Professional Documents
Culture Documents
Oculomotor Nerve 3
Oculomotor Nerve 3
Uploaded by
Sanreet Randhawa0 ratings0% found this document useful (0 votes)
27 views30 pagesThe oculomotor nerve (CN III) provides both motor and parasympathetic innervation to eye structures. It innervates most of the extraocular muscles except the lateral rectus and superior oblique muscles. The parasympathetic fibers from the oculomotor nerve relay in the ciliary ganglion before innervating the sphincter pupillae and ciliary muscles. Damage to the oculomotor nerve results in ptosis, external strabismus, dilated pupil, and impairment of accommodation.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe oculomotor nerve (CN III) provides both motor and parasympathetic innervation to eye structures. It innervates most of the extraocular muscles except the lateral rectus and superior oblique muscles. The parasympathetic fibers from the oculomotor nerve relay in the ciliary ganglion before innervating the sphincter pupillae and ciliary muscles. Damage to the oculomotor nerve results in ptosis, external strabismus, dilated pupil, and impairment of accommodation.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
27 views30 pagesOculomotor Nerve 3
Oculomotor Nerve 3
Uploaded by
Sanreet RandhawaThe oculomotor nerve (CN III) provides both motor and parasympathetic innervation to eye structures. It innervates most of the extraocular muscles except the lateral rectus and superior oblique muscles. The parasympathetic fibers from the oculomotor nerve relay in the ciliary ganglion before innervating the sphincter pupillae and ciliary muscles. Damage to the oculomotor nerve results in ptosis, external strabismus, dilated pupil, and impairment of accommodation.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 30
Oculomotor Nerve
& Ciliary Ganglion
DR KANIKA SACHDEVA
PROFESSOR ANATOMY
• The oculomotor nerve - Third cranial nerve (CN III).
• It provides motor and parasympathetic innervation to some of the
structures within the bony orbit.
• Functions:
1. Motor – Innervates the majority of the extraocular muscles (levator
palpebrae superioris, superior rectus, inferior rectus, medial rectus
and inferior oblique).
2. Parasympathetic – Supplies the sphincter pupillae and the ciliary
muscles of the eye.
3. Sympathetic – No direct function, but sympathetic fibres run with
the oculomotor nerve to innervate the superior tarsal muscle (helps
to raise the eyelid).
Functional Components of Oculomotor Nerve
1. General Somatic Efferent Fibres/ Somato motor fibres:
• Supply all extraocular muscles except Lateral Rectus (supplied by 6th cranial
nerve) and superior oblique (supplied by 4th cranial nerve).
• The GSE fibres arise from the somatic component of oculomotor nucleus (also
called the somatic motor nucleus).
2. General visceral efferent fibres:
• They supply the sphincter pupillae and ciliaris muscles.
• They arise from the parasympathetic component of oculomotor nucleus (also
called the Edinger–Westphal nucleus).
• These are preganglionic parasympathetic fibres and relay in the ciliary
ganglion.
• The postganglionic parasympathetic fibres arise from the ganglion and supply
the sphincter pupillae and ciliaris muscles.
3. Proprioreceptive Fibres: from most of extra ocular muscles. Cell
bodies of these neurons are located in mesencephalic nucleus of
trigeminal nerve
Functional Components & nuclei of Oculomotor Nerve
Central Connections of Oculomotor Nerve
• The oculomotor nucleus is situated in the ventromedial part of central grey
matter of midbrain at the level of superior colliculus. Ventrolaterally, it is
closely related to the medial longitudinal bundle.
• The nucleus is connected:
1. To the pyramidal tracts of both sides which form the supranuclear pathway
of the nerve.
2. To the pretectal nuclei of both sides for the direct & concensual light reflex.
3. To medial longitudinal fasciculus by which it is connected to the 4th , 6th &
8th for coordination of the eye movements.
