Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
13 viewsEndocrine System
Endocrine System
Uploaded by
Divya JaiswalThe endocrine system consists of glands that secrete hormones directly into the bloodstream. The pituitary gland, also known as the "master gland", regulates other endocrine glands and plays an important role in homeostasis. It has two lobes - the anterior lobe secretes seven hormones including growth hormone and prolactin, while the posterior lobe stores and releases oxytocin and antidiuretic hormone produced by the hypothalamus. Together, the hormones of the endocrine system control processes like growth, metabolism, and reproduction throughout the body.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You might also like
- SCIENCE-10-Q3 WORKSHEET REVISED COPY-week-1-7Document46 pagesSCIENCE-10-Q3 WORKSHEET REVISED COPY-week-1-7Gian Evangelista67% (6)
- Boys and Puberty BookletDocument9 pagesBoys and Puberty Bookletఫణీంద్ర నర్సెట్టి50% (2)
- Endocrine SystemDocument96 pagesEndocrine SystemSandhya Kakkar100% (3)
- LECTURE 1 Endocrine Diseases Lecture 1 January 10-020Document68 pagesLECTURE 1 Endocrine Diseases Lecture 1 January 10-020aleen qawareetNo ratings yet
- endocrine فسيولوجياDocument49 pagesendocrine فسيولوجياAUDEH AHMADNo ratings yet
- Endocrine PhysiologyDocument98 pagesEndocrine PhysiologyMohan GuptaNo ratings yet
- ENDOCRINE SYSTEM DISORDERS PROPER BestDocument370 pagesENDOCRINE SYSTEM DISORDERS PROPER BestronaronixstheboyNo ratings yet
- Hormones 080623Document83 pagesHormones 080623Rao Asad MubeenNo ratings yet
- Hypothalamus and Pituitary GlandDocument62 pagesHypothalamus and Pituitary GlandphyMedza AppNo ratings yet
- Endocrinology Endocrinology: H. KibichoDocument370 pagesEndocrinology Endocrinology: H. KibichoMursal RashidNo ratings yet
- CBSE Quick Revision Notes (Class-11 Biology) Chapter-22 Chemical Coordination and IntegrationDocument3 pagesCBSE Quick Revision Notes (Class-11 Biology) Chapter-22 Chemical Coordination and IntegrationNANDAKUMAR BABUNo ratings yet
- CBSE Quick Revision Notes (Class-11 Biology) Chapter-22 Chemical Coordination and IntegrationDocument3 pagesCBSE Quick Revision Notes (Class-11 Biology) Chapter-22 Chemical Coordination and IntegrationNANDAKUMAR BABUNo ratings yet
- Ila College of Health: Endocrine PhysiologyDocument40 pagesIla College of Health: Endocrine PhysiologyDaniel DendaNo ratings yet
- Regulasi Endokrin 22 IntensifDocument25 pagesRegulasi Endokrin 22 IntensifWignes WarenNo ratings yet
- Hormonal BiochemistryDocument82 pagesHormonal BiochemistryRuthNo ratings yet
- Endocrine GlandsDocument36 pagesEndocrine GlandsnasyitahnorzlanNo ratings yet
- Hypothalamus & Pituitary GlandDocument39 pagesHypothalamus & Pituitary GlandVishal DodejaNo ratings yet
- Pituitary and ThyroidDocument54 pagesPituitary and ThyroidSaif AliNo ratings yet
- Endocrine SystemDocument30 pagesEndocrine SystemAkshat RastogiNo ratings yet
- Endocrine System: Endocrine: Which Have No Duct and ReleaseDocument36 pagesEndocrine System: Endocrine: Which Have No Duct and Releasedr_saleh77No ratings yet
- Hormones:: Signaling MoleculesDocument20 pagesHormones:: Signaling MoleculesSangeeta DwivediNo ratings yet
- EndocrineDocument94 pagesEndocrineHira NawazNo ratings yet
- Endo AnaphysioDocument9 pagesEndo AnaphysioShelley Jade MenorNo ratings yet
- Seminor On Hormons Slide2 by Prof - Dr.HariharDocument49 pagesSeminor On Hormons Slide2 by Prof - Dr.Hariharhariharb999_23960100No ratings yet
- HormonesDocument29 pagesHormonesCandy Chieng67% (3)
- Endocrine System - MorphophysiologyDocument88 pagesEndocrine System - MorphophysiologyKarina Bustillo100% (1)
- Metabolic & Endocrine DiseasesDocument280 pagesMetabolic & Endocrine DiseasesHussenNo ratings yet
- Hormones (Short Version)Document80 pagesHormones (Short Version)Vivek ChaudharyNo ratings yet
- HORMONESDocument65 pagesHORMONESsoumya palavalasaNo ratings yet
- Physiology 1STDocument10 pagesPhysiology 1STGW LEGENDNo ratings yet
- Endocrine PhysiologyDocument76 pagesEndocrine Physiologykidusabeje7No ratings yet
- Endocrine Anatomy and PhysiologyDocument10 pagesEndocrine Anatomy and PhysiologyJojo JustoNo ratings yet
- Hypothalamus and Pituitary GlandDocument48 pagesHypothalamus and Pituitary GlandMohsin AbbasNo ratings yet
- Endocrinology Apllied ScienceDocument44 pagesEndocrinology Apllied ScienceAdam PrabowoNo ratings yet
- The Endocrine System The Endocrine System: © 2018 Pearson Education, Ltd. 1Document12 pagesThe Endocrine System The Endocrine System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- Endocrine SystemDocument30 pagesEndocrine SystemBrenda Domaneo BaseNo ratings yet
- Endocrine Physiology For AnsthesiaDocument60 pagesEndocrine Physiology For AnsthesiaCHALIE MEQUNo ratings yet
- The Endocrine System PDFDocument27 pagesThe Endocrine System PDFpratiksha.bhattacharjeeNo ratings yet
- Endocrine SystemDocument22 pagesEndocrine SystemkwatsNo ratings yet
- Endocrine SystemDocument18 pagesEndocrine SystemDioh EmmanuelNo ratings yet
- Chemical Coordination and IntegrationDocument6 pagesChemical Coordination and IntegrationRonaldNo ratings yet
- Endocrine SystemDocument41 pagesEndocrine SystemMerrin EncarnacionNo ratings yet
- The Endocrine System: Endocrine Gland (Ductless Gland)Document50 pagesThe Endocrine System: Endocrine Gland (Ductless Gland)Mohammad AliNo ratings yet
- Quick Revision NotesDocument3 pagesQuick Revision NoteslinzihaoleoNo ratings yet
- Chemical Coordination and Integration Handwriten Notes For Neet and JeeDocument5 pagesChemical Coordination and Integration Handwriten Notes For Neet and JeetechnosonicindiaNo ratings yet
- PD22 Hap1 L03Document33 pagesPD22 Hap1 L03Ka Yan LAUNo ratings yet
- EndocrinologyDocument74 pagesEndocrinologysyedahaleemajunaidsNo ratings yet
