Professional Documents
Culture Documents
ICU One Pager Ketoacidosis v11
ICU One Pager Ketoacidosis v11
Uploaded by
Juan R Hernandez Lozano0 ratings0% found this document useful (0 votes)
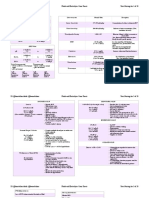
23 views1 pageThis document summarizes different types of ketosis disorders including their etiologies, presentations, and treatments.
Starvation ketosis results from fatty acid metabolism during starvation. Alcoholic ketoacidosis occurs in chronic alcoholics. Diabetic ketoacidosis is caused by complete insulin deficiency leading to high blood glucose and acidosis. Hypeglycemic hyposmolar state involves partial insulin deficiency causing high blood glucose and osmolality. The causes of diabetic ketoacidosis and hypeglycemic hyposmolar state should be investigated and treatment involves insulin, intravenous fluids, and electrolyte management.
Original Description:
Original Title
ICU_One_Pager_Ketoacidosis_v11
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document summarizes different types of ketosis disorders including their etiologies, presentations, and treatments.
Starvation ketosis results from fatty acid metabolism during starvation. Alcoholic ketoacidosis occurs in chronic alcoholics. Diabetic ketoacidosis is caused by complete insulin deficiency leading to high blood glucose and acidosis. Hypeglycemic hyposmolar state involves partial insulin deficiency causing high blood glucose and osmolality. The causes of diabetic ketoacidosis and hypeglycemic hyposmolar state should be investigated and treatment involves insulin, intravenous fluids, and electrolyte management.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
23 views1 pageICU One Pager Ketoacidosis v11
ICU One Pager Ketoacidosis v11
Uploaded by
Juan R Hernandez LozanoThis document summarizes different types of ketosis disorders including their etiologies, presentations, and treatments.
Starvation ketosis results from fatty acid metabolism during starvation. Alcoholic ketoacidosis occurs in chronic alcoholics. Diabetic ketoacidosis is caused by complete insulin deficiency leading to high blood glucose and acidosis. Hypeglycemic hyposmolar state involves partial insulin deficiency causing high blood glucose and osmolality. The causes of diabetic ketoacidosis and hypeglycemic hyposmolar state should be investigated and treatment involves insulin, intravenous fluids, and electrolyte management.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 1
ETOSIS DISORDERS
by Nick Mark MD ONE
onepagericu.c
om
Link to the
most current
ETIOLOGY OF KETOSIS version →
Ketone bodies are a normal metabolic energy source. Excessive unregulated production of @nickmmark
ketones, often accompanied by an anion gap acidosis, is seen in several disease states: Starvation Euglycemic DKA/HHS
AKA DKA HHS
Ketosis DKA Overlap
· Starvation ketosis – normal consequence of fatty acid (FA) metabolism. Tx: provide
carbohydrates (IVF or PO): The pt will produce endogenous insulin normally. Treat Physiologic Seen in Seen w/ SGLT2 DM1 (or ketosis DM1/2 DM2
other deficiencies (thiamine). Monitor for development of re-feeding syndrome. Etiology switch to FA chronic inhibitors, prone DM2) Highest mo
metabolism. alcoholics pregnancy Young > elderly rtality Elderly > young
· Alcoholic ketoacidosis (AKA) – seen in chronic alcoholics, often can be treated
with dextrose containing IVF & thiamine. Treat concomitant alcohol withdrawal.
· Diabetic ketoacidosis (DKA) – caused by complete insulin deficiency, leading to 800-
BG (mg/dL) <250 <250 <250 400-800 >800-1200
1000
marked anion gap acidosis (pH < 7.35) w/ elevated blood glucose. Euglycemic DKA is
a variant seen with SGLT inhibitors & pregnancy, where blood glucose (BG) is normal. Ketones ++++ ++ +++ +++ + -
· Hypeglycemic hyposmolar state (HHS) –partial insulin deficiency, causing minimal
ketosis but marked increase in BG & osmolality. Glucosuria causes massive volume loss. Acidosis - ++ +++ +++ ++ +
· DKA/HHS Overlap – features of both DKA & HHS and treated the same.
Fluid deficit (L) - - 2-4 L 6-8 L 6-10 LWhen BG 8-10 L
CAUSES/WORKUP OF DKA/HHS INSULIN bolus & gtt When AG
Identifying the cause of DKA/HHS is essential, because missing the underlying WHICH KETONE TO CHECK?
normal, add closed give
glucose to IVF SQ INSULIN
etiology is responsible for much of the morbidity/mortality. Consider the 5 I’s: Checking BHB is more accurate (fewer false positives & false negatives)
BG, AG, & Fluid Deficit
Etiology Workup Nitroprusside urine test is unreliable.
