Professional Documents
Culture Documents
1 JSOF - 2019 - Iyer - Oral - Cancer..
1 JSOF - 2019 - Iyer - Oral - Cancer..
Uploaded by
Wadhe Omara Tobing0 ratings0% found this document useful (0 votes)
29 views40 pagesThis document discusses principles of surgery for recurrent oral cancers. It emphasizes the importance of early diagnosis and aggressive treatment. Surgery is the main curative option but is more challenging due to prior treatment causing tissue fibrosis. Wide excision margins are needed and may require resection of adjacent structures. Reconstruction using free flaps is often necessary. For nodal recurrence, comprehensive neck dissection removing all lymph node levels is recommended. An multidisciplinary approach is critical for managing these difficult recurrent cases.
Original Description:
Original Title
1 JSOF_2019_iyer_oral_cancer..
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses principles of surgery for recurrent oral cancers. It emphasizes the importance of early diagnosis and aggressive treatment. Surgery is the main curative option but is more challenging due to prior treatment causing tissue fibrosis. Wide excision margins are needed and may require resection of adjacent structures. Reconstruction using free flaps is often necessary. For nodal recurrence, comprehensive neck dissection removing all lymph node levels is recommended. An multidisciplinary approach is critical for managing these difficult recurrent cases.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
29 views40 pages1 JSOF - 2019 - Iyer - Oral - Cancer..
1 JSOF - 2019 - Iyer - Oral - Cancer..
Uploaded by
Wadhe Omara TobingThis document discusses principles of surgery for recurrent oral cancers. It emphasizes the importance of early diagnosis and aggressive treatment. Surgery is the main curative option but is more challenging due to prior treatment causing tissue fibrosis. Wide excision margins are needed and may require resection of adjacent structures. Reconstruction using free flaps is often necessary. For nodal recurrence, comprehensive neck dissection removing all lymph node levels is recommended. An multidisciplinary approach is critical for managing these difficult recurrent cases.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 40
Principles of surgery in recurrent oral cancer
Gopal Iyer, MD PhD, FRCS
Acting Chair, Division of Surgical Oncology
Chief, Head and Neck Surgery
Disclosures
• Advisory board, Invitrocue
• “Centre of excellence program”, Johnson & Johnson
• Licensing of patent PCTSG2016-050231 to Vivo Surgical
• Spouse, Ad hoc advisory board, Astra Zeneca
Oral squamous cell cancers
• Prompt diagnosis and accurate staging
• Management priorities in head and neck cancer
– Eradication of disease with prevention of recurrence and prolongation
of survival
– Preservation of function (speech, swallowing, voice, shoulder) and
cosmesis
• Multi-disciplinary setting
Iyer NG et al, Nat Rev Clin Oncol 2018
Oral squamous cell cancers
• General guidelines:
– Stage I and II cancers: single modality therapy
– Stage III and IV cancers: multimodality treatment combining surgery,
followed by radiation therapy +/- chemotherapy
• Mainstay of curative treatment should be SURGERY
– Primary- wide resection
– Cervical lymph nodes- neck dissection elective vs therapeutic
• Radiation therapy (+/- chemo) is second choice: Iyer NG et al, Cancer 2015
– Lack of expertise
– Medical contraindication
– Patient’s will
Recurrent oral cancers
• Essential to diagnose early and institute aggressive treatment
• Recurrent disease is often more difficult to treat than the
original lesion
– Biologically aggressive, potentially radiation-resistant.
– Lack of a fixed pattern of spread
– Limitation of treatment options:
• Patients who have undergone prior irradiation, now have limitations in re-
irradiation dose, field, and greater toxicities.
