Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
25 viewsAdverse Blood Reaction and HDN
Adverse Blood Reaction and HDN
Uploaded by
Adeniran CharlesThis document discusses complications associated with blood transfusion, including both immediate and delayed complications. Immediate complications include febrile non-hemolytic transfusion reactions, hemolytic transfusion reactions, allergic reactions, anaphylaxis, and transfusion-associated lung injury. Delayed complications include hemolytic transfusion reactions, post-transfusion purpura, graft-versus-host disease, and infections transmitted through blood transfusions. The document also discusses hemolytic disease of the newborn, which occurs when a pregnant woman has antibodies against her fetus's red blood cells due to blood group incompatibility.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You might also like
- WBI11 01 Rms October 2021Document25 pagesWBI11 01 Rms October 2021Mariam Ali75% (4)
- Hema Transes 1Document13 pagesHema Transes 1Nico LokoNo ratings yet
- Complications of Blood TransfusionDocument18 pagesComplications of Blood TransfusionIqra ghafoorNo ratings yet
- Adverse Blood Reaction and HDNDocument34 pagesAdverse Blood Reaction and HDNAdeniran CharlesNo ratings yet
- Transfusion Reaction - DRGSPDocument42 pagesTransfusion Reaction - DRGSPGaurav PawarNo ratings yet
- HPB Adverse Transfusion ReactionDocument26 pagesHPB Adverse Transfusion ReactionFransiscus RivaldyNo ratings yet
- Adverse Reactions To Blood Transfusion1Document38 pagesAdverse Reactions To Blood Transfusion1Abby Liew100% (1)
- Transfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1Document33 pagesTransfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1UmikaguptaNo ratings yet
- BLOOD Transfusion ReactionDocument24 pagesBLOOD Transfusion Reactionanjali.shalin00No ratings yet
- Blood Transfusion and Its ComplicationsDocument31 pagesBlood Transfusion and Its ComplicationsSaima Hasnain MinhasNo ratings yet
- 5 Transfusion ReactionsDocument20 pages5 Transfusion ReactionsDeladem EmmanuelNo ratings yet
- Approach and Management of Bleeding NeonateDocument49 pagesApproach and Management of Bleeding NeonateG VenkateshNo ratings yet
- Blood ProductsDocument70 pagesBlood Productsjadhamade339No ratings yet
- A-Gvhd M.saeedDocument20 pagesA-Gvhd M.saeedaymenNo ratings yet
- Blood Transfusion ReactionsDocument8 pagesBlood Transfusion ReactionsStephanie AngelaNo ratings yet
- Transfusion Medicine by Dr. Sharad JohriDocument54 pagesTransfusion Medicine by Dr. Sharad JohriShashwat JohriNo ratings yet
- Lecture On Blood Groups, Transfusion, RH Incompatibility by Dr. RoomiDocument41 pagesLecture On Blood Groups, Transfusion, RH Incompatibility by Dr. RoomiMudassar Roomi100% (1)
- Blood Transfusion Reaction 3032018Document33 pagesBlood Transfusion Reaction 3032018Kelly YeowNo ratings yet
- Division of Blood Transfusion Services: Ministry of Health and Family WelfareDocument46 pagesDivision of Blood Transfusion Services: Ministry of Health and Family WelfareKirandragonNo ratings yet
- Hematology Transfusion ReactionDocument69 pagesHematology Transfusion ReactionSharmin Nahar NabilaNo ratings yet
- Blood and Its ComponentsDocument30 pagesBlood and Its ComponentskushalNo ratings yet
- Serious Hazards of Transfusion: DR Kenneth S Charles MB - Bs (Uwi), FRCP (Uk), Frcpath (Uk) Senior Lecturer in HaematologyDocument65 pagesSerious Hazards of Transfusion: DR Kenneth S Charles MB - Bs (Uwi), FRCP (Uk), Frcpath (Uk) Senior Lecturer in HaematologySuneil R AlsNo ratings yet
- 5 Transfusion ReactionsDocument34 pages5 Transfusion ReactionsFuentes, Jade Andrey R. BSMT 2-ANo ratings yet
- Unit - 5 Blood Banking HaematologyDocument82 pagesUnit - 5 Blood Banking HaematologySumit PandyaNo ratings yet
- Session 8Document6 pagesSession 8madcalNo ratings yet
- ICU Blood Transfusion & Electrolytes DisturbanceDocument26 pagesICU Blood Transfusion & Electrolytes Disturbancef6080683No ratings yet
- Adverse Effects: Blood TransfusionDocument43 pagesAdverse Effects: Blood TransfusionDumindu PereraNo ratings yet
- 7 Adverse Reactions ToDocument11 pages7 Adverse Reactions TodrkamalakarNo ratings yet
- Blood Transfusion Basic Concepts Blood Transfusion inDocument103 pagesBlood Transfusion Basic Concepts Blood Transfusion iniahmad9No ratings yet
