Professional Documents
Culture Documents
GERD Complications
GERD Complications
Uploaded by
Mikhael John Anil0 ratings0% found this document useful (0 votes)
1 views24 pagesThe document discusses various complications that can arise from untreated gastroesophageal reflux disease (GERD), including esophagitis, Barrett's esophagus, erosive esophagitis, and esophageal strictures. It covers the symptoms, diagnosis, and treatment options for each complication. Key treatment approaches involve lifestyle changes, proton pump inhibitors to reduce acid production, and endoscopic procedures to widen narrowed areas in severe cases of complications like esophageal strictures. Managing these complications properly can help prevent further issues and improve quality of life for GERD patients.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses various complications that can arise from untreated gastroesophageal reflux disease (GERD), including esophagitis, Barrett's esophagus, erosive esophagitis, and esophageal strictures. It covers the symptoms, diagnosis, and treatment options for each complication. Key treatment approaches involve lifestyle changes, proton pump inhibitors to reduce acid production, and endoscopic procedures to widen narrowed areas in severe cases of complications like esophageal strictures. Managing these complications properly can help prevent further issues and improve quality of life for GERD patients.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
1 views24 pagesGERD Complications
GERD Complications
Uploaded by
Mikhael John AnilThe document discusses various complications that can arise from untreated gastroesophageal reflux disease (GERD), including esophagitis, Barrett's esophagus, erosive esophagitis, and esophageal strictures. It covers the symptoms, diagnosis, and treatment options for each complication. Key treatment approaches involve lifestyle changes, proton pump inhibitors to reduce acid production, and endoscopic procedures to widen narrowed areas in severe cases of complications like esophageal strictures. Managing these complications properly can help prevent further issues and improve quality of life for GERD patients.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 24
GERD Complications:
Taming the Fire Within
by Mikhael John Anil
Roll no:-08
Introduction
What is GERD?
Complications of GERD
Diagnosis of GERD Complications
Treatment /Medication Options of each complication
Prevention of each GERD Complications
Reference used in this presention
Introductio
n
Gastroesophageal reflux disease, or
GERD, is a condition that affects
millions of people worldwide. While
many think of it as simply heartburn,
GERD can lead to serious
complications if left untreated.
In this presentation, we will explore
the various complications that can
arise from GERD and why it is crucial
to manage them. From esophagitis to
esophageal cancer, these
complications can have a significant
impact on your health and quality of
life. But don't worry, we will also
discuss the various treatment options
available to help you manage these
complications and prevent them from
occurring in the first place.
What is
GERD?
Gastroesophageal reflux disease (GERD) is
a chronic digestive disorder that occurs
when stomach acid flows back into the
esophagus. The most common symptom of
GERD is heartburn, which is a burning
sensation in the chest that can be
triggered by certain foods, drinks, or
activities. Other symptoms include
regurgitation, difficulty swallowing, and
chest pain.
The causes of GERD are multifactorial and
can include a weakened lower esophageal
sphincter (LES), obesity, pregnancy,
smoking, and certain medications. If left
untreated, GERD can lead to complications
such as esophagitis, Barrett's esophagus,
and even esophageal cancer.
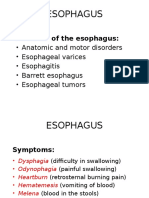
Complications of
GERD
Untreated GERD can lead to a variety of
complications that can significantly impact
a person's quality of life. One such
complication is esophagitis, which is
inflammation of the esophagus. This can
cause pain and difficulty swallowing,
making it hard to eat and drink normally.
Another potential complication of
untreated GERD is Barrett's esophagus,
which is a condition where the cells in the
lining of the esophagus change and
become abnormal. This increases the risk
of developing esophageal cancer, which is
one of the most serious complications of
GERD.
Barrett's Esophagus
Barrett's esophagus is a condition that occurs
when the cells in the lining of the esophagus
change and become abnormal. This is often
caused by long-term acid reflux, which can
lead to chronic inflammation of the
esophagus. The abnormal cells can increase
the risk of developing esophageal cancer,
making it an important complication to be
aware of for those with GERD.
