Professional Documents
Culture Documents
Disorders of The Immune System
Disorders of The Immune System
Uploaded by
RICHARD MOSSES0 ratings0% found this document useful (0 votes)
21 views56 pagesThe document discusses disorders of the immune system, including four main categories: autoimmunity, primary immunodeficiencies, acquired immunodeficiencies, and hypersensitivity. It focuses on autoimmune diseases and immunodeficiencies. Autoimmune diseases occur when the immune system attacks the body's own tissues. Immunodeficiencies involve impaired immune function, either from birth (primary) or due to external factors (secondary). Common causes of secondary immunodeficiencies include malnutrition, HIV/AIDS, and medications like chemotherapy.
Original Description:
Original Title
Untitled
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses disorders of the immune system, including four main categories: autoimmunity, primary immunodeficiencies, acquired immunodeficiencies, and hypersensitivity. It focuses on autoimmune diseases and immunodeficiencies. Autoimmune diseases occur when the immune system attacks the body's own tissues. Immunodeficiencies involve impaired immune function, either from birth (primary) or due to external factors (secondary). Common causes of secondary immunodeficiencies include malnutrition, HIV/AIDS, and medications like chemotherapy.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
21 views56 pagesDisorders of The Immune System
Disorders of The Immune System
Uploaded by
RICHARD MOSSESThe document discusses disorders of the immune system, including four main categories: autoimmunity, primary immunodeficiencies, acquired immunodeficiencies, and hypersensitivity. It focuses on autoimmune diseases and immunodeficiencies. Autoimmune diseases occur when the immune system attacks the body's own tissues. Immunodeficiencies involve impaired immune function, either from birth (primary) or due to external factors (secondary). Common causes of secondary immunodeficiencies include malnutrition, HIV/AIDS, and medications like chemotherapy.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 56
Disorders of the immune system
What can go wrong with your immune system?
There are grossly FOUR bad situations.
i) An immune system that turns against its own self
aka autoimmunity
ii) Being born with a weak immune system (aka
primary immunodeficiency-PID).
iii) Suffering a disease/process/event that weakens the
immune system (aka. acquired immunodeficiency).
iv) Have an immune system that is over active (aka.
Hypersensitivity ...)
1. Autoimmune disease
• An autoimmune disease (AD) is a condition arising
from an abnormal immune response to a normal body
part were the immune system attacks ones body
instead of protecting it
• It's unclear why autoimmune diseases occur but
there are at least 80 types of autoimmune diseases
which can involve any body part
• Symptoms of AD are nonspecific, diverse and the
symptoms are often recurrent i.e come and go.
• Autoimmune diseases can affect many types of
tissues and nearly any organ in your body
• They are associated with a variety of symptoms
including pain, tiredness (fatigue), rashes, nausea,
headaches, dizziness and more.
• Specific symptoms depend on the exact disease and
affected organ/tissue.
• “Experts don’t know why your immune system
turns on you. It is like it can no longer tell the
difference between self and what is not —
between what’s you and what’s an invader.
There are some theories about why this
happens, but experts aren’t quite sure why”
• Many ADs, eg. ulcerative colitis, are heritable
(genetic), quite common and can affect any
part/system of the body eg. skin, digestive,
reproductive, neural, joints and muscles, endocrine
systems.
• They affect at least 10% of the population,
predominantly women
• They are non communicable but can be fatal especially
in persons above 60 years
• Some ADs can affect conception and pregnancy and
one may require fertility treatments to conceive and
maintain pregnancy.
• For example, there is a higher risk for stillbirth or
preterm birth in females with an AD disease called
lupus erythomatosis.
Factors that may predispose autoimmune
disease
These include:
• Genetical: Some diseases run in families
• Some medications.
• Certain Infections
• Exposure to toxins.
• Being female — 78% of people who have an
autoimmune disease are natural women.
• Foods/feeding (eg obesity) .
Symptoms of autoimmune diseases
• Variable and depend on the disease and part of body
affected
Disease Symptoms
Organ/part affected
Diseases of the joints and muscles Muscle aches and pains.
Joint pain, stiffness and swelling.
Muscle weakness.
Diseases of the digestive tract: Bloating.