- Biochemistry of Hormones (Part 1)Document31 pagesBiochemistry of Hormones (Part 1)arun231187100% (1)
- Endocrine System/socialDocument33 pagesEndocrine System/socialrpant3165No ratings yet
- Option D - Unit 5 - HormonesDocument28 pagesOption D - Unit 5 - Hormonesjanafahmy1211No ratings yet
- Unit IXDocument10 pagesUnit IXPreeti ChouhanNo ratings yet
- Anatomy and Physiology of The Endocrine System: Presenté ParDocument64 pagesAnatomy and Physiology of The Endocrine System: Presenté ParYackson Frank100% (1)
- UntitledDocument12 pagesUntitledDerrick kinyaNo ratings yet
- Endocrine System: Glands & HormonesDocument78 pagesEndocrine System: Glands & HormonesJerilee SoCute WattsNo ratings yet
- 4 Pituitary HormonesDocument18 pages4 Pituitary HormonesRana AbdullahNo ratings yet
- Functional Anatomy and PhysiologyDocument38 pagesFunctional Anatomy and PhysiologyNawalNo ratings yet
- EndocrinologyDocument37 pagesEndocrinologyKochaMsangiNo ratings yet
- Hormones: Mark Angelo R. Jacosalem Faye Bernadette O. Reyes Ma. Elizabeth VerteraDocument40 pagesHormones: Mark Angelo R. Jacosalem Faye Bernadette O. Reyes Ma. Elizabeth VerteraGelo Robin JacosalemNo ratings yet
- Principles of Hormonal Control SystemDocument25 pagesPrinciples of Hormonal Control SystemFAHEEM UD DINNo ratings yet
- Hormones SubtopicsDocument77 pagesHormones SubtopicsSulaiman UmraniNo ratings yet
- Balancing Hormones Naturally: A Woman's Guide to Hormonal Harmony: HealthFrom EverandBalancing Hormones Naturally: A Woman's Guide to Hormonal Harmony: HealthNo ratings yet
- Thyroid Health: The Thyroid Solution Diet ExposedFrom EverandThyroid Health: The Thyroid Solution Diet ExposedRating: 3 out of 5 stars3/5 (2)
- Nervous SystemDocument140 pagesNervous SystemDivya JaiswalNo ratings yet
- 1 General Anatomy - Levels of Organization EtcDocument36 pages1 General Anatomy - Levels of Organization EtcDivya JaiswalNo ratings yet
- General Anatomy - 4Document22 pagesGeneral Anatomy - 4Divya JaiswalNo ratings yet
- 6 Human Anatomy - Muscular SystemDocument34 pages6 Human Anatomy - Muscular SystemDivya JaiswalNo ratings yet
- Acute Interstitial NephritisDocument36 pagesAcute Interstitial NephritisosaqerNo ratings yet
- CHOLECYSTITIS CASE STUDY Version 2.0Document57 pagesCHOLECYSTITIS CASE STUDY Version 2.0Gabriel Arch100% (1)
- Cara Membaca Foto Thoraks Yang BaikDocument2 pagesCara Membaca Foto Thoraks Yang BaikIdi Nagan RayaNo ratings yet
- IBDP Biology Option - D - SummaryDocument5 pagesIBDP Biology Option - D - SummaryRafi FarhanNo ratings yet
- Case Pres HydronephrosisDocument39 pagesCase Pres HydronephrosisLouie Dela Cruz100% (3)
- Review Article: Relevant Biliary Anatomy During CholecystectomyDocument11 pagesReview Article: Relevant Biliary Anatomy During CholecystectomyAbrar SabawiNo ratings yet
- PHPY 303 - GI Lecture #1 - March 10Document30 pagesPHPY 303 - GI Lecture #1 - March 10smhallmobileNo ratings yet
- General Surgery: (Gallbladder Disease)Document1 pageGeneral Surgery: (Gallbladder Disease)Matt100% (1)
- PHYSIOLOGYDocument10 pagesPHYSIOLOGYapi-1986354875% (4)
- Chapter 13 - The Peripheral Nervous System and Reflex ActivityDocument53 pagesChapter 13 - The Peripheral Nervous System and Reflex Activityramadan100% (1)
- Science 8 - 3Document5 pagesScience 8 - 3Sherine Marianne IgnacioNo ratings yet
- Jurnal 2 (2019)Document11 pagesJurnal 2 (2019)Inryuu ZenNo ratings yet
- Mod 8 ZooDocument10 pagesMod 8 ZooLM Tricia T. DE LA CRUZNo ratings yet
- B - SC Nursing I Year SyllabusDocument159 pagesB - SC Nursing I Year SyllabusSusheelabaiNo ratings yet
- Heart, Nerve and Mucsle, Membrane Transport Mcqs With KeyDocument8 pagesHeart, Nerve and Mucsle, Membrane Transport Mcqs With KeyMudassar Roomi100% (7)
- Brain Computer InterfaceDocument11 pagesBrain Computer InterfaceNeha ArifNo ratings yet
- Acute GlomerulonephritisDocument18 pagesAcute GlomerulonephritisdanielaNo ratings yet
- Anatomia de Puntos Craneometricos PDFDocument35 pagesAnatomia de Puntos Craneometricos PDFAlberto SalazarNo ratings yet
- Chapter 39 AntihypertensivesDocument4 pagesChapter 39 AntihypertensivesErika Joy Cabison TamayoNo ratings yet
- Benign Thyroid DiseasesDocument138 pagesBenign Thyroid DiseasesAliNo ratings yet
- 07 Post Mortem Examination (Autopsy)Document48 pages07 Post Mortem Examination (Autopsy)ARIF-UR-REHMAN100% (5)
- Previous Year'S Questions (Excretion)Document1 pagePrevious Year'S Questions (Excretion)veeresh punjaniNo ratings yet
- Digestive System in Non-RuminantsDocument5 pagesDigestive System in Non-RuminantsTumisang TlhabanoNo ratings yet
- Bikram Yoga PosturesDocument4 pagesBikram Yoga PosturesMony SánchezNo ratings yet
- Science6 ST1 Q2Document4 pagesScience6 ST1 Q2Meriam LuatNo ratings yet
- Chapter 10 - Immune Responses Against Tumors and TransplantsDocument11 pagesChapter 10 - Immune Responses Against Tumors and TransplantsFYMNo ratings yet
- Li 1 Anatomy, Histology, PhysiologyDocument17 pagesLi 1 Anatomy, Histology, PhysiologysandyaadindaNo ratings yet
- Lipids Metabolism ReviewerDocument2 pagesLipids Metabolism RevieweroperanacireNo ratings yet
Endocrine System
Endocrine System
Uploaded by
Divya Jaiswal0 ratings0% found this document useful (0 votes)
13 views69 pagesThe endocrine system consists of glands that secrete hormones directly into the bloodstream. The pituitary gland, also known as the "master gland", regulates other endocrine glands and plays an important role in homeostasis. It has two lobes - the anterior lobe secretes seven hormones including growth hormone and prolactin, while the posterior lobe stores and releases oxytocin and antidiuretic hormone produced by the hypothalamus. Together, the hormones of the endocrine system control processes like growth, metabolism, and reproduction throughout the body.
