Professional Documents
Culture Documents
Brucellosis
Brucellosis
Uploaded by
abel semu0 ratings0% found this document useful (0 votes)
3 views36 pagesThis document provides an overview of brucellosis. It discusses the epidemiology, microbiology, transmission, pathogenesis, clinical presentation, diagnosis, treatment, and prognosis of brucellosis. Brucellosis is caused by bacteria of the genus Brucella and is a zoonotic disease transmitted from animals to humans. It causes nonspecific flu-like symptoms and can infect any organ system. Diagnosis involves considering exposure risk factors and clinical presentation along with serological testing and culture. Treatment consists of prolonged antibiotic therapy.
Original Description:
Original Title
Brucellosis.pptx
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides an overview of brucellosis. It discusses the epidemiology, microbiology, transmission, pathogenesis, clinical presentation, diagnosis, treatment, and prognosis of brucellosis. Brucellosis is caused by bacteria of the genus Brucella and is a zoonotic disease transmitted from animals to humans. It causes nonspecific flu-like symptoms and can infect any organ system. Diagnosis involves considering exposure risk factors and clinical presentation along with serological testing and culture. Treatment consists of prolonged antibiotic therapy.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
3 views36 pagesBrucellosis
Brucellosis
Uploaded by
abel semuThis document provides an overview of brucellosis. It discusses the epidemiology, microbiology, transmission, pathogenesis, clinical presentation, diagnosis, treatment, and prognosis of brucellosis. Brucellosis is caused by bacteria of the genus Brucella and is a zoonotic disease transmitted from animals to humans. It causes nonspecific flu-like symptoms and can infect any organ system. Diagnosis involves considering exposure risk factors and clinical presentation along with serological testing and culture. Treatment consists of prolonged antibiotic therapy.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 36
Brucellosis
By: Dr. Hawine Bekele
Objective
At the end of this lecture students should be
able to:
• know the epidemiology, microbiology,
pathogenesis of brucella infection
• Understand the transmission mode and
treatment of the infection
• be aware about the prevention methods
Outline
• Introduction
• Epidemiology
• Microbiology
• Transmission
• Pathogenesis
• Clinical presentation
• DDX
• Diagnosis
• Treatment
• Prognosis
Introduction
• Brucellosis is a bacterial zoonotic infection
caused by the bacterial genus Brucella.
• It is transmitted to humans by contact with fluids
from infected animals (sheep, cattle, goats, pigs,
or other animals) or derived food products such
as unpasteurized milk and cheese.
• the disease is an old one that has been known
by various names, including meditranian fever,
Malta fever, gastric remittent fever.
• Humans are accidental hosts, but brucellosis
continues to be a major public health concern
world wide and is the most common zoonotic
infection.
• The global burden of human brucellosis
remains enormous: the infection cause more
than 500,000 infections per year world wide.
• Brucellosis has high morbidity both for humans
and animals; it is an important cause of
economic loss and public health problems in
many developing countries.
• The prevalence of brucellosis has been
increasing due to growing international tourism
and migration in addition to the potential use of
brucella as a biologic weapon.
• The organisms which are small aerobic
intracellular cocobacilli localize in the
reproductive organs of host animals, causing
abortions and sterility.
• They are shed in large numbers in the animal’s
urine, milk, placental fluid and other fluids.
• To date, 8 species have been identified, named
primarily for the source animal or features of
infection.
• Of these, the following 4 have moderate to
significant human pathogencity: Brucella
melitensis, Brucella suis, Brucella abortus and
Brucella canis.
• Familiarity with the manifestations of
brucellosis and knowledge of the optimal
laboratory studies are essential for the
recognition of this re-emerging zoonosis.
Epidemiology
• Brucellosis causes more than 500,000 infections per
year worldwide.
• Its geographic distribution is limited by effective
public and animal health programs, and the
prevalence of the disease varies widely from country
to country.
• Overall, the frequency of brucellosis is higher in
more agrarian societies and in places where handling
of animal products and diary products is less
stringent.
• The heaviest disease burden lies in countries
of the Mediterranean basin and Arabian
peninsula, and is also common in India,
Mexico, south and central America.
• Because of variable reporting, true estimates
in endemic areas are unknown. Incidence
rates of 1.2-70 cases per 100,000 people are
reported.
• In very resource poor countries ( such as some
African countries) in which brucellosis is
endemic, control through animal slaughter is a
poor option because of the fragile nature of
the food supply.