Constipation.
Acid reflux.
Nausea.
Food sensitivities.
Diseases of the skin Rashes, Itching, Dry eyes.
Hair loss, Dry skin
Diseases of the Dizziness. Headaches.
nervous system: Anxiety and depression.
Diagnosis of autoimmune diseases
It is a lengthy procedure and requires:
i) A detailed list of any symptoms and duration - how
long you’ve had them.
ii) A record of your family’s health history. Eg family
member with an autoimmune disease record.
iii) Analysis of symptoms, some blood tests eg.
• Antinuclear antibody test (ANA).
• Complete blood count (CBC).
• Erythrocyte sedimentation rate (ESR)
Examples of AD related/associated conditions
• Lupus
• Scleroderma
• Certain types of hemolytic anemia
• Vasculitis
• Type 1 diabetes (diabetes mellitus)
• Rheumatoid arthritis (aka Rheumatism)
• Multiple sclerosis)
• Some types of myopathy
• Alopecia
• TB, Leprosy, angina pectoris (myocarditis)
• Eg: 1)Rheumatoid arthritis (RA) is a long-term
autoimmune disorder that primarily affects
joints. It typically results in warm, swollen,
painful joints and deformity
• 2) Advanced stage leprosy
Rheumatoid arthritis
Le
Leprosy autoimune reaction leading to deformity of limbs grade 2
deformity ( D2G)
Treatment of autoimmune diseases
• There are no specific treatment regimes for
autoimmune diseases, therefore management is
done symptomatically
• Given that individuals’ immune system, genetics and
living environment are different, the treatment of
autoimmune diseases will also be unique.
• Most common treatments include:
• Painkillers, anti-inflammatories and
corticosteroids
• Alternative (traditional) medicines (herbs…
acupuncture have also been used
2. Immunodeficiencies
• Immunodeficiency, also known as
immunocompromisation, is a state in which
the immune system's ability to fight infectious
diseases and cancer cells is impaired
• There are two types of immunodeficiency disorders:
those a person is born with (ie primary aka innate),
and those that are acquired (secondary).
• Extrinsic factors can adversely (weakens) body’s
immune responses, producing states of secondary
immunodeficiency and consequent increased risk of
infections
• These immunodeficiencies can be encountered in
routine clinical practice and can arise from a
number of conditions eg.
i) Prolonged treatment with glucocorticoids and
immunomodulatory drugs
ii) Trauma and surgery
iii) Extremely stressful environmental conditions
iv) Chronic infections, such as those caused by
HIV.
2.1 Primary Immunodefficiency
Clinical manifestations of PIDs are highly variable
should be suspected in patients with:
i) Frequent recurrent sinus or ear infections or
ii) Repeated pneumonias within a 1 year period
iii) Failure to thrive (stunting, wasting)
iv) Poor response to prolonged use of antibiotics
v) Persistent thrush or skin abscesses;
vi) a family history of PID
• The treatment of PIDs is complex and
generally requires both supportive and
definitive strategies
• Ig replacement therapy is the most effective
therapy for B-cell disorders, as well as for
patients with combined immunodeficiency ( B
& T cell deficiencies), aka CID
• For disorders involving the T-cell arm of the
adaptive immune system, such as severe
combined immunodeficiency (SCID),
immediate immune reconstitution is required
supported with antibiotics and antifungals
• In worse cases vaccinations and bone marrow
transplantation may be employed.
2.2 Secondary immunodeficiencies (SID)
• Secondary immunodeficiency (SID) is said to occur
when the immune system is weakened by a
treatment or illness.
• Most common causes are:
- Disorders of blood due to bone marrow
malfunction (Leukemia),
- Drugs (medicines) for cancer treatment eg.
chemotherapy
- Immune-complex diseases, like viral
hepatitis and diabetes mellitus
- Severe burns
• Perhaps the most well known SID secondary
caused by HIV infection
• However, the most prevalent cause of
immunodeficiency worldwide is severe
malnutrition, which affects as many as 50% of
the population in many impoverished
communities.
• The immune defects observed in SID are usually
variable in their clinical presentation, and their
prognosis depends on the severity of the immune
defect.