Original Description:
Original Title
Untitled
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe endocrine system consists of glands that secrete hormones directly into the bloodstream. The pituitary gland, also known as the "master gland", regulates other endocrine glands and plays an important role in homeostasis. It has two lobes - the anterior lobe secretes seven hormones including growth hormone and prolactin, while the posterior lobe stores and releases oxytocin and antidiuretic hormone produced by the hypothalamus. Together, the hormones of the endocrine system control processes like growth, metabolism, and reproduction throughout the body.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
13 views69 pagesEndocrine System
Endocrine System
Uploaded by
Divya JaiswalThe endocrine system consists of glands that secrete hormones directly into the bloodstream. The pituitary gland, also known as the "master gland", regulates other endocrine glands and plays an important role in homeostasis. It has two lobes - the anterior lobe secretes seven hormones including growth hormone and prolactin, while the posterior lobe stores and releases oxytocin and antidiuretic hormone produced by the hypothalamus. Together, the hormones of the endocrine system control processes like growth, metabolism, and reproduction throughout the body.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 69
ENDOCRINE SYSTEM
• The nervous system and the endocrine system are
the two main coordinating and controlling systems
of the body.
• There are several differences between these two
systems. For example, the nervous system acts by
means of electrical impulses and chemical stimuli;
where as the endocrine system has more
widespread, slower, and longer lasting effects.
• The endocrine system also has more generalized
effects on the activities like growth, metabolism,
and reproduction.
• Despite difference, the two systems are closely
interrelated.
Hormones
• They are chemical messengers released by the
glands of endocrine system.
• Released directly into the blood stream and
carried to the tissues where they act.
•The blood reaches all the cells of body, but only
certain cells respond to specific hormones; these
responding cells have receptors to which specific
hormones attach.
• Only cells that have receptors for a particular
hormone will respond to that hormone; these
cells make up the target tissues.
Chemistry of Hormones
• Hormones fall chemically in two categories:
1. Proteins: All hormones except those of the
adrenal cortex and the sex glands are proteins
or related compounds composed of amino
acids.
2. Steroids: hormones derived from lipids and
produced by the adrenal cortex and the sex
glands.
• All hormones are extremely potent, & are
effective in very small amounts (Traces).
Endocrine Glands and Their Hormones
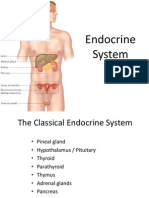
• The endocrine system consists of the glands that secrete
hormones.
• These glands are ductless glands because they secrete
their products directly into the blood stream, while the
exocrine glands, secrete into body cavities through their
ducts.
• Most endocrine glands, like exocrine glands, are made of
epithelial tissue. They have no ducts, but they have
extensive blood vessel network.
• So operations on endocrine glands, e.g. thyroid, require
care in the control of bleeding.
• Adrenal, or suprarenal, glands have the richest blood
supply & are located at the upper part of the kidneys.
• Some of the Endocrine glands e.g. pancreas and
the sex glands, have other non-endocrine
functions also, but hormone secretion is one of
their main functions.
• Some body organs, such as stomach, small
intestine, and kidney, produce hormones, but
their main function is not hormone production.
Endocrine System : Endocrine glands and cells are
located throughout the body and play an important role
in homeostasis.
The Pituitary Gland
• The pituitary gland or hypophysis, earlier called
the "Master gland", secretes several polypeptide
hormones that directly or indirectly regulate a
wide variety of metabolic and physiologic
processes, essential for normal growth and
development as well as for the maintenance of
homeostasis.
• Many hormones secreted by the pituitary gland
are critical for the activity of target glands, e.g.
thyroid, adrenal and gonads.
Anatomy of Pituitary gland
• The pituitary gland (hypophysis cerebri) is
located at the base of the brain, resting
with in the Sella Turcica of the sphenoid
bone.
• It maintains elaborate neural and vascular
connections with the hypothalamus of the
brain, & plays a central role in the
integration of neuro-endocrine activity
• The pituitary gland has two major divisions:
• The anterior lobe (adeno-hypophysis) and the
posterior lobe (neuro-hypophysis).
• Adeno-hypophysis has an elaborate vascular
system.
• There are five types of cells in anterior lobe of
Pituitary gland.
1. Somatotrophs, which secrete growth
hormone (hGH) or somatotropin.
2. Lactotrophs, which secret prolactin (PRL).
3. Corticotrophs, which produce corticotropin
(ACTH) and beta-lipotropin (beta-LPH).
4. Thyrotrophs, which secrete thyrotropin (TSH).
5. Gonadotrophs, which produce follicle
stimulating hormone ( FSH) and luteinizing
hormone (LH)
The anterior pituitary manufactures seven hormones. The
hypothalamus produces separate hormones that stimulate or
inhibit hormone production in the anterior pituitary. Hormones
from the hypothalamus reach the anterior pituitary via the
hypophyseal portal system.
Neuro-hypophysis (Posterior Pituitary)
• The neuro-hypophysis, which is connected directly to
the hypothalamus by the infundibular (Pituitary)
stalk, is rich in nerve fibers of hypothalamic origin
(the hypotahlamo-hypophyseal tract).
• Neurosecretory cells in the supra-optic and
paraventricular nuclei of the hypothalamus produce
two hormones: antidiuretic hormone (ADH or
Vasopressin) & oxytocin.
• These hormones are then transported along the
axons of the hypothalamo-hypophyseal tract to the
posterior lobe of the pituitary gland for storage and
ultimately released under hypothalamic control.
Posterior Pituitary Neurosecretory cells in the hypothalamus
release oxytocin (OT) or ADH into the posterior lobe of the
pituitary gland. These hormones are stored or released into the
blood via the capillary plexus.
Hormones of the Adeno-Hypophysis
• The secretion of hormones by the adeno-hypophysis is
controlled by hypo-thalamic regulatory (hypo-physeotropic)
hormones that are transported to the pituitary gland by the
hypothalamohypophyseal portal system.
• Six hormones secreted from the median eminence of the
hypothalamus:
1. Growth hormone-releasing hormone (GHRH; somatocrinin)
2. Growth hormone-inhibiting hormone (GHIH; somatostatin)
3. Corticotropin-releasing homone (CRH)
4. Thyrotropin-releasing hormone (TRH)
5. Gonadotropin-releasing hormone (GnRH)
6. Prolactin-inhibiting hormone (PIH)
1. Growth Hormone (GH); Somatotropin (STH) :
Human growth hormone (hGH) is a peptide
hormone composed of 191 amino acids, and is
secreted by the somatotrophs of the adeno-
hypophysis primarily under hypothamic control.
2. Factors Promoting GH Secretion
• GHRH (Somatocrinin)
• Hypoglycemia and fasting
• Elevated plasma levels of amino acids (e.g.,
arginine)
• Stress (physical or psychological)
• Exercise, Deep sleep, Levodopa & Glucagon
• Factors Inhibiting GH Secretion
• GHIH (Somatostatin)
• Hyperglycemia
• Elevated plasma levels of free fatty acids
• REM sleep, Cortisol,Alpha-adrenergic
blocking agents &
• GH (negative feedback mechanism): GH
secretion in response to hypoglycemia,
fasting, and exercise is reduced by obesity.
• Actions
• Effects on Growth: Growth is a influenced by
genetic, nutritional, and hormonal factors.
• In addition to growth hormone, thyroid
hormones, insulin, androgens, and estrogens also
affect normal human growth and development.
• GH accelerates overall body growth by increasing
the mass of both skeletal and soft tissues
through hyperplasia (increased cell number) and
hypertrophy (increased cell size).
• Effects of GH are more evident in skeletal tissues
where chondro-genesis (cartilage formation) and
osteogenesis (bone formation) are enhanced,
leading to an increase in growth and stature
before epiphyseal closure and increased bone
thickness after closure of epiphyses.
