Professional Documents
Culture Documents
Croup and Epiglottitis 2011
Croup and Epiglottitis 2011
Uploaded by
Minutes in MEDITATION0 ratings0% found this document useful (0 votes)
0 views25 pagesThe document discusses Croup and Epiglottitis. Croup is most common in children ages 2 and causes barking cough and stridor. It is usually caused by parainfluenza virus. Treatment includes humidity and racemic epinephrine. Epiglottitis involves bacterial infection of the epiglottis and is most common in children ages 2-7. It causes difficulty swallowing and sore throat. Immediate intubation may be needed to secure the airway.
Original Description:
Pediatric disorders
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses Croup and Epiglottitis. Croup is most common in children ages 2 and causes barking cough and stridor. It is usually caused by parainfluenza virus. Treatment includes humidity and racemic epinephrine. Epiglottitis involves bacterial infection of the epiglottis and is most common in children ages 2-7. It causes difficulty swallowing and sore throat. Immediate intubation may be needed to secure the airway.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
0 views25 pagesCroup and Epiglottitis 2011
Croup and Epiglottitis 2011
Uploaded by
Minutes in MEDITATIONThe document discusses Croup and Epiglottitis. Croup is most common in children ages 2 and causes barking cough and stridor. It is usually caused by parainfluenza virus. Treatment includes humidity and racemic epinephrine. Epiglottitis involves bacterial infection of the epiglottis and is most common in children ages 2-7. It causes difficulty swallowing and sore throat. Immediate intubation may be needed to secure the airway.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 25
Croup and Epiglottitis
Arthur B. Marshak, EdD, MS, RRT, RPFT
Cardiopulmonary Sciences
Loma Linda University
Objectives
Following the lecture the student should be able to:
1. Define or recognize a definition of Croup
2. Recognize the etiology of Croup
3. Identify the age-group of children affected by Croup
4. Recognize the classic radiographic sign(s) of Croup
5. Identify the clinical signs of Croup
7. Identify the treatment for Croup
8. Define or recognize a definition of Epiglottitis
9. Recognize the etiology of Epiglottitis
10. Identify the population age-group affected by Epiglottitis
11. Recognize the classic radiographic sign(s) of Epiglottitis
12. Identify the clinical signs of Epiglottitis
13. Identify the treatment for Epiglottitis
Croup: Background
Also called laryngotracheobronchitis (LTB)
Peak onset is in children 2 years of age
Primarily occurs in late fall and early winter
Very low mortality but high morbidity
About 5% of children have had at least one
episode of croup; and 5% of them have a
second episode
Croup: Etiology
Most often caused by parinfluenza virus
Also caused by RSV, influenza A and B and
other organisms
Rarely: mycoplasma pneumoniae, herpes, and
measles virus have been reported as causes
Croup: Pathophysiology
Inflammation may occur in both the upper and
lower airways
Subglottic swelling produces stridor when soft
tissues collapse during the negative pressure
of inspiration
Narrowing of the upper airway by 1 mm
reduces the cross-section by 50% in 2 yr old
Croup: Pathophysiology (cont.)
Inflammation of the lower airways can lead to
V/Q mismatching and hypoxemia
Large increases in the WOB are common
Decreases in ventilation are not common in
mild to moderate cases; may occur with severe
fatigue
Croup: Clinical Presentation
Physical
Hx of recent
examupper
helps airway
identify
infection
the severity
Now developnasal
Tachypnea, barking
flaring,
cough,
retractions
hoarseness,
and use
andofstridor
access. muscles
Low grade are common
fever common
CBC often normal,
Symptoms if done at night
often increase
Croup: Radiographic findings
Normal in many cases of croup
Decision to obtain neck film can be difficult and
is often done only in more severe cases and
when epiglottitis is suspected
Subglottic narrowing is seen with croup
Complications such as pneumonia should be
looked for when high fever and leukocytosis
are present
Croup: Radiographic findings cont.
Normal Trachea Trachea with Croup “Steeple Sign”
Croup: Signs of a more severe case
Stridor at rest or I and E stridor
inspiratory retractions
Severe tachypnea (>60/min)
Heavy use of accessory muscles
Abnormal sensorium
Poor response to treatment
Croup: Treatment
Humidity therapy is the first line of treatment
and improves symptoms in most cases
Racemic epinephrine; rapid acting but does not
change length of illness
Steroids: controversial and reserved for severe
cases (Dexamethasone 0.6 mg/kg)
Heliox decreases the WOB; used as an adjunct
Epiglottitis: Background
Also call supraglottitis
Caused by bacterial infection of the
supraglottic structures
Tends to occur in patients 2 to 7 years of age
but is now seen as often in adults
Hemophilus influenzae type B was most
common offending organism prior to 1998
Epiglottitis: Background
Probable cause of death for George
Washington in 1799
Occurs in about 1/100,000 adults in U.S.
