Professional Documents
Culture Documents
Acute Renal Failure: Dr. Sami Abdo Radman
Acute Renal Failure: Dr. Sami Abdo Radman
Uploaded by
Adeniran Charles0 ratings0% found this document useful (0 votes)
9 views23 pagesAcute renal failure (ARF) is a sudden decrease in kidney function that results in the buildup of waste products in the blood. It can be caused by decreased renal blood flow, direct kidney damage, or urinary tract obstruction. The main types are prerenal, renal, and postrenal. Prerenal ARF is most common and caused by low blood flow to the kidneys. Renal ARF is usually due to acute tubular necrosis from injury or toxicity. Postrenal ARF results from physical blockage of urine flow. Treatment involves correcting the underlying cause, managing fluid and electrolytes, and potentially dialysis in severe cases.
Original Description:
Original Title
Azotaemia, uraemia
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAcute renal failure (ARF) is a sudden decrease in kidney function that results in the buildup of waste products in the blood. It can be caused by decreased renal blood flow, direct kidney damage, or urinary tract obstruction. The main types are prerenal, renal, and postrenal. Prerenal ARF is most common and caused by low blood flow to the kidneys. Renal ARF is usually due to acute tubular necrosis from injury or toxicity. Postrenal ARF results from physical blockage of urine flow. Treatment involves correcting the underlying cause, managing fluid and electrolytes, and potentially dialysis in severe cases.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
9 views23 pagesAcute Renal Failure: Dr. Sami Abdo Radman
Acute Renal Failure: Dr. Sami Abdo Radman
Uploaded by
Adeniran CharlesAcute renal failure (ARF) is a sudden decrease in kidney function that results in the buildup of waste products in the blood. It can be caused by decreased renal blood flow, direct kidney damage, or urinary tract obstruction. The main types are prerenal, renal, and postrenal. Prerenal ARF is most common and caused by low blood flow to the kidneys. Renal ARF is usually due to acute tubular necrosis from injury or toxicity. Postrenal ARF results from physical blockage of urine flow. Treatment involves correcting the underlying cause, managing fluid and electrolytes, and potentially dialysis in severe cases.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 23
Acute Renal Failure
DR. SAMI ABDO RADMAN
Acute Renal Failure
Definition
Acute renal failure (ARF) is a syndrome
defined as an abrupt decrease in
glomerular filtration rate sufficient to
result in retention of nitrogenous waste
products (blood urea nitrogen [BUN] and
creatinine) and perturbation of
extracellular fluid volume and electrolyte
and acid-base homeostasis
Usually, but not invariably, reversible over a
period of days or weeks.
sufficiently severe to result in uraemia
Oliguria is usually, but not invariably, a
feature.
Cause sudden, life-threatening biochemical
Deterioration in renal function is
disturbances
Is a medical emergency..
Causes
ARF can result from
(1) diseases that cause a decrease of renal blood
flow (prerenal azotemia (
(2diseases that directly involve renal parenchyma
(renal azotemia)
(3) diseases associated with urinary tract
obstruction (postrenal azotemia)
Prerenal uraemia
Is the most common form of ARF
There is impaired perfusion of the kidneys with
blood.
Hypovolaemia,
Hypotension,
Impaired cardiac pump efficiency or
Vascular disease limiting renal blood flow,
Or combinations of these factors
Excretory function in prerenal uraemia improves
once normal renal perfusion has been restored.
CLINICAL MANIFESTATIONS
Thirst, dizziness
Hypotension and tachycardia,
Reduced jugular venous pressure,
Decreased skin turgor,
Dry mucous membranes,
Reduced axillary sweating.
History of intake of hypotensive drugs
Management
Correction of hypovolaemia and
hypotension,
Treatment of the undelying cause
recovery typically takes 1 to 2
weeks after normalization of renal
perfusion
Postrenal uraemia
Obstruction of the urinary tract at any point from the
calyces to the external urethral orifice.
Clinical exam:
Tenderness on the suprabubic region or renal angle
History of stones
History of Prostatic disease
Treatment
Removal of the obstruction
Renal Azotemia
Acute uraemia due to renal
parenchymal disease (Acute tubular
necrosis, ATN)
This is most commonly due to acute
renal tubular necrosis (Due to acute
ischemic or nephrotoxic insult)
Causes
Haemorrhage
Burns
Diarrhoea and vomiting
Diuretics
Myocardial infarction
Congestive cardiac failure
Snake bite
Myoglobinaemia
Haemoglobinaemia
(due to haemolysis, e.g. in falciparum
malaria, 'blackwater fever)
Hepatorenal syndrome
Drugs, e.g. aminoglycosides, NSAIDs,
ACE inhibitors
N.B:
In liver failure, acute renal result from rapidly reversible
vasomotor abnormalities within the kidney.