• Growth hormone stimulates certain tissues, e.g.
liver, to produce insulin like growth factors (IGF-I
and IGF-II) which mediate the growth-promoting
effects of GH, e.g. stimulation of collagen
synthesis and chondrogenesis.
• Metabolic Effects
• Protein metabolism: GH increases protein
synthesis and nitrogen retention by enhancing the
incorporation of amino acids into protein. The
protein anabolic action results from
1) Accelerated entry of amino acids into cells &
2) Increased RNA synthesis.
• In muscle and liver, the protein anabolic effects
are attributed directly to GH. However, in
cartilage, bone, and other body tissues, the
protein anabolic and growth-promoting actions
are mediated by insulin like growth factors
(somatomedins).
• 2. Prolactin (PRL)
• Control of Secretion Prolactin (PRL) is a peptide
hormone composed of 199 amino acids. Its secretion by
the lactotrophs of the adenohypoiphysis is tonically
suppressed by dopamine (also known as PIH) of
hypothalamic origin. Dopamine antagonists (eg,
antipsychotic drugs) promote PRL secretion by blocking
dopamine receptors, whereas dopamine agonists (eg,
bromocriptine) inhibit PRL secretion by activating
dopamine eceptors. Secretion of PRL increases during
pregnancy, peaking near the time of parturition. Sucking
and tactile stimulation of the nipple increase PRL
secretion. Prolactin facilitates the secretion of dopamine
in the hypothalamus, thereby regulating its own
secretion by a negative feedback mechanism.
• Actions : Prolactin initiates and maintains milk
secretion from breasts primed for lactation by
other hormones such as estrogens,
progesterone, and insulin. It also appears to
inhibit the effects of the gonadotropins and
may prevent ovulation in lactating women.
Excessive production of PRL
(hyperprolactinemia), which may accompany
some pituitary tumors, may cause an
ovulation and amenorrhea in women, and
may lead to impotence and infertility in men.
• Lipid metabolism: GH stimulates the
mobilization and utilization of fats by promoting
lipolysis in adipose tissue, thus enabling the
body to use stored fats as an energy source.
• Carbohydrate metabolism: GH elevates blood
glucose levels by increasing the hepatic output
of glucose (gluco-neogenesis) and impairing
glucose transport into muscle and adipose tissue
("anti-insulin" action). Excessive secretion of GH
may precipitate or increase the severity of
clinical diabetes mellitus ("diabetogenic" effect).
2. Prolactin (PRL)
• Control of Secretion
• Prolactin (PRL) is a peptide hormone composed of 199 amino
acids. Its secretion by the lactotrophs of the adenohypoiphysis
is tonically suppressed by dopamine (also known as PIH) of
hypothalamic origin. Dopamine antagonists (eg, antipsychotic
drugs) promote PRL secretion by blocking dopamine receptors,
whereas dopamine agonists (eg, bromo-criptine) inhibit PRL
secretion by activating dopamine receptors.
• Secretion of PRL increases during pregnancy, peaking near the
time of parturition. Sucking and tactile stimulation of the
nipple increase PRL secretion.
• Prolactin facilitates the secretion of dopamine in the
hypothalamus, thereby regulating its own secretion by a
negative feedback mechanism.
• Actions
• Prolactin initiates and maintains milk secretion from
breasts primed for lactation by other hormones
such as estrogens, progesterone, and insulin.
• It also appears to inhibit the effects of the
gonadotropins and may prevent ovulation in
lactating women.
• Excessive production of PRL (hyper-prolactinemia),
which occurs in some pituitary tumors, may cause
an ovulation and amenorrhea in women, and may
lead to impotence and infertility in men.
3. Follicle-Stimulating Hormone (FSH)
• Control of Secretion
• FSH is a glycoprotein, gonadotropic hormone whose
secretion is stimulated by hypothalamic GnRH. Inhibit, a
polypeptide produced by testicular sertoli cells in the
male and follicular granulosa cells in the female, acts
directly on the adenohypophysis to inhibit FSH
secretion.
• Actions
• FSH directly stimulates the sertoli cells in testicular
seminiferous tubles, there by promoting
spermatogenesis in the male. In the female, FSH
stimulates follicular growth and development within the
ovaries. The actions of FSH are mediated by cyclic AMP.
4. Luteinizing Hormone (LH; Interstitial Cell Stimulating
Hormone; ICSH)
• Control of Secretion : Like FSH, LH is a glycoprotein
hormone whose secretion is stimulated by GnRH.
Testosterone inhibits LH secretion through a direct
action on the adenohypophysis, as well as indirectly by
inhibiting hypothalamic GnRH production.
• The effects of female hormones on LH secretion are
more complex. Constant, moderate levels of estrogen
(without progesterone) have a negative feedback effect
on LH, whereas high estrogen levels exert a positive
feedback that leads to a surge in LH production. High
levels of progesterone and estrogen (luteal phase of the
ovulatory cycle) inhibit LH secretion.
• Actions
• In male, LH stimulates testosterone production
by testicular interstitial cells (of Leydig); so the
alternate name, interstitial cell stimulating
hormone (ICSH).
• In female, LH promotes maturation of ovarian
follicles and sustains their secretion of estrogens.
• LH is also responsible for ovulation and the
formation of the corpus luteum.
• The actions of LH are mediated by cyclic AMP.
5. Thyroid-Stimulating Hormone (Thyrotropin; TSH)
• Control of Secretion
• Thyrotropin-releasing hormone (TRH) and cold (especially in
infants) promote secretion of TSH by the thyrotrophs of the
adenohypophysis. Elevated plasma levels of free thyroid
hormones (T3 and T4) inhibit thyrotropin secretion. Stress
also inhibits TSH secretion.
• Actions
• Thyroid-stimulating hormone maintains the structural
integrity of the thyroid gland and promotes the synthesis and
release of thyroid hormones thyroxine (T4) and
triiodothyronine (T3).
• The actions of TSH on the thyroid gland are mediated by
cyclic AMP, and they are detailed in the section on the thyroid
gland.
6. Adrenocorticotropic Hormone
(Corticotropin; ACTH)
• Control of Secretion
• Adrenocorticotropic hormone (ACTH) is secreted in
irregular bursts that follow a diurnal circadian rhythm,
with peak production in the early morning.
• ACTH secretion is regulated by the hypophyseotropic &
corticotropin-releasing hormone (CRH)
• Increased production of ACTH in response to many
stressors appears to be mediated through the
hypothalamus and CRH. Elevated plasma free
glucocorticoid (cortisol) levels inhibit both CRH and
ACTH secretion.
• Actions of ACTH
• Adreno-cortico-tropic hormone exerts its
effects on the adrenal glands, promoting
structural integrity and steroido-genesis in the
adrenal cortex.
• The stimulation of corticosteroid production
(Steroido-genesis) in response to ACTH is
mediated by the second messenger, cyclic
AMP.
Hormones of the Neurohypophysis (Post Pituitary)
1. Antidiuretic Hormone (ADH; Vasopressin)
• Control of Secretion : Antidiuretic hormone (ADH) is
a : polypeptide hormone of hypothalamic origin that
is stored and released from the neurohypophysis in
response to a variety of stimuli e.g. increased
plasma osmolality, reduced extracellular fluid (ECF)
volume, pain, emotional stress, andpharmacologic
agents as morphine, nicotine, barbiturates, and
certain general anesthetics.
• Decreased plasma osmolality, increased ECF volume,
and alcohol inhibit ADH secretion.