Symptoms of Barrett's esophagus may not be
noticeable at first, but they can include
difficulty swallowing, chest pain, and
heartburn. It is important to undergo regular
screenings if you have been diagnosed with
GERD to monitor for any changes in the lining
of your esophagus.
Diagnosis
The diagnosis of Barrett's esophagus is
typically made through an endoscopy,
which allows a doctor to examine the
lining of the esophagus for any
abnormalities. During this procedure, a
thin, flexible tube with a camera on the
end is inserted through the mouth and
into the esophagus. If abnormal cells are
found, a biopsy may be performed to
confirm the diagnosis.
In addition to an endoscopy, other tests
may be used to diagnose Barrett's
esophagus, such as imaging tests like a
CT scan or MRI. However, these tests are
usually only used if there are concerns
about complications or if the patient is
not able to undergo an endoscopy.
Medication Option
Barrett's esophagus is a condition in which the
lining of the esophagus changes, becoming
more like the tissue that lines the intestines.
This can increase the risk of developing
esophageal cancer. While there is no cure for
Barrett's esophagus, medication can help
manage symptoms and reduce the risk of
complications.
There are several types of medication that may
be used to treat Barrett's esophagus, including
proton pump inhibitors (PPIs), which reduce the
amount of acid produced by the stomach. Other
medications may be used to reduce
inflammation or promote healing of the
esophagus. It is important to work closely with
a doctor to determine the best course of
treatment for each individual case.
Erosive Esophagitis
Erosive Esophagitis is a condition that occurs
when stomach acid repeatedly flows back
into the tube that connects your mouth and
stomach (esophagus). This acid can cause
inflammation and damage to the lining of the
esophagus, leading to painful symptoms and
potential complications if left untreated.
The most common symptoms of Erosive
Esophagitis include heartburn, difficulty
swallowing, and chest pain. These symptoms
can have a significant impact on a person's
daily life, making it difficult to eat and sleep
comfortably. While there are many potential
causes of Erosive Esophagitis, some of the
most common include obesity, smoking, and
certain medications.
Symptom
s
Erosive Esophagitis is a condition that causes
inflammation and irritation in the lining of
the esophagus. The most common symptom
of this condition is heartburn, which is a
burning sensation in the chest that can be
quite uncomfortable. Other symptoms
include difficulty swallowing, chest pain, and
regurgitation of food or liquid.
These symptoms can have a significant
impact on a person's daily life, making it
difficult to eat, sleep, and perform everyday
activities. For example, difficulty swallowing
may make it hard to enjoy meals with friends
and family, while chest pain can be mistaken
for a heart attack, causing anxiety and stress.
Diagnosis and Treatment
To diagnose erosive esophagitis, a doctor
may perform an endoscopy, which involves
inserting a thin, flexible tube with a camera
into the esophagus to look for signs of
inflammation or damage. A biopsy may
also be taken during the endoscopy to
confirm the diagnosis.
Treatment for erosive esophagitis typically
involves proton pump inhibitors, which
reduce the amount of acid produced in the
stomach, allowing the esophagus to heal.
Lifestyle changes, such as avoiding trigger
foods and not lying down immediately
after eating, can also help alleviate
symptoms and prevent recurrence.
Medication
Proton pump inhibitors (PPIs) are the most
commonly prescribed medications for erosive
esophagitis. PPIs work by blocking acid
production in the stomach, which reduces the
amount of acid that can flow back into the
esophagus and cause inflammation or damage.
Commonly prescribed PPIs include omeprazole,
lansoprazole, and esomeprazole. PPIs are
usually taken once a day, before a meal.
In addition to PPIs, doctors may also prescribe
H2 blockers, which reduce the amount of acid
produced in the stomach. H2 blockers are not as
effective as PPIs in treating erosive esophagitis,
but they can be useful in combination with PPIs
or for milder cases of the condition. Examples of
H2 blockers include ranitidine and famotidine.
Prevention
Maintain a healthy weight: Being
overweight increases the risk of developing
erosive esophagitis. Losing weight can help
reduce this risk.
Avoid trigger foods: Certain foods, such as
spicy or acidic foods, chocolate, and
caffeine, can trigger symptoms of erosive
esophagitis. Avoiding these foods can help
prevent symptoms from occurring.