• Technical difficulties operating in a previously irradiated or operated field
• Higher complication rates associated with salvage surgery
• Frequent need for reconstruction
Recurrent oral cancers
• Early diagnosis is essential
• 80% of recurrences occur within the first 2 years after initial therapy
• Most guidelines recommend surveillance ranging from 1-3
months for first 2 years, depending upon the presenting stage
and the expected risk for recurrence
• Imaging
– inaccessible to physical examination, not amenable to palpation
(fibrosed neck) or visualization
– CT or MRI
– PET scan
Surgery for recurrent oral cancers
• Multi-disciplinary approach is critical
• Depends on several factors:
– Extent of tumor
– Previous treatment modalities used
– Patient co-morbidities and fitness to undergo aggressive therapy
– Expertise available eg plastics expertise impacts on and flap choice for
use in reconstruction
Patterns of disease failure
• Related to original stage and treatment rendered
• Primary site or local failure
SURGERY
• Regional or lymph node recurrence
• Distant metastasis
Primary site or local failure
• Occurs in 20-30% of all patients
• Post-surgery - usually at margins of resection or areas with
devoid of normal fascial barriers (eg tongue musculature)
• Post-radiation - usually at the epicenter of the tumor where
cells are hypoxic, or regions which are inadequately radiated
due to technical errors or marginal misses
Primary site or local failure
• Risk factors:
– Positive surgical margins
– Perineural and lymphovascular invasion
– Depth of invasion
– Subsite of disease
• Eg buccal cancers have a higher propensity to recur locally than floor of
mouth cancers – treatment related?
Case 1
• 45 y.o. male presented with painless left tongue mass
• 3 cm tumor left anterior tongue, mobile
• No cervical lymphadenopathy was palpable.
• Initial staging T2N0M0
• SURGERY: partial glossectomy and SOHD
• Represented 9 months later with:
– worsening pain, trismus and ankyloglossia
– left lateral tongue mass extending to the floor of mouth,fixed to the
lingual surface of the lower gingiva / mandible and to midline
– No overt cervical lymphadenopathy
Physical exam
Imaging- MRI
Imaging- PET/CT
Surgery
• Staged as rT4N0M0
• Rule out distant mets
• Discussed at MDT
• Surgery:
– Segmental mandibulectomy
– Comprehensive neck dissection
– Free ALT flap reconstruction
Surgery
Surgery
Surgery
Principles of surgery for primary site recurrence
• Aggressive approach
• Margins need to be wide, especially within the tongue
musculature- 2 cm soft tissue margins
• Need for wide margins may necessitate resection of adjacent
structures
• Frozen section examination is often used to assess
intraoperative margins
• Concept of compartment resection
Compartment resection for oral cancers- tongue
Compartment resection for oral cancers- RMT/buccal
Compartment resection for oral cancers- RMT/buccal
Compartment resection for oral cancers- RMT/buccal
Principles of surgery for primary site recurrence
• Reconstruction
– Like for like where possible
– Soft tissue is priority
– Free flap preferred (ALT workhorse)
– Pect major is life-saver
• Appropriate treatment for the neck
– Comprehensive dissection or convert selective to comprehensive
Regional or lymph node recurrence
• Occurs in 10-15% of patients
• ?failure to adequately treat nodal basin during primary
treatment
• Redirected / abnormal lymphatic flow following prior therapy