• Brucellosis in the meditrranaian chiefly due to
B.melitensis has the highest age/sex related
incidence in males in their mid 20s.
• For unknown reasons, men aged 13-40 years
are particularly vulnerable to the
manifestations of illness due to B. Melitensis.
• Brucellosis is generally uncommon in infants.
The international literatures suggests that
brucellosis may be more common in children
in developing countries because of lack of
pasteurization and working in an agrarian
society.
• Worldwide, brucellosis is more common in
males than in females. Young adult males
predominate in most series of patients with
brucellosis compiled in areas of endemic
disease.
• A report from northern Saudi Arabia found the
male to female ratio 1.7: 1 chiefly individuals
aged 13-40 years.
• No racial predilection is found.
Pathophysiology
• Brucellae are aerobic gram- negative
cocobacilli that posses a unique ability to
invade both phagosyitic and nonphagocytic
cells and to survive in the intracellular
environment by finding ways to avoid the
immune system.
• It is a systemic illness and can involve almost
every organ system.
• Brucella can gain entry into the human body through
breaks in the skin mucous membranes, conjunctivae,
respiratory and GI tracts.
• Ingestion usually occur by way of unpasteurized milk
and meat products.
• Once within the blood stream , the organism quickly
become intracellular pathogens contained within
circulating PMN and macrophages making use of
numerous mechanisms to avoid or suppress
bactericidal responses.
• After ingestion by phagocytes, about 15-30%
of brucellae survive. Susuptability to
intracellular killing differs among specieces,
with B.abortus being radily killed and B.
Melitenesis rarely affected.
• Brucellae that survive are transported into the
lymphatic system and may replicate in the
kidney, spleen, liver, breast tissue or joints
causing both localized and systemic infection
• Any organ system can be involved (CNS, heart,
GUS, Pulmonary system, skin)
• Localization of the process may cause focal
symptoms or findings.
• After replication in the endoplastic reticulum ,
the brucellae are released with the help of
hemolysins and induce cell necrosis.
Microbiology
Small
Non-motile
Facultative intracellular aerobic rods
0.5-0.7 micron in diameter
0.6-1.5 micron in length
Gram negative coco bacilli
lacks capsule, spores and flagella
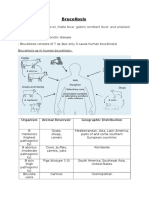
Ethiology
• Brucellosis is caused by infection with brucella
species. The traditional classification of these
species is based primarily based on the
preferred hosts.
Organism Animal reservoir Geographic distribution
Brucella Melitenisis Goats, sheep, camels Mediterranean, Asia,
Latin America, parts of
Africa and some southern
European countries
Brucella Abortus Cows, buffalo, camels, Worldwide
yaks
Brucella suis Pigs (biotype 1-3) South America, Southeast
Asia, USA
Brucella Canis Canines Cosmopolitan
Brucella ovis Sheep No known human case
Brucella neotomae Rodents No known human case
Brucella pinnipediae and Marine animals, dolphins, Human reports with
brucella cetaceae seals neurobrucellosis
• Of the 4 brucella species known to cause
disease in humans B.melitenisis is thought to
the most virulent and causes the most sever
and acute cases of brucellosis, it also the most
prevalent worldwide.
• B. Abortus is more widely distributed
thorough out the world but is less pathogenic
for both humans and animals.
• Slaughterhouse workers, primarily those in the
kill area become inoculated with brucellae
through aerozolization of fluids, contamination
of skin abrasions and splashing of mucus
membrane. Farmers and shepherds have
similar risk.
• Veteranians are usually infected by inadvertent
inoculation of animal vaccine against B.
Melitenisis and B.abortus
Clinical presentation
• A careful history is most helpful tool in the
diagnosis of brucellosis, since every case of
brucellosis involves exposure to an affected animal
either directly or indirectly.
• Fever is the most common symptom and sign of
brucellosis occurring in 80-100% of cases.
• Fever can be associated with a relative bradycardia
• FUO is a common initial diagnosis in patients with
low endemicity
• Constitutional symptoms of brucellosis include
anorexia, asthenia, fatigue, weakness, malaise
and weight loss are very common (>90%)
• Bone and joint symptoms include arthalgias,
low back pain, spine and joint pain and rarely
joint swelling
• Neuropsychiatric symptoms of brucellosis are
common despite the rare involvement of the
CNS.