Don't lie down immediately after eating:
Lying down after eating can cause stomach
acid to flow back into the esophagus,
leading to symptoms of erosive esophagitis.
Wait at least 2-3 hours after eating before
lying down.
Esophageal Strictures
The narrowing of the esophagus due to inflammation
and scarring is known as esophageal strictures. This
condition can cause difficulty in swallowing, chest pain,
and regurgitation. It is a common complication of GERD
that can be treated with medication or surgery
depending on the severity of the stricture.
Esophageal strictures can also increase the risk of
developing Barrett's esophagus, a precancerous
condition where the lining of the esophagus changes.
Regular monitoring and treatment of esophageal
strictures can help prevent further complications and
improve quality of life for patients.
Symptom
s
The narrowing of the esophagus due to
scarring or inflammation can cause a
condition called esophageal strictures.
This condition can cause difficulty in
swallowing, chest pain, and
regurgitation of food. In severe cases, it
can even lead to weight loss and
malnutrition.
Esophageal strictures can be caused by
long-term acid reflux, radiation therapy,
or injury to the esophagus. Treatment
may involve stretching or dilation of the
esophagus, medication, or surgery.
Diagnosis
Esophageal strictures are diagnosed
through a series of tests. The most
common test is an endoscopy, where
a thin tube with a camera is inserted
into the esophagus to examine the
area. Other tests may include a
barium swallow or X-ray, which can
help identify any blockages or
narrowing in the esophagus.
In some cases, a biopsy may be taken
during an endoscopy to determine the
cause of the strictures. This can help
guide treatment options and ensure
proper management of the condition.
Treatment
Options
Once an esophageal stricture is diagnosed,
treatment options may vary depending on the
severity of the condition. In mild cases,
medication such as proton pump inhibitors or
H2 blockers may be prescribed to reduce acid
reflux and inflammation. These medications
can also prevent further damage to the
esophagus and reduce the risk of
complications.
For more severe cases, endoscopic dilation
may be necessary. This procedure involves
inserting a thin tube with a balloon at the end
into the esophagus to stretch the narrowed
area. The balloon is then inflated to widen the
stricture and improve swallowing function. In
some cases, multiple dilation sessions may be
required to achieve the desired result.
Medication
In addition to endoscopic dilation, medication can
also be used to treat esophageal strictures. Proton
pump inhibitors and H2 blockers are commonly
prescribed to reduce acid reflux and inflammation,
which can help prevent further damage to the
esophagus. These medications work by reducing
the amount of acid produced in the stomach,
which in turn reduces the amount of acid that can
travel up the esophagus and cause irritation.
It's important to note that medication alone may
not be enough to fully treat an esophageal
stricture, especially if it is severe. However, in
combination with other treatments such as
endoscopic dilation, medication can be a valuable
tool in managing this condition.
Esophageal
Adenocarcino
ma
Esophageal adenocarcinoma is a type of cancer
that develops in the cells lining the lower part of
the esophagus. It is often associated with
gastroesophageal reflux disease (GERD) and
Barrett's esophagus, a condition in which the
normal cells in the lining of the esophagus are
replaced by abnormal cells. The risk of developing
esophageal adenocarcinoma increases with age,
male gender, obesity, smoking, and a family
history of the disease.
Symptoms of esophageal adenocarcinoma may
include difficulty swallowing, chest pain, weight
loss, and fatigue. Treatment options for this type
of cancer may include surgery, chemotherapy,
radiation therapy, or a combination of these
treatments. Early detection and treatment can
improve the chances of successful treatment and
survival.
Symptom
s
Esophageal adenocarcinoma is a type of cancer that
can cause various symptoms. One of the most
common symptoms is difficulty swallowing, also
known as dysphagia. This can occur when the tumor
grows and blocks the esophagus, making it difficult for
food to pass through. Chest pain is another symptom
that may occur due to the tumor pressing against the
chest wall or nerves. Weight loss and fatigue are also
common symptoms, which may occur due to the
body's increased energy demands in fighting cancer.