Ratio of incidence in children to adults is about
0.5:1
Death rate is about 7% for adults and 1% for
children
Epiglottitis – Background
Male to female ratio is about 3:1
Average age of adult onset is 45 yrs
Average age in children is 5 yrs
Incidence in children has declined in recent
years due to vaccine
Epiglottitis: Pathophysiology
Does not affect structures below the glottis
Trachea and bronchi are healthy in epiglottitis
Gas exchange is preserved in mild cases
Hypoxemia only occurs as a result of
hypercarbia in severe cases
Signs of hypoxemia indicate ventilatory failure
in most cases
Epiglottitis: Clinical features
Most common initial symptoms are fever,
difficult swallowing, and sore throat; abrupt
onset is classic
Stridor occurs in most cases and signals an
advanced case
A prolonged inspiratory time is common and
signals upper airway narrowing
Epiglottitis: Radiographic findings
Always abnormal if film quality is good
Lateral neck film shows enlarged supraglottic
structures and rounding of the epiglottitis
Tracheal air shadow is normal
Lateral neck film indicated whenever epiglottitis
is suspected; should never delay treatment in
severe cases
On the left, an endoscopic view of the throat shows
almost complete blockage of the airway (arrow).
This finding is typical of epiglottitis. On the right,
the airway has been opened (arrow) after insertion
and removal of an endotracheal tube, although
some redness and blood remain.
Epiglottitis: Lab Data
CBC shows leukocytosis
Electrolytes usually normal
Epiglottic swab: positive in 70% of cases
Blood culture positive in 90% of cases
Epiglottitis: Treatment
Prehospital care: DO NOT attempt to intubate
All patients suspected to have epiglottitis are
admitted to the hospital
Some patients need immediate intubation;
others may be able avoid intubation with
aggressive treatment
Children are intubated most often
Epiglottitis: Treatment
Broad spectrum antibiotics given initially after
airway evaluated and secured if needed
Avoid racemic epinephrine
More specific antibiotics can be given when
cultures return
Patient can usually be extubated in 2-3 days
Pneumonia is a possible complication (25%)
You might also like
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtFrom EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtRating: 5 out of 5 stars5/5 (1)
- Respiratory QuestionDocument79 pagesRespiratory QuestionTofik Mohammed100% (2)
- Community Acquired Pneumonia: Ang Gobonseng, Ed Gerard R. MedclerkDocument66 pagesCommunity Acquired Pneumonia: Ang Gobonseng, Ed Gerard R. MedclerkRyn Anfone100% (2)
- Expanded 3P Study Guide YasminaIrinaDocument79 pagesExpanded 3P Study Guide YasminaIrinaikNo ratings yet
- ENT Lecture FinalDocument65 pagesENT Lecture FinalNejib M/AminNo ratings yet
- Acute EpiglottisDocument20 pagesAcute EpiglottissuciNo ratings yet
- Infections of Larynx: Drravikumar M.S (ENT)Document57 pagesInfections of Larynx: Drravikumar M.S (ENT)Drravikumar BhandariNo ratings yet
- Laryngitis by DR - Ahmed.a.al-Zubiadi F.I.C.M.SDocument17 pagesLaryngitis by DR - Ahmed.a.al-Zubiadi F.I.C.M.SRini A. PujaDaraNo ratings yet
- Retropharyngeal Abscess ReportDocument49 pagesRetropharyngeal Abscess ReportAyen FornollesNo ratings yet
- Lower Respiratory Tract Diseases - KeyDocument45 pagesLower Respiratory Tract Diseases - KeyYugmaPandyaNo ratings yet
- Stridor: Anas ObeidDocument43 pagesStridor: Anas ObeidAnas ObiedNo ratings yet
- L2 PneumoniaDocument12 pagesL2 Pneumoniajojoanoo15No ratings yet
- CcroupDocument53 pagesCcroupOlivia BernadiNo ratings yet
- Acute Urti2 - 2010Document19 pagesAcute Urti2 - 2010Ssenyonga DominicNo ratings yet
- File 18584Document12 pagesFile 18584Mohammed MuthanaNo ratings yet
- Munity Acquired PneumoniaDocument4 pagesMunity Acquired PneumoniaDIVEN SolvonNo ratings yet
- Anatomy Head Neck EMRCS MCQDocument23 pagesAnatomy Head Neck EMRCS MCQTowhid HasanNo ratings yet
- Pediatric SmleDocument59 pagesPediatric SmleMoayad Zeyad M100% (1)
- Pyrexia of Unknown OriginDocument81 pagesPyrexia of Unknown OriginJithin Bhagavati Kalam100% (1)
- (Ped-W1) (Dr. Zuhair M. Al Musawi) Repiratory 2Document43 pages(Ped-W1) (Dr. Zuhair M. Al Musawi) Repiratory 2Haider Nadhem AL-rubaiNo ratings yet