• Headache, depression and fatigue are the frequently
reported symptoms.
• 50% of patients have GI complaints primarily dyspepsia.
• Genitourinary infections 2ndry to brucellosis include
orchitis, UTI and glomerulonephritis
• Neurologic symptoms include weakness, dizziness, gait
disturbance
• Cough and dyspnea develop in up to 19% of patients
• Endocarditis is also reported
• The incubation period ranges from one to four
weeks.
• Acute illness usually consists of the insidious
onset of fever, night sweats, atralgia, myalgia,
low back pain, weight loss, fatigue, malaise,
headache and diziness
• Physical findings are variable and non specific
may include hepatosplenomegally and/or
lymphadenopathy
• Localized infection: focal infection occur in about
30% of the cases
• Brucellosis can affect any organ system
• Chronic brucellosis refers to patients with clinical
manifestations for more than one year after the
diagnosis of brucellosis is established
• it is carachterized by localized infection and/or
relapse in patients with objective evidence of
infection
• Physical examination findings:
Complications
Osteo articular
Hepatobiliary and GI
Genetourinary
Cardiovascular
Pulmonary
Hematolgic
Diagnosis
• For the diagnosis of brucellosis the laboratory
finding together with the exposure history,
clinical manifestation, occupation is important.
• Laboratory tools for the diagnosis of brucellosis
include culture, serology and PCR
• Ideally the diagnosis is made by culture of the
organism from blood or other sites such as
bone marrow or liver biopsy specimen
• Results of routine labratory studies are usually
non specifc. White blood cell count are usually
normal to low, pancytopenia can occur.
• Minor abnormalities in hepatic enzymes are
relatively common
• The standard test for the diagnosis of
brucellosis is the isolation of organism from
blood or tissues .
• The sensitivity of blood culture with improved
techniques is approximately 60%
Differential diagnosis
TB
Bacterial pneumonia
FUO
Lymphoma
GU TB
acute epididimitis
bronchitis
Infectious mononucleosis
Meningitis
osteomylitis
Typhoid fever
Treatment
• The goal of medical therapy in brucellosis is to
control symptoms as quickly as possible in
order to prevent complication and relapse.
• Initial care for brucellosis is supportive. Given
the non-specific symptoms the patient
complains it is difficult to diagnose in the ED.
• Although multiple antibiotics display in vitro
activity against brucella species, clinical
respones has been demonstrated with only a
limited number of agents.
• The following drugs display clinical activity
with low relapse rate
• Doxycycline, gentamycin, streptomycin,
rifampin, cotrimoxazole
You might also like
- MCQs in Medical MicrobiologyDocument14 pagesMCQs in Medical Microbiologysidharta_chatterjee100% (8)
- Architects Illustrated Pocket DictionaryDocument558 pagesArchitects Illustrated Pocket DictionaryFlavia ValNo ratings yet
- BrucellosisDocument24 pagesBrucellosisdr. snehal patilNo ratings yet
- Brucellosis 2Document70 pagesBrucellosis 2Zara IftikharNo ratings yet
- Epidemiology & Control of Brucellosis (د عبدالله محرم)Document19 pagesEpidemiology & Control of Brucellosis (د عبدالله محرم)Aiman Al-SharabiNo ratings yet
- BrucellosisDocument55 pagesBrucellosistummalapalli venkateswara rao50% (2)
- Brucellosis: Ali Naim 1 2 0 1 3 1 4 6 2Document19 pagesBrucellosis: Ali Naim 1 2 0 1 3 1 4 6 2Hakim oğluNo ratings yet
- Pathogen Es IsDocument3 pagesPathogen Es Iskarenkaren09No ratings yet