- Blood Transfusion Notes..Document9 pagesBlood Transfusion Notes..queenethNo ratings yet
- Adverse Effects of TransfusionDocument5 pagesAdverse Effects of Transfusionlubna aloshibiNo ratings yet
- Adverse Effects of TransfusionDocument5 pagesAdverse Effects of Transfusionlubna aloshibiNo ratings yet
- Adverse Effects of Plasma TherapyDocument80 pagesAdverse Effects of Plasma TherapyShaiji ShahidNo ratings yet
- Transfusion Medicine: DR Abdullah AnsariDocument53 pagesTransfusion Medicine: DR Abdullah AnsariFabsNo ratings yet
- ITP LectureDocument20 pagesITP LectureReza MajidiNo ratings yet
- Blood Transfusion Reactions: Dr. Madhuvan GuptaDocument42 pagesBlood Transfusion Reactions: Dr. Madhuvan GuptaDr. Madhuvan GuptaNo ratings yet
- Blood Transfusion 2Document12 pagesBlood Transfusion 2Helene AlawamiNo ratings yet
- Hemolytic Disease of The Fetus /newbornDocument46 pagesHemolytic Disease of The Fetus /newbornK.M.S. ChathunikaNo ratings yet
- Give The Purpose of Incubation in The Saline Tube MethodDocument3 pagesGive The Purpose of Incubation in The Saline Tube MethodBrielleNo ratings yet
- Blood Transfusion AlexDocument33 pagesBlood Transfusion AlexaymenNo ratings yet
- Adverse Effects of Blood TransfusionsDocument3 pagesAdverse Effects of Blood Transfusionsay254No ratings yet
- Blood Transfusion Blood Grouping and Cross MatchingDocument46 pagesBlood Transfusion Blood Grouping and Cross MatchingHa LeemNo ratings yet
- TransfusionDocument48 pagesTransfusionSandy LavedaNo ratings yet
- Transfusion Medicine: Dr. C.C. Okany Consultant Physician/Haematologist LuthDocument27 pagesTransfusion Medicine: Dr. C.C. Okany Consultant Physician/Haematologist LuthisuhuNo ratings yet
- Probleme La TransfuziiDocument6 pagesProbleme La TransfuziiAdina TîrnoveanuNo ratings yet
- AABB Pediatric Transfusion - Risks and GuidelinesDocument57 pagesAABB Pediatric Transfusion - Risks and GuidelinesDR.RAJESWARI SUBRAMANIYANNo ratings yet
- Red Cell AlloimmunizationDocument30 pagesRed Cell AlloimmunizationjarssooNo ratings yet
- AIHADocument48 pagesAIHAsaudlinks2No ratings yet
- Transfusion of Blood and Red CellsDocument34 pagesTransfusion of Blood and Red CellsAdams Westlifer SophianoNo ratings yet
- Blood Transfusion ProblemsDocument52 pagesBlood Transfusion ProblemsAulia RahmanNo ratings yet
- 11a. Blood TransfusionDocument28 pages11a. Blood TransfusionMuwanga faizoNo ratings yet
- Blood Transfusion and Transfusion Reactions: Life Threatening ProcessDocument52 pagesBlood Transfusion and Transfusion Reactions: Life Threatening Processanam farzand100% (2)
- Abo Typing Discrepancies: Rene Jesus Alfredo R. Dinglasan, RMTDocument14 pagesAbo Typing Discrepancies: Rene Jesus Alfredo R. Dinglasan, RMTdirenjan100% (1)
- Surgery Slide 6 - Blood TransfusionsDocument54 pagesSurgery Slide 6 - Blood TransfusionsEman NazzalNo ratings yet
- Local Media4202655613631600684Document6 pagesLocal Media4202655613631600684Haniya KhanNo ratings yet
- Ascorbic Acid NCPDocument8 pagesAscorbic Acid NCPJohann OrtizNo ratings yet
- Blood TransfusionDocument55 pagesBlood Transfusionanand7504100% (2)
- Complications of Blood TransfusionsDocument4 pagesComplications of Blood TransfusionsZain Hadi100% (1)
- RJDocument2 pagesRJRj King AstreroNo ratings yet
- Alert Medical Series: USMLE Alert I, II, IIIFrom EverandAlert Medical Series: USMLE Alert I, II, IIIRating: 2 out of 5 stars2/5 (1)
- Mollison's Blood Transfusion in Clinical MedicineFrom EverandMollison's Blood Transfusion in Clinical MedicineRating: 4.5 out of 5 stars4.5/5 (1)
- Complications & Diseases Associated With Blood TransfusionDocument15 pagesComplications & Diseases Associated With Blood TransfusionAdeniran CharlesNo ratings yet
- Anxiolytic and Hypnotic Drugs 2Document44 pagesAnxiolytic and Hypnotic Drugs 2Adeniran CharlesNo ratings yet
- Cell Wall InhibitorDocument99 pagesCell Wall InhibitorAdeniran CharlesNo ratings yet
- Acute Renal Failure: Dr. Sami Abdo RadmanDocument23 pagesAcute Renal Failure: Dr. Sami Abdo RadmanAdeniran CharlesNo ratings yet
- Protein Synthesis InhibitorDocument113 pagesProtein Synthesis InhibitorAdeniran CharlesNo ratings yet
- The Drawing WebsiteDocument99 pagesThe Drawing WebsiteAdeniran CharlesNo ratings yet
- Haematologic Manifestations of Systemic DiseasesDocument38 pagesHaematologic Manifestations of Systemic DiseasesAdeniran CharlesNo ratings yet
