikrobiologi
Fakultas Kedokteran
Universitas Hang Tuah
FOOD (SEAFOOD) BORNE
OUTBREAKS
Outbreak
When two or more people get the same
illness from the same contaminated food or
drink, the event is called a foodborne disease
outbreak.
A series of events occurs between the time a
person is infected and the time public health
officials can determine that the person is part
of an outbreak.
Vibrio species
Vibrio organisms are Gram-negative, halophilic bacteria that are
widespread and naturally present in marine and estuarine
environments.
Environmental factors influence their growth, and their numbers are
highest when the water is warm.
The genus Vibrio includes 30 species, of which at least 14 are recognized
as pathogenic in humans.
Vibrio infections are acquired through ingestion of contaminated
seafood or through exposure of an open wound to seawater.
Vibrioparahaemolyticus and Vibrio vulnificus are the species most
commonly associated with reported infection.
V. parahaemolyticus has been associated with sporadic infections and
outbreaks of gastroenteritis, while V. vulnificus infections occur almost
exclusively as sporadic cases in the United States
Clinical features most often associated with V.parahaemolyticus
infection include watery diarrhea, abdominal cramps, nausea, and
vomiting; wound infections and septicemia occur less commonly.
V. vulnificus is particularly virulent, especially among patients with
liver disease and iron storage disorders, who are at increased risk
of invasive disease.
V. vulnificus infections can lead to sepsis and severe wound
infections.
Severe infections, such as bloodstream and wound infections,
require prompt antimicrobial therapy.
The case fatality rate is about 50% for bloodstream infections and
25% for wound infections.
Laboratory diagnosis is made by isolation of
the organism from clinical specimens,
including blood, stool, and wound samples.
Because they can be overlooked on standard
agar plates, Vibrio organisms in stool or
wound samples are best identified on
selective media, such as thiosulfate-citrate-
bile salts-sucrose (TCBS) agar
Cases of Vibrio infections have a marked seasonal distribution;
most occur during summer and early fall, corresponding to the
period of warmer temperatures.
Almost all cases of food-borne Vibrio infection are associated
with a recent history of seafood consumption, primarily raw
oyster consumption.
Like other organisms found in water, vibrios can be concentrated
in the tissues of filter-feeding bivalve mollusks.
Measures to prevent food-borne Vibrio infections include
consumer education regarding the dangers of eating raw or
undercooked shellfish, particularly among persons with medical
conditions, such as liver disease, that predispose them to severe
illness.
Thoroughly cooking shellfish and preventing raw seafood from
cross-contaminating other foods are effective measures for
consumers to reduce risk.
Regulatory control measures have included monitoring of
harvest waters and microbiological sampling of oysters.
However, it is important that the presence of vibrios is not
associated with fecal contamination.
Therefore, monitoring waters for fecal coliform bacteria is not
effective as an indicator of the presence of Vibrio in harvest
environments.
Finally, postharvest processing methods, such as high-pressure
treatment, irradiation, quick-freezing, and pasteurization, are
available to make oysters safer.
Vibrio infections are reportable to state health departments, and
traceback of oysters associated with human Vibrio infection is
strongly encouraged
Salmonella
Salmonellae are Gram-negative bacilli.
Approximately 2,500 Salmonella serotypes have been identified,
causing a variety of clinical syndromes ranging from
asymptomatic carriage to invasive disease.
Salmonella most commonly causes acute gastroenteritis, with
symptoms including diarrhea, abdominal cramps, and fever.
Other clinical manifestations can include enteric fever, urinary
tract infections, bacteremia, and severe focal infections.
Isolation of Salmonella organisms from cultures of stool, blood,
or other clinical samples is diagnostic; isolates are referred to
public health laboratories for serotype characterization.
Salmonella is a leading cause of food-borne illness, causing
approximately 1.4 million illnesses annually in the United States.
Incidence is highest among infants and the elderly, and infections are
more likely to occur during summer and early fall.
Each Salmonella serotype has its individual biology and ecological niche.