A kidney removed from a patient with hepatic cirrhosis
and liver failure dying with oliguric renal failure may
function normally immediately after transplantation into a
normal individual
Pathogenesis
Intrarenal microvascular
vasoconstriction:
Tubular cell injury
Ischaemic injury results in rapid depletion
of intracellular ATP stores resulting in cell
death
Glomerular contraction reducing the
surface area available for filtration
Obstruction of the tubule by debris
shed from ischaemic tubular cells
Clinical Course
Depending on the severity and duration of the
renal insult.
Oliguria is common in the early stages: non-
oliguric renal failure is usually a result of a less
severe renal insult.
Recovery of renal function typically occurs after
7-21 days,
ATN may last for up to 6 weeks, even after a
relatively short-lived initial insult
Clinical and biochemical features
The features of the causal condition
together with features of rapidly
progressive uraemia
serum urea and creatinine
concentrations depend upon the rate of
tissue breakdown(trauma, sepsis and
surgery)
Pulmonary oedema
Symptoms of uraemia such as
anorexia,
nausea, vomiting
pruritus develop,
drowsiness, fits, coma and haemorrhagic
episodes.
Epistaxes and gastrointestinal haemorrhage
Severe infection may have initiated the acute
renal failure or have complicated it owing to the
( impaired immune defences)
URINALYSIS in ARF
Anuria suggests complete urinary tract
obstruction OR severe cases of prerenal or
intrinsic renal ARF
Wide fluctuations in urine output raise the
possibility of intermittent obstruction,
Polyuria in partial urinary tract obstruction
Transparent hyaline casts In prerenal ARF,
(secreted by epithelial cells of the loop of Henle)
Hematuria and pyuria are common in patients with
intraluminal obstruction or prostatic disease.
Epithelial casts present in ATN (ischemic or
nephrotoxic ARF)
Red blood cell casts indicate glomerular injury
Eosinophiluria is common in
antibiotic-induced allergic interstitial
nephritis
Bilirubinuria may provide a clue to
the presence of hepatorenal syndrome.
Urine should be tested for free
haemoglobin and myoglobin,
Laboratory findings in ARF
Blood tests include measurement of serum
urea, electrolytes, creatinine, calcium,
phosphate, albumin,
Increase serum Creatinine
Hyperkalemia, hyperphosphatemia,
hypocalcemia
Severe anemia in the absence of hemorrhage
indicates hemolysis
Systemic eosinophilia suggests allergic
interstitial nephritis
RADIOLOGICAL
INVESTIGATIONS
A plain film of the abdomen
Ultrasonography
Pelvicalyceal dilatation is usual
with urinary tract obstruction
Retrograde or anterograde
pyelography
Management
General measures
Consistent documentation of fluid intake and output,
Measurement of daily bodyweight
Emergency measures
Correction of acidosis with intravenous sodium
bicarbonate
Pulmonary oedema Duiretics
Treatment of sepsis
Fluid and electrolyte balance
Diet
Protien restriction (40 gm daily)
sodium and potassium restriction
Management …cont
Dialysis is indicated in
Symptoms of uraemia
Complications of uraemia, such as pericarditis
Hyperkalaemia not controlled by conservative measures
Pulmonary oedema
Severe acidosis
For removal of drugs causing the acute renal failure, e.g.
Gentamicin, lithium, severe aspirin overdose.