may lead to unpredictable patterns of spread outside of the
treated field
• More likely with aggressive disease that traverses tissue
planes (eg extra-capsular spread of nodal disease)
Regional or lymph node recurrence
• Risk factors:
– Higher number of metastatic nodes
– Larger size of metastatic focus
– Contralateral nodal disease vs. Ipsilateral nodal disease
– Extracapsular spread
– Level of spread: metastases to second and third echelon of nodes
worse outcome than first echelon nodes
• Outside treatment field:
– Parotid, level 2B, occipital, low level 4, central compartment
– contralateral
Case 2
• 58 y.o. male smoker presented with right buccal cancer T2N1
– 2.5 cm level 2 node, irregular margin
• Radiotherapy to primary site and right neck at outside
institution
• Represented 14 months later with:
– Right neck mass
Physical exam
Imaging- CT
Surgery
• Modified radical neck dissection
• Clear level 1-5
• Be radical
• Preserve only if possible
• Single transverse incision
preferred
Surgery- plastysma with node
Surgery- SAN
Surgery-SAN
Surgery-IJV
Surgery-IJV
Surgery
Principles of surgery for nodal recurrence
• Comprehensive neck dissection:
– Post RT- levels 1-5
– Previous surgery- remaining levels
• No role for selective neck dissection
• Aggressive approach:
– Adjacent structures: SCM, IJV, spinal accessory nerve
– Others: external carotid, hypoglossal, phrenic, vagus
– Remove previous scar
– Other muscles
• Carotid sheath is a clean plane
Principles of surgery for nodal recurrence
• Skin coverage where necessary
– Free or pedicled flaps
• Consider contralateral neck
– Level 1 involvement
– Primary tumor crossing midline
• Other tips and pearls:
– nerve monitoring for vagus
– marking suspicious sites with liga clips
– Number of nodes harvested
– Get to the carotid sheath
Summary
• Essential to diagnose early and institute aggressive treatment
• Recurrent disease more difficult to treat than original lesion
• Surgery is only curative option
– Technical difficulties operating in a previously operated/ irradiated
field related to tissue fibrosis and impaired wound healing
• Flap reconstruction may be essential
• Adjuvant therapy including re-irradiation
– Get involved in RT planning
Thank you
gopaliyer@nccs.com.sg
You might also like
- Details of Students Admitted Through NEET PG 2020-21-701 1400Document700 pagesDetails of Students Admitted Through NEET PG 2020-21-701 1400Minerva Medical Treatment Pvt LtdNo ratings yet
- Sample FFS-Final ReportDocument22 pagesSample FFS-Final ReportSuparerk Sirivedin100% (4)
- 24 Olsen Variations ParotidectomyDocument33 pages24 Olsen Variations ParotidectomyAngga Witra NandaNo ratings yet
- 15.oral Premalignant and Malignant ConditionDocument31 pages15.oral Premalignant and Malignant Conditionabhishek chaudharyNo ratings yet
- Presenter: DR Muthulingesh, SR-RO Moderator: DR Shyama Prem, ProfessorDocument51 pagesPresenter: DR Muthulingesh, SR-RO Moderator: DR Shyama Prem, ProfessorGousalyaNo ratings yet
- Salivary Gland Tumors: Marka Crittenden M.D. PH.DDocument54 pagesSalivary Gland Tumors: Marka Crittenden M.D. PH.DNeeti JainNo ratings yet
- Canceroflarynx 161013111800Document35 pagesCanceroflarynx 161013111800Naveen AngamuthuNo ratings yet
- Principles of RadiotherapyDocument41 pagesPrinciples of Radiotherapywabaly100% (1)
- Management of Thyroid CancerDocument57 pagesManagement of Thyroid CancerAshis SahaNo ratings yet