• Actions of ADH:
• The principal physiologic role of ADH is to regulate
extracellular fluid volume and osmolality by
controlling the final volume and concentration of
urine.
• ADH increases the permeability of the distal nephron
to water. The enhanced reabsorption of water from
the renal tubules results in the production a
concentrated urine that is reduced in volume.
• Pharmacologic amounts of ADH produce a pressor
(hypertensive) effect that results from a direct
constrictor action of the hormone on vascular
smooth muscle.
2. Oxytocin
• Control of Secretion and Actions
• The two major physiologic actions of oxytocin are exerted on the female
breast and uterus.
• Oxytocin binds to a G-protein coupled receptor that ultimately brings
about elevated intracellular calcium levels.
• Galactokinetic Action (Milk Ejection Reflex). The ejection of milk from a
primed, lactating mammary gland follows a neuroendocrine reflex in
which oxytocin serves as the efferent limb. The reflex is normally initiated
by sucking, which stimulates cutaneous receptors in the areola of the
breast. Afferent nerve impulses travel to the supraoptic and
paraventricular nuclei of the hypothalamus to effect the release of
oxytocin from the neurohypophysis. Oxytocin is carried by the blood to
the mammary gland, where it causes contraction of myoepithelial cells
surrounding the alveoli and lactiferous ducts to bring about the ejection
of milk (milk letdown). In lactating women, tactile stimulation of the
breast areola, emotional stimuli, and genital stimulation may also lead to
oxytocin release and activate the ejection of milk.
• Oxytocic Action. Oxytocin acts directly on
uterine smooth muscle to elicit strong, rhythmic
contractions of the myometrium. Uterine
sensitivity to oxytocin varies with its physiologic
state and with hormonal balance.
• The gravid (Pregnant) uterus is highly sensitive
to oxytocin, particularly in the late stages.
• Uterine sensitivity to oxytocin is greatly
enhanced by estrogen and inhibited by
progesterone.
Thyroid Gland
• Hormones of the thyroid gland exert a wide variety of metabolic
and physiologic actions that affect almost every tissue in the
body.
• Anatomy
• Thyroid gland is a bi-lobed organ overlying the trachea anteriorly
& is composed of numerous closely packed spheres or follicles.
Each follicle consists of a simple cuboidal epithelium (follicular
cells) enclosing a lumen or cavity containing a viscous hyaline
substance called colloid.
• Chief constituent of the colloid is the iodinated glycoprotein
thyroglobulin.
• Interspersed among the follicles are small clusters of
parafollicular (C) cells, which secrete calcitonin, a hormone
affecting calcium metabolism.
• Thyroid Hormones
• Thyroid gland secrete two hormones, thyroxine
(Tetraiodothyronine or T4) and Triiodothyronine
(T3).
• The plasma levels of these hormones are regulated
by the hypothalamo-pituitary axis as outlined in
Figure 8-2.
• Intrinsic (intrathyroidal) mechanisms, as well as
bioavailability of iodine, influence thyroid hormone
production.
• T3 and T4 remain stored within the colloid bound
to thyroglobulin until a stimulus by TSH for
secretion.
Thyroid Hormones : Actions
• Thyroid hormones increase the rate of
metabolism, total heat production, and oxygen
consumption in most body tissues except adult
brain, spleen, lymph nodes, uterus, and testes.
• Thyroid hormones promote normal physical
growth and development, and are essential for
normal myelination and development of the
nervous system in early life.
• In infants Hypothyroidism causes severe mental
retardation and defective myelination of nerve
fibers.
• Thyroid hormones increase the number and affinity of
beta-adrenergic cardiac receptors for catecholamines, so
increases heart rate, myocardial contractile force, and
cardiac output.
• The metabolic actions of the thyroid hormones are
dependent on its blood level & on the presence of other
hormones, e.g. catecholamines and insulin.
• In normal physiologic amounts, thyroid hormones
stimulate protein synthesis, increase lipid turnover,
lower plasma cholesterol, and promote GI absorption of
glucose.
• T3 is more potent and more rapidly active than T4; in
fact, the latter may be considered a prohormone, since
most target cells convert T4 into T3.
Parathyroid Glands
• These are four in number & embedded in the dorsal surface of
the thyroid gland.
• In response to hypocalcemia (low plasma calcium), it secretes a
single 84- amino-acid polypeptide hormone known as
parathyroid hormone (PTH).
• PTH acts on the Bone so that Calcium & Phosphate levels of
blood increases.
• PTH promotes renal tubular reabsorption of calcium and
increases urinary excretion of phosphate by blocking its
reabsorption.
• PTH also stimulates the activity of a renal enzyme that catalyzes
the formation of calcitriol, an active metabolite of vitamin D
• Calcitriol elevates plasma calcium and phosphate levels primarily
by promoting the intestinal absorption of both ions, & by
increasing renal tubular reabsorption of calcium and phosphate.
The Pancreas
• In pancreas islets of Langerhans (also called pancreatic
islets) are found which are small, highly vascularized
masses of cells scattered throughout the pancreas and
represent only 1% to 3% of the entire organ.
• Islets of Langerhans contain four types of secretary cells:
• Alpha (A) cells, 75%, & secrete glucagon
• Beta (B) cells, 20% & secrete insulin
• Delta (D) cells, 3-5% & secrete somatostatin
• PP (F) cells, 2% & secrete pancreatic polypeptide which
slows food absorption & inhibits the secretion of insulin
& glucagons.
• The paracrine relationship exists within the
pancreatic islets, with one hormone affecting
the secretion of other pancreatic hormones.
Somatostatin inhibits the secretion of insulin,
glucagons, and pancreatic polypeptide.
• Insulin inhibits the secretion of glucagons,
whereas glucagon stimulates the secretion of
insulin and somatostatin.
• 1. Glucagon
• Glucagon is a 29-amino-acid polypeptide
hormone secreted by the alpha cells of the
pancreatic islets primarily in response to
hypoglycemia (low blood sugar).
• Glucagon is essentially a catabolic hormone that
decreases carbohydrate and lipid energy stores
and increases the amount of glucose and fatty
acids available for oxidation.
• Control of Secretion of Glucagon
• The plasma glucose concentration is the major
physiologic regulator of glucagon secretion.
• Glucagons secretion is promoted by
hypoglycemia and fasting, amino acids, exercise,
stress, gastrin, cortisol, CCK, acetylcholine, and
beta-adrenergic stimulation.
• Glucagon secretion is inhibited by elevated
blood levels of glucose, free fatty acids, and by
somatostatin, insulin, secretin, phenytoin, and
alpha-adrenergic stimulation.
• Major Actions
• Carbohydrate metabolism: Glucagon stimulates hepatic
glycogenolysis, thereby promoting the release of glucose
from liver glycogen stores.
• Lipid metabolism: Glucagon stimulates lipolysis, thereby
increasing the release of free fatty acids and glycerol from
adipose tissue. Glucagon also enhances hepatic ketogenesis
by facilitating conversion of fatty acids to ketone bodies.
• Protein metabolism: Glucagon has a catabolic action on
hepatic proteins and inhibits the incorporation of amino
acids into hepatic protein.
• Cardiac effects: large amounts of exogenous glucagon
produce appositive inotropic effect on the heart by
increasing myocardial levels of cyclic AMP.
Insulin
• Structure, Biosynthesis, and Secretion
• Insulin is a polypeptide hormone composed of
51 amino acids.