Many natural reservoirs for the different Salmonella serotypes have been
identified.
Humans are the only known reservoir for Salmonella serotype Typhi;
many animal hosts (birds, reptiles, and mammals) serve as reservoirs for
nontyphoidal serotypes.
With improvements in sanitation over the past several decades,
Salmonella serotype Typhi went from being the leading cause of
Salmonella infection to becoming relatively uncommon.
However, nontyphoidal Salmonella infections have emerged as a public
health problem since the 1950s
Routes of Salmonella transmission include food-borne and
waterborne routes, person-to-person contact, and contact with
animals, particularly reptiles.
Most cases of nontyphoidal salmonellosis are caused by
ingestion of contaminated food, and outbreaks have been
associated with a wide range of food vehicles in the United
States.
Seafood-associated outbreaks have been caused by fish,
shrimp, oysters, and clams.
Studies to determine the prevalence of Salmonella spp. in
oysters from domestic bays and testing of sampled oysters
from domestic seafood samples by the U.S. Food and Drug
Administration (FDA) have demonstrated the presence of
salmonellae in a variety of fish and shellfish, including seafood
intended for consumption without further preparation upon
distribution, requiring minimal cooking, and shellfish eaten raw.
Fish and shellfish can acquire Salmonella from polluted
waters.
Historically, sewage contamination of shellfish harvest
beds led to large shellfish-associated outbreaks of
Salmonella serotype Typhi infections.
Control measures aimed at detecting contamination of
harvest waters, such as monitoring fecal coliform counts
in these waters, have been effective at reducing the risk of
Salmonella contamination of seafood occurring before
harvest.
Additionally, seafood can become contaminated with
Salmonella during storage and processing.
Salmonella infection can be prevented by adequate
cooking, proper storage and processing after harvest, and
avoidance of cross contamination during seafood handling
Shigella species
Shigella species are Gram-negative bacilli.
Four species have been identified, and clinical presentations vary
by species.
Clinical manifestations of Shigella infection range from watery,
loose stools to more severe symptoms, including fever, abdominal
pain, tenesmus, and bloody diarrhea.
Complications are rare and include seizures in young children,
toxic megacolon, bacteremia, Reiter’s syndrome, and hemolytic-
uremic syndrome.
Diagnosis is made by isolation of Shigella from feces or rectal
swabs.
Cases occur worldwide, in endemic and epidemic forms. Most
cases occur among children aged 10 years.
Humans are the primary reservoir of Shigella.
Transmission occurs through direct or indirect
contact with feces of infected persons.
Shigella infection is highly communicable, because
ingestion of as few as 10 viable organisms is
sufficient for infection to occur.
The low infectious dose contributes to the potential
for large outbreaks.
Outbreaks have been associated with person-to-
person transmission in crowded or unhygienic
environments and with ingestion of contaminated
food and water.
Foods can become contaminated during handling or
preparation by an infected food handler.
With seafood, contamination can occur if seafood is
harvested from sewagecontaminated water, as
occurred in an outbreak caused by consumption of
raw oysters harvested from waters where sewage
was dumped overboard from the oyster harvest
boat.
Shigella organisms can survive outside the host, but
they are killed readily by cooking.
Control strategies to prevent shigellosis associated
with seafood have included monitoring of harvest
water for fecal coliforms, prohibition of harvesting
from sewage-contaminated areas, enforced control
of dumping sewage overboard, and guidelines for
seafood handling in restaurants
Clostridium botulinum
Clostridium botulinum is a sporeforming, anaerobic,
Gram-positive bacillus that is widespread in the
environment.
The bacterium produces a potent neurotoxin under
anaerobic, low-acid conditions.
Seven types of botulism toxin have been identified;
toxin types A, B, and E cause most human illnesses.
Food-borne botulism is caused by the ingestion of
food contaminated with preformed toxin produced
by spores of C.botulinum.
Botulism is characterized by an acute, symmetric,
descending flaccid paralysis.
