Professional Documents
Culture Documents
HPAxis 3rd (Autosaved)
HPAxis 3rd (Autosaved)
Uploaded by
Jess Peltra0 ratings0% found this document useful (0 votes)
8 views29 pagesOriginal Title
HPAxis 3rd [Autosaved]
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
8 views29 pagesHPAxis 3rd (Autosaved)
HPAxis 3rd (Autosaved)
Uploaded by
Jess PeltraCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 29
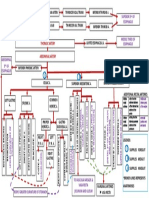
Hypothalamic Pituitary Axis
Gerardo Carmelo B. Salazar, MD
3rd Year LPUSC School of Health Sciences
Copyrights apply
Copyrights apply
Copyrights apply
HPAxis
• A complex set of direct influences and
feedback interactions among three
components: the hypothalamus, the
pituitary gland and the effector glands
Copyrights apply
Raised Intracranial Pressure
MJ 15 Male
• CC: headaches
• Noticed to be gaining weight at age 14 yrs old with occasional fatigue and cold intolerance
• Dull, continuous headaches of 4/5 relieved with paracetamol. Headaches are worse on lying
down and on turning to sides.
• Upon getting out of bed, had feeling of blacking out. He is also noticed to be moving his tablet
horizontally when reading.
• He claims to be urinating frequently
• Because of the progressive headaches becoming 7-8/10 the past week with episodes of vomiting.
Complete the above case
• Is there a neurologic problem?
• If yes, what level is the neurologic problem?
• Localize
• What is the temporal profile?
• Etiologic DDX
Differentials
• Pituitary Gland Tumor ( Macroadenoma)
• Brainstem glioma/tumor
• Giant carotid aneurysm
• Cavernous sinus syndrome
• Migraine
Work up
• IMAGING
• Brain MRI with and without contrast is the gold standard.
• ENDOCRINE EVALUATION
• Baseline serum electrolytes, serum and urine osmolality, thyroid studies, morning and evening cortisol levels, growth
hormone levels, and luteinizing and follicle-stimulating hormone levels, in pediatric as well as adult patients.
• In emergent cases, hormonal testing should be limited to diagnosing diabetes insipidus, hypoadrenalism, and
hypothyroidism, as these hormones require the initiation of treatment prior to surgery.
• HISTOLOGIC
• Three main types: adamantinomas, papillary craniopharyngiomas, and mixed tumors.
• The MIB-1 labeling index is a measure of the disease’s proliferative activity. It is determined by using an
immunohistochemical method with monoclonal antibody MIB-1 and may be useful for the planning of adjuvant
therapy. One study reported that an MIB-1 labeling index of greater than 7% predicted regrowth/recurrence.
Diabetes Insipidus
versus SIADH
T1 Weighted Images
Adamantinomatous
craniopharyngioma
Papillary
craniopharyngiomas
Craniopharyngioma
• Slow-growing, extra-axial, epithelial-squamous, calcified, and cystic tumor arising from
remnants of the craniopharyngeal duct and/or Rathke cleft and occupying the
sellar/suprasellar region
Craniopharyngioma
• Rare malformational tumours of low histological malignancy arising along the craniopharyngeal duct.
• Benign but locally invasive tumours of the sellar region that arise from ectopic embryonic remnants of Rathke's pouch,
• The two histological subtypes, adamantinomatous craniopharyngioma (ACP) and papillary craniopharyngioma (PCP),
differ in genesis and age distribution.
• ACPs are diagnosed with a bimodal peak of incidence (5–15 years and 45–60 years), whereas PCPs are restricted to
adults mainly in the fifth and sixth decades of life.
• ACPs are driven by somatic mutations in CTNNB1 (encoding β-catenin) that affect β-catenin stability and are
predominantly cystic in appearance.
• PCPs frequently harbour somatic BRAFV600E mutations and are typically solid tumours.
• Clinical manifestations due to increased intracranial pressure, visual impairment and endocrine deficiencies should
prompt imaging investigations, preferentially MRI.