- Treatment of Cancer Surgical PrinciplesDocument28 pagesTreatment of Cancer Surgical PrinciplesrebeccaboukenjNo ratings yet
- Carcinoma Penis: Pravin NarkhedeDocument36 pagesCarcinoma Penis: Pravin Narkhedepravin narkhede100% (1)
- Biology and Principles Of-18Document49 pagesBiology and Principles Of-18megahedhazeemNo ratings yet
- Management of Carcinoma Penis: DR Akhilesh Mishra Senior Resident Radiation Oncology Irch, AiimsDocument51 pagesManagement of Carcinoma Penis: DR Akhilesh Mishra Senior Resident Radiation Oncology Irch, AiimsWirawan Amirul BahriNo ratings yet
- Principles of Surgical Management of Cancer PatientDocument63 pagesPrinciples of Surgical Management of Cancer PatientbashiruaminuNo ratings yet
- MX Protocols Oropharyngeal Malignancy CompatDocument42 pagesMX Protocols Oropharyngeal Malignancy CompatBikram ChoudhuryNo ratings yet
- Extremity STS: Dr. S. Srivatsan Dr. M. Anto, Dr. Thirumuruganand Prof. K.S.Ravishankar UnitDocument66 pagesExtremity STS: Dr. S. Srivatsan Dr. M. Anto, Dr. Thirumuruganand Prof. K.S.Ravishankar UnitArul KumarNo ratings yet
- DR Aamir Advances EntDocument36 pagesDR Aamir Advances EntAamir YousufNo ratings yet
- Recent Advances in Radiation Oncology: DR M Spoorthi Shelometh Department of Radiation OncologyDocument53 pagesRecent Advances in Radiation Oncology: DR M Spoorthi Shelometh Department of Radiation Oncologyspoorthi shelomethNo ratings yet
- Esophageal CarcinomaDocument34 pagesEsophageal Carcinomaapi-19916399100% (1)
- Oral CancerDocument53 pagesOral CancerMugdha FrancisNo ratings yet
- PNET, Pineal TumorsDocument58 pagesPNET, Pineal TumorsGed OlayanNo ratings yet
- London Cancer Head and Neck Radiotherapy Protocol March 2013Document10 pagesLondon Cancer Head and Neck Radiotherapy Protocol March 2013handrionoNo ratings yet
- M Sandamela Salivary Gland SandamelaDocument45 pagesM Sandamela Salivary Gland SandamelaRockson SamuelNo ratings yet
- Evidence-Based Medicine: Facial Skin MalignancyDocument38 pagesEvidence-Based Medicine: Facial Skin MalignancyTonie AbabonNo ratings yet
- Salivary Gland TumoursDocument34 pagesSalivary Gland Tumoursnsv.epicNo ratings yet
- Principles of Cancer Management20022013b.Document62 pagesPrinciples of Cancer Management20022013b.Bashiru AminuNo ratings yet
- Oral Cancer and ManagementDocument148 pagesOral Cancer and ManagementFadilaNo ratings yet
- Laryngeal Mass: John F. Mcguire, MD, MbaDocument33 pagesLaryngeal Mass: John F. Mcguire, MD, MbaIvan DarioNo ratings yet
- Management of Rectal Cancer... by DR Kassahun GirmaDocument50 pagesManagement of Rectal Cancer... by DR Kassahun GirmaKassahun Girma Gelaw100% (1)
- Management of Lung Cancer by DR Abdul-AzizDocument89 pagesManagement of Lung Cancer by DR Abdul-AzizAbdulaziz HassenNo ratings yet
- HN Interstitial BrachyDocument99 pagesHN Interstitial BrachySayan DasNo ratings yet
- Journal Reading Double JohnDocument31 pagesJournal Reading Double JohnCarlos JohnsonNo ratings yet
- Testicular Tumors The EndDocument67 pagesTesticular Tumors The EndRamesh ReddyNo ratings yet
- Head and NeckDocument274 pagesHead and NeckRahul PandaNo ratings yet
- Colorectal Carcinoma: Haryono YarmanDocument18 pagesColorectal Carcinoma: Haryono Yarmanmayones80No ratings yet
- ARTSCANIIIDocument61 pagesARTSCANIIIKishoreChandraKoradaNo ratings yet
- Treatment of Lung NeoplasmsDocument18 pagesTreatment of Lung NeoplasmsVenzNo ratings yet