- Clinical Blood TransfusionDocument13 pagesClinical Blood TransfusionAdeniran CharlesNo ratings yet
- Neuromuscular Pharmacology 305-1Document43 pagesNeuromuscular Pharmacology 305-1Adeniran CharlesNo ratings yet
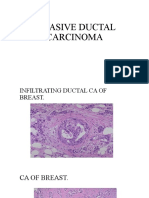
- Invasive Ductal CarcinomaDocument3 pagesInvasive Ductal CarcinomaAdeniran CharlesNo ratings yet
- CM2-CU10-Modification of Mendelian RatiosDocument17 pagesCM2-CU10-Modification of Mendelian RatiosClaire GonoNo ratings yet
- GOBIOM BrochureDocument4 pagesGOBIOM BrochureGVK Bio Sciences Private LimitedNo ratings yet
- Circulatory System VCE BiologyDocument6 pagesCirculatory System VCE BiologyCallum KennyNo ratings yet
- Neonatal Resuscitation PDFDocument1 pageNeonatal Resuscitation PDFOdessa EnriquezNo ratings yet
- Paper 2 Biology 1996 Paper 2+ansDocument19 pagesPaper 2 Biology 1996 Paper 2+ansapi-3812894100% (1)
- NCC-61 With RET ENG - User Manual V2020 - 01 - 21 - 011900 (046-090)Document45 pagesNCC-61 With RET ENG - User Manual V2020 - 01 - 21 - 011900 (046-090)Zoulikifil Abdou KarimNo ratings yet
- The Circulatory System (Heart)Document3 pagesThe Circulatory System (Heart)NinaNo ratings yet
- Chapter 1: An Overview of Clinical LaboratoryDocument13 pagesChapter 1: An Overview of Clinical LaboratoryAshley Tañamor100% (2)
- Neonatal Jaundice DR - MaslianiDocument58 pagesNeonatal Jaundice DR - MaslianiHengky HanggaraNo ratings yet
- - ملحق كونكت بلس excellenceDocument17 pages- ملحق كونكت بلس excellenceDinaNo ratings yet
- Tourniquet Test (Capillary Fragility) : Normal Findings Indications Test ExplanationDocument2 pagesTourniquet Test (Capillary Fragility) : Normal Findings Indications Test ExplanationAaron James RuedasNo ratings yet
- Smart Breath 2014-05-26 Book ENGDocument34 pagesSmart Breath 2014-05-26 Book ENGAndrej MilutinovicNo ratings yet
- NCLEX Study GuideDocument7 pagesNCLEX Study Guidemmgoodall22100% (3)
- Tensiometro Shock ProofDocument2 pagesTensiometro Shock ProofjessikaNo ratings yet
- Du TestDocument14 pagesDu TestlalhaiagustinNo ratings yet
- Thrombocytopenia Pocket GuideDocument8 pagesThrombocytopenia Pocket GuideAnnisaValentKhanNo ratings yet
- Ijett V67i3p218Document4 pagesIjett V67i3p218nhel anonymousNo ratings yet
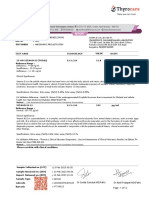
- Patient Name Age / Gender Uhid/Mr No. OP Visit No Sample Collected On: 03-07-2018 18:33 Reported On LRN# Specimen Ref DoctorDocument2 pagesPatient Name Age / Gender Uhid/Mr No. OP Visit No Sample Collected On: 03-07-2018 18:33 Reported On LRN# Specimen Ref DoctormukhleshNo ratings yet
- Transport in Humans - MCQDocument4 pagesTransport in Humans - MCQAhmed Kaleem Khan Niazi100% (1)
- Eurton Electric Co., Inc.: AbbottDocument16 pagesEurton Electric Co., Inc.: Abbottjose navaNo ratings yet
- Blood Bank Quality Manage 2797670Document21 pagesBlood Bank Quality Manage 2797670Rahul Behl0% (1)
- Understanding CBC Histogram PDFDocument17 pagesUnderstanding CBC Histogram PDFSuresh ShresthaNo ratings yet
- Foreign MagicksDocument63 pagesForeign MagicksMiguel Pérez García-PliegoNo ratings yet
- Camille Suzaine Pradas - Labs and DrugsDocument7 pagesCamille Suzaine Pradas - Labs and DrugsCamille Suzaine PradasNo ratings yet
- Concise Atlas of Basic HemopoiesisDocument14 pagesConcise Atlas of Basic HemopoiesisdynndgrNo ratings yet
- The Respiratory System 2019 dk-20191118110326Document26 pagesThe Respiratory System 2019 dk-20191118110326Jackson JastariNo ratings yet
- Report 10 46Document11 pagesReport 10 46Subham MukherjeeNo ratings yet
- Practical PathologyDocument94 pagesPractical Pathologyadi raghavNo ratings yet
Adverse Blood Reaction and HDN
Adverse Blood Reaction and HDN
Uploaded by
Adeniran Charles0 ratings0% found this document useful (0 votes)
25 views34 pagesThis document discusses complications associated with blood transfusion, including both immediate and delayed complications. Immediate complications include febrile non-hemolytic transfusion reactions, hemolytic transfusion reactions, allergic reactions, anaphylaxis, and transfusion-associated lung injury. Delayed complications include hemolytic transfusion reactions, post-transfusion purpura, graft-versus-host disease, and infections transmitted through blood transfusions. The document also discusses hemolytic disease of the newborn, which occurs when a pregnant woman has antibodies against her fetus's red blood cells due to blood group incompatibility.
