Professional Documents
Culture Documents
Training Slides For Prescribing Clinicians
Training Slides For Prescribing Clinicians
Uploaded by
20SMB24 - Shafana0 ratings0% found this document useful (0 votes)
10 views15 pagesThis will help you to study in easier way
Original Title
5_TK3_P3T4-Training_Slides_for_Prescribing_Clinicians_Phase_3 (2)
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis will help you to study in easier way
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
10 views15 pagesTraining Slides For Prescribing Clinicians
Training Slides For Prescribing Clinicians
Uploaded by
20SMB24 - ShafanaThis will help you to study in easier way
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 15
Nursing Home Antimicrobial Stewardship Guide
Help Clinicians Choose the Right Antibiotic
Toolkit 3. How To Develop and Implement
an Antibiogram Program
Phase 3. Implementation
Training Slides for
Prescribing Clinicians
www.ahrq.gov/NH-ASPGuide ● May 2014
AHRQ Pub. No. 14-0023-5-EF
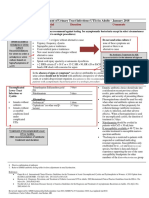
Ms. Lee
• Situation: dementia, dysuria, urinary frequency, and
urinary urgency.
• Vital signs are HR 88, RR 16, BP 136/84, T 100.2 F,
SpO2 98%.
• A urine dip shows 2+ leukocytes and 2+ nitrites.
• Which antibiotic do you prescribe?
– Oral quinolone (e.g., ciprofloxacin)
– Bactrim (Trimethoprim and Sulfamethoxazole)
– Cephalexin
– Nitrofurantoin
– Beta Lactam (e.g., amoxicillin)
– Amoxicillin + clavulanate (Augmentin®)
– An oral 3rd generation cephalosporin
– Other
Mr. Jones
• Situation: dementia, hypertension, and osteoarthritis. He has
been coughing for 3 days and developed a fever; has a
hacking cough; and is bringing up yellow/green sputum.
• Vital signs: T 100.5 F, HR 88, RR 16, BP 136/84, SpO2 95%.
• Which antibiotic do you prescribe?
– 3rd- or 4th-generation quinolone (e.g., levofloxacin)
– Macrolide (e.g., azithromycin)
– Beta Lactam (e.g., amoxicillin)
– Amoxicillin + clavulanate (Augmentin®)
– Bactrim (Trimethoprim and Sulfamethoxazole)
– Doxycycline
– 3rd generation cephalosporin (e.g., cefpodoxime)
Objectives
• Implement an antibiogram at this nursing
home
• Set a goal of improving initial (empiric)
prescribing of antibiotics
• Follow the impact of the antibiogram on
nursing home prescribing
Background: Antibiotic Prescribing
• Antibiotics are frequently prescribed in
nursing homes.
– Broad-spectrum antibiotics are frequently
prescribed.
• Initial antibiotic decisions are empiric;
clinician’s judgment is based on:
– Patient factors (e.g., age, symptoms)
– Nursing home factors (type, historical experience,
formulary)
– Preference/knowledge
Background: Antibiograms
• An antibiogram is a tool to provide
clinicians with local microbiologic
sensitivity data to assist in their empiric
prescribing.
• Hospitals have used antibiograms to:
– Identify important local resistance patterns.
– Increase recommended antibiotic prescribing
for acute infections.
Key Findings From Antibiogram
• Most data come from urine cultures:
– Of XX cultures used to make the antibiograms,
• XX % were urine cultures.
• XX % were wound cultures.
• XX % were sputum cultures.
– The antibiograms will be most applicable when selecting
antibiotics to treat urine infections and systemic infections that
may have come from the urine.
– The leading organisms for positive urine cultures were:
• E. coli: XX % of urine cultures
• Enterococcus species: XX %
• Klebsiella pneumoniae: XX %
• Proteus mirabilis: XX %
Key Findings From Antibiogram
Not all antibiotics are tested
•One antibiotic from each class is usually tested.
•Antibiotics from the same class are likely to have
similar resistance patterns; for example, with
cephalosporins:
– 1st generation: Cefazolin (Ancef) was tested; a
comparable oral agent is cephalexin (Keflex).
