Professional Documents
Culture Documents
Wound Treatment Options
Wound Treatment Options
Uploaded by
khaista bacha0 ratings0% found this document useful (0 votes)
20 views52 pagesThis document discusses various wound treatment options including dressings and therapies. It provides details on different types of dressings such as transparent films, hydrocolloids, hydrogels, foams, collagen dressings, and antimicrobial dressings. It explains how each dressing works, what wound types it can be used for, and considerations for application and changing. The document also briefly mentions mechanical treatment options like negative pressure wound therapy and compression therapy. The overall document focuses on educating about appropriate wound dressing selection and use based on wound assessment and goals of care.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses various wound treatment options including dressings and therapies. It provides details on different types of dressings such as transparent films, hydrocolloids, hydrogels, foams, collagen dressings, and antimicrobial dressings. It explains how each dressing works, what wound types it can be used for, and considerations for application and changing. The document also briefly mentions mechanical treatment options like negative pressure wound therapy and compression therapy. The overall document focuses on educating about appropriate wound dressing selection and use based on wound assessment and goals of care.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
20 views52 pagesWound Treatment Options
Wound Treatment Options
Uploaded by
khaista bachaThis document discusses various wound treatment options including dressings and therapies. It provides details on different types of dressings such as transparent films, hydrocolloids, hydrogels, foams, collagen dressings, and antimicrobial dressings. It explains how each dressing works, what wound types it can be used for, and considerations for application and changing. The document also briefly mentions mechanical treatment options like negative pressure wound therapy and compression therapy. The overall document focuses on educating about appropriate wound dressing selection and use based on wound assessment and goals of care.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 52
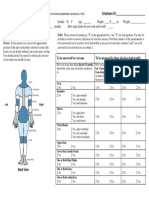
Lecture 6
Wound Treatment Options
Being able to differentiate among the various
treatment options, when and how to apply them, in
what combinations, and when to change them has
indeed become both an art and a science.
Providing quality care for wound patients starts with
an analysis of the patient’s individualized wound
assessment and continues with developing a plan of
care, selecting the proper product, and re-evaluating
the plan of care as appropriate.
Wound dressings can present a challenging decision
for clinicians
Treatment Decisions
Optimal wound interventions should be
dependent on the basic principles of wound
care, attentive wound assessment, and
expected outcomes.
A complete wound assessment should be the
driving element in all treatment decisions.
Wound assessment should be based on the
principles of wound care.
Principles of Care: The MEASURES Acronym
Treatment goals may aim to achieve a clean
wound, heal the wound, maintain a clean
wound bed, or place the patient in another
setting to continue care.
The goal of care then becomes using the right
product on the right wound at the right time.
For example, a granular, non draining moist
or wet wound needs to maintain a moisture
balance that is conducive to healing.
The primary dressing choice would be a product
that maintains a moist environment but doesn’t
cause maceration of the wound bed.
In another example, the goal of dressing selection
for a necrotic draining wound is to loosen or
soften the eschar for surgical debridement or to
assist in autolytic debridement of the wound
absorb the excess exudate, and prevent trauma to
surrounding tissue.
Secondary dressings are those that cover a
primary dressing or secure a dressing in
place.
Clinicians should know which dressings are
safe to be put into the wound itself and which
are used as securement products.
Several dressings on the market act as both
primary and secondary dressings.
Dressings should be matched carefully to the
wound, the patient, and the setting.
For example, a deep wound with a large
amount of drainage will require a highly
absorbent dressing such as foam.
As the depth and amount of drainage
decrease, a dressing such as a hydrogel,
hydrocolloid, or film might be used.
Moist Wound Therapy and Dressing
Options
The essential function of a wound dressing is to
provide the right environment to enhance and
promote wound healing.
Research over the past 50 years has led to the
generally accepted phenomenon that moist wound
dressings create an optimal environment for
wounds to heal faster and with less scar formation.
The following synopsis reviews the major dressing
categories and provides helpful practice points on
what, when, and how to use these dressings.
Transparent Film Dressings
Transparent film dressings are thin
polyurethane membranes. They are coated with
an adhesive that allows them to adhere to the
wound margins without sticking to the actual
wound.
Transparent films have no absorptive capacity
but do transmit moisture vapor and are
semipermeable to gases.
This covering allows epithelial cells to migrate
over the surface of the wound.
Fluid may accumulate under these dressings.
This fluid is sometimes mistaken for pus, a
sign of infection
When excess fluid accumulates or leaks out
from the sides of the dressing, the dressing
needs to be changed.
Transparent film dressings provide a valuable
protective barrier against outside
contaminants, fluid, and bacteria.
Transparent films also add a layer of
protection to the wound bed to minimize
further damaging trauma.
They provide protection from friction and aid
in autolytic debridement and pain control.
Most films can be left on for up to 7 days.
These dressings are indicated for wounds
with absent or low levels of exudate.