Other less common symptoms of esophageal
adenocarcinoma include hoarseness, coughing,
vomiting, and hiccups. These symptoms may occur
due to the tumor affecting the nerves and muscles
around the esophagus. It is important to note that
these symptoms can also be caused by other
conditions, so it is essential to consult a healthcare
provider if any of these symptoms persist.
Diagnosis
Diagnosing esophageal adenocarcinoma can be a
complex process, as the symptoms are often similar to
other conditions. If a patient presents with symptoms
such as difficulty swallowing, chest pain, or weight loss,
their healthcare provider may recommend further
testing. One common test is an endoscopy, which
involves inserting a thin, flexible tube with a camera into
the esophagus to examine the area and take tissue
samples for biopsy. Other tests may include imaging
scans such as CT or PET scans to look for any
abnormalities in the esophagus or surrounding tissues.
Once a diagnosis of esophageal adenocarcinoma has
been confirmed, staging tests may be performed to
determine the extent of the cancer and whether it has
spread to other parts of the body. This information is
important in developing a treatment plan tailored to the
patient's specific needs. It is essential for patients to
work closely with their healthcare team to ensure timely
and accurate diagnosis, as early detection can greatly
improve outcomes.
Treatment Option
Once a diagnosis of esophageal adenocarcinoma has been
confirmed, treatment options may include surgery,
radiation therapy, chemotherapy, or a combination of these
approaches. The choice of treatment depends on the stage
and location of the cancer, as well as the patient's overall
health and preferences. Surgery may involve removing part
or all of the esophagus, nearby lymph nodes, and other
affected tissues. Radiation therapy uses high-energy beams
to kill cancer cells, while chemotherapy uses drugs to
destroy cancer cells throughout the body.
In recent years, targeted therapy and immunotherapy have
emerged as promising new treatment options for
esophageal adenocarcinoma. Targeted therapy involves
using drugs that specifically target certain proteins or genes
involved in cancer growth, while immunotherapy works by
stimulating the immune system to attack cancer cells.
These treatments may be used alone or in combination
with other therapies, depending on the individual case.
Medication
In addition to surgery, radiation therapy, and
chemotherapy, medication can also play a role in the
treatment of esophageal adenocarcinoma. One type of
medication commonly used is called proton pump
inhibitors (PPIs), which reduce the amount of acid
produced by the stomach. This can help relieve symptoms
such as heartburn and acid reflux, which are common in
patients with esophageal adenocarcinoma. PPIs may also
have a protective effect against further damage to the
esophagus.
Another type of medication that may be used is called
targeted therapy. This involves using drugs that specifically
target proteins or genes involved in cancer growth. For
example, some targeted therapies may block the activity of
a protein called HER2, which is overexpressed in some
cases of esophageal adenocarcinoma. By blocking this
protein, the drug can slow or stop the growth of cancer
cells. Targeted therapy may be used alone or in
combination with other treatments.
References used:
1. Lagergren J, Smyth E, Cunningham D,
Lagergren P. Oesophageal cancer. Lancet.
2017;390(10110):2383-2396.
2. Thrift AP, Shaheen NJ, Gammon MD, et
al. Obesity and risk of esophageal
adenocarcinoma and Barrett's esophagus:
a Mendelian randomization study. J Natl
Cancer Inst. 2014;106(11):dju252.
3. Singh S, Garg SK, Singh PP, Iyer PG, El-
Serag HB. Acid-suppressive medications
and risk of oesophageal adenocarcinoma
in patients with Barrett's oesophagus: a
systematic review and meta-analysis. Gut.
2014;63(8):1229-1237.