– 2nd generation: Cefoxitin (Mefoxin) was tested; a
comparable oral agent is cefuroxime (Ceftin).
– 3rd generation: Ceftriaxone (Rocephin) was tested; a
comparable oral agent is cefpodoxime (Simplicef, Vantin).
Key Findings From Antibiogram
Urinary tract infections (UTIs) from gram-negative organisms
•XX% of positive urine cultures were due to gram-negative
organisms.
•Significant resistance to commonly used antibiotics is seen
among the gram-negative organisms that frequently cause UTIs
(E. coli, Klebsiella):
– TMP/SMX (Bactrim) sensitivity for E. coli is limited (XX %).
– Quinolones’ sensitivity for E. coli is limited (levofloxacin [Levaquin] XX
%, ciprofloxacin [Cipro] XX %).
– First-generation cephalosporins’ sensitivity for E. coli is limited: cefazolin
(Ancef) XX %.
•Nitrofurantoin (Macrobid) has good sensitivity for E. coli (XX %)
but poor activity against other urinary pathogens.
Key Findings From Antibiogram
Gram positives
•XX of XX (XX %) Staphylococcus aureus
cultures were methicillin-resistant
Staphylococcus aureus (MRSA).
•MRSA was XX% sensitive to TMP/SMX
(Bactrim), but only XX% was sensitive to
clindamycin (Cleocin).
Ms. Lee
• Situation: dementia, dysuria, urinary frequency, and
urinary urgency.
• Vital signs are HR 88, RR 16, BP 136/84, T 100.2 F,
SpO2 98%. A urine dip shows 2+ leukocytes and 2+
nitrites.
• Which antibiotic do you prescribe?
– Oral quinolone (e.g. ,ciprofloxacin)
– Bactrim (Trimethoprim and Sulfamethoxazole)
– Cephalexin
– Nitrofurantoin
– Beta Lactam (e.g., amoxicillin)
– Amoxicillin + clavulanate (Augmentin®)
– An oral 3rd generation cephalosporin
– Other
Mr. Jones
• Situation: dementia, hypertension, and osteoarthritis. He
has had a hacking cough for 3 days, developed a fever,
and is bringing up yellow/green sputum.
• Vital signs: T 100.5 F, HR 88, RR 16, BP 136/84, SpO2
95%.
• Which antibiotic do you prescribe?
– 3rd or 4th generation quinolone (e.g. ,levofloxacin)
– Macrolide (e.g., azithromycin)
– Beta Lactam (e.g., amoxicillin)
– Amoxicillin + clavulanate (Augmentin®)
– Bactrim (Trimethoprim and Sulfamethoxazole)
– Doxycycline
– 3rd generation cephalosporin (e.g., cefpodoxime)
Limitations
• Source of infection
– “Hospital-acquired”: so nursing home
microbiology and antibiogram are less
applicable.
– “Facility-acquired”: acquired while at nursing
home; therefore, antibiogram is more
applicable.
• Sample size:
– Organisms with fewer than 30 isolates should
be interpreted with caution, as small numbers
may bias the group susceptibilities.
Questions?