• Insulin is derived from a precursor-proinsulin
which is synthesized in the endoplasmic
reticulum of beta cells
• Control of Secretion of Insulin
• The secretion of insulin is regulated primarily by the blood
glucose level. An elevation of blood glucose (hyperglycemia),
increases production and release of insulin.
• Ingested glucose effects a far greater secretion of insulin than an
equivalent amount of intravenously glucose because several
gastrointestinal hormones, e.g. gastrin, secretin, CCK, gastric
inhibitory polypeptide (GIP), and glucagons, stimulate insulin
secretion.
• Insulin secretion is also increased by mannose, certain amino
acids, vagal stimulation (acetylcholine), cyclic AMP, beta
adrenergic stimulation, potassium, and oral hypoglycemic drugs
such as tolbutamide.
• Hyperglycemia, somatostatin, alpha-adrenergic stimulation,
thiazide diuretics, phenytoin, and diazoxide inhibit insulin
secretion.
• Actions
• Cellular membrane permeability: Insulin
facilitates the transport of glucose across
selected cell membranes, thereby accelerating
the entry of glucose into muscle, adipose tissue,
fibroblasts, leukocytes, mammary glands,and
the anterior pituitary.
• The transport of glucose into the liver, brain,
renal tubules, intestinal mucosa, and
erythrocytes is independent of insulin.
• Exercise and hypoxia mimic the effect of
insulin on cellular permeability to glucose in
skeletal muscle. The insulin requirements of
diabetics engaging in strenuous exercise may
be reduced substantially and therefore must
be monitored carefully to void hypoglycemia.
• Insulin also increases cellular permeability to
amino acids, fatty acids, and potassium in
muscle and adipose tissue.
• Carbohydrate metabolism: Insulin
lowers the level of blood glucose by
enhancing the transport and peripheral
utilization of glucose.
• Insulin increases muscle and liver
glycogen
• Glycolytic enzymes are also activated by
insulin, & enzymes involved in
gluconeogenesis are inhibited.
• Protein metabolism: Insulin is
strongly anabolic, increases protein
synthesis and inhibits protein
catabolism.
• Lipid metabolism: Insulin stimulates
formation of triglycerides
(lipogenesis) and inhibits their
breakdown (lipolysis).
3. Pancreatic Somatostatin
• Unlike glucagon and insulin, pancreatic
somatostatin does not directly regulate
intermediary metabolism. Rather, it slows
digestion and absorption of nutrients by
exerting several inhibitory effects on digestive
processes (eg, reduced gastric acid secretion
decreased gastric emptying and inhibition of
CCK secretion and gallbladder contraction).
• Pancreatic somatostatin secretion is
stimulated by elevations and gastrointestinal
hormones (eg, CCK).
The Adrenal Glands
• The adrenal (suprarenal) glands are paired yellowish
masses of tissue situated at the superior pole of each
kidney.
• Each gland consists of −an outer adrenal cortex and
an inner adrenal medulla.
• Adrenal Medulla
• The adrenal medulla develops from the embryonic
ectoderm & remains functionally associated with the
sympathetic nervous system, secrete the
catecholamine hormones epinephrine (adrenaline)
and nor-epinephrine (noradrenalin) under control of
Hypothalamus.
• Actions of Adrenal Modullary Hormones
• Epinephrine and nor-epinephrine mimic the effects of
sympathetic nerve discharge, producing the following effects:
• Direct increase in cardiac rate and myocardial force of
contraction
• Dilation of coronary and skeletal muscle blood vessels
• Constriction of the cutaneous and visceral blood vessels.
• Relaxation of respiratory smooth muscle
• Inhibition of GI motility
• Pupillary dilation (mydriasis)
• Glycogenolysis in liver and muscle
• Lipolysis
• Elevation of metabolic rate (calorigenic action), stimulate CNS,
increase alertness, and stimulate respiration.
• Adrenal Cortex
• The adrenal cortex develops from the mesoderm
during embryonic life.
• Adrenal cortex is structurally arranged into three
concentric regions or zones: a thin outer zona
glomerulosa, a thick middle zona fasciculate,
and an inner zona reticularis bordering on the
adrenal medulla.
• Hormones of the adrenal cortex, are steroids -
Adrenocorticoids, & all are derivatives of cholesterol
& are secreted under ACTH control
• Adrenocorticoid hormones are divided into three
groups:
• Mineralocorticoids, such as aldosterone, which
regulate electrolyte and water balance.
• Glucocorticoids, such as cortisol, which affect
carbohydrate, protein, and fat metabolism &
• Adrenogenital steroids or sex hormones : three
types: Androgens (dehydroepiandrosterone),
Estrogens (estradiol), and Progestins (progesterone).
1. Mineralo-corticoids
• Control of Secretion and Actions.
• Aldosterone is the principal physiologic
mineralocorticoid secreted by the zona glomerulosa.
Its secretion is regulated primarily by the renin-
angiotensin mechanism.
• The plasma concentrations of sodium and potassium
are involved in the control of aldosterone secretion.
• Aldosterone plays a major role in the maintenance of
electrolyte and fluid balance by promoting the renal
tubular reabsorption of sodium and the secretion of
potassium and hydrogen ions.
2. Gllucocorticoids
• Control of Secretion and Actions.
• Glucocorticoid secretion, occurs from Zona Fasciculate
of Adrenal Cortex, & is controlled by ACTH, under
stressful conditions e.g. anxiety, fear, hypoglycaemia,
hypotension, and haemorrhage & elevate blood levels
of cortisol (the principal physiologic glucocorticoid).
• Elevated blood levels of free cortisol exert a negative
feedback control over further secretion of ACTH.
• Prolonged ACTH secretion results in hypertrophy and
hyperplasia of the adrenal cortex and excessive
secretion of all Adrenocorticoid hormones.
• The metabolic and physiologic actions of
Glucocorticoids are
• Carbohydrate metabolism: Glucocorticoids
stimulate hepatic gluconeogenesis and inhibit
peripheral uptake and utilization of glucose by
skeletal muscle and adipose tissue, thereby
promoting hyperglycemia.
• Protein metabolism: Glucocorticoids exert
protein catabolic and anti-anabolic actions,
promoting the breakdown of existing proteins
while inhibiting the incorporation of amino acids
into new proteins.
• Lipid metabolism: Glucocorticoids inhibit
lipogenesis and favor mobilization of fats from
adipose tissues. When present in large amounts,
these hormones favor redistribution of adipose
stores by promoting loss of fat from the
extremities, and accumulation of fat depots in
central body regions (e.g., “moon face” and
“buffalo hump” formation).
• Permissive Actions: Clucocorticoids are essential
for normal vascular reactivity to the
catecholamines. Other permissive effects include
support for the metabolic actions (particularly
lipolysis) of the catecholamines and glucagons.
• Blood and immunologic effects: Glucocorticoids
inhibit the immune response, cause involution of
lymphoid tissue, and reduce blood levels of
lymphocytes, eosinophils, and basophils.
These hormones also stimulate erythropoiesis
and elevate circulating levels of platelets and
neutrophils.
• GI tract effects: Glucocorticoid hormones
stimulate gastric acid and pepsin secretion and
inhibit the production of protective mucus,
thereby favouring development of gastric ulcers.
The Sex Glands
• The sex glands, the ovaries in female and testes in male,
not only produce the sex cells but also endocrine organs.