4. To the tectobulbar tract by which it is connected to visual cortex through
superior colliculus for visuoprotective reflexes.
5. To mesencephalic nucleus of trigeminal nerve.
Oculomotor Nuclear Complex
• CCN: Caudal Central Nucleus
• DLN: Dorso lateral Nucleus
• EWN: Edinger Westphal Nucleus
• IN: Intermediate Nucleus
• RN: Raphe Nucleus
• VMN: Ventro Median Nucleus
• (IO): Inferior Obliques
• (IR): Inferior Rectus
• (LPS): Levator Palpabrae Superioris
• (MR): Medial Rectus
• (SR): Superior Rectus
• All muscles of eyeball are suppled by ipsilateral
neurons except superior rectus & LPS which
are supplied bilaterally
The nuclear complex includes the following parts
• Dorsolateral—to supply inferior rectus muscle
• Intermediate—to inferior oblique
• Ventromedial—to medial rectus
• Caudal central—to part of levator palpabrae superioris
• Median raphe—to superior rectus
• Edinger-Westphal—to ciliaris and sphincter pupillae muscles.
Course
Superficial Origin of Nerve:
• From Oculomotor nuclear complex, fibres pass forwards forming a series of convex
lateral curves through tegmentum of midbrain, red nucleus & medial part of
substantia nigra
• Fibres form a single nerve trunk which passes through a sulcus on medial side of
cerebral peduncles of midbrain and appears in the interpeduncular fossa.
Course at base of brain & intracranial course:
• Runs forward and laterally in interpeduncular cistern between the posterior
cerebral and superior cerebellar arteries and lateral to the posterior
communicating artery
• Passes through the tentorial notch of tentorium cerebelli to reach the middle
cranial fossa.
• It pierces the dura mater in the oculomotor triangle lying in between the free and
attached margins of tentorium cerebelli in the roof of the cavernous sinus and
enters the lateral wall of the cavernous sinus.
Relation of Oculomotor nerve and cavernous
sinus
Intracavernous Course:
• Enters cavernous sinus by piercing posterior
part of roof on lateral side of posterior
clinoid process.
• Soon it descends in lateral wall of sinus
where it lies superior to the trochlear,
ophthalmic, and maxillary nerves, and lateral
to the internal carotid artery.
• In the anterior part of the cavernous sinus,
the nerve divides into upper and lower
divisions: small superior & larger lower
rami.
Intracavernous Course
In the Orbit:
• The two divisions enter the orbit through the middle part of superior
orbital fissure within the common tendinous ring/ Annular ring of Zinn.
• The nasociliary nerve intervenes between the two divisions & abducent
nerve lies inferolateral to inferior division.
• The smaller upper division passes above the optic nerve on the inferior
surface of superior rectus (which it supplies), and then passes through the
superior rectus to supply the levator palpebrae superioris
• The larger inferior division of the oculomotor nerve passes below the optic
nerve and immediately gives three branches which supply the medial
rectus, inferior rectus, and inferior oblique muscles.
• The nerve to inferior oblique is longest & gives preganglionic
parasympathetic/motor fibres to the ciliary ganglion
Superior Orbital Fissure
Branches of Oculomotor Nerve
Oculomotor Nerve Palsy
The most common structural causes include:
• Compression by aneurysm of the posterior communicating artery as it
passes between posterior cerebral and superior cerebellar arteries.
• Compression by aneurysm of the internal carotid artery as it passes
through the lateral wall of the cavernous sinus.
• Compression by transtentorial uncal herniation as it passes through the
tentorial notch, Raised intracranial pressure (compresses the nerve against
the temporal bone).
• Cavernous sinus infection or trauma.
• Other pathological causes of oculomotor nerve palsy such as diabetes,
multiple sclerosis, myasthenia gravis and giant cell arteritis
Clinical features of CN III injury are associated with the eye:
• Ptosis (drooping upper eyelid) – due to paralysis of the levator palpabrae superioris and
unopposed activity of the orbicularis oculi muscle.