Craniopharyngioma
• Most frequently arise in the pituitary stalk and project into the hypothalamus. They extend horizontally
along the path of least resistance in various directions, as follows:
• Anteriorly - Into the prechiasmatic cistern and subfrontal spaces
• Posteriorly - Into the prepontine and interpeduncular cisterns, cerebellopontine angle, third ventricle, [3] posterior
fossa, and foramen magnum
• Laterally - Toward the subtemporal spaces
• Clinical behavior and the choice of surgical approach are dictated by the primary location of the tumor
and its extension pattern.
• Prechiasmatic craniopharyngiomas (extending into the subfrontal spaces)
• Retrochiasmatic craniopharyngiomas (expanding into the posterior fossa) may become large before being diagnosed.
Treatment Approach
1. attempt a gross total resection
2. perform a planned subtotal resection followed by radiotherapy or some other adjuvant therapy.
Successful management is determined by the ability to preserve independent social functioning,
prevent symptomatic recurrence, and increase survival rate.
There has been significant debate in recent years regarding the outcomes of GTR (Gross total removal)
in the pediatric population given the high risk for hypothalamic injury and deficits, which can be life-
altering in children (i.e., extreme obesity, deterioration in educational abilities).
Prognosis
• Neuropsychological deficits represent the major limiting factor for independent social
functioning because
• (1) patients often can overcome minor neurologic deficits and
• (2) hormone replacement therapies are widely available.
• The degree of psychosocial impairment correlates directly with the degree of hypothalamic
injury sustained at the time of surgery.
• Atypical antidepressants. These medications don't fit neatly into any
of the other antidepressant categories. More commonly prescribed
antidepressants in this category include trazodone, mirtazapine
(Remeron), vortioxetine (Trintellix), vilazodone (Viibryd) and
bupropion (Wellbutrin SR, Wellbutrin XL, others). Bupropion is one
(antidepressants) of the few antidepressants not frequently associated with sexual side
effects.
• Tricyclic antidepressants. Tricyclic antidepressants — such as
• Selective serotonin reuptake inhibitors (SSRIs). imipramine (Tofranil), nortriptyline (Pamelor), amitriptyline, doxepin
Doctors often start by prescribing an SSRI. These and desipramine (Norpramin) — tend to cause more side effects than
medications generally cause fewer bothersome side newer antidepressants. So tricyclic antidepressants generally aren't
effects and are less likely to cause problems at higher prescribed unless you've tried other antidepressants first without
therapeutic doses than other types of antidepressants improvement.
are. SSRIs include fluoxetine (Prozac), paroxetine • Monoamine oxidase inhibitors (MAOIs). MAOIs — such as
(Paxil, Pexeva), sertraline (Zoloft), citalopram tranylcypromine (Parnate), phenelzine (Nardil) and isocarboxazid
(Celexa) and escitalopram (Lexapro). (Marplan) — may be prescribed, often when other medications haven't
• Serotonin and norepinephrine reuptake worked, because they can have serious side effects. Using an MAOI
requires a strict diet because of dangerous (or even deadly)
inhibitors (SNRIs). Examples of SNRI medications
interactions with foods — such as certain cheeses, pickles and wines
include duloxetine (Cymbalta), venlafaxine (Effexor
— and some medications, including pain medications, decongestants
XR), desvenlafaxine (Pristiq) and levomilnacipran
and certain herbal supplements. Selegiline (Emsam), an MAOI that
(Fetzima).
you stick on your skin as a patch, may cause fewer side effects than
other MAOIs. These medications can't be combined with SSRIs.