Infection BCx, Ucx, Procalcitonin, CXR, exam, POCUS Fatty acid (FA) IVF boluses for
breakdown hypovolemic
Ischemia Lactate, Troponin, EKG shock
β-hydroxybutyrate Acetoacetate Acetone NORMAL RANGE
Inflammation Lipase, CRP Gradual correction of
remaining fluid deficit
Blood test Urine test Breath test or
Intoxication Serum Osmolarity (Osm), Blood EtOH, Utox
(most accurate) (semi-quantitative) “sweat” breath odor INITIAL INTERMEDIATE RESOLUTION
Insulin (deficiency) History (e.g. ran out of insulin, oral meds)
Phase
Consider new meds (e.g. steroids, diuretics, etc) INITIAL PHASE INTERMEDIATE PHASE RESOLUTION PHASE
Resuscitation & stabilization Gradual correction Normalization & de-escalation
TREATMENT OF KETOSIS: INSULIN Bolus INSULIN 10 units IV then Adjust INSULIN gtt to achieve
Once AG closed, give SQ
The three pillars of treating DKA/HHS are INSULIN GOAL: correct BG, AG, & acidosis INSULIN. 0.1 units/kg. Stop
Start INSULIN gtt 0.1 units/kg/hr 50 mg/dL/hr reduction in BG INSULIN gtt 2 hrs later
(to stop ketogenesis), IVF (to restore fluid deficit & Monitor BG, Chem10
correct hyperosmolarity), & ELECTROLYTES (to
(Don’t add K to IVF as it
correct numerous derangements & prevent arrythmia) slows rate of infusion)
HHS requires more FLUID and less INSULIN than DKA Replete K+ to >4 mEq/L Use caution if K+ < 3.3 mmol/L; Resume diet; Start
ELECTROLYTES
(because of greater fluid deficit and less acidosis) (ideally both PO and IV) consider decreasing insulin gtt basal, prandial, &
GOAL: normalize K+, Mg2+, Ca2+, PO4, correction INSULIN.
Mild DKA can be treated with SQ INSULIN in the ED and HCO3 to avoid arrythmias If HCO3 < 6.9 give Correct Mg deficits to
Stop IVF. Begin oral
or medical wards (does not require ICU admission) Monitor Chem10, ± VBG, EKG NaHCO3 bolus ± gtt reduce further K wasting
ELECTROLYTE
v1.1 (2022-06-14) CC BY-SA 3.0
(Acidosis greatly increases the risk replacement.
Expected AG is 2.5x albumin (usually <12 mOsm/L); of cardiac arrest during intubation;
with treatment AG should normalize to expected consider NIPPV)
Replace fluid deficits with
AG. If not improving consider concomitant IV FLUID isotonic IVF ~200 ml/hr Once
GOAL: restore circulating volume, tolerating PO
lactic acidosis or other metabolic derangement. If in hypovolemic shock,
correct fluid deficit & hyperosmolarity, correct rapidly w/ IVF boluses Once corrected Na is >140
Corrected Sodium accounts for spurious low Na+ avoid cerebral edema by correcting the mEq/L switch to hypotonic IVF When BG < 200 mg/dL switch
(e.g. 1 L of LR or 0.9% NS)
measurements when blood glucose is high. For corrected sodium gradually. to avoid overcorrection to glucose containing IVF
every 100 mg/dL increase in BG, the corrected Na (Use volume responsiveness to guide (e.g. D5LR or D5 ½NS)
calculate corrected Na & Fluid Deficit (e.g. 0.45% NS, LR)
resuscitation; Consider balanced
is increased by 2.4 mEq/L. Monitor Osm, serum Na, urine output crystalloids. E.g Plasmalyte 148)
You might also like
- OutlineDocument3 pagesOutlineTuấn NguyễnNo ratings yet
- DKA HHS Johns Hopkins Hospital PDFDocument1 pageDKA HHS Johns Hopkins Hospital PDFAsdruval ZepedaNo ratings yet
- Chronic Wounds PowerpointDocument34 pagesChronic Wounds PowerpointAnin DitaNo ratings yet
- ICU One Pager KetoacidosisDocument1 pageICU One Pager KetoacidosisjalilNo ratings yet
- ICU One Pager Ketoacidosis v12Document1 pageICU One Pager Ketoacidosis v12jhngzpk6tsNo ratings yet