• Lateral squint/ External Strabismus: ‘Down and out‘ position of the eye at rest – due to
paralysis of the superior, inferior and medial rectus, and the inferior oblique (and therefore
the unopposed activity of the lateral rectus and superior oblique).
The patient is unable to elevate, depress or adduct the eye.
• Dilated pupil – due to the unopposed action of the dilator pupillae muscles due to paralysis
of parasympathetic fibres to sphincter pupillae muscle.
• Loss of accommodation due to paralysis of ciliary muscles
• Slight proptosis, i.e. forward projection of the eye, due to relaxation of the muscles of the
eyeball.
• Diplopia/ double vision occurs on looking medially, inferiorly, and superiorly, due to paraly-
sis of the medial rectus, inferior rectus, and inferior oblique muscles.
• Pupillary light reflex in affected eye is absent : Pupil dilates and becomes fixed to light
• Right oculomotor nerve palsy, characterised by the ‘down and
out’ dilated pupil with ipsilateral ptosis
• A midbrain lesion causing contralateral hemiplegia and ipsilateral
paralysis of the third nerve is known as Weber’s syndrome- due to
interruption of corticospinal tract of cerebral peduncles.
• Supranuclear paralysis of the third nerve causes loss of conjugate
movement of the eyes.
• Compression of III nerve:
Compression of III nerve due to extradural haematoma causes dilatation
of pupil.
Parasympathetic fibres lying superficial get affected first.
Pupil dilates on affected side and there is little response to light.
• Aneurysm/ Periarteritis of posterior cerebral or superior cerebellar
artery, microaneurysm of posterior communicating artery(periarteritis
common in neurosyphilis): compress III nerve as it passes between them
CILIARY GANGLION
• It is a peripheral parasympathetic ganglion
• Topographically it is connected to the nasociliary nerve from
ophthalmic division of the trigeminal
• Functionally it is connected to the oculomotor nerve
• Location:
• It is a minute body (2 mm in diameter)- pin head size, reddish grey in
colour; lying near the apex of orbit between the optic nerve and lateral
rectus muscle.
• It contains multipolar neurons
• Flattened, irregular having 4 angles- anterosuperior, anteroinferior,
posterosuperior and posteroinferior
• Roots: Three roots enter its posterior end- Parasympathetic,
Sympathetic & Sensory
Roots & Distribution of Ciliary Ganglion
Parasympathetic Root: mainly
concerned with focussing
Nerve to Inferior Fibres relay
Edinger Westphal Oblique Muscle
Nucleus Midbrain Postganglionic
Fibres
Preganglionic
Fibres Short Sphincter
Oculomotor Communicating Ciliaris
Nerve Pupillae
Branches Muscle
7%
95%- More
voluminous
Inferior Division muscle
of Oculomotor CILIARY
Nerve GANGLION
Parasympathetic Functions
• There are two structures in the eye that receive parasympathetic
innervation from the oculomotor nerve:
• Sphincter pupillae – constricts the pupil, reducing the amount of light
entering the eye.
• Ciliary muscles – contracts, causes the lens to become more
spherical, and thus more adapted to short range vision.
• The pre-ganglionic parasympathetic fibres travel in the inferior branch
of the oculomotor nerve. Within the orbit, they branch off and
synapse in the ciliary ganglion. The post-ganglionic fibres are carried
to the eye via the short ciliary nerves.