Original Description:
Original Title
Adverse Blood reaction and HDN
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses complications associated with blood transfusion, including both immediate and delayed complications. Immediate complications include febrile non-hemolytic transfusion reactions, hemolytic transfusion reactions, allergic reactions, anaphylaxis, and transfusion-associated lung injury. Delayed complications include hemolytic transfusion reactions, post-transfusion purpura, graft-versus-host disease, and infections transmitted through blood transfusions. The document also discusses hemolytic disease of the newborn, which occurs when a pregnant woman has antibodies against her fetus's red blood cells due to blood group incompatibility.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
25 views34 pagesAdverse Blood Reaction and HDN
Adverse Blood Reaction and HDN
Uploaded by
Adeniran CharlesThis document discusses complications associated with blood transfusion, including both immediate and delayed complications. Immediate complications include febrile non-hemolytic transfusion reactions, hemolytic transfusion reactions, allergic reactions, anaphylaxis, and transfusion-associated lung injury. Delayed complications include hemolytic transfusion reactions, post-transfusion purpura, graft-versus-host disease, and infections transmitted through blood transfusions. The document also discusses hemolytic disease of the newborn, which occurs when a pregnant woman has antibodies against her fetus's red blood cells due to blood group incompatibility.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 34
COMPLICATIONS AND DISEASES
ASSOCIATED WITH BLOOD
TRANSFUSION
Dr OT Ojo
Introduction
• Blood transfusion is a life saving procedure but
potentially hazardous.
• In spite of measures designed to remove adverse
effects of blood transfusion, complications remain a
source of concern.
• The type and frequency of complication however
depend on the amount of care exercised in the
preparation for, and the supervision of the
transfusion procedure.
• Blood transfusion should be considered only when
there is no alternative means of treatment.
Complications of transfusion
Immediate Delayed
• Immunological • Immunological
Febrile non haemolytic transfusion
reactions Haemolytic transfusion
Haemolytic transfusion reaction reaction
Allergic reaction Post transfusion purpura
Anaphylaxis
Transfusion-associated lung injury
GVHD
• Non immunological • Non immunological
Circulatory overload Transfusion of infectious
Bacterial contamination of donor
blood unit
agents
Air embolism Iron overload
FNHTR
• Due to reaction of alloantibodies in the recipient against
transfused leucocyte antigen.
• Also due to release of cytokines from leucocytes in the
stored blood.
• Common in previously sensitized individual- previous
transfusion or pregnancy.
• Present with fever, occasional chills, rigors, headache.
• Occur within 30-60mins of transfusion.
• R/O HTR and bacterial contamination of donor unit.
• Management- Stop transfusion, give antipyretics/
antihistamine, slow speed of transfusion.
• Prevention- Leucocyte-depleted packed cells.
HTR
• Haemolytic complication results from premature
destruction of donor cells as a result of immune
antibodies in the recipient.
• Classification- immediate (acute) haemolytic and
delayed haemolytic.
• Immediate: Often result from ABO
incompatibility mediated by by IgM or
sometimes IgG Anti-A or Anti-B.
Usually due to Clerical error- incorrect
identification of recipient and incorrect labelling
of sample bottle or filling of request form
HTR…
• Pathogenesis:
Antibodies in patient plasma bind to donor
red cells→ full complement activation (C5-
C9)→ Acute intravascular haemolysis.
C3a & C5a cause vasodilation →hypotension,
ARF.
Release of procoagulant from destroyed RBC
→activation of coagulation →DIC
HTR…
• Clinical features:
Occurs within mins of starting transfusion
Heat or pain at the infusion site, loin or low back
pain, chest tightness, breathlessness, throbbing
headache, nausea/ vomiting, Pyrexia, rigor,
Hypotension and vascular collapse.
Others include Haemoglobinuria, DIC, Acute renal
failure with Oliguria, and death.
Anaesthetized patient- hypotension, DIC
Management
• Stop blood transfusion
• restore blood volume and blood pressure.
• Investigate
Investigations
• Confirm that recipient identity is the same as that on compatibility
label and donor unit
• Repeat grouping on pre-and post-transfusion sample of recipient ,
as well as donor sample.
• Repeat the crossmatch on donor cell against recipient pre and
post-transfusion sample.
• DAT on post-transfusion sample
• Check plasma for haemoglobinaemia (pink colouration)
• urine for Haemogloninuria
• LFT - ↑ unconjugated bilirubin
• Test for DIC- PLT, PT/APTT, FDPs
• E/u/Cr
• Bacteria contamination-
black/ purple discolouration of RC with evidence of haemolysis
Blood culture
Delayed HTR
• Due to secondary response in a patient
already previously sensitized to antigens
present on recently transfused red cells.
• It occurs within 5 to 10 days.
• Cf- Anaemia and jaundice
• Usually caused by Rh (anti-c) and Kidd (anti-
JK).
• DAT is +ve
Post-transfusion purpura
• This is characterised by a sudden onset of severe
thrombocytopaenia 7 -10 days post-transfusion.
• It follows a history of previous transfusion or
pregnancy and is far commoner in women.
• It is due to Anti-HPA -1a, both transfused and
recipient PLT are destroyed.
• Usu. self-limiting.
• Otherwise, Immunoglobulin or plasma exchange
may be needed.
Anaphylactic reaction
• It is caused by Anti-IgA in an IgA deficient person.
• Prior sensitization or without stimulation
• Anti-IgA-IgA complex activate complement → C3a &C5a
generation.