(anxiolytics)
• Benzodiazepines
• Ca channel inhibitors
• Antihistamine
You might also like
- Nsg2hpb Exam PDFDocument23 pagesNsg2hpb Exam PDFCourtney B100% (1)
- Davao Doctors College General Malvar Street, Davao City Nursing ProgramDocument5 pagesDavao Doctors College General Malvar Street, Davao City Nursing ProgramJhoneric Vencer EscultorNo ratings yet
- Цветн - атлас Биопсий НерваDocument272 pagesЦветн - атлас Биопсий НерваBertramVrelling100% (1)
- Rutger's PANRE and PANCE Practice Questions 1 of 2Document35 pagesRutger's PANRE and PANCE Practice Questions 1 of 2nubianlocks100% (3)
- MycologyDocument129 pagesMycologyPriyanka Rajput100% (4)
- Mental Health and Psychiatric Nursing: Vernalin B. Terrado, RNDocument35 pagesMental Health and Psychiatric Nursing: Vernalin B. Terrado, RNverna100% (1)
- A Guide To Psychotropic DrugsDocument16 pagesA Guide To Psychotropic DrugsNokz M. Raki-inNo ratings yet
- Antidepressants ChristianDocument37 pagesAntidepressants ChristianciaranNo ratings yet
- Medical Student Psychopharmacology - PPTX 2015-16 John WDocument99 pagesMedical Student Psychopharmacology - PPTX 2015-16 John WMrLarry DolorNo ratings yet
- Psychopharmacology in Psychopharmacology in Psychiatry PsychiatryDocument16 pagesPsychopharmacology in Psychopharmacology in Psychiatry PsychiatryHasnain HyderNo ratings yet
- Psychopharmacology Presentation1Document25 pagesPsychopharmacology Presentation1Juliax ClintonNo ratings yet
- Antidepressants DESKTOP MHAO1SHDocument19 pagesAntidepressants DESKTOP MHAO1SHjanemwanza003No ratings yet
- Commonly Used Medication For Older AdultsDocument3 pagesCommonly Used Medication For Older AdultsRaze AlemaniaNo ratings yet
- Antidepressants PrintedDocument3 pagesAntidepressants PrintedRahul Kumar DiwakarNo ratings yet
- Not Associated With Significant Weight GainDocument9 pagesNot Associated With Significant Weight GainDima MasadehNo ratings yet
- Drugs For Anxiety and InsomniaDocument10 pagesDrugs For Anxiety and InsomniaApple MaeNo ratings yet
- Bimbel Ukmppd FarmakoDocument92 pagesBimbel Ukmppd FarmakoJavier AntaresNo ratings yet
- Tai Lieu U Khoa Mien Pho Cho Nguoi MoiDocument17 pagesTai Lieu U Khoa Mien Pho Cho Nguoi MoiDT PVNo ratings yet
- PsychopharmacologyDocument77 pagesPsychopharmacologychachaazkaNo ratings yet
- LECTURE 9 AnxietyDocument25 pagesLECTURE 9 AnxietyreemqnsuaNo ratings yet
- Psychotropic Drugs: By: Rheajane Aguilar-RosalesDocument77 pagesPsychotropic Drugs: By: Rheajane Aguilar-Rosalesjean samson100% (1)
- Trifluridine and TipiracilDocument3 pagesTrifluridine and TipiracilKristine AcasioNo ratings yet
- Antiadrenergic-Hypotension Antimuscarinic (Anticholinergic) - Dry Mouth, BlurredDocument8 pagesAntiadrenergic-Hypotension Antimuscarinic (Anticholinergic) - Dry Mouth, Blurredwafaa alwafiNo ratings yet
- Medical Student Psychopharmacology - PPTX 2015-16 John WDocument98 pagesMedical Student Psychopharmacology - PPTX 2015-16 John WDr TNTNo ratings yet
- Psychotropic DrugsDocument81 pagesPsychotropic DrugsJoan100% (2)
- Antidepressant DrugsDocument55 pagesAntidepressant Drugsmaheen aurangzaib100% (2)
- Antidepressant DrugsDocument47 pagesAntidepressant DrugsOjambo Flavia75% (4)
- PsychopharmacologyDocument32 pagesPsychopharmacologyCms CSU100% (1)
- Antidepressants AntianxietyDocument95 pagesAntidepressants AntianxietyCharles YiuNo ratings yet
- Farmakovigilans: Ni Made Amelia Ratnata Dewi, M.Farm - Klin., AptDocument41 pagesFarmakovigilans: Ni Made Amelia Ratnata Dewi, M.Farm - Klin., AptUpuUt Putrhie MinchuuetNo ratings yet