Postganglionic
Sympathetic Root White Ramus Plexus Around Internal Fibres
Communicantes Carotid Artery
Intermediolateral
Nucleus of T1 Stellate Ganglion
segment of Spinal Communicating Ophthalmic
Cord (Lateral horn) twig to 3rd nerve Nerve
in cavernous
Preganglionic Middle Cervical sinus
Fibres Ganglion
Ventral Root of T1 Nasociliary
Nerve to Inferior Nerve
Superior Cervical Oblique
Ganglion
T1 Spinal Nerve Long Ciliary
Nerves
CILIARY GANGLION
Fibres relay
Blood
Ventral Ramus of T1 Short Ciliary Nerve: Blood vessels Vessels
(95%), Dilator Pupillae (5%)
Sensory Root Enter communicating
Main Sensory Nucleus &
Nucleus of Spinal Tract of
ramus of ciliary Trigeminal Nerve
Sensory fibres from
ganglion
eyeball (cornea, iris,
choroid)
2nd Order Neurons
Preganglionic Enter Nasociliary cross to opposite side in
Nerve Trigeminal Lemniscus
Fibres Short Ciliary
Nerves
Reach Ventral
Posteromedial Nucleus
Ophthalmic Nerve
CILIARY GANGLION of Thalamus
Fibres donot relay Trigeminal Nerve 3rd Order Neurons pass
to Post Central Gyrus
Branches:
• The ganglion gives off 8 to 10 short ciliary nerves which divide into 15
to 20 branches
• They contain fibres from all the three roots of the ganglion
• They run above and below the optic nerve towards the eyeball
• On reaching the eyeball they pierce the sclera around the attachment
of the optic nerve and pass forwards in the space between the sclera
and choroid to reach the target organs.
Applied Anatomy:
The ciliary ganglion is blocked to produce dilatation of pupil before
cataract extraction.
You might also like
- BTKV - Cardiac - Carpentier's Reconstructive Valve SurgeryDocument363 pagesBTKV - Cardiac - Carpentier's Reconstructive Valve SurgeryDavid Christian100% (1)
- Oculomotor Nerve: DR / Hytham NafadyDocument52 pagesOculomotor Nerve: DR / Hytham NafadyGetLyricsNo ratings yet
- Oculomotor NerveDocument4 pagesOculomotor NerveHuzaifah IbrahimNo ratings yet
- Optic Nerve: Presented By: Aqsa Irfan Presented To: Dr. Sania ZehraDocument21 pagesOptic Nerve: Presented By: Aqsa Irfan Presented To: Dr. Sania ZehraAqsa100% (1)
- Anatomy of Eyelid: Presenter:-Dr. Vijayalaxmi Moderator:-Dr. SanjanaDocument49 pagesAnatomy of Eyelid: Presenter:-Dr. Vijayalaxmi Moderator:-Dr. SanjanaRidhi Bhandari100% (1)
- What Is AstigmatismDocument2 pagesWhat Is AstigmatismJA QuibzNo ratings yet
- Anatomy and Physiology of Visual PathwayDocument39 pagesAnatomy and Physiology of Visual PathwayAdarsh KeshariNo ratings yet
- Medical Neuroscience Tutorial Notes: Blood Supply To The BrainDocument6 pagesMedical Neuroscience Tutorial Notes: Blood Supply To The BrainsoyyosoloyoNo ratings yet
- Blood Supply of Cerebral CortexDocument3 pagesBlood Supply of Cerebral CortexashrafNo ratings yet
- Clinical Skills Week 1Document3 pagesClinical Skills Week 1Aishah SiddiqahNo ratings yet
- 06 Refractive ErrorDocument12 pages06 Refractive ErrorMwanja MosesNo ratings yet
- Epidural Hematoma Neuro SurgeryDocument2 pagesEpidural Hematoma Neuro SurgeryA Novita Dewi AryantiNo ratings yet