- BrucellosisDocument37 pagesBrucellosisAhlam AliNo ratings yet
- BrucellosisDocument5 pagesBrucellosisOjambo FlaviaNo ratings yet
- JurnalDocument6 pagesJurnalancillaagraynNo ratings yet
- BrucellosisDocument65 pagesBrucellosisKotha Chaitanya AbhiramNo ratings yet
- Brucellosis Is A Disease Caused by Bacteria in The Genus BrucellaDocument28 pagesBrucellosis Is A Disease Caused by Bacteria in The Genus BrucellaAhmed J AlhindaweNo ratings yet
- Brucelosis en Pediatría2018 PDFDocument5 pagesBrucelosis en Pediatría2018 PDFLuis RaymundoNo ratings yet
- 5ZoonosisHandout2009) PDFDocument12 pages5ZoonosisHandout2009) PDFابراهيم القويعىNo ratings yet
- What Is BrucellosisDocument6 pagesWhat Is BrucellosisVenkatesan VidhyaNo ratings yet
- BrucellosisDocument30 pagesBrucellosisMuhammad AwaisNo ratings yet
- Brucella: Melitensis (The Usual Animal Hosts Are Sheep and Goats), B. Abortus (The UsualDocument3 pagesBrucella: Melitensis (The Usual Animal Hosts Are Sheep and Goats), B. Abortus (The UsualGregorio ValllejoNo ratings yet
- BrucellosisDocument27 pagesBrucellosisMah SalNo ratings yet
- What Is BrucellosisDocument2 pagesWhat Is BrucellosisSumbul RafatNo ratings yet
- 7 Brucellosis Plague AnthraxDocument29 pages7 Brucellosis Plague AnthraxHariharanNo ratings yet
- Brucellosis: (The Highly Contagious Zoonosis)Document14 pagesBrucellosis: (The Highly Contagious Zoonosis)swathika'No ratings yet
- Brucellosis: Aka: Mediterranean Fever, Malta Fever, Gastric Remittent Fever, and Undulant FeverDocument11 pagesBrucellosis: Aka: Mediterranean Fever, Malta Fever, Gastric Remittent Fever, and Undulant Feverfairuz160194No ratings yet
- Physics ProjectDocument14 pagesPhysics Projectswathika'No ratings yet
- Brucellosis - SaudiDocument16 pagesBrucellosis - SaudiFaizah Al GhamdiNo ratings yet
- Brucellosis: Diana Samara Department of Occupational Health Faculty of Medicine Trisakti UniversityDocument39 pagesBrucellosis: Diana Samara Department of Occupational Health Faculty of Medicine Trisakti UniversityI Kadek Dwi PradnyanaNo ratings yet
- Zoonotic ImportanceDocument12 pagesZoonotic ImportanceAndika Budi KurniantoNo ratings yet
- Brucella, Francisella and Yersinia Pestis: Gram Negative Rods of ZoonosesDocument12 pagesBrucella, Francisella and Yersinia Pestis: Gram Negative Rods of ZoonosesJanice LiNo ratings yet
- 9 BJDocument21 pages9 BJAna Belén GonzálezNo ratings yet
- Soil Transmitted Helminthiasis IHCPDocument50 pagesSoil Transmitted Helminthiasis IHCPARACELI RAITNo ratings yet
- Brucellosis: By: Samira MuhyadinDocument19 pagesBrucellosis: By: Samira MuhyadinHUSNAH SULAIMANNo ratings yet
- Brucellosis: Synonyms in AnimalsDocument5 pagesBrucellosis: Synonyms in AnimalsVenkatapradeepNo ratings yet
- A Review On Bovine Brucellosis: Epidemiology, Diagnosis and Control OptionsDocument14 pagesA Review On Bovine Brucellosis: Epidemiology, Diagnosis and Control OptionsSajjad LaghariNo ratings yet
- SK320 Section SummariesDocument15 pagesSK320 Section Summariescylon3No ratings yet
- Brucellosis Presentation 11pmDocument34 pagesBrucellosis Presentation 11pmDr abdirauuf Ali mohamedNo ratings yet
- Bioterrorism Agents/Diseases: Student Name: Ayesha AndleebDocument15 pagesBioterrorism Agents/Diseases: Student Name: Ayesha AndleebAisha rana100% (1)
- K-4 PR - Soil Transmitted HelminthiasisDocument45 pagesK-4 PR - Soil Transmitted HelminthiasissantayohanaNo ratings yet
- BrucellosisDocument38 pagesBrucellosisEslam HamadaNo ratings yet
- Hematology PCIDocument50 pagesHematology PCIandebetgetnet78100% (2)