Early signs and symptoms of botulism often
include cranial nerve palsies, with diplopia, ptosis,
slurred speech, and difficulty swallowing
progressing to descending weakness and paralysis.
Symptoms can progress to cause paralysis of the
respiratory muscles, requiring ventilatory support.
Cases of botulism are rare but serious; an
estimated 60 food-borne cases occur each year in
the United States.
Most cases are sporadic, but foodborne botulism
outbreaks are reported each year.
Food-borne botulism cases are most often associated with home-
canned foods.
Other food vehicles identified in outbreak investigations have
included fermented or salted seafood, potatoes baked in aluminum
foil, garlic in oil, onions held under butter, and homemade salsa.
Most seafood-associated cases are caused by toxin type E, which is
associated most commonly with eating traditional Alaska Native
foods, such as fermented salmon heads, salmon eggs, and blubber
and skin from marine animals (muktuk).
C. botulinum type E spores are commonly found in fish and aquatic
animals, and implicated seafood has been fermented under
anaerobic conditions that favor the germination of C. botulinum.
Measures to prevent seafood-borne botulism have included
educational efforts to promote proper methods to ferment foods
and to boil fermented foods before consumption, especially if they
were stored in tightly sealed plastic or glass containers.
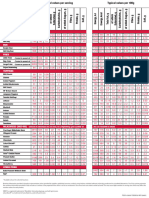
TABLE 1. Seafood-associated outbreaks of infection, by etiology
and seafood commodity, 1973 to 2006 (Modification)
TABLE 1. Seafood-associated outbreaks of infection, by etiology
and seafood commodity, 1973 to 2006 (Modification)
Refference Source
Martha Iwamoto, Tracy Ayers, Barbara E. Mahon, and
David L. Swerdlow. (2010). Epidemiology of Seafood-
Associated Infections in the United States. Clinical
Microbiology Reviews, Vol. 23, No. 2, p. 399–411.
Salmonella-Factsheet CDC : cdc.gov/salmonella
You might also like
- Rudolph PediatricDocument9 pagesRudolph PediatricMuhammad RezaNo ratings yet
- Case Study Salmonella in Caribbean FINALDocument21 pagesCase Study Salmonella in Caribbean FINALGuia PurificacionNo ratings yet
- Free-Living Microorganisms: 5.1 Human Pathogenic Vibrio SpeciesDocument16 pagesFree-Living Microorganisms: 5.1 Human Pathogenic Vibrio SpeciesJin SiclonNo ratings yet
- Food Borne DiseasesDocument9 pagesFood Borne DiseasesaringkinkingNo ratings yet
- Vibrio Parahaemolyticus Food PoisoningDocument4 pagesVibrio Parahaemolyticus Food PoisoninghrNo ratings yet
- Public Health IntroductionDocument13 pagesPublic Health IntroductionMohammed AlwardiNo ratings yet
- English Paper "Gastroenteritis": Manado Health PolytechnicDocument8 pagesEnglish Paper "Gastroenteritis": Manado Health Polytechnicprayitno tabraniNo ratings yet
- Vibrio and Grimontia Hollisae Infections: Investigative Guidelines May 2018Document10 pagesVibrio and Grimontia Hollisae Infections: Investigative Guidelines May 2018PONGSATHORN SITTICHAN (PEUN)No ratings yet
- Shupe AssignmentDocument7 pagesShupe AssignmentBright Kasapo BowaNo ratings yet
- Emergent Treatment of GastroenteritisDocument28 pagesEmergent Treatment of GastroenteritisLaura Anghel-MocanuNo ratings yet