- Anti Depresan1Document39 pagesAnti Depresan1Akmal SafwanNo ratings yet
- Interaksi Obat Dan HerbalDocument23 pagesInteraksi Obat Dan HerbalEka Puji LestariNo ratings yet
- An Tide Prees AntDocument38 pagesAn Tide Prees Antnamah odatNo ratings yet
- AntidepressantsDocument4 pagesAntidepressantsGrace CabilloNo ratings yet
- Drug Classification: Generic and Brand Name of The DrugsDocument6 pagesDrug Classification: Generic and Brand Name of The DrugsFlora May LuzadasNo ratings yet
- Antidepressants (Igor Iezhitsa) Students Copy (ME219)Document40 pagesAntidepressants (Igor Iezhitsa) Students Copy (ME219)Zobayer AhmedNo ratings yet
- Gastrointestinal Drugs: By: Ma. Jennifer E. Benida-RN, MSNDocument49 pagesGastrointestinal Drugs: By: Ma. Jennifer E. Benida-RN, MSNSidney Bon LuceroNo ratings yet
- Psychopharma 1Document7 pagesPsychopharma 1Mitchee Zialcita100% (1)
- Anti Anxiety DrugsDocument15 pagesAnti Anxiety DrugsMr. Psycho Sam100% (1)
- AntidepressantsDocument9 pagesAntidepressantsGabriel KidagayoNo ratings yet
- Drug StudyDocument4 pagesDrug StudyDean Angelo BarrientosNo ratings yet
- Anti-Depressants: Bitek BrianDocument28 pagesAnti-Depressants: Bitek BrianMwanja MosesNo ratings yet
- Antiemetics: Prof. Dr. Fatima Rizvi Department of PharmacologyDocument44 pagesAntiemetics: Prof. Dr. Fatima Rizvi Department of PharmacologydrfatimarizNo ratings yet
- Gastrointestinal DrugsDocument49 pagesGastrointestinal DrugsMae Antonette OrlinaNo ratings yet
- Antispastics Emtyaz FDocument57 pagesAntispastics Emtyaz FMuhammed MuhsinNo ratings yet
- Extrapyramidal Symptom AssessmentDocument6 pagesExtrapyramidal Symptom AssessmentJNo ratings yet
- Antipsychotics Risks and BenefitsDocument38 pagesAntipsychotics Risks and BenefitsElleNo ratings yet
- PsychopharmacologyDocument50 pagesPsychopharmacologyapi-3703352No ratings yet
- Overview of Psychotropic DrugsDocument7 pagesOverview of Psychotropic Drugsnad101No ratings yet
- Nausea Movement DisorderDocument5 pagesNausea Movement DisorderoladapoNo ratings yet
- Beers List 350301Document22 pagesBeers List 350301Christine WaspNo ratings yet
- Lorazepam and FlumazenilDocument16 pagesLorazepam and FlumazenilACanNo ratings yet
- Drugs Used in Psychiatric HospitalDocument28 pagesDrugs Used in Psychiatric Hospitalmercygreat2014No ratings yet
- Anxiolytic and Hypnotic AgentsDocument50 pagesAnxiolytic and Hypnotic AgentsMoxie Macado100% (1)
- Antidepressent (AutoRecovered)Document11 pagesAntidepressent (AutoRecovered)chakdiva11No ratings yet
- Sedation, Analgesia & Patient Controlled Analgesia 2Document28 pagesSedation, Analgesia & Patient Controlled Analgesia 2Arshad SyahaliNo ratings yet
- Antidepressants AntidepressantsDocument38 pagesAntidepressants AntidepressantsjaneNo ratings yet
- Pharmacology PremedicationDocument12 pagesPharmacology PremedicationspringshemantNo ratings yet
- ANXIOLYTICSDocument33 pagesANXIOLYTICSCletus MichaelNo ratings yet
- Depression Primary Care Part2Document4 pagesDepression Primary Care Part2Shazwani KKTSNo ratings yet
- Pharmacologic Management of Adult Depression: Stephen M. Adams, MD Karl E. Miller, MD and Robert G. Zylstra, Edd, LCSWDocument8 pagesPharmacologic Management of Adult Depression: Stephen M. Adams, MD Karl E. Miller, MD and Robert G. Zylstra, Edd, LCSWruth_villagraNo ratings yet
- Pharmacotherapy For Insomnia in Adults - UpToDateDocument57 pagesPharmacotherapy For Insomnia in Adults - UpToDateEduardo AguilarNo ratings yet