Transparent films can be used on a variety of
wound types, such as stage I and II pressure
ulcers, superficial wounds, minor burns, or
lacerations; over sutures, catheter sites, and
superficial dermal ulcers; and for protection
of the skin against friction.
Transparent dressings can be used on central
lines, peripherally inserted central catheter
lines, and infected wounds.
Hydrocolloid Dressings
Hydrocolloid dressings were introduced in the
1980s and were the mainstay for wound
management for many years.
Hydrocolloids are impermeable to gases and
water vapors and are composed of opaque
mixtures of adhesive, absorbent polymers,
pectin gelling agents etc. (Fig. 9-4).
Hydrophilic particles within the dressing react
with the wound fluid to form a soft gel over the
wound bed.
Hydrocolloid dressings may have a noticeable
odor during dressing changes. This is normal in
the absence of clinical signs of infection.
Hydrocolloid dressings are sold in sheet, paste,
and powder forms and are available in many
sizes.
Adhesive properties and ability to absorb exudate
vary by product. Most of these dressings are
adhesive so care must be taken when using on
fragile skin.
Correct application requires the dressing to be
bigger than the actual wound size.
The dressing should be changed as
recommended from 3 to 7 days and often
depends on the amount of exudate.
Hydrocolloids are indicated for minimally to
moderately heavy exudating wounds,
lacerations, pressure ulcers, granular wounds, or
necrotic wounds as well as under compression
wraps.
Hydrocolloids also provide a moist
environment that is conducive to autolytic
debridement.
Excessive maceration can occur if the
dressing isn’t changed appropriately.
Hydrocolloids are often used as a preventive
dressing on high-risk areas (sacrum, heels)
and around surgical wounds to protect the
skin from frequent tape removal.
Hydrogel Dressings
Hydrogel dressings have provided clinicians
with a viable means to hydrate or, stated
differently, donate moisture to dry wound
beds.
This moist environment facilitates autolysis
and removal of devitalized tissue.(Fig. 9-5).
The main application for hydrogels is
hydrating dry wound beds and softening and
loosening slough and necrotic wound debris.
Hydrogels have a limited absorptive capacity
due to their high water concentration.
Some hydrogels have other ingredients, such
as collagen, or starch, to enhance their
absorptive capacity and will absorb low to
moderate amounts of exudate.
They can be used for many types of wounds,
including pressure ulcers, partial and full-
thickness wounds, and vascular ulcers.
One of the benefits of a hydrogel is that it can
be used with topical medications or
antibacterial agents.
Hydrogels are packaged as sheets, tube gels,
sprays, and impregnated gauze pads or strips
for packing tunneling and undermined areas
within the wound bed.
Some require a secondary dressing to secure
the hydrogel; new versions have adhesive
borders.
Foam Dressings
Foam dressings are highly absorbent and are
usually made from a polyurethane base with
a heat- and pressure-modified wound contact
layer (Fig. 9-7).
Foam dressings are permeable to both gases
and water vapor, and their hydrophilic
properties allow for absorption of exudate
into the layers of the foam.
Foam dressings are indicated for wounds with
moderate to heavy exudate, prophylactic
protection over bony prominences or friction
areas, partial and full-thickness wounds, necrotic
wound beds, skin tears, under compression
wraps, surgical wounds, in combination with
other primary dressings.
They can also be used on infected wounds and
can be left on up to 7 days, depending on product
and exudates.
Foams shouldn’t be used on dry eschar
wound beds because they could cause further
desiccation of the wound site.
Foams may be used in combination with
topical treatments and/or enzymatic
debriders.
Foams are available in many sizes and
shapes, including cavity dressings.
Caution with fragile skin may be warranted.
Collagen Dressings
Collagen is a major protein of the body and is
necessary for wound healing and repair.
Collagen dressings either are 100% collagen or
may be combined with alginates or other
products.
They are a highly absorptive, hydrophilic, moist
wound dressing (Fig. 9-9).
Seaman suggests that collagen powders,
particles, and pads are useful in treating highly
exudative wounds.
If the wound has low to moderate exudate, sheets
should be used. If the wound is dry, gels should be
used.
Collagen dressings can be used on granulating or
necrotic wounds and on partial- or full-thickness
wounds.
They may be used with other topical agents. A
collagen dressing should be changed every 3 to 7
days.
Collagen dressings require a secondary dressing for
securement.
Antimicrobial Dressings
Antimicrobial dressings are different than topical
antibiotic therapy.
They provide the benefit of an antimicrobial effect against
bacteria and a moist environment for healing. (Fig. 9-10).
Antimicrobial dressings do not replace the need for
systemic antibiotic therapy; rather, they serve as an
adjunct in treating wound infections.
Antimicrobial dressings are available in a variety of forms:
transparent dressings, gauze, foams, and absorptive fillers
etc.
Some of these dressings can remain in place for 7 days.