- Brucellosis - DR Esayas Kebede GudinaDocument44 pagesBrucellosis - DR Esayas Kebede GudinaEsayas KebedeNo ratings yet
- Topic 3 Chain of Infection, Disease Transamission, Control and PreventionDocument38 pagesTopic 3 Chain of Infection, Disease Transamission, Control and PreventionF2056 SITI AISYAH BINTI MOHAMMED NOORNo ratings yet
- Key Facts of UltrasonographyDocument2 pagesKey Facts of UltrasonographySajjad LaghariNo ratings yet
- ParasitologyDocument43 pagesParasitologyBatool SherbiniNo ratings yet
- Brucellosis From Mayo ClinicDocument6 pagesBrucellosis From Mayo Clinicد.أحمد ماهر العجوزNo ratings yet
- Malaria: by Tadele Kegnu (MD, MSC.)Document57 pagesMalaria: by Tadele Kegnu (MD, MSC.)semere demissieNo ratings yet
- Chapter 13: Infectious Diseases (Week 26, 27 & 28) : Powerpoint Slides by Ms Lina TangDocument70 pagesChapter 13: Infectious Diseases (Week 26, 27 & 28) : Powerpoint Slides by Ms Lina TangHanaOmarNo ratings yet
- Nam chp24 PDFDocument17 pagesNam chp24 PDFJannatur RahmahNo ratings yet
- Principles of Disease and EpidemiologyR1Document35 pagesPrinciples of Disease and EpidemiologyR1Biancia MckenzieNo ratings yet
- Species Affected: Bluetongue (BTV)Document3 pagesSpecies Affected: Bluetongue (BTV)Andrei CiobanuNo ratings yet
- 4.4 Emerging and Re-Emerging Infectious DiseaseDocument75 pages4.4 Emerging and Re-Emerging Infectious DiseasenorazlienaNo ratings yet
- Zoonotic DiseaseDocument34 pagesZoonotic Diseasebajarangi_chaudhary100% (2)
- Communicable Disease Control in DisasterDocument78 pagesCommunicable Disease Control in DisasterMohamed AhmedNo ratings yet
- NTD and PovertyDocument87 pagesNTD and Povertyfareehakanwar93No ratings yet
- Communicable DiseasesDocument19 pagesCommunicable DiseasesSuad OmarNo ratings yet
- OAJMB16000227Document3 pagesOAJMB16000227Anisha RautNo ratings yet
- Schistomiasis 2014Document110 pagesSchistomiasis 2014officialmwalusambaNo ratings yet
- Course Title: Ruminant and Non-Ruminant Preventive MedicineDocument32 pagesCourse Title: Ruminant and Non-Ruminant Preventive MedicineFarhan NobelNo ratings yet
- Soil-Transmitted Helminth InfectionsDocument7 pagesSoil-Transmitted Helminth InfectionsDiane GaliNo ratings yet
- Emerging DiseasesDocument27 pagesEmerging DiseasesMadhavi ModaNo ratings yet
- Biology Project: Topic: Human Health and DiseasesDocument17 pagesBiology Project: Topic: Human Health and DiseasesSagar Kumar0% (1)
- Brucella Infection in Domestic Animals in Nigeria A ReviewDocument7 pagesBrucella Infection in Domestic Animals in Nigeria A ReviewSajjad LaghariNo ratings yet
- Mediterranean Fever, (Brucellosis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandMediterranean Fever, (Brucellosis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- SyphilisDocument115 pagesSyphilisabel semuNo ratings yet
- Elonnn MuuuuuskDocument27 pagesElonnn Muuuuuskabel semuNo ratings yet
- Ethiopian TB 2008 PDFDocument207 pagesEthiopian TB 2008 PDFabel semuNo ratings yet
- StdsDocument71 pagesStdsabel semuNo ratings yet
- PertussisDocument63 pagesPertussisabel semuNo ratings yet
- MeningitisDocument80 pagesMeningitisabel semuNo ratings yet
- AnthraxDocument47 pagesAnthraxabel semuNo ratings yet
- 2005Document67 pages2005abel semu100% (1)
- Sarcomastigophora: A Phylum of PROTOZOA Subphyla: SARCODINA and Have Flagella or PseudopodiaDocument20 pagesSarcomastigophora: A Phylum of PROTOZOA Subphyla: SARCODINA and Have Flagella or Pseudopodiaabel semuNo ratings yet
- CholeraDocument59 pagesCholeraabel semuNo ratings yet