- FURUNCULOSIS Group1Document19 pagesFURUNCULOSIS Group1Yashodha HettiarachchiNo ratings yet
- Infectious DiseaseDocument200 pagesInfectious DiseaseSyed Faayez KaziNo ratings yet
- 1 s2.0 S2090123210000743 Main PDFDocument12 pages1 s2.0 S2090123210000743 Main PDFcamilaNo ratings yet
- Integrated Pest ManagementDocument3 pagesIntegrated Pest Managementvignesh9489No ratings yet
- Articulo E.coliDocument19 pagesArticulo E.coliHelio GrullónNo ratings yet
- MODULE 12 - Foodborne DiseasesDocument16 pagesMODULE 12 - Foodborne DiseasesFil HynneyNo ratings yet
- 11 - Last LectureDocument42 pages11 - Last LectureAl-Homam SalahNo ratings yet
- What Diseases Are Commonly Caused by Wastewater?Document7 pagesWhat Diseases Are Commonly Caused by Wastewater?RimaQuitainNo ratings yet
- Vibrio Parahaemolyticus: Fact SheetDocument2 pagesVibrio Parahaemolyticus: Fact SheetPONGSATHORN SITTICHAN (PEUN)No ratings yet
- Other Gram Negative Enteric PathogensDocument51 pagesOther Gram Negative Enteric Pathogensyosef awokeNo ratings yet
- Disease Trasmitted From Fish To HumanDocument6 pagesDisease Trasmitted From Fish To HumanDr.Kedar Karki ,M.V.Sc.Preventive Vet.Medicine CLSU Philippines100% (5)
- Food Borne DiseasesDocument42 pagesFood Borne DiseasesJesse LeeNo ratings yet
- 142 P - Introductory-Food-Microbiology-FDocument142 pages142 P - Introductory-Food-Microbiology-FdrjoyloverNo ratings yet
- Food Borne Diseases:: Dr. Amr El-Dakroury Dept. of Medical Commission Supreme Council of HealthDocument42 pagesFood Borne Diseases:: Dr. Amr El-Dakroury Dept. of Medical Commission Supreme Council of Healthhadi yusufNo ratings yet
- Vibrio SheetDocument2 pagesVibrio SheettaklalaNo ratings yet
- Microbial Diseases - Digestive SystemDocument200 pagesMicrobial Diseases - Digestive SystemNolan Cabral100% (2)
- BackgroundDocument12 pagesBackgroundDii AnneNo ratings yet
- Primer 1531468992 1Document20 pagesPrimer 1531468992 1taklalaNo ratings yet
- Food Safety: Foodborne Illness Disease-Causing GermsDocument22 pagesFood Safety: Foodborne Illness Disease-Causing GermsMariel DelossantosNo ratings yet
- Zoonatic and Non Infectious DiseasesDocument43 pagesZoonatic and Non Infectious DiseasesZyra AbrazadoNo ratings yet
- Gastroenteritis: Saima Alam AfridiDocument23 pagesGastroenteritis: Saima Alam AfridiMahnoor ParvezNo ratings yet
- Yersinia and Vibrio Associated DiseaseDocument19 pagesYersinia and Vibrio Associated DiseaseCurious PersonNo ratings yet
- Final Written ReportDocument5 pagesFinal Written ReportJillianne MoyanoNo ratings yet
- Bacillary DyssenteryDocument9 pagesBacillary DyssenteryZarah Jane Rull NateNo ratings yet
- Pediatrics in Review 2013 SalmonelosisDocument11 pagesPediatrics in Review 2013 SalmonelosisCarlos Elio Polo VargasNo ratings yet
- Drought Awareness Newsletter by SlidesgoDocument61 pagesDrought Awareness Newsletter by SlidesgovetNo ratings yet
- FST-602 Food Safety Bacterial Food Infections (Part-3) Lecture # 5Document18 pagesFST-602 Food Safety Bacterial Food Infections (Part-3) Lecture # 5muqaddasNo ratings yet
- Cryptosporidium ParvumDocument8 pagesCryptosporidium Parvumpray423No ratings yet
- Types of Hazards and Food SafetyDocument5 pagesTypes of Hazards and Food SafetyAarajita ParinNo ratings yet