• Features :
Nausea, abdominal cramps, vomitting, diarrhoea,
hypotension, breathlessness, facial edema
Shock may occur rarely and can be potentially fatal.
• Stop transfusion immediately.
• Treat with antihistamine, hydrocortisone, adrenaline.
Allergic Reactions
• Due to reaction between plasma proteins and
IgE antibodies in recipient’s plasma→release
of histamine.
• Cf- Urticaria, rash and pruritus.
• Treatment-antihistamine & hydrocortisone
Transfusion-related acute lung Injury
(TRALI)
• Leucoagglutinins from donor+ leucocytes in
recipient= leucocyte aggregate, lodgement in
pulmonary microcirculation causes increase in
vascular permeability.
• Cf- fever, chills, respiratory distress, dry cough
• CXR- Diffuse pulmonary infiltrate
• Donors usu. Multiparous women.
• Treatment-supportive
Graft-versus-host disease(GvHD)
• occurs when live lymphocyte are transfused to
an immunocompromised patient.
• Cf-fever, skin rash, vomiting, diarrhoea,
hepatitis, pancytopaenia.
• Prevention- Irradiation of blood.
• NON-IMMUNOLOGICAL
COMPLICATIONS
Transfusion of infectious agents
• These include Hepatitis B virus (HBV), Hepatitis C
virus (HCV), Human Immunodeficiency virus
(HIV), Cytomegalovirus (CMV), Filaria, Syphilis,
toxoplasma and Malaria.
• Reaction to bacteria and or its pyrogen:
This is rare because of sterilization of fluid and
disposable equipment.
Can present with circulatory collapse.
Prevention is by the use of aseptic techniques in
blood donation, and the storage of blood at a
temperature of 2-80C.
Circulation Overload
• Due to rapid transfusion of large volumes of
blood without equivalent blood loss.
• Can also occur after transfusion of small amt
of blood to a patient with abnormal cardiac or
renal function.
• Treatment: Prop up in bed,O2, diuretic
• Prevention: give packed cells
use diuretics.
• Thrombophlebitis: This is due to indwelling
venous canula.
• Air embolism: This has been eliminated by the
use of plastic bags and a closed system.
• Post-transfusion iron overload occurs in
multiply transfused individuals.
Complication of massive blood
transfusion
• Replacement of a patient’s total blood volume
with stored blood within 24hrs.
Dilution of Platelets, Reduction of coagulation
factors, especially factors Va and VIIIa
Hypocalcaemia and Hyperkaleamia –
Acidosis
Hypothermia causing cardiac irregularities
•HAEMOLYTIC
DISEASE OF THE
NEWBORN (HDN)
Introduction
• It is a disease in which there is destruction of
RBCs of the fetus or newborn by maternal
alloantibodies against paternal antigens on the
child’s RBCs.
• Maternal antibodies is stimulated due to blood
group incompatibility between mother and fetus.
• Causal Red cell antigens-Rh-D, Rh-c, kell, A and B.
• Rh-D, Rh-c, kell- can cause severe HDN while ABO
incompatibility cause mild disease.
• Others- Duffy, Kidd
•Rh HDN
Introduction
• RhD negative mother pregnant with RhD +ve
baby.
• RhD +ve fetal RBC cross into maternal
circulation at parturition/ 3rd trimester and
sensitize the mother to produce anti-D.
• Sensitization could also be due to
Amniocentesis, External cephalic version,
threatened abortion, and chorion villus
sampling or trauma to placenta.
Pathogenesis
• Fetomaternal haemorrhage→10 Immune response
with production of IgM abs in the 1st pregnancy, baby
is not affected
• FMH in 2nd pregnancy→ 20 Immune response with
production of IgG abs which cross placenta to coat
fetal RhD +ve RBC.
• IgG coated fetal RBCs are destroyed in the spleen→
anaemia →erythroid hyperplasia in the BM
→extramedulary erythropoesis in the spleen and
liver.
• uncojugated bilirubin in fetus cross into maternal
circulation and metabolised
• ↑uncojugated bilirubin in neonate due to
immaturity of glucoronyl transferase, this may cross
the BBB and damage basal ganglia → kernicterus.
Clinical features
• Variable
• Mild anaemia & jaundice
• Kernicterus-neurological deficit resulting in
deafness, mental retardation, spasticity, and
epilepsy
• Still birth (Hydop fetalis)-severe anaemia,
hepatosplenomegaly, ascitis and anarsarca
Laboratory investigations
ANC:
• mother
History of sensitization
Blood group-ABO and Rh
Antibody screening, identification, titer
• Blood group of the father
• Fetal
Amniocentesis- assess conc. of bilirubin done between
28-32wks GA, but if bad obstetric Hx done 10wks prior
to the date of previous fetal or neonatal death.
Laboratory investigations…
Indicated when maternal anti-D titer is 1:32, rising anti-D
titer on ff up visit, bad obstetric hx (previously severely
affected offspring).