You might also like
- Taking The Long View On MetabolismDocument3 pagesTaking The Long View On Metabolismaudesing100% (3)
- Test Bank For Medical Physiology 3rd Edition Walter Boron Emile BoulpaepDocument3 pagesTest Bank For Medical Physiology 3rd Edition Walter Boron Emile BoulpaepMisti Keane100% (34)
- Herbs For Gastroesophageal Reflux DiseaseDocument4 pagesHerbs For Gastroesophageal Reflux DiseasegandhicgandhiNo ratings yet
- AM - ICD-10-AM GuideDocument26 pagesAM - ICD-10-AM GuidedrrskhanNo ratings yet
- Esophageal Disorders Types, Risks, Symptoms and TDocument14 pagesEsophageal Disorders Types, Risks, Symptoms and TKolade YousuffNo ratings yet
- BarrettDocument6 pagesBarrettdbhangui6528No ratings yet
- Gastroesophageal Reflux DiseaseDocument4 pagesGastroesophageal Reflux DiseasemrbrutusNo ratings yet
- UlcersDocument2 pagesUlcersAngelic SalongaNo ratings yet
- Gastroesophageal Reflux DiseaseDocument4 pagesGastroesophageal Reflux DiseasemariatheressamercadoNo ratings yet
- GERD GuideDocument8 pagesGERD GuidemirazainiNo ratings yet
- What's Acid Reflux and GERDDocument10 pagesWhat's Acid Reflux and GERDSelim HanNo ratings yet
- The Clinical Management of Gastroesophageal Reflux DiseaseDocument12 pagesThe Clinical Management of Gastroesophageal Reflux DiseaseMahmoud SamiNo ratings yet
- Gastroesophageal Reflux Disease: SymptomsDocument8 pagesGastroesophageal Reflux Disease: Symptomspragna novaNo ratings yet
- Duodenum Esophagus Stomach Meckel's Diverticulum: Pylori. Infection Usually Persists For ManyDocument3 pagesDuodenum Esophagus Stomach Meckel's Diverticulum: Pylori. Infection Usually Persists For ManyKim Andrew SantosNo ratings yet
- KLMPK 2 Ulkus Peptikum EnglishDocument13 pagesKLMPK 2 Ulkus Peptikum EnglishWulan KiranaNo ratings yet
- Patient Information Gastroesophageal Reflux Disease (Hiatal Hernia and Heartburn)Document7 pagesPatient Information Gastroesophageal Reflux Disease (Hiatal Hernia and Heartburn)Gail AidNo ratings yet
- Peptic Ulcer DiseaseDocument12 pagesPeptic Ulcer Diseasehya2284No ratings yet
- Chris L. Place, MD January 27, 2005Document56 pagesChris L. Place, MD January 27, 2005Satrasala AshokkumarNo ratings yet
- Barrett’s Esophagus, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandBarrett’s Esophagus, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Gastroesophageal Reflux (GERD) : Prepared By/ Eman Abdelmobdy AliDocument12 pagesGastroesophageal Reflux (GERD) : Prepared By/ Eman Abdelmobdy AliMahmoud Abdel MoneimNo ratings yet
- What Is A Peptic UlcerDocument4 pagesWhat Is A Peptic UlcerIrah May Dela Tina0% (1)
- Symptoms: Dyspepsia. The Most Common Symptoms of Peptic Ulcer Are Known Collectively As Dyspepsia. However, PepticDocument10 pagesSymptoms: Dyspepsia. The Most Common Symptoms of Peptic Ulcer Are Known Collectively As Dyspepsia. However, Pepticmiz uNo ratings yet
- EsophagitisDocument8 pagesEsophagitisRani SujithNo ratings yet
- Case Reporrt GerdDocument7 pagesCase Reporrt GerdKarina WidyaNo ratings yet
- Case Study 1 PDFDocument2 pagesCase Study 1 PDFania ojedaNo ratings yet
- Ebp PaperDocument5 pagesEbp Paperapi-251752244No ratings yet
- Activity #2 Digestive System AnaphyDocument8 pagesActivity #2 Digestive System AnaphyGabriela sullanoNo ratings yet
- GERD - PPT 11Document30 pagesGERD - PPT 11pharmaguy111No ratings yet
- Barrett's Esophagus: Possible ComplicationsDocument3 pagesBarrett's Esophagus: Possible ComplicationsindahkurNo ratings yet