- Acutegastroenteritis: Nancy S. GravesDocument15 pagesAcutegastroenteritis: Nancy S. GravesEri EriNo ratings yet
- Vibrio CholeraeDocument4 pagesVibrio CholeraeRigobertoNo ratings yet
- Infectious Diarrheal Disease and DehydrationDocument12 pagesInfectious Diarrheal Disease and DehydrationSNo ratings yet
- Makalah B.inggris GasteoenteritisDocument15 pagesMakalah B.inggris GasteoenteritisRahmat YunandaNo ratings yet
- Food Safety HazardDocument7 pagesFood Safety HazardPrithu GoelNo ratings yet
- Amebiasis and Giardiasis-FinalDocument25 pagesAmebiasis and Giardiasis-FinalDaniel AtiehNo ratings yet
- Concept of Food Contamination and Food-Borne IllnessDocument88 pagesConcept of Food Contamination and Food-Borne IllnessSheirra SantosNo ratings yet
- TropicalDocument29 pagesTropicalsuraj rajpurohitNo ratings yet
- Diarrhea Crampy Abdominal Pain Nausea Vomiting: Gastroenteritis CausesDocument7 pagesDiarrhea Crampy Abdominal Pain Nausea Vomiting: Gastroenteritis CausesClefford TagapanNo ratings yet
- Staphylococcus AureusDocument1 pageStaphylococcus AureusHarida WirawatiNo ratings yet
- Pattern of Disease - AlicawayDocument2 pagesPattern of Disease - AlicawayMonica AlicawayNo ratings yet
- Salmonella, Campylobacter, and Enterohaemorrhagic Escherichia ColiDocument3 pagesSalmonella, Campylobacter, and Enterohaemorrhagic Escherichia ColikharismaNo ratings yet
- Unit 11 Bacterial Food Infections: StructureDocument15 pagesUnit 11 Bacterial Food Infections: StructureShubhendu ChattopadhyayNo ratings yet
- Lection 2 PDFDocument64 pagesLection 2 PDFSanyam KhannaNo ratings yet
- 10 ParasitesDocument10 pages10 ParasitesErin Trisha Kristel GaspanNo ratings yet
- Historical BackgroundDocument4 pagesHistorical Backgroundindra_moniagaNo ratings yet
- Gastroenteritis Bronchopneumonia Ear InfectionDocument34 pagesGastroenteritis Bronchopneumonia Ear InfectionAnn Michelle TarrobagoNo ratings yet
- Concept of Food Contamination and Food-Borne IllnessDocument88 pagesConcept of Food Contamination and Food-Borne IllnessMicah ClearNo ratings yet
- CHAPTER 1-Public Health (Environmental Pollution and Control)Document18 pagesCHAPTER 1-Public Health (Environmental Pollution and Control)muhdakmaladnan100% (4)
- The Big Book of Infectious Disease Trivia: Everything You Ever Wanted to Know about the World's Worst Pandemics, Epidemics and DiseasesFrom EverandThe Big Book of Infectious Disease Trivia: Everything You Ever Wanted to Know about the World's Worst Pandemics, Epidemics and DiseasesNo ratings yet
- Cellulitis Rrapi, R.Document13 pagesCellulitis Rrapi, R.AkasorachiNo ratings yet
- Knee OADocument29 pagesKnee OAAkasorachiNo ratings yet
- Pemeriksaan Tulang BelakangDocument4 pagesPemeriksaan Tulang BelakangAkasorachiNo ratings yet
- Agents of Quarantine Diseases 02Document15 pagesAgents of Quarantine Diseases 02AkasorachiNo ratings yet
- Jurnal Sirosis MalaysiaDocument11 pagesJurnal Sirosis MalaysiaAkasorachiNo ratings yet
- Geriatric MedicineDocument3 pagesGeriatric MedicineAkasorachiNo ratings yet
- SM 20Document1 pageSM 20MUBASHIRNo ratings yet
- Multiple Choice: Test:Topic 6 Cooking PoultryDocument5 pagesMultiple Choice: Test:Topic 6 Cooking Poultrynurin.shNo ratings yet