• Management of the PIDs often results in
improvement of the immunodeficiency;
• However, this is sometimes not possible, and the risk
of infections must be reduced with prompt
antimicrobial treatment and prophylaxis
• The restoration of immunity in SIDs is
generally achieved with the management of
the primary condition eg good nutrition or
the removal or attenuation of the offending
agent eg. suppressing HIV by using ART.
MALNUTRITION
• Worldwide, protein-calorie malnutrition is the
most common cause of immunodeficiency.
• Malnutrition can result from limited access to
food sources, eating habits and chronic
diseases that induce cachexia, such as
neoplastic (cancerous) diseases.
• Diarrhea caused by infections and respiratory
tract infections are common in such
communities.
• T-cell production and function decrease in
proportion to the severity of hypoproteinemia;
• Although , specific antibody titers and immune
responses to vaccines can be detected in a
malnourished subject for a prolonged period.
• Eventually, these immune responses decrease
too if malnutrition persists.
• The deficiency of micronutrients (eg, zinc and
ascorbic acid) contributes to increased
susceptibility to infections through the
weakening of skin and mucosa barriers, which
facilitates a pathogen invasiveness.
• Vitamin D appears to be necessary in the
macrophage activity against intracellular
pathogens, remarkably Mycobacterium
tuberculosis
• Correction of the nutritional deficiencies often
results in the resolution of these immunologic
defects.
HIV
• HIV is transmitted sexually, for the most part,
but it is also transmitted parenterally among
intravenous drug users and vertically from
mothers to their infants
• Initially recognized during the early 1980s in a
handful of cases, it is currently estimated that
more than million persons are infected with
HIV worldwide.
• Two thirds of HIV subjects are living in the sub-
Saharan region of Africa, and approximately half of
them are women and childr
• Significant reduction of HIV related diseases has
been achieved in the past two decades thanks to
antiretroviral use
• However, there is an increasing number of reports of
viral multidrug resistance and clinical complications
caused by the chronic use of antiretroviral drugs.
HIV infection process
The HIV uses CD4 cell receptors on the surface of the T-
helper (Th) lymphocyte gain entry into this important
immune regulator cell
-The virus achieves this through its viral
envelope protein known as gp120
- T helper cells (Th) are lymphocytes that are
an essential part of the human immune system.
- They are commonly referred to as CD4+ cells, or T4
because of the specific type of peptide molecules
constituting it.
CD means Cluster of differentiation, and there are over 300
such clusters on different cells of animals and humans
• They are called helper cells because one of
their main roles is to send signals to other
types of immune cells, including CD8, aka
cytotoxic killer cells, which specifically destroy
cells infected with intracellular pathogens.
• CD4+ is indeed a co-receptor on the
T cell receptor (TCR) surface and
assists the latter in communicating with
antigen-presenting cells in normal health
situations
• The TCR-CD4 complex bind to distinct regions
of the antigen-presenting cells
• HIV then inserts a fusion peptide into the Th cell that
allows the outer membrane of the virus to fuse with
the cell membrane
• Gradually it transduces the CD4+Tcell into producing
more of HIV particles and later cell dies while more
HIV particles are released to continue with the
cascade
• HIV infection leads to a progressive reduction in the
number of T cells expressing CD4+ in the lymphatic
system
• Ultimately the entire cell mediated arm of immune
defense becomes impaired
• Consequently, the body becomes weakened and more
vulnerable to pathogens, including high rise of
opportunistic infections
• HIV infection can be suppressed by use of
antiretroviral (ARV) drugs
• To monitor infection status medical
professionals refer to the CD4+ cell count to
appreciate the level of severity of disease for
inception of ARV use during HIV infection,
• Recent WHO guidelines require
treatment at all HIV victims, regardless the
CD4+ count soonest if HIV is diagnosed
• A CD4+ count merely indicate the number of
T cells expressing CD4+ but are not a direct
HIV test—e.g. they do not check the presence
of viral DNA load.