- Understand GerdDocument10 pagesUnderstand GerdAfnindy Leo PutraNo ratings yet
- Signs and Symptoms: AdultsDocument15 pagesSigns and Symptoms: AdultsHelen McClintock100% (1)
- GastritisDocument6 pagesGastritisErmawati ErmaNo ratings yet
- Pharmacotherapy For GERDDocument6 pagesPharmacotherapy For GERDJoon HyungNo ratings yet
- GERD Sartiwi DestriliaDocument1 pageGERD Sartiwi Destriliasartiwi DestriliaNo ratings yet
- What Is Gastritis? What Causes Gastritis?: Upper Gastrointestinal EndosDocument5 pagesWhat Is Gastritis? What Causes Gastritis?: Upper Gastrointestinal EndosjaiologyNo ratings yet
- LO Gastro1bDocument4 pagesLO Gastro1bviryamedikaNo ratings yet
- GERDDocument4 pagesGERDAmomymousNo ratings yet
- Tugas Artikel Gastritis: Sekolah Tinggi Ilmu Kesehatan Cirebon Kampus 2 Rs CiremaiDocument10 pagesTugas Artikel Gastritis: Sekolah Tinggi Ilmu Kesehatan Cirebon Kampus 2 Rs CiremaiM Ibnu WismoyoNo ratings yet
- Functional DyspepsiaDocument19 pagesFunctional DyspepsiaMahmoud AliNo ratings yet
- Centers of GastroenterologyDocument8 pagesCenters of GastroenterologyLia Mbag LiaNo ratings yet
- Gastroesophageal Reflux DiseaseDocument8 pagesGastroesophageal Reflux DiseaseRicoSopoNo ratings yet
- GastritisDocument6 pagesGastritisNader Smadi100% (5)
- Peptic UlcerDocument5 pagesPeptic UlcermerobabuNo ratings yet
- Intestinal Obstructions Definition and Patient EducationDocument1 pageIntestinal Obstructions Definition and Patient EducationOlabode AdeolaNo ratings yet
- GerdDocument8 pagesGerdLoms KotopNo ratings yet
- Aspiration Prevention Management of Gastroesophageal Reflux Aspiration - HS - AP - GERD - V2Document6 pagesAspiration Prevention Management of Gastroesophageal Reflux Aspiration - HS - AP - GERD - V2RobertNo ratings yet
- GastritisDocument5 pagesGastritisIasSonghuiNo ratings yet
- GerdDocument8 pagesGerdarinrinNo ratings yet
- Unit 5 Research Gastroesophageal Reflux DiseaseDocument35 pagesUnit 5 Research Gastroesophageal Reflux Diseasecindyfuller68No ratings yet
- Heartburn, Gastroesophageal Reflux (GER), and Gastroesophageal Reflux Disease (GERD)Document8 pagesHeartburn, Gastroesophageal Reflux (GER), and Gastroesophageal Reflux Disease (GERD)Aya SorayaNo ratings yet
- PDF GuidelineforgerdDocument1 pagePDF GuidelineforgerdFilip HarasimiukNo ratings yet
- Heart BurnDocument6 pagesHeart BurnNader SmadiNo ratings yet
- Peptic UlcerDocument12 pagesPeptic UlcerhaddejNo ratings yet
- Peptic UlcerDocument12 pagesPeptic UlcerhaddejNo ratings yet
- Peptic UlcerDocument12 pagesPeptic UlcerhaddejNo ratings yet
- GERD Focused Academic ReadingDocument3 pagesGERD Focused Academic ReadingKM PanganibanNo ratings yet
- Gastroesofag RefluxDocument4 pagesGastroesofag RefluxRizaldy KehiNo ratings yet
- Gastroesophageal Reflux Disease PharmacotherapyDocument22 pagesGastroesophageal Reflux Disease PharmacotherapyrinirhynNo ratings yet
- The Nursing Assessment of Peptic UlcerDocument14 pagesThe Nursing Assessment of Peptic UlcerVelia suwandiNo ratings yet
- Research RefluxDocument40 pagesResearch RefluxSebastian LisNo ratings yet
- Common Digestive Disorder: Presented byDocument11 pagesCommon Digestive Disorder: Presented byRalph Reneal Baltazar CalapateNo ratings yet
- Gastritis: Acute Gastritis Occurs Suddenly and Is More Likely To Cause Nausea andDocument7 pagesGastritis: Acute Gastritis Occurs Suddenly and Is More Likely To Cause Nausea andronilaNo ratings yet