Liley’s chart- Zone 1 (low), II (middle), III (high)
Zone III indicate severely affected fetus with imminent
death: GA<34wks- intrauterine transfusion, GA >34wks-
delivery
Zone II- repeat and do as in I
Zone I-proceed to term
• Cordocentesis- estimate Hb and bilirubin, blood group,
DAT
• Velocimetry of fetal middle cerebral artery by doppler
USS- ↑vel correlate with fetal anaemia (IUFT)
Laboratory investigations…
• Newborn
Blood group
PBF- numerous NRBCs (erythroblastosis),
polychromasia
DAT-+ve
Hb and bilirubin conc.-do urgent EBT if Hb<
12g/dL or unconjugated bilirubin> 5mg/dL
• Maternal post delivery-Betke-Kleihauer test/ flow
cytometry for FMH vol. estimation
Rh HDN
Blood film from a baby with Rh HDN due to anti-D showing
polychromasia and large numbers of NRCs, but relatively few
spherocytes.
Treatment
• Fetus- IUFT or delivery depending on fetal
lung maturity
• Neonate-
EBT if bilirubin is rising rapidly
Phototherapy
Albumin infusion
Prevention of Rh isoimmunisation
• During antenatal- anti-D IgG given to RhD-ve mother
with potentially sensitizing episode, 250iu given
before 20wks GA and 500iu thereafter.
• Post delivery-
administer anti-D IgG to RhD –ve mother within 72hrs
of delivery of Rh D +ve neonate.
Dose-500iu of anti-D IgG to neutralize 4mls of fetal
red cell.
Increase anti-D dose if there is FMH> 4mls, at 125iu/
mL of FMH > 4mL
ABO HDN
• Commoner than Rh HDN.
• Usually mild
• Usually cause by immune IgG abs in group O
mothers carry group A or B fetus.
• Ist pregnancy may be affected.
• DAT may be –ve or weakly +ve.
• PBF- spherocytosis, polychromasia
• Treatment-phototherapy, EBT in severe
hyperbilirubinaemia.
ABO HDN
Blood film from a neonate with ABO HDN due to anti-A,
showing very large numbers of spherocytes,
polychromasia and no nucleated red cells.
You might also like
- WBI11 01 Rms October 2021Document25 pagesWBI11 01 Rms October 2021Mariam Ali75% (4)
- Hema Transes 1Document13 pagesHema Transes 1Nico LokoNo ratings yet
- Complications of Blood TransfusionDocument18 pagesComplications of Blood TransfusionIqra ghafoorNo ratings yet
- Adverse Blood Reaction and HDNDocument34 pagesAdverse Blood Reaction and HDNAdeniran CharlesNo ratings yet
- Transfusion Reaction - DRGSPDocument42 pagesTransfusion Reaction - DRGSPGaurav PawarNo ratings yet
- HPB Adverse Transfusion ReactionDocument26 pagesHPB Adverse Transfusion ReactionFransiscus RivaldyNo ratings yet
- Adverse Reactions To Blood Transfusion1Document38 pagesAdverse Reactions To Blood Transfusion1Abby Liew100% (1)
- Transfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1Document33 pagesTransfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1UmikaguptaNo ratings yet
- BLOOD Transfusion ReactionDocument24 pagesBLOOD Transfusion Reactionanjali.shalin00No ratings yet
- Blood Transfusion and Its ComplicationsDocument31 pagesBlood Transfusion and Its ComplicationsSaima Hasnain MinhasNo ratings yet
- 5 Transfusion ReactionsDocument20 pages5 Transfusion ReactionsDeladem EmmanuelNo ratings yet
- Approach and Management of Bleeding NeonateDocument49 pagesApproach and Management of Bleeding NeonateG VenkateshNo ratings yet
- Blood ProductsDocument70 pagesBlood Productsjadhamade339No ratings yet
- A-Gvhd M.saeedDocument20 pagesA-Gvhd M.saeedaymenNo ratings yet
- Blood Transfusion ReactionsDocument8 pagesBlood Transfusion ReactionsStephanie AngelaNo ratings yet
- Transfusion Medicine by Dr. Sharad JohriDocument54 pagesTransfusion Medicine by Dr. Sharad JohriShashwat JohriNo ratings yet
- Lecture On Blood Groups, Transfusion, RH Incompatibility by Dr. RoomiDocument41 pagesLecture On Blood Groups, Transfusion, RH Incompatibility by Dr. RoomiMudassar Roomi100% (1)
- Blood Transfusion Reaction 3032018Document33 pagesBlood Transfusion Reaction 3032018Kelly YeowNo ratings yet
- Division of Blood Transfusion Services: Ministry of Health and Family WelfareDocument46 pagesDivision of Blood Transfusion Services: Ministry of Health and Family WelfareKirandragonNo ratings yet
- Hematology Transfusion ReactionDocument69 pagesHematology Transfusion ReactionSharmin Nahar NabilaNo ratings yet
- Blood and Its ComponentsDocument30 pagesBlood and Its ComponentskushalNo ratings yet
- Serious Hazards of Transfusion: DR Kenneth S Charles MB - Bs (Uwi), FRCP (Uk), Frcpath (Uk) Senior Lecturer in HaematologyDocument65 pagesSerious Hazards of Transfusion: DR Kenneth S Charles MB - Bs (Uwi), FRCP (Uk), Frcpath (Uk) Senior Lecturer in HaematologySuneil R AlsNo ratings yet