3 Hypersensitivity
• Hypersensitivity reaction or intolerance) refers
to undesirable reactions by the normal immune
system
• It is the third major disorder of the immune
system, also referred to as an overreaction of
the immume mechanism
• Hypersensitivity may cause a severe discomfort
to an individual and in some cases serious
impairment and even death
Types of Hypersensitivity
There a four types (i-iv) of hypersensitivity
Type I hypersensitivity
• Type I hypersensitivity occurs as a result of
exposure of an antigen to the immune
system after which two stages of events occur,
namely sensitization and the effect stages.
• In the "sensitization" stage, the
host experiences an asymptomatic reaction to
the antigen.
• In a subsequent re-encounter with the antigen , ie in
the "effect" period, the sensitized host over reacts
to the antigen
• This over-reaction is also referred to as type 1
anaphylactic, atopic or allergic immune response.
Triggers of Hypersensitivity Type I include:
• Foods products: nuts, eggs,
soy, wheat, shellfish…,
• Animal/insect sources: bee, wasp, hairs of
cats, rats,
• Environmental factors: dust mites, latex,
pollen, molds, etc.
Immune responses include:
• Allergic asthma, allergic rhinitis, conjunctivitis,
dermatitis, etc.
• Medication-associated allergic reactions vs
antibiotics, sulphonamides
Type II hypersensitivity
Type II hypersensitivity reaction is also referred to as
antibody-mediated immune reaction
• In this type, antibodies (IgG or IgM) are directed
against “self” cellular or extracellular antigens with
the resultant “self”cellular destruction, functional
loss, or damage to tissues.
• Damage can be accomplished via three
different mechanisms:
i) Antibody binding to cell surface receptors and
altering cellular activity
ii) Activation of the complement pathway ending
with MAC.
ii) Antibody-dependent cellular cytotoxicity.
Type III hypersensitivity
• In type III hypersensitivity reaction, an abnormal
immune response is mediated by the formation
of Ag-Ab aggregates (aka "immune
complexes)".
• These complexes then precipitate in various
tissues such as skin, joints, vessels, or glomeruli,
and trigger the classical complement pathway.
• Complement activation leads to the recruitment of
inflammatory cells (monocytes and neutrophils) that
release lysosomal enzymes and free radicals eg (O-)at
the site of immune complexes, causing tissue damage.
• The most common diseases involving a type III
hypersensitivity reaction include: serum sickness,
post-streptococcal glomerulonephritis, post
streptococcal pericarditis (angina pectoris),’
hypersensitivity pneumonitis, and rheumatoid
arthritis.
• The principal feature that distingishes type III
reactions from other hypersensitivity reactions is that
in type III reaction, the antigen-antibody complexes
are pre-formed in the circulation before their
deposition in tissues.
Type IV hypersensitivity
• Type IV hypersensitivity reactions are, to some
extent, “normal” physiological events that help
fight infections, and dysfunction in this system can
predispose to multiple opportunistic infections.
• Adverse events can also occur due to these
reactions when an undesirable interaction between
the immune system and an allergen happens.
See summary Figure 2 (nxt slide)
Rheumatoid arthritis
Management of Immediate hypersensitivity reactions
• The treatment of reactions may include:
(i) Treatment of anaphylaxis with intramuscular
epinephrine and antihistamine
(iii)Sustaining blood pressure with fluids,
(iv)Avoiding latex materials (eg gloves) if
handling who are allergic to rubber
(v) Surgical procedures such as tracheotomy in
case of severe laryngeal edema.
Allergic bronchial asthma can be treated with any of
the following:
• Inhalation of short- and long-acting bronchodilators
(anticholinergics and corticosteroids)
• Maintaining allergen (dust, hairs, polen..) free
environmental control to avoid contact with allergens
as much as possible.
• Use of anti-IgE antibody where available .
Treatment of delayed hypersensitivity (iv)reactions
• It involves the treatment of the eliciting cause
eg: The most common drugs to treat tuberculosis
include isoniazid, rifampin, ethambutol.
For drug-resistant TB, a combination of antibiotics such
as amikacin and kanamycin, should be used.
• The most common drugs to treat
multibacillary leprosy include rifampicin and
clofazimine in combination with dapsone for
leprosy.
• A single dose of antimicrobial combination to
cure single lesion paucibacillary leprosy
comprises ofloxacin, rifampicin, and
minocycline.