- Treatment of Gastric Adenocarcinoma: Presented by Rajendra MaharjanDocument45 pagesTreatment of Gastric Adenocarcinoma: Presented by Rajendra MaharjanajNo ratings yet
- Csextcp 2115Document33 pagesCsextcp 2115api-308629385No ratings yet
- Gastriccancer 150312174027 Conversion Gate01Document64 pagesGastriccancer 150312174027 Conversion Gate01torr123No ratings yet
- Laryngeal Recurrence Sites in Patients Previously Treated With Transoral Laser Microsurgery For Squamous Cell CarcinomaDocument24 pagesLaryngeal Recurrence Sites in Patients Previously Treated With Transoral Laser Microsurgery For Squamous Cell CarcinomaMuhammad Tawfiq ZamriNo ratings yet
- Surgical Treatment of Oral Cavity CancersDocument6 pagesSurgical Treatment of Oral Cavity CancersbekkouchealiwalidNo ratings yet
- Basics of Anatomy, Planning, and Delivery: Gastrointestinal CancersDocument77 pagesBasics of Anatomy, Planning, and Delivery: Gastrointestinal CancersgammasharkNo ratings yet
- 13) Traitement Chirurgical Des Cancers de La Cavité BuccaleDocument6 pages13) Traitement Chirurgical Des Cancers de La Cavité BuccalebekkouchealiwalidNo ratings yet
- Radiotherapy in Penile Carcinoma: Dr. Ayush GargDocument32 pagesRadiotherapy in Penile Carcinoma: Dr. Ayush GargMohammad Mahfujur RahmanNo ratings yet
- EBM 2018 - Head and CancersDocument136 pagesEBM 2018 - Head and CancersChandramohan SettyNo ratings yet
- Debulking (Cytoreductive) SurgeryDocument23 pagesDebulking (Cytoreductive) Surgerytsega tilahunNo ratings yet
- X FilesDocument47 pagesX FilespopNo ratings yet
- Carcinoma Penis Management: Dr. Lilamani Rajthala MS Resident Moderator: Dr. Samir ShresthaDocument63 pagesCarcinoma Penis Management: Dr. Lilamani Rajthala MS Resident Moderator: Dr. Samir ShresthaBibek GhimireNo ratings yet
- Gastrointestinal CancerDocument5 pagesGastrointestinal CancerTurky DallolNo ratings yet
- Management of Oral Cavity Bhans-1Document91 pagesManagement of Oral Cavity Bhans-1BhanuNo ratings yet
- ATC Surgical ManaegementDocument6 pagesATC Surgical ManaegementLuciana ThioNo ratings yet
- Acoustic NeuromaDocument23 pagesAcoustic Neuromacefiroth100% (1)
- A Simple BoyDocument13 pagesA Simple BoyJoren FernecitaNo ratings yet
- Case Presentation 2Document20 pagesCase Presentation 2api-390596832No ratings yet
- Rectal Cancer Talk 1228785749826555 9Document54 pagesRectal Cancer Talk 1228785749826555 9Jantima SirisophonwattanaNo ratings yet
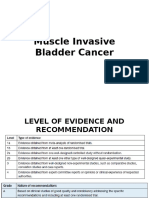
- Muscle Invasive Bladder CancerDocument39 pagesMuscle Invasive Bladder CancerBernardNo ratings yet
- Management of Sinonasal Tumors: Prognostic Factors and Outcomes: A 10 Year Experience at A Tertiary Care HospitalDocument67 pagesManagement of Sinonasal Tumors: Prognostic Factors and Outcomes: A 10 Year Experience at A Tertiary Care HospitalDinaNihayatiNo ratings yet
- Terapi Tumor TelingaDocument25 pagesTerapi Tumor TelingaTitaPuspitasariNo ratings yet
- Thyroid Malignancies: DR Rajesh P SDocument37 pagesThyroid Malignancies: DR Rajesh P SdrrajeshpsmsNo ratings yet
- Medical Imaging Technique and ProceduresFrom EverandMedical Imaging Technique and ProceduresRating: 5 out of 5 stars5/5 (1)
- DR Yadi - Early Breast Cancer JSOF 2019.....Document25 pagesDR Yadi - Early Breast Cancer JSOF 2019.....Wadhe Omara TobingNo ratings yet
- DR DIANI - JSOF - DK - Rev1....Document27 pagesDR DIANI - JSOF - DK - Rev1....Wadhe Omara TobingNo ratings yet
- KASUS 3 Early Staged Breast CancerDocument27 pagesKASUS 3 Early Staged Breast CancerWadhe Omara TobingNo ratings yet