- Optic Nerve (Cranial Nerve Ii) : Abdul Wahab RasyidDocument12 pagesOptic Nerve (Cranial Nerve Ii) : Abdul Wahab RasyidWahab Rasyid100% (1)
- Anatomy of Visual Pathway, Field Defects AND Its Lesions.: By-Dr. Ruchi PherwaniDocument43 pagesAnatomy of Visual Pathway, Field Defects AND Its Lesions.: By-Dr. Ruchi Pherwanisafasayed100% (1)
- The Pupillary Light Reflex PathwayDocument5 pagesThe Pupillary Light Reflex PathwayNauli PanjaitanNo ratings yet
- Pupillary Dilatation ReflexDocument7 pagesPupillary Dilatation ReflexEden Canonizado ChengNo ratings yet
- Excitation of HeartDocument17 pagesExcitation of HeartdevdsantoshNo ratings yet
- Encephalitis Is An Acute Inflammation of The Brain. Encephalitis With Meningitis IsDocument4 pagesEncephalitis Is An Acute Inflammation of The Brain. Encephalitis With Meningitis IsDivya GuptaNo ratings yet
- 3.1 Anatomy and Physiology of The Eye - Nov. 3 - Dr. CastilloDocument13 pages3.1 Anatomy and Physiology of The Eye - Nov. 3 - Dr. CastilloHanako Sasaki AranillaNo ratings yet
- Cranial Nerve Nadz FinalDocument58 pagesCranial Nerve Nadz Finalnadzirah ruslanNo ratings yet
- AdelineDocument34 pagesAdelineEmmanuel NdukaNo ratings yet
- Pupillary Pathways &reactions: Assistant Professor, Department of Ophthalmology Nepalgunj Medical CollegeDocument16 pagesPupillary Pathways &reactions: Assistant Professor, Department of Ophthalmology Nepalgunj Medical CollegeDrBikram ThapaNo ratings yet
- Anatomy of RetinaDocument39 pagesAnatomy of Retinadr_dev100% (1)
- Retina: Zarieh Dawn L. Novela Medicine 2Document50 pagesRetina: Zarieh Dawn L. Novela Medicine 2Zari NovelaNo ratings yet
- Oculomotor Nerve: Arista Prima NDocument7 pagesOculomotor Nerve: Arista Prima NArista Prima N100% (1)
- Diseases of The Optic Nerve 09Document25 pagesDiseases of The Optic Nerve 09somebody_maNo ratings yet
- TF00001028 (Autosaved)Document10 pagesTF00001028 (Autosaved)Cid MusaNo ratings yet
- Neurology: by Dennis Jason Alcantara, RN, USRN, MAN CanDocument213 pagesNeurology: by Dennis Jason Alcantara, RN, USRN, MAN CanKristel-Mia Dimalanta RamosNo ratings yet
- Anatomy of The Uvea: Ruth Antolin, MD Doh Eye CenterDocument75 pagesAnatomy of The Uvea: Ruth Antolin, MD Doh Eye CenterRuth AntolinNo ratings yet
- PBL Modul Blindness KLP 14Document25 pagesPBL Modul Blindness KLP 14033010969No ratings yet
- Auditory SystemDocument2 pagesAuditory SystemLyron GuemoNo ratings yet
- Optic Disc EvaluationDocument45 pagesOptic Disc EvaluationAnurag SrivastavaNo ratings yet
- Pupillary Reflexes: Rohith. A Roll No-66Document34 pagesPupillary Reflexes: Rohith. A Roll No-66Karthikeyan100% (1)
- The Swinging Flashlight Test: Learning Objective: Facts About The PupilDocument3 pagesThe Swinging Flashlight Test: Learning Objective: Facts About The Pupilsiti hazard aldinaNo ratings yet
- Visual SystemDocument37 pagesVisual Systemmalinda100% (1)
- Pupillary PathwayDocument21 pagesPupillary PathwaySurbhi Bharti100% (1)
- NystagmusDocument37 pagesNystagmusMalik AllahbachayaNo ratings yet