• Praziquantel can be useful for treating
infections caused by all Schistosoma spp
• Hydroxychloroquine and chloroquine can be
use in the therapy of sarcoidosis involving the
skin, lungs, and the nervous system.
You might also like
- Nursing Care Plan - ConstipationDocument2 pagesNursing Care Plan - Constipationderic86% (72)
- Pharmacology Case Study2.11.14Document3 pagesPharmacology Case Study2.11.14NickCiardielloNo ratings yet
- Spinal Cord InjuryDocument35 pagesSpinal Cord InjuryRhOmadona GenzoneNo ratings yet
- ATI Bible 1Document205 pagesATI Bible 1jeanmcqueen767698% (40)
- Biology Project For Class 12Document21 pagesBiology Project For Class 12kishore kolanjiNo ratings yet
- Autoimmune Disorders: DR Muhammad ZUBAIR Consultant Chemical PathologistDocument52 pagesAutoimmune Disorders: DR Muhammad ZUBAIR Consultant Chemical PathologistZubair YousafNo ratings yet
- Disorders and Diseases of Immune SystemDocument21 pagesDisorders and Diseases of Immune SystemWijesiri D WNo ratings yet
- PDF DocumentDocument63 pagesPDF Documentfakeye kayodeNo ratings yet
- Immunodeficiency Disorder: Supervisor: Dr. Rebar Mohammed Name Student: Nazo Rashid AliDocument12 pagesImmunodeficiency Disorder: Supervisor: Dr. Rebar Mohammed Name Student: Nazo Rashid Alinazo rashid aliNo ratings yet
- Autoimmune DiseasesDocument70 pagesAutoimmune DiseasesAdebisi OluwatomiwaNo ratings yet
- Immunodeficiency DiseasesDocument5 pagesImmunodeficiency DiseasesOghenetega RamsonNo ratings yet
- Chapter 4Document30 pagesChapter 4Noriani ZakariaNo ratings yet
- Autoimmune Diseases CompletedDocument21 pagesAutoimmune Diseases Completedapi-568740587No ratings yet
- Hiv/AidsDocument6 pagesHiv/Aidsampogison08No ratings yet
- Immune DisorderDocument37 pagesImmune DisorderJessica TieuNo ratings yet
- Sepsis and Diabetes MellitusDocument20 pagesSepsis and Diabetes MellitusOlga GoryachevaNo ratings yet
- Document 22Document3 pagesDocument 22nicolasdanica018No ratings yet
- Health and DieseassDocument41 pagesHealth and Dieseassxwylav1No ratings yet
- Autoimmune Diseases: Clinical NutritionDocument39 pagesAutoimmune Diseases: Clinical NutritionRachael TheisenNo ratings yet
- CHAPTER 6 Infection and DiseasesDocument17 pagesCHAPTER 6 Infection and DiseasesDanica DaniotNo ratings yet
- Anglais 3Document2 pagesAnglais 3Afdal BiosicaNo ratings yet
- Health: Quarter 4 - Module 7: Prevention and Control of Diseases and DisorderDocument7 pagesHealth: Quarter 4 - Module 7: Prevention and Control of Diseases and DisorderRico Alinsunurin Fajardo0% (1)
- Why Do We Fall Ill NotesDocument6 pagesWhy Do We Fall Ill NotessrianshNo ratings yet
- Immuno Lec 1&2&3Document33 pagesImmuno Lec 1&2&3Ali AlhamdaniNo ratings yet
- Immune DisordersDocument43 pagesImmune Disorderssivagurunathan.P75% (4)
- EpidemicDocument60 pagesEpidemickya ho agarNo ratings yet
- Diseases of Immune System Part 2Document47 pagesDiseases of Immune System Part 2KundaNo ratings yet
- AIDSDocument33 pagesAIDSs2021244080No ratings yet
- 6246bb700cf2ee69840e3596 OriginalDocument24 pages6246bb700cf2ee69840e3596 Originalsoma5koshasNo ratings yet
- Autoimmune DiseaseDocument15 pagesAutoimmune DiseaseSebastian GhermanNo ratings yet
- Immunologic Agents PDFDocument104 pagesImmunologic Agents PDFgherlethrNo ratings yet