- Question Viva Pharmacology 2021Document6 pagesQuestion Viva Pharmacology 2021Parketic GamerNo ratings yet
- Fibromyalgia: Medications and Alternative Fibromyalgia Treatments: The most important information you need to improve your healthFrom EverandFibromyalgia: Medications and Alternative Fibromyalgia Treatments: The most important information you need to improve your healthRating: 2 out of 5 stars2/5 (1)
- Net Notes CardioDocument9 pagesNet Notes CardioJess PeltraNo ratings yet
- Net Notes AuditoryDocument8 pagesNet Notes AuditoryJess PeltraNo ratings yet
- COVID-19 Life EventsDocument30 pagesCOVID-19 Life EventsJess PeltraNo ratings yet
- Case For SGD GI 12072021Document1 pageCase For SGD GI 12072021Jess PeltraNo ratings yet
- Blood FlowDocument1 pageBlood FlowJess PeltraNo ratings yet
- PharmaDocument14 pagesPharmaJess PeltraNo ratings yet
- Complications Associated With Surgical Treatment of Congenital Intrinsic Duodenal ObstructionDocument4 pagesComplications Associated With Surgical Treatment of Congenital Intrinsic Duodenal ObstructionJess PeltraNo ratings yet
- CPG Early and Locally Advanced Non-Small-Cell LungDocument6 pagesCPG Early and Locally Advanced Non-Small-Cell LungJess PeltraNo ratings yet
- Lateral Region Simplified For TransDocument4 pagesLateral Region Simplified For TransJess PeltraNo ratings yet
- Chapter 9 - The Brainstem and Cranial NervesDocument8 pagesChapter 9 - The Brainstem and Cranial NervesJess PeltraNo ratings yet
- Surgery of The SkinDocument66 pagesSurgery of The SkinJess PeltraNo ratings yet
- 9.2.2 The Fetal Patient - Fetal Assessment - April 05 - Dra. MeerDocument3 pages9.2.2 The Fetal Patient - Fetal Assessment - April 05 - Dra. MeerJess PeltraNo ratings yet
- Cubital Tunnel SyndromeDocument18 pagesCubital Tunnel SyndromeJess PeltraNo ratings yet
- Y3 Immunologic DsesDocument65 pagesY3 Immunologic DsesJess PeltraNo ratings yet
- Burch Wartofsky 1993 Thyroid Storm Endocrinol Metab Clin North AmDocument15 pagesBurch Wartofsky 1993 Thyroid Storm Endocrinol Metab Clin North AmJess PeltraNo ratings yet
- Histology: Male Reproductive SystemDocument24 pagesHistology: Male Reproductive SystemJess PeltraNo ratings yet
- Malignant Skin Disorders-HandoutDocument5 pagesMalignant Skin Disorders-HandoutJess PeltraNo ratings yet
- 8.2 Inguinal Hernias, PUV, and VUR - March 14 - Dr. Gellido & Dr. LawenkoDocument8 pages8.2 Inguinal Hernias, PUV, and VUR - March 14 - Dr. Gellido & Dr. LawenkoJess PeltraNo ratings yet
- 1650607611411302Document53 pages1650607611411302Jess PeltraNo ratings yet
- 8.3 Acute Kidney Injury - March 16 - Dr. Austria.Document6 pages8.3 Acute Kidney Injury - March 16 - Dr. Austria.Jess PeltraNo ratings yet
- Know The Word Questions1Document3 pagesKnow The Word Questions1Jess PeltraNo ratings yet
- Pregnancy Complication - HypertensionDocument37 pagesPregnancy Complication - HypertensionJess PeltraNo ratings yet
- 8.4 Chronic Kidney Disease - March 17 - Dra. BasilanDocument9 pages8.4 Chronic Kidney Disease - March 17 - Dra. BasilanJess PeltraNo ratings yet
- Img 20180605 0004Document2 pagesImg 20180605 0004Jess PeltraNo ratings yet
- Eye Physiology For TransDocument5 pagesEye Physiology For TransJess PeltraNo ratings yet
- Phonetic Sounds and SymbolsDocument11 pagesPhonetic Sounds and SymbolsJess PeltraNo ratings yet
- Direction: Underline The Modal That Best Completes The SentenceDocument1 pageDirection: Underline The Modal That Best Completes The SentenceJess PeltraNo ratings yet