You might also like
- Oral Physiology and Occlusion ReviewerDocument100 pagesOral Physiology and Occlusion ReviewerNUELLAELYSSE DELCASTILLO100% (3)
- Acute Renal FailureDocument33 pagesAcute Renal FailureAqsa Akbar AliNo ratings yet
- Acute Renal FailureDocument34 pagesAcute Renal Failureaibaloca67% (9)
- Lecture - Acute Renal FailureDocument57 pagesLecture - Acute Renal FailureJames StiltonNo ratings yet
- Acute Kidney InjuryDocument21 pagesAcute Kidney InjuryAtif Gazali100% (1)
- ACUTE AND CHRONIC RENAL FailureDocument15 pagesACUTE AND CHRONIC RENAL Failuremaggayj11100% (1)
- Acrf CDocument70 pagesAcrf CHussain AzharNo ratings yet
- Acute Renal Failur E: By: Miss Santoshi Naik Assistant Professor Yenepoya Pharmacy College & Research CentreDocument15 pagesAcute Renal Failur E: By: Miss Santoshi Naik Assistant Professor Yenepoya Pharmacy College & Research CentreAnusikta PandaNo ratings yet
- ACUTE RENAL FAILURE-JessicaDocument8 pagesACUTE RENAL FAILURE-JessicaCarolina JaeZeeNo ratings yet
- Acute Kidney InjuryDocument23 pagesAcute Kidney InjuryBaraka SayoreNo ratings yet
- Acute Renal FailureDocument31 pagesAcute Renal FailureODONG MARTINNo ratings yet
- College of Nursing: Civil HospitalDocument15 pagesCollege of Nursing: Civil HospitalDipal Jignesh PatelNo ratings yet
- Acute Kidney InjuryDocument21 pagesAcute Kidney InjuryLALITH SAI KNo ratings yet
- Acute Kidney Injury Md3Document24 pagesAcute Kidney Injury Md3juliuskahabi1No ratings yet
- Learning Issue: Acute Kidney InjuryDocument6 pagesLearning Issue: Acute Kidney InjuryAnnisa WidjanarkoNo ratings yet
- Acute Kidney Injury: Hailemariam Bekele Hayelom MichaelDocument77 pagesAcute Kidney Injury: Hailemariam Bekele Hayelom MichaelShafira WidiaNo ratings yet
- Inter'Medic AKIDocument48 pagesInter'Medic AKIMAHEJS HDNo ratings yet
- Renal Diseaseppt2789Document112 pagesRenal Diseaseppt2789Sundeep SharmaNo ratings yet
- Acute Renal FailureDocument28 pagesAcute Renal FailureAs SyarifNo ratings yet
- Acute-Renal-Failure Lecture OnlyDocument17 pagesAcute-Renal-Failure Lecture OnlyeyesontheskyNo ratings yet
- Presented By: Sonia Dagar: Renal FailureDocument40 pagesPresented By: Sonia Dagar: Renal FailureRavanshi ThakurNo ratings yet
- Acute Renal Failure: Presented by Peter Fumo, MD, FACPDocument20 pagesAcute Renal Failure: Presented by Peter Fumo, MD, FACPlagathurcNo ratings yet
- Acute Renal FailureDocument38 pagesAcute Renal Failurechesang507No ratings yet
- Acute Renal FailureDocument9 pagesAcute Renal FailureananNo ratings yet
- Acute Renal FailureDocument13 pagesAcute Renal FailureGlorianne Palor100% (2)
- Acute Renal FailureDocument101 pagesAcute Renal FailureRowshon AraNo ratings yet
- Aki (New)Document40 pagesAki (New)Mithun GowdaNo ratings yet
- Acute Renal FailureDocument6 pagesAcute Renal FailureNaqash NobleNo ratings yet
- Renal Calculi & Renal FailureDocument17 pagesRenal Calculi & Renal Failureazlan100% (1)
- Acute Kidney InjuryDocument20 pagesAcute Kidney InjuryTishya MukherjeeNo ratings yet
- Acute Kidney FailureDocument1 pageAcute Kidney FailureiizamuddinNo ratings yet
- Acute Renal FailureDocument6 pagesAcute Renal Failurearif kurnia timurNo ratings yet
- Acute Renal FailureDocument10 pagesAcute Renal FailureSypheruNo ratings yet
- 2D2016 3.4-2 Azotemia and Urinary Abnormalities (Harrison's)Document7 pages2D2016 3.4-2 Azotemia and Urinary Abnormalities (Harrison's)elleinas100% (1)
- Acute Kidney Failure OverviewDocument5 pagesAcute Kidney Failure OverviewNiña CastroNo ratings yet
- Sistem UrinariaDocument42 pagesSistem UrinariaHanny da GamaNo ratings yet