- Use of Urine Electrolytes and Urine Osmolality in The Clinical Diagnosis of Fluid, Electrolytes, and Acid-Base DisordersDocument14 pagesUse of Urine Electrolytes and Urine Osmolality in The Clinical Diagnosis of Fluid, Electrolytes, and Acid-Base Disordersrogelio cruzNo ratings yet
- KAadD IMELasS (Compatibility Mode)Document26 pagesKAadD IMELasS (Compatibility Mode)Jennifer BryantNo ratings yet
- Hyperglycemia DKA and HHSDocument39 pagesHyperglycemia DKA and HHSYasir MehmoodNo ratings yet
- Urine Osmolality in The Clinical Diagnosis of Fluid, Electrolytes, and Acid-Base DisordersDocument14 pagesUrine Osmolality in The Clinical Diagnosis of Fluid, Electrolytes, and Acid-Base DisordersLuis octavio carranzaNo ratings yet
- Diabetic Ketoacidosis (DKA) & Hyperglycemic Hyperosmolar State (HHS)Document36 pagesDiabetic Ketoacidosis (DKA) & Hyperglycemic Hyperosmolar State (HHS)Ismail GunawanNo ratings yet
- Diabetic KetoacidosisDocument7 pagesDiabetic Ketoacidosismm7--No ratings yet
- 23.Keto-Asidosis DiabetikDocument30 pages23.Keto-Asidosis DiabetikmutiaNo ratings yet
- Diabetic KetoacidosisDocument9 pagesDiabetic KetoacidosisFeliipe CruzzNo ratings yet
- Fluid - Electrolytes Cram SheetDocument20 pagesFluid - Electrolytes Cram SheetMark Jefferson LunaNo ratings yet
- Group 2 DkaDocument59 pagesGroup 2 DkaAkio OzaragaNo ratings yet
- Fluid & Electrolytes Cram SheetDocument20 pagesFluid & Electrolytes Cram SheetTine GuibaoNo ratings yet
- ENDO 6B. Acute Complications of DMDocument6 pagesENDO 6B. Acute Complications of DMCharisse Angelica MacedaNo ratings yet
- Ketone Bodies CVDDocument10 pagesKetone Bodies CVDPeter McPhersonNo ratings yet
- (Biochem B) Overview of Metabolism-Viliran (Cheezus)Document10 pages(Biochem B) Overview of Metabolism-Viliran (Cheezus)bero beroNo ratings yet
- Diabetic-Ketoacidosis Queensland PDFDocument4 pagesDiabetic-Ketoacidosis Queensland PDFroshan bhandariNo ratings yet
- Module 7-Git DrugsDocument10 pagesModule 7-Git DrugsAlexa De GuzmanNo ratings yet
- Biochem - Beta Oxidation, Lipid, Fatty Acid and EicosanoidsDocument6 pagesBiochem - Beta Oxidation, Lipid, Fatty Acid and EicosanoidscosmoNo ratings yet
- Aspirin Overdose Pathophysiology and Treatment: Supplemental GlucoseDocument6 pagesAspirin Overdose Pathophysiology and Treatment: Supplemental GlucoseJohnNo ratings yet
- DKA and HHS The Washington Manual of Critical CareDocument6 pagesDKA and HHS The Washington Manual of Critical Careمحمد عقيلي100% (1)
- Niara Baksh and Selina Beharry - Ketoacidosis ProjectDocument7 pagesNiara Baksh and Selina Beharry - Ketoacidosis ProjectSelina BeharryNo ratings yet
- BCCH Diabetic Ketoacidosis Protocol Toolkit: Endocrinology & Diabetes UnitDocument16 pagesBCCH Diabetic Ketoacidosis Protocol Toolkit: Endocrinology & Diabetes UnitaseelNo ratings yet
- Hypokalemia FT 2020Document49 pagesHypokalemia FT 2020ebkai98No ratings yet
- Coma Hyperglycemic Hyperosmolar NonketoticDocument10 pagesComa Hyperglycemic Hyperosmolar NonketoticD An0% (1)
- Diabetic Ketoacidosi S: Prepared byDocument28 pagesDiabetic Ketoacidosi S: Prepared byفيصل الاعرجNo ratings yet
- BiochemistryDocument17 pagesBiochemistryrohishaakNo ratings yet
- The Pathophysiology & Practical Management of Diabetic Ketoacidosis - 2006Document43 pagesThe Pathophysiology & Practical Management of Diabetic Ketoacidosis - 2006Sri NathNo ratings yet