- Medical BiotechnologyDocument135 pagesMedical BiotechnologyrahelNo ratings yet
- Activity 14 Understanding Immune SystemDocument20 pagesActivity 14 Understanding Immune SystemKendrix Aguiluz FlorendoNo ratings yet
- ASCIA PCC Autoimmune Diseases 2019Document2 pagesASCIA PCC Autoimmune Diseases 2019Hamza ziaNo ratings yet
- Activity 14Document4 pagesActivity 14acrehell8No ratings yet
- Autoimmune Disease: Duhok Polytechnic University Duhok Technical Institute Department of PharmacyDocument17 pagesAutoimmune Disease: Duhok Polytechnic University Duhok Technical Institute Department of PharmacyRasheed AliNo ratings yet
- 4TH Quarter in HealthDocument1 page4TH Quarter in HealthAlexis AguilarNo ratings yet
- Nursing Care SLEDocument26 pagesNursing Care SLEIsabela SintyaNo ratings yet
- Disorder of The Immune System 2Document58 pagesDisorder of The Immune System 2Daniel OkakaNo ratings yet
- Aids FinalDocument7 pagesAids Finalscarletbullet0820No ratings yet
- Immune FinalDocument53 pagesImmune FinalJaylord VerazonNo ratings yet
- BIO 100 Discoveries in Biology Lecture:09 Autoimmune DisordersDocument29 pagesBIO 100 Discoveries in Biology Lecture:09 Autoimmune DisordersIsmail Hossen RajuNo ratings yet
- Autoimmune DiseasesDocument14 pagesAutoimmune Diseasesdr_swaralipiNo ratings yet
- Lo PlenoDocument100 pagesLo PlenoBilqis ElfariantiNo ratings yet
- Summary of Mod 5-7 ClassesDocument4 pagesSummary of Mod 5-7 ClassesKayden KrajcarNo ratings yet
- Can Be Made Immunogenic by Conjugation To A Suitable CarrierDocument14 pagesCan Be Made Immunogenic by Conjugation To A Suitable CarrierAnmol KumarNo ratings yet
- Disease Process HIVDocument4 pagesDisease Process HIValeksdj1987No ratings yet
- Prevention and Control of Diseases and DisordersDocument17 pagesPrevention and Control of Diseases and DisordersCarissa Asuan-MorenoNo ratings yet
- Understanding Autoimmune Disease PDFDocument18 pagesUnderstanding Autoimmune Disease PDFLiz TaylorNo ratings yet
- Systemic Lupus ErythematousDocument8 pagesSystemic Lupus ErythematousampalNo ratings yet
- HEA 101 Lecture # 2 Section # 2Document33 pagesHEA 101 Lecture # 2 Section # 2mahfuzNo ratings yet
- Kelompok 1: Oleh: David Septra Fifi Fitri Yanti Herlinda Oktavia Vinta Yolanda ReskiDocument9 pagesKelompok 1: Oleh: David Septra Fifi Fitri Yanti Herlinda Oktavia Vinta Yolanda ReskiFifi Fitri YantiNo ratings yet
- Auto-Immune DiseasesDocument10 pagesAuto-Immune Diseasesjaisri nandhiniNo ratings yet
- Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS)Document28 pagesHuman Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS)AbirajanNo ratings yet
- 7 - Aging and Immune system-FEDocument26 pages7 - Aging and Immune system-FE20154712No ratings yet
- Immune Disorders..Ppt FairDocument79 pagesImmune Disorders..Ppt FairSumi SebastianNo ratings yet
- Autoimun MekanismeDocument22 pagesAutoimun MekanismeMeity ElvinaNo ratings yet
- Borrel Ios IsDocument20 pagesBorrel Ios IsRohan TejaNo ratings yet
- Lect.12 - Immunologic and Endocrine Alterations in ChildrenDocument61 pagesLect.12 - Immunologic and Endocrine Alterations in ChildrenlouradelNo ratings yet
- Non Communicable Disease Grade 7Document4 pagesNon Communicable Disease Grade 7Joshua RamirezNo ratings yet