- Renal SystemDocument20 pagesRenal SystemRahul DasNo ratings yet
- Renal FailureDocument41 pagesRenal Failure12046No ratings yet
- Acute Kidney InjuryDocument60 pagesAcute Kidney InjuryAbegail Fermanejo-GeneraoNo ratings yet
- AkiDocument38 pagesAkiPhillip MartinezNo ratings yet
- Acute Renal Failure DXDocument7 pagesAcute Renal Failure DXfarid akbarNo ratings yet
- Acute Kidney InjuryDocument3 pagesAcute Kidney InjuryBrigitta IsabellaNo ratings yet
- Renal Faliure 1Document50 pagesRenal Faliure 1180045No ratings yet
- Acute Renal Failure/ Gagal Ginjal Akut: Tunggul Adi P., M.SC., Apt. Lab Farmasi Klinik, Farmasi, FKIK, UNSOEDDocument27 pagesAcute Renal Failure/ Gagal Ginjal Akut: Tunggul Adi P., M.SC., Apt. Lab Farmasi Klinik, Farmasi, FKIK, UNSOEDPramita Purbandari100% (1)
- Renal Failur E: Mamta Kumari Asst - Prof. Igims-ConDocument51 pagesRenal Failur E: Mamta Kumari Asst - Prof. Igims-ConMamta KumariNo ratings yet
- Acute Kidney InjuryDocument17 pagesAcute Kidney InjuryIndah Hane50% (2)
- Lo Week 2-1Document8 pagesLo Week 2-1Martien Silviandy SetiawanNo ratings yet
- Acute Kidney Injury (AKI) : by Prof Grace Irimu Consultant Pediatrician and NephrologistDocument43 pagesAcute Kidney Injury (AKI) : by Prof Grace Irimu Consultant Pediatrician and Nephrologistokwadha simionNo ratings yet
- Acute and Chronic Renal FailureDocument21 pagesAcute and Chronic Renal FailureStephina ImmaculateNo ratings yet
- 7.acute Renal Failure (ARF)Document20 pages7.acute Renal Failure (ARF)Mahesh RathnayakeNo ratings yet
- Cute Enal Ailure: Dr. Shumaila Rafi Assistant Professor MedicineDocument27 pagesCute Enal Ailure: Dr. Shumaila Rafi Assistant Professor MedicineMuhammad MakkiNo ratings yet
- Acute Kidney InjuryDocument18 pagesAcute Kidney InjuryV RakeshreddyNo ratings yet
- Approach To Patient With Diseases of The Kidney and Urinary Tract FINALDocument9 pagesApproach To Patient With Diseases of The Kidney and Urinary Tract FINALgelskNo ratings yet
- Presentation by Joann Czech Rn/Cds St. Cloud HospitalDocument13 pagesPresentation by Joann Czech Rn/Cds St. Cloud HospitalTrajceNo ratings yet
- Acute Renal FailureDocument12 pagesAcute Renal FailureRifa Aprillia CahyaniNo ratings yet
- Acute Tubular NecrosisDocument15 pagesAcute Tubular NecrosisDeepak patelNo ratings yet
- Genitourinary DisordersDocument2 pagesGenitourinary DisordersGwenn SalazarNo ratings yet
- Approach To Acute Renal FailureDocument40 pagesApproach To Acute Renal FailureMochammad Fariz AmsalNo ratings yet
- Hepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Hepatic Encephalopathy: Causes, Tests, and Treatment OptionsFrom EverandHepatic Encephalopathy: Causes, Tests, and Treatment OptionsRating: 3.5 out of 5 stars3.5/5 (2)
- Adverse Blood Reaction and HDNDocument34 pagesAdverse Blood Reaction and HDNAdeniran CharlesNo ratings yet
- Complications & Diseases Associated With Blood TransfusionDocument15 pagesComplications & Diseases Associated With Blood TransfusionAdeniran CharlesNo ratings yet
- Anxiolytic and Hypnotic Drugs 2Document44 pagesAnxiolytic and Hypnotic Drugs 2Adeniran CharlesNo ratings yet
- Neuromuscular Pharmacology 305-1Document43 pagesNeuromuscular Pharmacology 305-1Adeniran CharlesNo ratings yet
- Protein Synthesis InhibitorDocument113 pagesProtein Synthesis InhibitorAdeniran CharlesNo ratings yet
- Cell Wall InhibitorDocument99 pagesCell Wall InhibitorAdeniran CharlesNo ratings yet
- The Drawing WebsiteDocument99 pagesThe Drawing WebsiteAdeniran CharlesNo ratings yet