- Anatomy Pupillary Pathways AND Abnormal Pupils: Dr. Ravula Hasika M.S.Ophthalmology (1 YR)Document100 pagesAnatomy Pupillary Pathways AND Abnormal Pupils: Dr. Ravula Hasika M.S.Ophthalmology (1 YR)Sonia Afika Aziza100% (1)
- Traktus UveaDocument90 pagesTraktus UveaAudrey Ira Yunita100% (1)
- Cornea-Anatomy and PhysiologyDocument10 pagesCornea-Anatomy and PhysiologyMido KimoNo ratings yet
- Visual ND Pupillary PathwayDocument43 pagesVisual ND Pupillary PathwayAdarsh KeshariNo ratings yet
- Colour Vision AnomaliesDocument27 pagesColour Vision AnomaliesGershon Hayford100% (1)
- Head and Spinal Cord Injury (Ci)Document111 pagesHead and Spinal Cord Injury (Ci)azmerawNo ratings yet
- Dr. Azza ZakiDocument53 pagesDr. Azza ZakiVandana Ravi100% (1)
- Development of EyeDocument21 pagesDevelopment of Eyeklauss starNo ratings yet
- Automated RefractionDocument5 pagesAutomated RefractionCarpetali GatitaNo ratings yet
- Motor TractDocument4 pagesMotor TractRaden Achmad Candra PutraNo ratings yet
- WSD Brochure Update1Document8 pagesWSD Brochure Update1Fabianto SantosoNo ratings yet
- Optic NeuritisDocument32 pagesOptic NeuritisNajaf Ali Khan100% (1)
- LR Vor VSRDocument53 pagesLR Vor VSRAlfira UlfaNo ratings yet
- Physiology of VisionDocument12 pagesPhysiology of VisionAlexis Bondad100% (2)
- Visual PathwayDocument39 pagesVisual Pathwayhuman anatomyNo ratings yet
- Anatomy and Physiology of Optic Nerve.: Dr. Sumit Pandey, MD Lecturer, COMSDocument61 pagesAnatomy and Physiology of Optic Nerve.: Dr. Sumit Pandey, MD Lecturer, COMSNaman Mishra100% (1)
- Vision Photoreceptor MechanismDocument29 pagesVision Photoreceptor MechanismTanishq Hitesh GuptaNo ratings yet
- Anatomy of UveaDocument46 pagesAnatomy of UveaSukhman kaur ButtarNo ratings yet
- Week 4 - Development of The EyeDocument5 pagesWeek 4 - Development of The EyeAleia GoNo ratings yet
- Nystagmus HDocument6 pagesNystagmus HReza AkbarNo ratings yet
- EmbryologyDocument28 pagesEmbryologyKamleshwari RenganathanNo ratings yet
- Review of Anatomy of The EarDocument16 pagesReview of Anatomy of The EarSahrish IqbalNo ratings yet
- Hey, Doc! What’S Wrong with My Eye?: A General Guide to Eye SymptomsFrom EverandHey, Doc! What’S Wrong with My Eye?: A General Guide to Eye SymptomsNo ratings yet
- Cranial NervesDocument61 pagesCranial NervesGuo YageNo ratings yet
- Fatty Acid Synthesis 11.12.19Document18 pagesFatty Acid Synthesis 11.12.19Sanreet Randhawa100% (1)
- Lipid ChemistryDocument93 pagesLipid ChemistrySanreet RandhawaNo ratings yet
- Lipid - Digestion and AbsorptionDocument26 pagesLipid - Digestion and AbsorptionSanreet Randhawa100% (2)
- EnzymesDocument95 pagesEnzymesSanreet RandhawaNo ratings yet
- Anatomy 3.0: Anatomical EmbryologicalDocument49 pagesAnatomy 3.0: Anatomical EmbryologicalShenali SilvaNo ratings yet
- Diagnosa Gagal NafasDocument34 pagesDiagnosa Gagal NafasFariz Auliadi KhalilNo ratings yet
- Cardiovascular Module2Document27 pagesCardiovascular Module2Gracia MayaNo ratings yet