- Dka AlgorithmDocument1 pageDka AlgorithmAbhinav AggarwalNo ratings yet
- Diabetic Ketoacidosis in ChildrenDocument6 pagesDiabetic Ketoacidosis in ChildrenviharadewiNo ratings yet
- Cad Primer 2020 PDFDocument20 pagesCad Primer 2020 PDFVictor Rojas SahagúnNo ratings yet
- Hyperglycemic Emergencies: Boston University School of Medicine July, 2013 Marie Mcdonnell, MDDocument62 pagesHyperglycemic Emergencies: Boston University School of Medicine July, 2013 Marie Mcdonnell, MDBeyene FelekeNo ratings yet
- Diabetic KetoacidosisDocument37 pagesDiabetic KetoacidosisjjNo ratings yet
- Msud FinalDocument14 pagesMsud Finals2023100336No ratings yet
- Hyperglycemic CrisisDocument25 pagesHyperglycemic CrisisVentya Edita Madelyn SimamoraNo ratings yet
- 77-Ketone Bodies PDFDocument3 pages77-Ketone Bodies PDFmakram_0451No ratings yet
- BiochemistryDocument38 pagesBiochemistryPrachiSinghNo ratings yet
- 107208crwill 1Document80 pages107208crwill 1Ayush GuptaNo ratings yet
- Ketones and The Cardiovascular SystemDocument13 pagesKetones and The Cardiovascular Systemmiguel saba sabaNo ratings yet
- Final Corrected DKA AselaDocument32 pagesFinal Corrected DKA AselaabelNo ratings yet
- Diabetes Metabolism Res - 2000 - Laffel - Ketone Bodies A Review of Physiology Pathophysiology and Application ofDocument15 pagesDiabetes Metabolism Res - 2000 - Laffel - Ketone Bodies A Review of Physiology Pathophysiology and Application ofLê Hữu ToànNo ratings yet
- Cetoacidosis y Edo Hiperglicemico HiperO 2013Document19 pagesCetoacidosis y Edo Hiperglicemico HiperO 2013RosolinaNo ratings yet
- The Biochemical Panel: Is The Diagnosis Hiding in Plain Site?Document47 pagesThe Biochemical Panel: Is The Diagnosis Hiding in Plain Site?Silvia RoseNo ratings yet
- Pediatric Diabetic Ketoacidosis (DKA) Algorithm (Page 1-ED) : DKA Diagnosed DKA Not DiagnosedDocument2 pagesPediatric Diabetic Ketoacidosis (DKA) Algorithm (Page 1-ED) : DKA Diagnosed DKA Not Diagnosedrolland_arrizaNo ratings yet
- DKA ProtocolDocument3 pagesDKA Protocolpinky222255554100% (1)
- Ipd - Kelas Ac - Kad Dan Hhs - DR - DR.K Heri Nugroho HS, SP - PD, K-EmdDocument51 pagesIpd - Kelas Ac - Kad Dan Hhs - DR - DR.K Heri Nugroho HS, SP - PD, K-EmdTeresia MaharaniNo ratings yet
- Liddle, Gitelman, BarterDocument2 pagesLiddle, Gitelman, BarterHildemaro GutierrezNo ratings yet
- Molluscan: Inhibition of Protein Synthesis Prolongs Ca2 - Mediated Reduction of K+ Currents in NeuronsDocument5 pagesMolluscan: Inhibition of Protein Synthesis Prolongs Ca2 - Mediated Reduction of K+ Currents in NeuronsAmale RachaNo ratings yet
- Diabetes TestingDocument16 pagesDiabetes TestingyamaNo ratings yet
- DKA Management Algorithm Adult Patients 230525Document1 pageDKA Management Algorithm Adult Patients 230525Haneen FaqeehNo ratings yet
- Emergency HyperglicemicDocument5 pagesEmergency HyperglicemicerwinNo ratings yet
- Diabetic Ketoacidosis: Presented By:dr. Hina Asif AbbasiDocument11 pagesDiabetic Ketoacidosis: Presented By:dr. Hina Asif AbbasiAzhar AliNo ratings yet
- Metabolism of Ketone BodiesDocument22 pagesMetabolism of Ketone BodiesUbaid AhmedNo ratings yet
- Shelly DKADocument18 pagesShelly DKARizkyastari OnnyNo ratings yet
- Ketone Bodies-A Review of Physiology, Pathophysiology and Application of Monitoring To DiabetesDocument15 pagesKetone Bodies-A Review of Physiology, Pathophysiology and Application of Monitoring To DiabetesCamilo VidalNo ratings yet