- 5 Transfusion ReactionsDocument34 pages5 Transfusion ReactionsFuentes, Jade Andrey R. BSMT 2-ANo ratings yet
- Unit - 5 Blood Banking HaematologyDocument82 pagesUnit - 5 Blood Banking HaematologySumit PandyaNo ratings yet
- Session 8Document6 pagesSession 8madcalNo ratings yet
- ICU Blood Transfusion & Electrolytes DisturbanceDocument26 pagesICU Blood Transfusion & Electrolytes Disturbancef6080683No ratings yet
- Adverse Effects: Blood TransfusionDocument43 pagesAdverse Effects: Blood TransfusionDumindu PereraNo ratings yet
- 7 Adverse Reactions ToDocument11 pages7 Adverse Reactions TodrkamalakarNo ratings yet
- Blood Transfusion Basic Concepts Blood Transfusion inDocument103 pagesBlood Transfusion Basic Concepts Blood Transfusion iniahmad9No ratings yet
- Blood Transfusion Notes..Document9 pagesBlood Transfusion Notes..queenethNo ratings yet
- Adverse Effects of TransfusionDocument5 pagesAdverse Effects of Transfusionlubna aloshibiNo ratings yet
- Adverse Effects of TransfusionDocument5 pagesAdverse Effects of Transfusionlubna aloshibiNo ratings yet
- Adverse Effects of Plasma TherapyDocument80 pagesAdverse Effects of Plasma TherapyShaiji ShahidNo ratings yet
- Transfusion Medicine: DR Abdullah AnsariDocument53 pagesTransfusion Medicine: DR Abdullah AnsariFabsNo ratings yet
- ITP LectureDocument20 pagesITP LectureReza MajidiNo ratings yet
- Blood Transfusion Reactions: Dr. Madhuvan GuptaDocument42 pagesBlood Transfusion Reactions: Dr. Madhuvan GuptaDr. Madhuvan GuptaNo ratings yet
- Blood Transfusion 2Document12 pagesBlood Transfusion 2Helene AlawamiNo ratings yet
- Hemolytic Disease of The Fetus /newbornDocument46 pagesHemolytic Disease of The Fetus /newbornK.M.S. ChathunikaNo ratings yet
- Give The Purpose of Incubation in The Saline Tube MethodDocument3 pagesGive The Purpose of Incubation in The Saline Tube MethodBrielleNo ratings yet
- Blood Transfusion AlexDocument33 pagesBlood Transfusion AlexaymenNo ratings yet
- Adverse Effects of Blood TransfusionsDocument3 pagesAdverse Effects of Blood Transfusionsay254No ratings yet
- Blood Transfusion Blood Grouping and Cross MatchingDocument46 pagesBlood Transfusion Blood Grouping and Cross MatchingHa LeemNo ratings yet
- TransfusionDocument48 pagesTransfusionSandy LavedaNo ratings yet
- Transfusion Medicine: Dr. C.C. Okany Consultant Physician/Haematologist LuthDocument27 pagesTransfusion Medicine: Dr. C.C. Okany Consultant Physician/Haematologist LuthisuhuNo ratings yet
- Probleme La TransfuziiDocument6 pagesProbleme La TransfuziiAdina TîrnoveanuNo ratings yet
- AABB Pediatric Transfusion - Risks and GuidelinesDocument57 pagesAABB Pediatric Transfusion - Risks and GuidelinesDR.RAJESWARI SUBRAMANIYANNo ratings yet
- Red Cell AlloimmunizationDocument30 pagesRed Cell AlloimmunizationjarssooNo ratings yet
- AIHADocument48 pagesAIHAsaudlinks2No ratings yet
- Transfusion of Blood and Red CellsDocument34 pagesTransfusion of Blood and Red CellsAdams Westlifer SophianoNo ratings yet
- Blood Transfusion ProblemsDocument52 pagesBlood Transfusion ProblemsAulia RahmanNo ratings yet
- 11a. Blood TransfusionDocument28 pages11a. Blood TransfusionMuwanga faizoNo ratings yet
- Blood Transfusion and Transfusion Reactions: Life Threatening ProcessDocument52 pagesBlood Transfusion and Transfusion Reactions: Life Threatening Processanam farzand100% (2)
- Abo Typing Discrepancies: Rene Jesus Alfredo R. Dinglasan, RMTDocument14 pagesAbo Typing Discrepancies: Rene Jesus Alfredo R. Dinglasan, RMTdirenjan100% (1)
- Surgery Slide 6 - Blood TransfusionsDocument54 pagesSurgery Slide 6 - Blood TransfusionsEman NazzalNo ratings yet
- Local Media4202655613631600684Document6 pagesLocal Media4202655613631600684Haniya KhanNo ratings yet
- Ascorbic Acid NCPDocument8 pagesAscorbic Acid NCPJohann OrtizNo ratings yet
- Blood TransfusionDocument55 pagesBlood Transfusionanand7504100% (2)
- Complications of Blood TransfusionsDocument4 pagesComplications of Blood TransfusionsZain Hadi100% (1)
- RJDocument2 pagesRJRj King AstreroNo ratings yet
- Alert Medical Series: USMLE Alert I, II, IIIFrom EverandAlert Medical Series: USMLE Alert I, II, IIIRating: 2 out of 5 stars2/5 (1)
- Mollison's Blood Transfusion in Clinical MedicineFrom EverandMollison's Blood Transfusion in Clinical MedicineRating: 4.5 out of 5 stars4.5/5 (1)