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5825)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Urine Analysis ExaminationDocument28 pagesUrine Analysis ExaminationAnna AgustinaNo ratings yet
- A New Point-Of-Care Test For The Rapid Detection of Urinary Tract InfectionsDocument8 pagesA New Point-Of-Care Test For The Rapid Detection of Urinary Tract InfectionsAntika CahyatiNo ratings yet
- Isk - AapDocument14 pagesIsk - AapRoberto SoehartonoNo ratings yet
- Study of Relationship Between Anemia and Urinary Tract Infection in Pregnant WomenDocument5 pagesStudy of Relationship Between Anemia and Urinary Tract Infection in Pregnant WomenIvana ThiodoraNo ratings yet
- UTI Guideline Example 2 Appendix B PDFDocument4 pagesUTI Guideline Example 2 Appendix B PDFamira catriNo ratings yet
- Urinary EliminationDocument50 pagesUrinary EliminationAime MvuyekureNo ratings yet
- Utiva - Ultimate UTI Guide - Ebook - Final LinkDocument58 pagesUtiva - Ultimate UTI Guide - Ebook - Final Linkciliazt togepNo ratings yet
- CL7 Urinary Tract Infection 20192020-20191212060056Document50 pagesCL7 Urinary Tract Infection 20192020-20191212060056Nur Ain IzzatiNo ratings yet
- Lecture ISK UKI - Dr. Sahala Panggabean SP - PDDocument25 pagesLecture ISK UKI - Dr. Sahala Panggabean SP - PDBen HonorseekerNo ratings yet
- K - 9 Urinary Tract Infection (Ilmu Penyakit Dalam)Document24 pagesK - 9 Urinary Tract Infection (Ilmu Penyakit Dalam)Ruthra Devi NarayanasamyNo ratings yet
- Infectious Disease Essentials HandbookDocument157 pagesInfectious Disease Essentials HandbookCalin Popa100% (3)
- Prostate Biopsy - UpToDateDocument47 pagesProstate Biopsy - UpToDateCésar Aguirre RomeroNo ratings yet
- Apsic Guide For Prevention of Catheter Associated Urinary Tract Infections (Cautis)Document5 pagesApsic Guide For Prevention of Catheter Associated Urinary Tract Infections (Cautis)Sari DeviNo ratings yet
- Case Report: Chromobacterium Violaceum: A Rare Cause of UrinaryDocument3 pagesCase Report: Chromobacterium Violaceum: A Rare Cause of UrinaryHyacinth A RotaNo ratings yet
- Thomas M Hooton, MD Kalpana Gupta, MD, MPH Stephen B Calderwood, MD Allyson Bloom, MDDocument14 pagesThomas M Hooton, MD Kalpana Gupta, MD, MPH Stephen B Calderwood, MD Allyson Bloom, MDMusicBestLiveNo ratings yet
- EAU Guidelines Urological Infections 2016 1 PDFDocument16 pagesEAU Guidelines Urological Infections 2016 1 PDFMaria Jose Zamorano SepulvedaNo ratings yet
- Urinary Tract Infection: PGI FRANCISCO, Maria Ellaine Pgi Galvez, AngeloDocument74 pagesUrinary Tract Infection: PGI FRANCISCO, Maria Ellaine Pgi Galvez, AngeloNica Lopez FernandezNo ratings yet
- Aynadis Thesis CorrectedDocument78 pagesAynadis Thesis CorrectedBantider GetachewNo ratings yet
- 09 Urinary Tract Infections in The ElderlyDocument19 pages09 Urinary Tract Infections in The Elderlypatel bhaumikNo ratings yet
- Guía de Práctica Clínica Europea ITUDocument7 pagesGuía de Práctica Clínica Europea ITUVICTORIA GONZALEZ VEGANo ratings yet
- 1242 5026 1 PBDocument5 pages1242 5026 1 PBivanNo ratings yet
- Urinary Tract Infection (UTI) in Males: Signs and SymptomsDocument33 pagesUrinary Tract Infection (UTI) in Males: Signs and Symptomssyak turNo ratings yet
- Urinary Tract Infections Core Curriculum 2024Document11 pagesUrinary Tract Infections Core Curriculum 2024Amanda EscorciaNo ratings yet
- 1 35Document8 pages1 35Saiful HudaNo ratings yet
- Management of CAUTIDocument7 pagesManagement of CAUTIsunil abrahamNo ratings yet
- Moh A. Pps Hcai Manual 2.12.21Document136 pagesMoh A. Pps Hcai Manual 2.12.21Nurfarzana NadhirahNo ratings yet
- Campeel IutDocument86 pagesCampeel IutRosa TorresNo ratings yet
- Catheter-Associated UTIDocument54 pagesCatheter-Associated UTIAmeng GosimNo ratings yet
- ELE - PID Treatment To UTI and ProstatitisDocument10 pagesELE - PID Treatment To UTI and ProstatitisJane DoeNo ratings yet
- AUA GuidelinesDocument9 pagesAUA GuidelinesAna Maria rendonNo ratings yet