- K Disorders CCN PDFDocument14 pagesK Disorders CCN PDFLuis CuestaNo ratings yet
- Diabetic Ketoacidosis (Dka)Document18 pagesDiabetic Ketoacidosis (Dka)dr.Bobi Ahmad Sahid, S.Kep100% (2)
- Biochem One LinersDocument25 pagesBiochem One LinersRv DeanNo ratings yet
- Anjana Bhattacharjee - Self ConceptDocument4 pagesAnjana Bhattacharjee - Self Conceptmademerlin92No ratings yet
- Ausi DentalDocument451 pagesAusi DentalWaf EtanoNo ratings yet
- Anaphylaxis - 1Document12 pagesAnaphylaxis - 1Ronald WiradirnataNo ratings yet
- Lesson Plan Eating Disorser in AdolscenceDocument38 pagesLesson Plan Eating Disorser in AdolscencePreeti lata KujurNo ratings yet
- Checklist For Delivery RoomDocument4 pagesChecklist For Delivery RoomKarl Kiw-isNo ratings yet
- Digestive SystemDocument45 pagesDigestive SystemEzequiel ManluluNo ratings yet
- Harm ReductionDocument2 pagesHarm ReductionDarren CariñoNo ratings yet
- The Effects of Alcohol To The Academic Performance of Senior High School StudentDocument9 pagesThe Effects of Alcohol To The Academic Performance of Senior High School Studentjohn taylorNo ratings yet
- Petition To Remove James Wiley Conservator of The Estate of Henry C.MunozDocument2 pagesPetition To Remove James Wiley Conservator of The Estate of Henry C.MunozpropertylenderNo ratings yet
- Tuberculosis of Bones and JointsDocument19 pagesTuberculosis of Bones and JointsreinNo ratings yet
- Poster FinalDocument1 pagePoster Finalapi-652215108No ratings yet
- Two Ethics Case ScenariosDocument3 pagesTwo Ethics Case ScenariosEguia NielNo ratings yet
- KROMA RESET BROCHURE 9aug23revDocument36 pagesKROMA RESET BROCHURE 9aug23revvianca.v.vazquezNo ratings yet
- Rupees 80 Thousand Monthly Salary-Ayurveda DRDocument2 pagesRupees 80 Thousand Monthly Salary-Ayurveda DRAyushiBamstuition Dr ArathiNo ratings yet
- Mom-20 03 2024Document7 pagesMom-20 03 2024smn.ussharNo ratings yet
- Guidelines For The Management of Traumatic Dental Injuries: 2. Avulsion of Permanent TeethDocument6 pagesGuidelines For The Management of Traumatic Dental Injuries: 2. Avulsion of Permanent TeethAminatu Nur RahmaNo ratings yet
- Autoclaving LaryngoscopeDocument7 pagesAutoclaving Laryngoscopelarst06No ratings yet
- Country Fiche NL - Final - RevisedDocument5 pagesCountry Fiche NL - Final - RevisedPranav DubeyNo ratings yet
- Manual Handling TrainingDocument19 pagesManual Handling TrainingMadhan MNo ratings yet
- Hepatomegaly PDFDocument9 pagesHepatomegaly PDFKhadija IbrahimNo ratings yet
- Advanced English For Nursing English DialogueDocument4 pagesAdvanced English For Nursing English Dialogueirfani28No ratings yet
- NCPDocument4 pagesNCPRachel PerandoNo ratings yet
- EHS Programme - PPT FormatDocument1 pageEHS Programme - PPT FormatMesha100% (1)
- Leadership Roles in Disaster NursingDocument2 pagesLeadership Roles in Disaster NursingLouisse Angeli AbucejoNo ratings yet
- 1.113.medication Administration TimingDocument14 pages1.113.medication Administration TimingSophiaNo ratings yet
- Looking For A Keynote SpeakerDocument6 pagesLooking For A Keynote SpeakerSN NairNo ratings yet
- S. No Topic Learning Objectives: P.D.A Building, Block # IV, Phase-V, Hayatabad PeshawarDocument2 pagesS. No Topic Learning Objectives: P.D.A Building, Block # IV, Phase-V, Hayatabad PeshawarWaqasNo ratings yet
- Assignment 1 TQM Waqar Haider 1811199Document2 pagesAssignment 1 TQM Waqar Haider 1811199waqar HaiderNo ratings yet