- Auto Immune DiseasesDocument18 pagesAuto Immune DiseasesNareshNo ratings yet
- Systemic Lupus Erythematosus: Medical Surgical and Critical Care DepartmentDocument31 pagesSystemic Lupus Erythematosus: Medical Surgical and Critical Care DepartmentLalisaM ActivityNo ratings yet
- Systemic Lupus Erythematosus: Medical Surgical and Critical Care DepartmentDocument31 pagesSystemic Lupus Erythematosus: Medical Surgical and Critical Care DepartmentLalisaM ActivityNo ratings yet
- Drug ComplianceDocument5 pagesDrug Complianceratriii02No ratings yet
- Helminth 4Document1 pageHelminth 4FarlogyNo ratings yet
- Drug Study On CARBOPROSTDocument4 pagesDrug Study On CARBOPROSTshadow gonzalez100% (1)
- Endocrinology, Diabetes, and Metabolism - American Board of Internal Medicine - ABIMDocument3 pagesEndocrinology, Diabetes, and Metabolism - American Board of Internal Medicine - ABIMabimorgNo ratings yet
- CardiologistDocument72 pagesCardiologistArun Talluri100% (1)
- Bipolar DisorderDocument83 pagesBipolar DisorderEko PriyantoNo ratings yet
- StrabismusDocument30 pagesStrabismusEjay Jacob Ricamara100% (1)
- Psychogenic VoiceDocument11 pagesPsychogenic VoiceAna MoraisNo ratings yet
- Application Form Residency & PostRes 2022Document2 pagesApplication Form Residency & PostRes 2022Franz LibreNo ratings yet
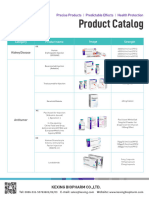
- 02-Kexing Product Catalogue (Index)Document2 pages02-Kexing Product Catalogue (Index)londonpharmauzNo ratings yet
- Schizophrenic Survey Quick Quiz AnswersDocument3 pagesSchizophrenic Survey Quick Quiz Answersapi-242882478No ratings yet
- Invitation ReportDocument11 pagesInvitation ReportTyro ClubNo ratings yet
- Awareness of Radiologic Technology As A CareerDocument19 pagesAwareness of Radiologic Technology As A CareerAnderson OrtegaNo ratings yet
- 7 Things You Should Know About Egg DonationDocument4 pages7 Things You Should Know About Egg DonationNini LekishviliNo ratings yet
- Cyclamen: Chilly PulsatillaDocument10 pagesCyclamen: Chilly Pulsatillaअनुरूपम स्वामीNo ratings yet
- EnglezaDocument8 pagesEnglezaAndreea Cosmina GrigoreNo ratings yet
- Emnc 4 North Drug StudyDocument12 pagesEmnc 4 North Drug StudyFrancesca Aurea MagumunNo ratings yet
- Hba1C Direct With Calibrator: 30 Days at 2-8°C. Do Not FreezeDocument2 pagesHba1C Direct With Calibrator: 30 Days at 2-8°C. Do Not FreezeSanjay KumarNo ratings yet
- Chap1 Eks 2ed AddendumDocument19 pagesChap1 Eks 2ed AddendumCamroc BraineryNo ratings yet
- Botulism EpiDocument26 pagesBotulism EpiMaria PavlovaNo ratings yet
- Median Lethal Dose (LD)Document4 pagesMedian Lethal Dose (LD)Christian ConsignaNo ratings yet
- Cholangiocarcinoma: (Klatskin Tumour)Document24 pagesCholangiocarcinoma: (Klatskin Tumour)trlNo ratings yet
- Pregnancy 1Document12 pagesPregnancy 1Toni FauziNo ratings yet
- Preoperative Care of The Patient Undergoing Orthopedic SurgeryDocument26 pagesPreoperative Care of The Patient Undergoing Orthopedic SurgeryAbdul Gafoor CPNo ratings yet
- Psych HESI Hints: Members For The Client's Safety (E.g., Suicide Plan) and Optimal TherapyDocument7 pagesPsych HESI Hints: Members For The Client's Safety (E.g., Suicide Plan) and Optimal TherapyChristina100% (10)
- History What Is STI? BackgroundDocument4 pagesHistory What Is STI? BackgroundAko Si LibroNo ratings yet