- KASUS 1 Advanced Stage Oral Cancer.Document37 pagesKASUS 1 Advanced Stage Oral Cancer.Wadhe Omara TobingNo ratings yet
- R Walters MimiDocument19 pagesR Walters MimiCalWonkNo ratings yet
- Immobi Ad SpecsDocument32 pagesImmobi Ad SpecsManuj KhuranaNo ratings yet
- MAN 568 - Session 1 - IntroductionDocument25 pagesMAN 568 - Session 1 - IntroductionOnur YamukNo ratings yet
- Structure AnswersDocument7 pagesStructure Answersbunshin AAANo ratings yet
- Chapter 3 Key Points On Process CostingDocument4 pagesChapter 3 Key Points On Process CostingKyeienNo ratings yet
- Heat Treatment Manual Part IIDocument21 pagesHeat Treatment Manual Part IIAnonymous lmCR3SkPrK100% (3)
- Unit 3 - Task 4 - Oral Production - Let's TalkDocument9 pagesUnit 3 - Task 4 - Oral Production - Let's TalkTatiana FrancoNo ratings yet
- 2237-Article Text-7597-1-10-20191021Document8 pages2237-Article Text-7597-1-10-20191021rohmanNo ratings yet
- Student Tox LectureDocument49 pagesStudent Tox Lecturelenin_villaltaNo ratings yet
- H43701 3P Cylinder (Component Parts) (New) ## L1421Dt: Update Date: 28/05/2021 Printing Date: 18/06/2021Document2 pagesH43701 3P Cylinder (Component Parts) (New) ## L1421Dt: Update Date: 28/05/2021 Printing Date: 18/06/2021SpinNo ratings yet
- CXC - Csec - Electrical Electronnics - Sba Booklet 2010Document38 pagesCXC - Csec - Electrical Electronnics - Sba Booklet 2010api-255989257No ratings yet
- Duodenal Stenosis PDFDocument9 pagesDuodenal Stenosis PDFDorcas KafulaNo ratings yet
- Fact Sheet CellD 300 en PDFDocument2 pagesFact Sheet CellD 300 en PDFCharmer JiaNo ratings yet
- DS-2CD2620F-IZ (S) 2.0MP 1/2.7" CMOS ICR Bullet Network CameraDocument4 pagesDS-2CD2620F-IZ (S) 2.0MP 1/2.7" CMOS ICR Bullet Network CameraArun.V1984No ratings yet
- Anti-Arson FormDocument4 pagesAnti-Arson FormLennart AnderssonNo ratings yet
- Mechanisms of NSAID-Induced HepatotoxicityDocument16 pagesMechanisms of NSAID-Induced HepatotoxicityRonald WiradirnataNo ratings yet
- Liturgy Chapter 5Document41 pagesLiturgy Chapter 5Blue macchiatoNo ratings yet
- AirpaxDocument2 pagesAirpaxkaru2275243No ratings yet
- Craig-1977-The Structure of JacaltecDocument442 pagesCraig-1977-The Structure of JacaltecmaclbaisNo ratings yet
- Multiple Choice Practice Questions/Answer For Online/Omr AITT-2020 2 Year Electronics Mech. Trade TheoryDocument66 pagesMultiple Choice Practice Questions/Answer For Online/Omr AITT-2020 2 Year Electronics Mech. Trade TheoryAbcNo ratings yet
- Tech Spec 8mvaDocument40 pagesTech Spec 8mvachekurivishnu7No ratings yet
- KBN Proforma BIWE Welding and Plumbing Materials.Document23 pagesKBN Proforma BIWE Welding and Plumbing Materials.Gilbert KamanziNo ratings yet
- World Islamic Banking Competitiveness Report 2013 - 2014Document84 pagesWorld Islamic Banking Competitiveness Report 2013 - 2014Lena HafizNo ratings yet
- Statistical Softwares: Excel Stata SpssDocument1 pageStatistical Softwares: Excel Stata SpssJeison Manotas ScarpattisNo ratings yet
- Polar I ScopesDocument6 pagesPolar I Scopessaurabh_acmasNo ratings yet
- Catalog: Kawai Music IndonesiaDocument20 pagesCatalog: Kawai Music IndonesiaKhairul UmamNo ratings yet
- FluteDocument8 pagesFlutegiuseppeNo ratings yet
- Acceptability of Banana Cheese Balls For Students in Colegio de Los BanosDocument4 pagesAcceptability of Banana Cheese Balls For Students in Colegio de Los BanosBSED SOCSTUD I-C Manese,JeremyNo ratings yet