- Study of These Parasitic Worms and Their Medical ConsequenceDocument33 pagesStudy of These Parasitic Worms and Their Medical Consequenceabel semuNo ratings yet
- Toxo For 2Document13 pagesToxo For 2abel semuNo ratings yet
- PDFDocument65 pagesPDFabel semu100% (1)
- PDFDocument30 pagesPDFabel semuNo ratings yet
- AmraDocument6 pagesAmraShantu ShirurmathNo ratings yet
- Ec8252 SyllabusDocument1 pageEc8252 SyllabusSarika AyyathuraiNo ratings yet
- GRILL StationDocument19 pagesGRILL Stationradwa.talaatNo ratings yet
- Thesis CoutureDocument6 pagesThesis Couturemariapolitepalmdale100% (2)
- The Learners Demonstrate An Understanding of Some Important Properties of SolutionsDocument4 pagesThe Learners Demonstrate An Understanding of Some Important Properties of Solutionsjennelyn malaynoNo ratings yet
- Thesis On Wind Power PlantDocument6 pagesThesis On Wind Power PlantPaperWritingServicesBestEvansville100% (2)
- MEO Class 1 ProjectDocument2 pagesMEO Class 1 ProjectAshish Ranjan0% (1)
- Trigonometry - Straight Lines - Voronoy Diagrams - Basic Concepts of FunctionsDocument6 pagesTrigonometry - Straight Lines - Voronoy Diagrams - Basic Concepts of FunctionselenaNo ratings yet
- 15 Combined Cycle Power Plant OperationDocument21 pages15 Combined Cycle Power Plant OperationParmeshwar Nath Tripathi100% (4)
- TRC 495 ManualDocument20 pagesTRC 495 ManualRich RitterbuschNo ratings yet
- CT Scan BasicsDocument28 pagesCT Scan BasicsPauline Burgos100% (1)
- Astm D1193Document6 pagesAstm D1193eaarizac100% (7)
- Exponential Shadow Maps: BstractDocument7 pagesExponential Shadow Maps: BstractTed De LeonNo ratings yet
- List of en StandardsDocument21 pagesList of en StandardsKaranjaNo ratings yet
- Delegate List - 10th IMRC With Contact Details - Removed (1) - RemovedDocument234 pagesDelegate List - 10th IMRC With Contact Details - Removed (1) - RemovedSharon SusmithaNo ratings yet
- Annex HDocument5 pagesAnnex HAdriana Andrade CNo ratings yet
- Kenwood Krc-15rg 179ra RG Rya Ryg 25ra RG 279ra RG Rya Ryg 281rgDocument21 pagesKenwood Krc-15rg 179ra RG Rya Ryg 25ra RG 279ra RG Rya Ryg 281rgNenadBlaškovićNo ratings yet
- Cherry 1900 Bulbing Blind Rivet: SPS Fastener Division, ADocument4 pagesCherry 1900 Bulbing Blind Rivet: SPS Fastener Division, AДенис СергеевичNo ratings yet
- Cold Injuries and HypothermiaDocument34 pagesCold Injuries and HypothermiaRam Kirubakar ThangarajNo ratings yet
- SolidWorks Routing Piping and TubingDocument2 pagesSolidWorks Routing Piping and Tubingbadmus babatundeNo ratings yet
- Unit 4 Travel and Holidays: Pre IeltsDocument21 pagesUnit 4 Travel and Holidays: Pre IeltsQuoc Tan HuynhNo ratings yet
- Instruction Manual Pygmy Current Meter Model Oss-Pc1: Hyquest Solutions Pty LTDDocument17 pagesInstruction Manual Pygmy Current Meter Model Oss-Pc1: Hyquest Solutions Pty LTDTomás Londoño GarcíaNo ratings yet
- Angelika de Vera CWTS123Document6 pagesAngelika de Vera CWTS123Angelika De VeraNo ratings yet
- 01-M115 Iss 2 (BS en 1290 - Electromagnet, (Fluorescent) )Document3 pages01-M115 Iss 2 (BS en 1290 - Electromagnet, (Fluorescent) )DeepakNo ratings yet
- Material Safety Data Sheet June'09 Update: Product Name: Product Code: Date PrintedDocument3 pagesMaterial Safety Data Sheet June'09 Update: Product Name: Product Code: Date PrintedEDSON CARLOS SOUSANo ratings yet
- Pump SystemsDocument45 pagesPump SystemsJagdip ShethNo ratings yet
- Emissivity Measurement of Radiating SurfacesDocument4 pagesEmissivity Measurement of Radiating Surfacesashish100% (1)
- Grade 9 Math Q1 M1Document12 pagesGrade 9 Math Q1 M1Renny Romero Luzada100% (2)