- Jaundice: Signs and SymptomsDocument6 pagesJaundice: Signs and Symptomshero111983No ratings yet
- 1 PredDocument7 pages1 PredandreaNo ratings yet
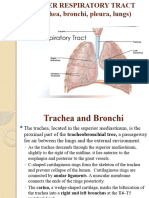
- Lower Resp TractDocument32 pagesLower Resp TractTakshikaNo ratings yet
- Clinical ExaminationsDocument1,596 pagesClinical ExaminationsmdasNo ratings yet
- Pulp LectureDocument71 pagesPulp LectureMohamad TallNo ratings yet
- MCH Urology Dissertation TopicsDocument7 pagesMCH Urology Dissertation TopicsBuyAPaperOnlineBaltimore100% (1)
- Obat NefrotoksikDocument5 pagesObat NefrotoksikIndah Nur LathifahNo ratings yet
- Congenital Heart Diseases: Non Cyanotic PlethoraDocument43 pagesCongenital Heart Diseases: Non Cyanotic PlethoraFauzi SatriaNo ratings yet
- C2 ExamDocument29 pagesC2 ExamauNo ratings yet
- What Is EcgDocument5 pagesWhat Is EcgLeeyan MeeNo ratings yet
- Transport of Substances in Humans (LQ)Document13 pagesTransport of Substances in Humans (LQ)Wan Ching ChanNo ratings yet
- PDF Quick Reference Guide To Pediatric Care 2Nd Edition Deepak M Kamat Ebook Full ChapterDocument53 pagesPDF Quick Reference Guide To Pediatric Care 2Nd Edition Deepak M Kamat Ebook Full Chapterlarry.bagwell682100% (3)
- Gastrointestinal DisordersDocument4 pagesGastrointestinal DisordersJerica Mae VenoyaNo ratings yet
- CVS ExamDocument35 pagesCVS Examtravis efraimNo ratings yet
- MCQ - Cardiovasuclar SystemDocument3 pagesMCQ - Cardiovasuclar SystemAmacus NirvanaNo ratings yet
- LABORATORY EXERCISE The Gastrointestinal System With Accessory GlandDocument5 pagesLABORATORY EXERCISE The Gastrointestinal System With Accessory GlandGelo AlonzoNo ratings yet
- Deep Vein Thrombosis Oet Reading Task SampleDocument6 pagesDeep Vein Thrombosis Oet Reading Task SampleKrischen CaiseNo ratings yet
- Buerger Allen Exercise To Improve Peripheral Vascular CirculationDocument4 pagesBuerger Allen Exercise To Improve Peripheral Vascular CirculationArun KumarNo ratings yet
- NatokinaseDocument6 pagesNatokinasefabadioNo ratings yet
- Hypertension in Geriatrics 2010Document51 pagesHypertension in Geriatrics 2010Andre HawkNo ratings yet
- Sledai-2K: Data Collection Sheet: Total ScoreDocument1 pageSledai-2K: Data Collection Sheet: Total ScoreSuryadi Limardi0% (1)
- Quality of Life of Patients Who Have Undergone Percutaneous Transluminal Coronary Angioplasty (PTCA) and Coronary Artery Bypass Graft (CABG) in A Selected Hospital, KottayamDocument3 pagesQuality of Life of Patients Who Have Undergone Percutaneous Transluminal Coronary Angioplasty (PTCA) and Coronary Artery Bypass Graft (CABG) in A Selected Hospital, KottayamInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- DVT NotesDocument3 pagesDVT NotesTodd EvansNo ratings yet
- Pericardial Effusion and Cardiac TamponadeDocument18 pagesPericardial Effusion and Cardiac TamponadeSiti Hamidah Abd Aziz100% (1)
- Head To Toe Checklist (Masroni)Document13 pagesHead To Toe Checklist (Masroni)hillary elsaNo ratings yet
- Chap22 PDFDocument9 pagesChap22 PDFSam CryshnaNo ratings yet