• The hormones produced by these organs are required in
the development of the sexual characteristics, which
usually appear in the early teens and for the
maintenance of the reproductive apparatus once full
development has been attained.
• The main androgen produced by the male sex glands,
testosterone, is responsible for the growth of and
functioning of the male reproductive tract.
• Testosterone is also responsible for male secondary sex
characteristics such as a deep voice and facial hair.
• In the female, the hormones are Estrogens.
• Estrogens contribute to the development of the
female secondary sex characteristics &
functioning of the reproductive organs.
• The other hormone produced by the female sex
glands, called Progesterone, assists in the normal
development of pregnancy.
Thymus Gland
• Thymus gland lies in the upper part of the chest
above the heart.
• Through the production of a hormone called
thymosin, it helps in the development of certain
white blood cells, called ‘T’ Lymphocytes that
help protect the body against foreign organisms.
• This gland is most active before birth and early
in life, it is large during childhood but gradually
shrinks in size as one reach adulthood.
Pineal Gland
• The pineal gland is a small, flattened, cone-
shaped structure located between the two
parts of the thalamus, produces a hormone
called melatonin
• Melatonin, is thought to regulate the release
of certain substances from the hypothalamus,
which may in turn regulate the secretion of
gonadotropins from the pituitary.
• Production of melatonin is regulated by the
amount of light in the environment.
• The secretion of melatonin may influence the
body’s circadian rhythms, the dark-light
fluctuations that affect not only sleepiness and
wakefulness, but also appetite and body
temperature.
• Children have higher melatonin levels than
adults, which may prevent the release of
gonadotropins from the anterior pituitary, so
inhibiting the onset of puberty.
• An antioxidant role of melatonin is under
investigations.
You might also like
- SCIENCE-10-Q3 WORKSHEET REVISED COPY-week-1-7Document46 pagesSCIENCE-10-Q3 WORKSHEET REVISED COPY-week-1-7Gian Evangelista67% (6)
- Boys and Puberty BookletDocument9 pagesBoys and Puberty Bookletఫణీంద్ర నర్సెట్టి50% (2)
- Endocrine SystemDocument96 pagesEndocrine SystemSandhya Kakkar100% (3)
- LECTURE 1 Endocrine Diseases Lecture 1 January 10-020Document68 pagesLECTURE 1 Endocrine Diseases Lecture 1 January 10-020aleen qawareetNo ratings yet
- endocrine فسيولوجياDocument49 pagesendocrine فسيولوجياAUDEH AHMADNo ratings yet
- Endocrine PhysiologyDocument98 pagesEndocrine PhysiologyMohan GuptaNo ratings yet
- ENDOCRINE SYSTEM DISORDERS PROPER BestDocument370 pagesENDOCRINE SYSTEM DISORDERS PROPER BestronaronixstheboyNo ratings yet
- Hormones 080623Document83 pagesHormones 080623Rao Asad MubeenNo ratings yet
- Hypothalamus and Pituitary GlandDocument62 pagesHypothalamus and Pituitary GlandphyMedza AppNo ratings yet
- Endocrinology Endocrinology: H. KibichoDocument370 pagesEndocrinology Endocrinology: H. KibichoMursal RashidNo ratings yet
- CBSE Quick Revision Notes (Class-11 Biology) Chapter-22 Chemical Coordination and IntegrationDocument3 pagesCBSE Quick Revision Notes (Class-11 Biology) Chapter-22 Chemical Coordination and IntegrationNANDAKUMAR BABUNo ratings yet
- CBSE Quick Revision Notes (Class-11 Biology) Chapter-22 Chemical Coordination and IntegrationDocument3 pagesCBSE Quick Revision Notes (Class-11 Biology) Chapter-22 Chemical Coordination and IntegrationNANDAKUMAR BABUNo ratings yet
- Ila College of Health: Endocrine PhysiologyDocument40 pagesIla College of Health: Endocrine PhysiologyDaniel DendaNo ratings yet
- Regulasi Endokrin 22 IntensifDocument25 pagesRegulasi Endokrin 22 IntensifWignes WarenNo ratings yet
- Hormonal BiochemistryDocument82 pagesHormonal BiochemistryRuthNo ratings yet
- Endocrine GlandsDocument36 pagesEndocrine GlandsnasyitahnorzlanNo ratings yet
- Hypothalamus & Pituitary GlandDocument39 pagesHypothalamus & Pituitary GlandVishal DodejaNo ratings yet
- Pituitary and ThyroidDocument54 pagesPituitary and ThyroidSaif AliNo ratings yet
- Endocrine SystemDocument30 pagesEndocrine SystemAkshat RastogiNo ratings yet
- Endocrine System: Endocrine: Which Have No Duct and ReleaseDocument36 pagesEndocrine System: Endocrine: Which Have No Duct and Releasedr_saleh77No ratings yet
- Hormones:: Signaling MoleculesDocument20 pagesHormones:: Signaling MoleculesSangeeta DwivediNo ratings yet
- EndocrineDocument94 pagesEndocrineHira NawazNo ratings yet
- Endo AnaphysioDocument9 pagesEndo AnaphysioShelley Jade MenorNo ratings yet
- Seminor On Hormons Slide2 by Prof - Dr.HariharDocument49 pagesSeminor On Hormons Slide2 by Prof - Dr.Hariharhariharb999_23960100No ratings yet
- HormonesDocument29 pagesHormonesCandy Chieng67% (3)
- Endocrine System - MorphophysiologyDocument88 pagesEndocrine System - MorphophysiologyKarina Bustillo100% (1)
- Metabolic & Endocrine DiseasesDocument280 pagesMetabolic & Endocrine DiseasesHussenNo ratings yet
- Hormones (Short Version)Document80 pagesHormones (Short Version)Vivek ChaudharyNo ratings yet
- HORMONESDocument65 pagesHORMONESsoumya palavalasaNo ratings yet
- Physiology 1STDocument10 pagesPhysiology 1STGW LEGENDNo ratings yet
- Endocrine PhysiologyDocument76 pagesEndocrine Physiologykidusabeje7No ratings yet
- Endocrine Anatomy and PhysiologyDocument10 pagesEndocrine Anatomy and PhysiologyJojo JustoNo ratings yet
- Hypothalamus and Pituitary GlandDocument48 pagesHypothalamus and Pituitary GlandMohsin AbbasNo ratings yet
- Endocrinology Apllied ScienceDocument44 pagesEndocrinology Apllied ScienceAdam PrabowoNo ratings yet
- The Endocrine System The Endocrine System: © 2018 Pearson Education, Ltd. 1Document12 pagesThe Endocrine System The Endocrine System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- Endocrine SystemDocument30 pagesEndocrine SystemBrenda Domaneo BaseNo ratings yet
- Endocrine Physiology For AnsthesiaDocument60 pagesEndocrine Physiology For AnsthesiaCHALIE MEQUNo ratings yet