- Haematologic Manifestations of Systemic DiseasesDocument38 pagesHaematologic Manifestations of Systemic DiseasesAdeniran CharlesNo ratings yet
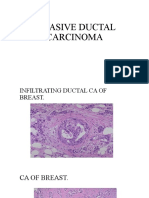
- Invasive Ductal CarcinomaDocument3 pagesInvasive Ductal CarcinomaAdeniran CharlesNo ratings yet
- Clinical Blood TransfusionDocument13 pagesClinical Blood TransfusionAdeniran CharlesNo ratings yet
- Pathophysiology of ShockDocument56 pagesPathophysiology of ShockDr. Haricharan ANo ratings yet
- Summative Test in MacromoleculesDocument3 pagesSummative Test in MacromoleculesCalebamaziah BonzonNo ratings yet
- Test Bank For Biology 12th by RavenDocument52 pagesTest Bank For Biology 12th by RavenAmberClineagwbd100% (43)
- Review Paper 1 + MSDocument9 pagesReview Paper 1 + MSYohanes Alvin GoenawanNo ratings yet
- Anaphy PPT - Nervous SystemDocument36 pagesAnaphy PPT - Nervous SystemJamaica TuellaNo ratings yet
- Worksheet 15-ENZYMESDocument4 pagesWorksheet 15-ENZYMESNaz BasaranNo ratings yet
- Exposing and Retracting InstrumentsDocument8 pagesExposing and Retracting Instrumentsyamie sulongNo ratings yet
- Biomechanics 1Document15 pagesBiomechanics 1Usama RafiqNo ratings yet
- Oxidative Stress and Sport PerformanceDocument6 pagesOxidative Stress and Sport PerformanceFatur Sang Ahli WarNo ratings yet
- Reproductive SystemDocument7 pagesReproductive SystemshaniaericaNo ratings yet
- Form 86 2022 Health Examination RecordDocument1 pageForm 86 2022 Health Examination RecordMA. GLIZA TANNo ratings yet
- Fundamentals of Anatomy and Physiology 12Th Global Edition Frederic Martini Full ChapterDocument67 pagesFundamentals of Anatomy and Physiology 12Th Global Edition Frederic Martini Full Chapternaomi.parker972100% (11)
- CHM4116 Nitrogen Metab ReviewerDocument22 pagesCHM4116 Nitrogen Metab ReviewerBEA FRANCINE DELOS SANTOSNo ratings yet
- COURSE WORK MOLECULAR BIOLOGY & GeneticsDocument3 pagesCOURSE WORK MOLECULAR BIOLOGY & Geneticsusaeed00000No ratings yet
- FINAL CVS Module Time TableDocument5 pagesFINAL CVS Module Time TableAimen KhanNo ratings yet
- Sympathetic OphthalmiaDocument13 pagesSympathetic Ophthalmiamohamed salamaNo ratings yet
- Kamota Mock Examinations 2023 s.6 BiologyDocument4 pagesKamota Mock Examinations 2023 s.6 Biologymungufeni amosNo ratings yet
- Microscopic Study of Epithelial Tissue and Connective TissueDocument16 pagesMicroscopic Study of Epithelial Tissue and Connective TissueSinger Rahul Sharma100% (1)
- Desmoid Tumor PathophysiologyDocument4 pagesDesmoid Tumor Pathophysiologyjo_annamae4413No ratings yet
- Pharmacology: Notes On Endocrine DrugsDocument2 pagesPharmacology: Notes On Endocrine DrugsByron ChuNo ratings yet
- Session #34 SAS - AnaPhy (Lab)Document7 pagesSession #34 SAS - AnaPhy (Lab)Cristina SottoNo ratings yet
- DGST - KP - CV - Template - For All Students and Postdocs 1Document4 pagesDGST - KP - CV - Template - For All Students and Postdocs 1Abid Ahmad100% (1)
- Characteristics of Leaf MorphologyDocument11 pagesCharacteristics of Leaf MorphologyJuwita PardedeNo ratings yet
- Virtual Lab Plant and AnimalDocument3 pagesVirtual Lab Plant and AnimalJose Mendieta0% (1)
- Hemodynamics (Copy)Document41 pagesHemodynamics (Copy)BerihunNo ratings yet
- Cell Biology Mixed Question QuizDocument17 pagesCell Biology Mixed Question QuizMariamNo ratings yet
- Neuroanatomy - Neurophysiology 2Document45 pagesNeuroanatomy - Neurophysiology 2Saja AbuasbehNo ratings yet
- Human Anatomy Synopsis Spine PDFDocument109 pagesHuman Anatomy Synopsis Spine PDFInês Fernandes100% (1)
- May 2021 Mark Scheme 2BDocument17 pagesMay 2021 Mark Scheme 2BMeenakshie ChaudrieNo ratings yet