- Edukasyon Sa Pagpapakatao Curriculum Guide Grade 1-10Document3 pagesEdukasyon Sa Pagpapakatao Curriculum Guide Grade 1-10Jess PeltraNo ratings yet
- Future ProgressiveDocument2 pagesFuture ProgressiveJess PeltraNo ratings yet
- Program Commencement 2014Document21 pagesProgram Commencement 2014Jess PeltraNo ratings yet
- Cutaneous and Superficial Abscesses: Key Practice PointsDocument10 pagesCutaneous and Superficial Abscesses: Key Practice PointsFofiuNo ratings yet
- Alali - Yasser - 202011 - MSC - ThesisDocument104 pagesAlali - Yasser - 202011 - MSC - Thesistanay tripathiNo ratings yet
- RBC, PCV, ESR, Blood IndicesDocument5 pagesRBC, PCV, ESR, Blood IndicesUjjwal Kumar MauryaNo ratings yet
- RockerDocument2 pagesRockerwan hseNo ratings yet
- Skin Lessions Covid-19Document15 pagesSkin Lessions Covid-19JUAN PABLO DE JESUS CASTRO MORANo ratings yet
- Tetraogy of FallotDocument9 pagesTetraogy of FallotMary Louise MadariagaNo ratings yet
- Degenerasi Hialin Pada: Pyelonefritis KronikDocument16 pagesDegenerasi Hialin Pada: Pyelonefritis KronikNininghrNo ratings yet
- Deep Vein ThrombosisDocument5 pagesDeep Vein ThrombosisnikaaraaaNo ratings yet
- Autism: DefinitionDocument6 pagesAutism: DefinitionBallave SudiptaNo ratings yet
- Assessment Diagnosis Scientific Explanation Planning Interventions Rationale Expected Outcome Subjective: O Short Term: Short TermDocument3 pagesAssessment Diagnosis Scientific Explanation Planning Interventions Rationale Expected Outcome Subjective: O Short Term: Short TermRaidis PangilinanNo ratings yet
- Chronic Renal FailureDocument29 pagesChronic Renal Failuregeorgia.langNo ratings yet
- Neuro Form 4 By: Sergio AnguloDocument7 pagesNeuro Form 4 By: Sergio AnguloJohnny AppleseedNo ratings yet
- AldDocument17 pagesAldMuli MaroshiNo ratings yet
- Oral Cancer Awareness Among Non-Medical Professionals - A Cross Sectional Study in LadakhDocument8 pagesOral Cancer Awareness Among Non-Medical Professionals - A Cross Sectional Study in LadakhIJAR JOURNALNo ratings yet
- Nightmares and Night Terrors: What Is A Nightmare? What To Do?Document2 pagesNightmares and Night Terrors: What Is A Nightmare? What To Do?Ambreen “khuwazhey”No ratings yet
- Hornick Carcinoma of Unknown Primary 8 June 1400Document87 pagesHornick Carcinoma of Unknown Primary 8 June 1400Olteanu Dragos-NicolaeNo ratings yet
- Pediatric Cholestasis: Epidemiology, Genetics, Diagnosis, and Current ManagementDocument5 pagesPediatric Cholestasis: Epidemiology, Genetics, Diagnosis, and Current ManagementAnnisa SusiloNo ratings yet
- 12 - Epstein Barr Virus (EBV)Document20 pages12 - Epstein Barr Virus (EBV)Lusiana T. Sipil UnsulbarNo ratings yet
- GingivitisDocument30 pagesGingivitisSharon DingNo ratings yet
- A Guide To Common Blood TestsDocument3 pagesA Guide To Common Blood TestsshahjituNo ratings yet
- DIETDocument4 pagesDIETPrabu G SatiyaNo ratings yet
- Contoh Sbar 3Document2 pagesContoh Sbar 3ria saraswatiNo ratings yet
- All About Pito-Pito LeavesDocument6 pagesAll About Pito-Pito LeavesDerrick Yson (Mangga Han)100% (1)
- Genetic Role of UBASH3A in Autoimmune Disease in Down SyndromeDocument23 pagesGenetic Role of UBASH3A in Autoimmune Disease in Down SyndromeGlobalDownSyndrome100% (1)
- PSPv2022 01 19Document31 pagesPSPv2022 01 19Bernard Jayve PalmeraNo ratings yet
- Asa Physical Status Classification SystemDocument2 pagesAsa Physical Status Classification SystemWanditoGayuhUtomoNo ratings yet