- Diagnosis and Management of Functional HeartburnDocument9 pagesDiagnosis and Management of Functional Heartburnal ghiffari muhammad rayhanNo ratings yet
- ERMPDocument80 pagesERMPMatt ZewduNo ratings yet
- Accepted Manuscript: Journal of Pediatric SurgeryDocument36 pagesAccepted Manuscript: Journal of Pediatric SurgeryWilliam Rafael AscanioNo ratings yet
- Pharmacotheraphy Gastrointestinal Tract: OutlineDocument34 pagesPharmacotheraphy Gastrointestinal Tract: OutlineMaharani Dewi NugrahaNo ratings yet
- Evidence-Based Clinical Practice Guidelines For Gastroesophageal Reflux Disease 2015Document17 pagesEvidence-Based Clinical Practice Guidelines For Gastroesophageal Reflux Disease 2015carolina.rahardjaNo ratings yet
- StomatitisDocument17 pagesStomatitis4A - Hazel Ann G. EspinolNo ratings yet
- Master Radiology Notes GITDocument115 pagesMaster Radiology Notes GITuroshkg100% (2)
- Gerd CPG PDFDocument17 pagesGerd CPG PDFJamie SebastianNo ratings yet
- Performance Measures For Upper Gastrointestinal Endoscopy: A European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement InitiativeDocument22 pagesPerformance Measures For Upper Gastrointestinal Endoscopy: A European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement InitiativeMadalina StoicescuNo ratings yet
- Esophagus: Diseases of The EsophagusDocument60 pagesEsophagus: Diseases of The EsophagusSalma NajjarNo ratings yet
- Test Bank On GI PathologyDocument14 pagesTest Bank On GI PathologySeff CausapinNo ratings yet
- PATHO 4-3 Diseases of The EsophagusDocument7 pagesPATHO 4-3 Diseases of The EsophagusMiguel Cuevas DolotNo ratings yet
- Carcinoma of EsophagusDocument41 pagesCarcinoma of EsophagusBiju ViswambharanNo ratings yet
- L28 - Esophageal DiseasesDocument16 pagesL28 - Esophageal DiseasesNimer Abdelhadi AliNo ratings yet
- Gerd Blok 2 6Document43 pagesGerd Blok 2 6Mus TofaNo ratings yet
- نم انوسنت لا مكوجرأ ,يلهلا و يل ةيراج ةقدص مكئاعد حلا ص Please Grace us with your good prayersDocument538 pagesنم انوسنت لا مكوجرأ ,يلهلا و يل ةيراج ةقدص مكئاعد حلا ص Please Grace us with your good prayersSahan EpitawalaNo ratings yet
- What Are Common Conditions That Affect The Esophagus? - Dr. Samrat JankarDocument2 pagesWhat Are Common Conditions That Affect The Esophagus? - Dr. Samrat JankarDr. Samrat JankarNo ratings yet
- Final Interpretation of Endoscopic Gastrointestinal BiopsyDocument107 pagesFinal Interpretation of Endoscopic Gastrointestinal BiopsyyourinmyheartNo ratings yet
- Gastroesophageal Reflux DiseaseDocument17 pagesGastroesophageal Reflux DiseasearshimulNo ratings yet
- Gerd PDFDocument51 pagesGerd PDFaddfreNo ratings yet
- Gastro-Esophageal Reflux Disease (GERD) : Prof DRDocument21 pagesGastro-Esophageal Reflux Disease (GERD) : Prof DRmohammed salahNo ratings yet
- Mikami 2015Document11 pagesMikami 2015Andrés HerrónNo ratings yet
- EndoskopiDocument7 pagesEndoskopicacingpandoraNo ratings yet
- Proton Pump Inhibitors, Adverse Events and Increased Risk of MortalityDocument36 pagesProton Pump Inhibitors, Adverse Events and Increased Risk of MortalityMohammad Mahmudur RahmanNo ratings yet
- 3B CTC08 Gerd 10.01.16Document41 pages3B CTC08 Gerd 10.01.16Adriel PizarraNo ratings yet
- The Effective Use of Gastrointestinal Histopathology: Guidance For Endoscopic Biopsy in The Gastrointestinal TractDocument5 pagesThe Effective Use of Gastrointestinal Histopathology: Guidance For Endoscopic Biopsy in The Gastrointestinal TractHồng Khuyên LưuNo ratings yet