- EpiglotitisDocument12 pagesEpiglotitisFecky Fihayatul IchsanNo ratings yet
- Board Review Pediatrics PDFDocument215 pagesBoard Review Pediatrics PDFJoanne Blanco100% (1)
- Disorders of The Pleura: Pleural EffusionDocument50 pagesDisorders of The Pleura: Pleural EffusionAmosNo ratings yet
- Chapter IIDocument34 pagesChapter IINycoNo ratings yet
- Upper Airway Obstruction: Jordan Virbalas, MD Lee P. Smith, MD, FACSDocument15 pagesUpper Airway Obstruction: Jordan Virbalas, MD Lee P. Smith, MD, FACSPhilippe Ceasar C. BascoNo ratings yet
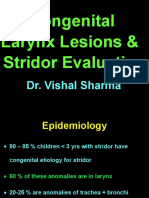
- 12 Congenital Lesions of Larynx and Evaluation of StridorDocument77 pages12 Congenital Lesions of Larynx and Evaluation of StridorAbhishek ShahNo ratings yet
- Upper Airway Obstruction & Infection: PediatricDocument71 pagesUpper Airway Obstruction & Infection: PediatricLuke RosenczweigNo ratings yet
- Dr. Sana Bashir DPT, MS-CPPTDocument46 pagesDr. Sana Bashir DPT, MS-CPPTbkdfiesefll100% (1)
- 13 Inflammatory Disorders of LarynxDocument83 pages13 Inflammatory Disorders of LarynxAbhishek ShahNo ratings yet
- Tracheomalacia 131030001629 Phpapp01Document52 pagesTracheomalacia 131030001629 Phpapp01SaaraAlleyahAlAnaziNo ratings yet
- Board Review: PediatricsDocument215 pagesBoard Review: Pediatricsokurimkuri94% (16)
- NCP PneumoniaDocument2 pagesNCP Pneumoniajulz_otso6359No ratings yet
- Multidisciplinary Case-Based Teaching: Prof. S. O 'Neill Dr. D. Royston Dr. S. ShaikhDocument90 pagesMultidisciplinary Case-Based Teaching: Prof. S. O 'Neill Dr. D. Royston Dr. S. Shaikhmynoidanh19No ratings yet
- CompilationDocument24 pagesCompilationKath RubioNo ratings yet
- Acute LaryngitisDocument18 pagesAcute LaryngitisROXTA RAHULNo ratings yet
- Diseases and TreatmentsDocument72 pagesDiseases and TreatmentsJared Tristan LewisNo ratings yet
- 8.3 Medicine - Tropical Infectious Diseases Leptospirosis 2014ADocument7 pages8.3 Medicine - Tropical Infectious Diseases Leptospirosis 2014ABhi-An BatobalonosNo ratings yet
- Suppurative Lung Diseases.Document37 pagesSuppurative Lung Diseases.Salman KhanNo ratings yet
- Tropical Pulmonary EosinophiliaDocument20 pagesTropical Pulmonary EosinophiliaTamzid Rabby TanmoyNo ratings yet
- 06-TB 1Document51 pages06-TB 1Mihraban OmerNo ratings yet
- BronchiectasisDocument60 pagesBronchiectasisArulNo ratings yet
- Ear, Nose and Throat EmergenciesDocument3 pagesEar, Nose and Throat Emergenciesfmta100% (1)
- StridorDocument3 pagesStridorDrTarek Mahmoud Abo KammerNo ratings yet
- Management of Respiratory EmergencyDocument17 pagesManagement of Respiratory EmergencyVictor BeranNo ratings yet
- Croup (Laryngotracheobronchitis) : EtiologyDocument13 pagesCroup (Laryngotracheobronchitis) : EtiologyOmar mohamedNo ratings yet
- Jnma00736 0021Document3 pagesJnma00736 0021talenticaxo1No ratings yet
- CroupDocument18 pagesCroupSonny WijanarkoNo ratings yet
- Pneumonia AnswersDocument5 pagesPneumonia AnswersColeen Mae CamaristaNo ratings yet
- Acute Respiratory InfectionDocument28 pagesAcute Respiratory InfectionMazharNo ratings yet
- PneumoniaDocument27 pagesPneumoniamohammedghassan53No ratings yet
- Pulmonary EmbolismDocument19 pagesPulmonary EmbolismIbrahimNo ratings yet
- Clinical Manifestations and Complications of Pulmonary Tuberculosis - UpToDateDocument20 pagesClinical Manifestations and Complications of Pulmonary Tuberculosis - UpToDatedixama9519No ratings yet
- RD in NeonatesDocument55 pagesRD in NeonatesAbdallah K. RamadanNo ratings yet
- Critical Care (Emergency Medicine) : HemothoraxDocument7 pagesCritical Care (Emergency Medicine) : HemothoraxOrlando PiñeroNo ratings yet
- A Case of BreathlessnessDocument5 pagesA Case of BreathlessnesschuhuaNo ratings yet
- Shoku AnafilaktikDocument16 pagesShoku AnafilaktikindeenikeNo ratings yet
- MCQ PneuDocument60 pagesMCQ PneuYanesh Bishundat0% (1)
- Pleural Effusion, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandPleural Effusion, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Medical Mnemonic Sketches : Pulmonary DiseasesFrom EverandMedical Mnemonic Sketches : Pulmonary DiseasesNo ratings yet