- The Endocrine System PDFDocument27 pagesThe Endocrine System PDFpratiksha.bhattacharjeeNo ratings yet
- Endocrine SystemDocument22 pagesEndocrine SystemkwatsNo ratings yet
- Endocrine SystemDocument18 pagesEndocrine SystemDioh EmmanuelNo ratings yet
- Chemical Coordination and IntegrationDocument6 pagesChemical Coordination and IntegrationRonaldNo ratings yet
- Endocrine SystemDocument41 pagesEndocrine SystemMerrin EncarnacionNo ratings yet
- The Endocrine System: Endocrine Gland (Ductless Gland)Document50 pagesThe Endocrine System: Endocrine Gland (Ductless Gland)Mohammad AliNo ratings yet
- Quick Revision NotesDocument3 pagesQuick Revision NoteslinzihaoleoNo ratings yet
- Chemical Coordination and Integration Handwriten Notes For Neet and JeeDocument5 pagesChemical Coordination and Integration Handwriten Notes For Neet and JeetechnosonicindiaNo ratings yet
- PD22 Hap1 L03Document33 pagesPD22 Hap1 L03Ka Yan LAUNo ratings yet
- EndocrinologyDocument74 pagesEndocrinologysyedahaleemajunaidsNo ratings yet
- Biochemistry of Hormones (Part 1)Document31 pagesBiochemistry of Hormones (Part 1)arun231187100% (1)
- Endocrine System/socialDocument33 pagesEndocrine System/socialrpant3165No ratings yet
- Option D - Unit 5 - HormonesDocument28 pagesOption D - Unit 5 - Hormonesjanafahmy1211No ratings yet
- Unit IXDocument10 pagesUnit IXPreeti ChouhanNo ratings yet
- Anatomy and Physiology of The Endocrine System: Presenté ParDocument64 pagesAnatomy and Physiology of The Endocrine System: Presenté ParYackson Frank100% (1)
- UntitledDocument12 pagesUntitledDerrick kinyaNo ratings yet
- Endocrine System: Glands & HormonesDocument78 pagesEndocrine System: Glands & HormonesJerilee SoCute WattsNo ratings yet
- 4 Pituitary HormonesDocument18 pages4 Pituitary HormonesRana AbdullahNo ratings yet
- Functional Anatomy and PhysiologyDocument38 pagesFunctional Anatomy and PhysiologyNawalNo ratings yet
- EndocrinologyDocument37 pagesEndocrinologyKochaMsangiNo ratings yet
- Hormones: Mark Angelo R. Jacosalem Faye Bernadette O. Reyes Ma. Elizabeth VerteraDocument40 pagesHormones: Mark Angelo R. Jacosalem Faye Bernadette O. Reyes Ma. Elizabeth VerteraGelo Robin JacosalemNo ratings yet
- Principles of Hormonal Control SystemDocument25 pagesPrinciples of Hormonal Control SystemFAHEEM UD DINNo ratings yet
- Hormones SubtopicsDocument77 pagesHormones SubtopicsSulaiman UmraniNo ratings yet
- Balancing Hormones Naturally: A Woman's Guide to Hormonal Harmony: HealthFrom EverandBalancing Hormones Naturally: A Woman's Guide to Hormonal Harmony: HealthNo ratings yet
- Thyroid Health: The Thyroid Solution Diet ExposedFrom EverandThyroid Health: The Thyroid Solution Diet ExposedRating: 3 out of 5 stars3/5 (2)
- Nervous SystemDocument140 pagesNervous SystemDivya JaiswalNo ratings yet
- 1 General Anatomy - Levels of Organization EtcDocument36 pages1 General Anatomy - Levels of Organization EtcDivya JaiswalNo ratings yet
- General Anatomy - 4Document22 pagesGeneral Anatomy - 4Divya JaiswalNo ratings yet
- 6 Human Anatomy - Muscular SystemDocument34 pages6 Human Anatomy - Muscular SystemDivya JaiswalNo ratings yet
- Acute Interstitial NephritisDocument36 pagesAcute Interstitial NephritisosaqerNo ratings yet
- CHOLECYSTITIS CASE STUDY Version 2.0Document57 pagesCHOLECYSTITIS CASE STUDY Version 2.0Gabriel Arch100% (1)
- Cara Membaca Foto Thoraks Yang BaikDocument2 pagesCara Membaca Foto Thoraks Yang BaikIdi Nagan RayaNo ratings yet
- IBDP Biology Option - D - SummaryDocument5 pagesIBDP Biology Option - D - SummaryRafi FarhanNo ratings yet
- Case Pres HydronephrosisDocument39 pagesCase Pres HydronephrosisLouie Dela Cruz100% (3)
- Review Article: Relevant Biliary Anatomy During CholecystectomyDocument11 pagesReview Article: Relevant Biliary Anatomy During CholecystectomyAbrar SabawiNo ratings yet
- PHPY 303 - GI Lecture #1 - March 10Document30 pagesPHPY 303 - GI Lecture #1 - March 10smhallmobileNo ratings yet
- General Surgery: (Gallbladder Disease)Document1 pageGeneral Surgery: (Gallbladder Disease)Matt100% (1)
- PHYSIOLOGYDocument10 pagesPHYSIOLOGYapi-1986354875% (4)
- Chapter 13 - The Peripheral Nervous System and Reflex ActivityDocument53 pagesChapter 13 - The Peripheral Nervous System and Reflex Activityramadan100% (1)
- Science 8 - 3Document5 pagesScience 8 - 3Sherine Marianne IgnacioNo ratings yet
- Jurnal 2 (2019)Document11 pagesJurnal 2 (2019)Inryuu ZenNo ratings yet
- Mod 8 ZooDocument10 pagesMod 8 ZooLM Tricia T. DE LA CRUZNo ratings yet
- B - SC Nursing I Year SyllabusDocument159 pagesB - SC Nursing I Year SyllabusSusheelabaiNo ratings yet
- Heart, Nerve and Mucsle, Membrane Transport Mcqs With KeyDocument8 pagesHeart, Nerve and Mucsle, Membrane Transport Mcqs With KeyMudassar Roomi100% (7)
- Brain Computer InterfaceDocument11 pagesBrain Computer InterfaceNeha ArifNo ratings yet
- Acute GlomerulonephritisDocument18 pagesAcute GlomerulonephritisdanielaNo ratings yet
- Anatomia de Puntos Craneometricos PDFDocument35 pagesAnatomia de Puntos Craneometricos PDFAlberto SalazarNo ratings yet
- Chapter 39 AntihypertensivesDocument4 pagesChapter 39 AntihypertensivesErika Joy Cabison TamayoNo ratings yet
- Benign Thyroid DiseasesDocument138 pagesBenign Thyroid DiseasesAliNo ratings yet
- 07 Post Mortem Examination (Autopsy)Document48 pages07 Post Mortem Examination (Autopsy)ARIF-UR-REHMAN100% (5)
- Previous Year'S Questions (Excretion)Document1 pagePrevious Year'S Questions (Excretion)veeresh punjaniNo ratings yet
- Digestive System in Non-RuminantsDocument5 pagesDigestive System in Non-RuminantsTumisang TlhabanoNo ratings yet
- Bikram Yoga PosturesDocument4 pagesBikram Yoga PosturesMony SánchezNo ratings yet
- Science6 ST1 Q2Document4 pagesScience6 ST1 Q2Meriam LuatNo ratings yet
- Chapter 10 - Immune Responses Against Tumors and TransplantsDocument11 pagesChapter 10 - Immune Responses Against Tumors and TransplantsFYMNo ratings yet
- Li 1 Anatomy, Histology, PhysiologyDocument17 pagesLi 1 Anatomy, Histology, PhysiologysandyaadindaNo ratings yet
- Lipids Metabolism ReviewerDocument2 pagesLipids Metabolism RevieweroperanacireNo ratings yet