- SOAL Kelas 8 DAN KUNCI PTS2 - BHS ING - KLS 8 - 2021-2022Document13 pagesSOAL Kelas 8 DAN KUNCI PTS2 - BHS ING - KLS 8 - 2021-2022rfkdzr27vkNo ratings yet
- Project Digestion of Starch Class 12Document15 pagesProject Digestion of Starch Class 12Shreyash PolNo ratings yet
- Biodiesel From Animal FatDocument5 pagesBiodiesel From Animal FatWeng Keat Chong100% (1)
- I. Choose The Best Answer by Circling A, B, C or DDocument5 pagesI. Choose The Best Answer by Circling A, B, C or DDuy NguyễnNo ratings yet
- 500 Word Essay SampleDocument4 pages500 Word Essay Samplegatxsknbf100% (2)
- Present Perfect - Positive 1: 1) (I / Study / French)Document5 pagesPresent Perfect - Positive 1: 1) (I / Study / French)achsanaauliya22No ratings yet
- Zomato Creative BriefDocument5 pagesZomato Creative Brieflishikajain23No ratings yet
- Административная контрольная работа по английскому (6 класс)Document2 pagesАдминистративная контрольная работа по английскому (6 класс)AlexKubrickNo ratings yet
- Shudz Belaviar: Seienbhe Shud7 O.Cheice O IndinduasDocument11 pagesShudz Belaviar: Seienbhe Shud7 O.Cheice O IndinduasayushiNo ratings yet
- Yokozawa Takafumi No Baai Vol. 1Document86 pagesYokozawa Takafumi No Baai Vol. 1Nirrah Kaye Alonzo AquilesNo ratings yet
- Anatomy LungsDocument4 pagesAnatomy LungsLoreine SinfuegoNo ratings yet
- Guide Lines PackagingDocument98 pagesGuide Lines Packagington_bela4911No ratings yet
- FGUK Nutritional Info - DIGITAL V130421Document1 pageFGUK Nutritional Info - DIGITAL V130421arivannoorvNo ratings yet
- Bad & BSF Sunscreen Fact SheetDocument9 pagesBad & BSF Sunscreen Fact SheetArkadiyNo ratings yet
- Modicare Digital Booklet Hindi April 2022Document21 pagesModicare Digital Booklet Hindi April 2022Digital ChiragNo ratings yet
- Learning The Parts of Speech: Hazel D. Joaquin, PHDDocument21 pagesLearning The Parts of Speech: Hazel D. Joaquin, PHDRose PanaoNo ratings yet
- Test VI Present SimpleDocument2 pagesTest VI Present SimpleSimona Cadar TzicNo ratings yet
- Reading Life in FutureDocument2 pagesReading Life in FutureCarmen Blanco De GraciaNo ratings yet
- English: Use of Direct and Reported SpeechDocument19 pagesEnglish: Use of Direct and Reported SpeechEugenio MuellaNo ratings yet
- Entrepreneurship: Business Plan D'Licious Enterprise Frozen Food and ConfectioneryDocument12 pagesEntrepreneurship: Business Plan D'Licious Enterprise Frozen Food and Confectionerynurul hanizaNo ratings yet
- Planning Design Handbook by FajardopdfDocument345 pagesPlanning Design Handbook by FajardopdfMuscadin MakensonNo ratings yet
- Review Unit 789Document10 pagesReview Unit 789Ngoc AnhNo ratings yet
- ELS - Q2 - Summative Test 2Document6 pagesELS - Q2 - Summative Test 2Lucas GodfreyNo ratings yet
- Science 4 Exam With TosDocument6 pagesScience 4 Exam With TosroseNo ratings yet
- Reading and Writing SkdasillDocument3 pagesReading and Writing SkdasillReza Gunandi FadillahNo ratings yet
- Motivation Model For Alcohol Use (Cox & Klinger)Document14 pagesMotivation Model For Alcohol Use (Cox & Klinger)Angelica BeñaresNo ratings yet
- MS Sas 5 PDFDocument3 pagesMS Sas 5 PDFGwenn SalazarNo ratings yet
- g11 Module 1 in General Chemistry 1pdfDocument39 pagesg11 Module 1 in General Chemistry 1pdfAlthea EdulanNo ratings yet