- Complications & Diseases Associated With Blood TransfusionDocument15 pagesComplications & Diseases Associated With Blood TransfusionAdeniran CharlesNo ratings yet
- Anxiolytic and Hypnotic Drugs 2Document44 pagesAnxiolytic and Hypnotic Drugs 2Adeniran CharlesNo ratings yet
- Cell Wall InhibitorDocument99 pagesCell Wall InhibitorAdeniran CharlesNo ratings yet
- Acute Renal Failure: Dr. Sami Abdo RadmanDocument23 pagesAcute Renal Failure: Dr. Sami Abdo RadmanAdeniran CharlesNo ratings yet
- Protein Synthesis InhibitorDocument113 pagesProtein Synthesis InhibitorAdeniran CharlesNo ratings yet
- The Drawing WebsiteDocument99 pagesThe Drawing WebsiteAdeniran CharlesNo ratings yet
- Haematologic Manifestations of Systemic DiseasesDocument38 pagesHaematologic Manifestations of Systemic DiseasesAdeniran CharlesNo ratings yet
- Clinical Blood TransfusionDocument13 pagesClinical Blood TransfusionAdeniran CharlesNo ratings yet
- Neuromuscular Pharmacology 305-1Document43 pagesNeuromuscular Pharmacology 305-1Adeniran CharlesNo ratings yet
- Invasive Ductal CarcinomaDocument3 pagesInvasive Ductal CarcinomaAdeniran CharlesNo ratings yet
- CM2-CU10-Modification of Mendelian RatiosDocument17 pagesCM2-CU10-Modification of Mendelian RatiosClaire GonoNo ratings yet
- GOBIOM BrochureDocument4 pagesGOBIOM BrochureGVK Bio Sciences Private LimitedNo ratings yet
- Circulatory System VCE BiologyDocument6 pagesCirculatory System VCE BiologyCallum KennyNo ratings yet
- Neonatal Resuscitation PDFDocument1 pageNeonatal Resuscitation PDFOdessa EnriquezNo ratings yet
- Paper 2 Biology 1996 Paper 2+ansDocument19 pagesPaper 2 Biology 1996 Paper 2+ansapi-3812894100% (1)
- NCC-61 With RET ENG - User Manual V2020 - 01 - 21 - 011900 (046-090)Document45 pagesNCC-61 With RET ENG - User Manual V2020 - 01 - 21 - 011900 (046-090)Zoulikifil Abdou KarimNo ratings yet
- The Circulatory System (Heart)Document3 pagesThe Circulatory System (Heart)NinaNo ratings yet
- Chapter 1: An Overview of Clinical LaboratoryDocument13 pagesChapter 1: An Overview of Clinical LaboratoryAshley Tañamor100% (2)
- Neonatal Jaundice DR - MaslianiDocument58 pagesNeonatal Jaundice DR - MaslianiHengky HanggaraNo ratings yet
- - ملحق كونكت بلس excellenceDocument17 pages- ملحق كونكت بلس excellenceDinaNo ratings yet
- Tourniquet Test (Capillary Fragility) : Normal Findings Indications Test ExplanationDocument2 pagesTourniquet Test (Capillary Fragility) : Normal Findings Indications Test ExplanationAaron James RuedasNo ratings yet
- Smart Breath 2014-05-26 Book ENGDocument34 pagesSmart Breath 2014-05-26 Book ENGAndrej MilutinovicNo ratings yet
- NCLEX Study GuideDocument7 pagesNCLEX Study Guidemmgoodall22100% (3)
- Tensiometro Shock ProofDocument2 pagesTensiometro Shock ProofjessikaNo ratings yet
- Du TestDocument14 pagesDu TestlalhaiagustinNo ratings yet
- Thrombocytopenia Pocket GuideDocument8 pagesThrombocytopenia Pocket GuideAnnisaValentKhanNo ratings yet
- Ijett V67i3p218Document4 pagesIjett V67i3p218nhel anonymousNo ratings yet
- Patient Name Age / Gender Uhid/Mr No. OP Visit No Sample Collected On: 03-07-2018 18:33 Reported On LRN# Specimen Ref DoctorDocument2 pagesPatient Name Age / Gender Uhid/Mr No. OP Visit No Sample Collected On: 03-07-2018 18:33 Reported On LRN# Specimen Ref DoctormukhleshNo ratings yet
- Transport in Humans - MCQDocument4 pagesTransport in Humans - MCQAhmed Kaleem Khan Niazi100% (1)
- Eurton Electric Co., Inc.: AbbottDocument16 pagesEurton Electric Co., Inc.: Abbottjose navaNo ratings yet
- Blood Bank Quality Manage 2797670Document21 pagesBlood Bank Quality Manage 2797670Rahul Behl0% (1)
- Understanding CBC Histogram PDFDocument17 pagesUnderstanding CBC Histogram PDFSuresh ShresthaNo ratings yet
- Foreign MagicksDocument63 pagesForeign MagicksMiguel Pérez García-PliegoNo ratings yet
- Camille Suzaine Pradas - Labs and DrugsDocument7 pagesCamille Suzaine Pradas - Labs and DrugsCamille Suzaine PradasNo ratings yet
- Concise Atlas of Basic HemopoiesisDocument14 pagesConcise Atlas of Basic HemopoiesisdynndgrNo ratings yet
- The Respiratory System 2019 dk-20191118110326Document26 pagesThe Respiratory System 2019 dk-20191118110326Jackson JastariNo ratings yet
- Report 10 46Document11 pagesReport 10 46Subham MukherjeeNo ratings yet
- Practical PathologyDocument94 pagesPractical Pathologyadi raghavNo ratings yet