Mechanical
A large number of devices and therapies can be
considered in the group of mechanical modalities.
Included in this category are negative pressure
wound therapy (NPWT), compression therapy,
and energy-based therapy (electrical stimulation,
light, and ultrasonic).
Mechanical therapies impact wound healing via
several mechanisms including angiogenesis,
cellular stimulation, bioburden reduction, and
enhanced tissue perfusion.
Negative Pressure Wound Therapy
NPWT is in its third decade of use in the United
States and has become an accepted therapy for
many chronic and, in some cases, acute wounds.
It is commonly used to assist with wound closure.
In general, NPWT is indicated for full-thickness
wounds that require contraction and granulation
tissue formation.
Reduction of wound volume is one of the most
widely recognized outcomes from using NPWT.
NPWT applies subatmospheric pressure, or
suction, to the wound bed by way of a device
that is attached to a wound contact layer
(interface dressing) through a plastic tube
(Fig. 9-11).
Most clinicians have migrated to the use of
foam interfaces based on adverse outcomes
that have been reported with gauze.
Compression Therapy
Venous Compression Therapy
Compression therapy is the foundation for successful
management in patients with edematous wounds
caused by venous insufficiency and/or lymphedema.
Compression therapy wraps are used to manage fluid
accumulation and promote sufficient return of venous
blood back to the central system and lymph back into
the bloodstream.
The substances transported by the lymphatic system
are called lymphatic loads and consist of protein,
water, and fat from the digestive system.
It is worth noting that the edema associated
with venous insufficiency is different in
consistency from the edema or fluid
accumulation that is seen in lymphedema.
Protein-rich lymphedema fluid appears to be
more “viscous” or thicker than the edema
associated with venous insufficiency and
requires different treatment interventions,
including higher compression forces when using
wraps or garments.
Compression Dressings
Short-stretch or rigid compression systems are
particularly suited to managing the fluid
accumulation of lymphedema and are also
indicated for patients with a combination of
venous insufficiency and lymphedema in the
same leg.
An Unna boot is a “short-stretch” system that
includes a moist layer impregnated with several
substances, including zinc oxide, calamine.
Long-stretch bandages are so called due to
their large amount of extensibility and elastic
recoil back to near-original configuration.
While short-stretch bandages require the
patient to be ambulatory or able to engage
the calf muscles effectively (ideally by
walking), long-stretch bandages have been
shown to be suitable for individuals who are
not active or who are nonambulatory.
Clinicians need to be trained and skilled to
proficiently and safely apply these
compression wraps, keeping in mind that
they should be applied according to the
manufacturer’s detailed directions(Fig. 9-15).
Compression Devices
Some compression systems do not fall into
the wrap or bandage category.
These include garments that are usually
short-stretch systems consisting of material
that does not give way during ambulation;
these systems often include Velcro straps to
help secure and conform the garment to the
extremity contours (Fig. 9-16).
Electrical Stimulation
Electrical stimulation has been used for more than
three decades to accelerate the rate of chronic
wound healing.
Healthcare professionals who have used ES
consider it to be one of the most cost effective,
therapeutically efficacious tissue repair and wound
healing accelerators in our wound care tool kit.
Unfortunately, ES is not widely used due to the
lack of knowledge, education, and training in the
application of this energy.
ES uses an electrical current to transfer energy to the
tissue. This energy produces a number of cellular
processes and physiological responses that are
important to wound healing, including:
stimulation of fibroblasts to enhance collagen and
DNA synthesis
increase in the number of receptor sites for growth
factors
alteration in the direction of fibroblast migration,
activation of cells in the wound site, improved tissue
perfusion, and decreased edema.
Ultrasonic Energy
Therapeutic ultrasound delivers energy through
mechanical vibrations in the form of sound waves
at frequencies above detection by the human ear
(>20 kHz). Ultrasound affects tissue through
thermal and non thermal mechanisms, which are
determined by the physical properties, which are
associated with ultrasound:
(1) frequency or the number of oscillations a
molecule undergoes in 1 second and
(2) intensity or level of power.
High-Frequency Ultrasound:
High-frequency ultrasound is used 1 to 3 MHz range to
promote soft tissue injury healing and occasionally
reported to facilitate wound healing.
Low-Frequency Ultrasound:
Recently, low-frequency ultrasound (LFU) available for
wound care and is the most common type of US device
used in wound care today.
Delivery of LFU to wounds has been shown to effectively
deride necrotic tissue, eradicate some strains of bacteria
from the wound, and facilitate the wound healing process.
Scar Management
Patients, clinicians, and researchers are all
concerned about scar appearance. Progress has
been made in our understanding of the
mechanisms involved in producing an
exaggerated scar.
The scientific principles for scar management and
minimization—support, controlled inflammation,
adequate hydration, and remodeling/maturation
of collagen form the basis of product selection for
scar control strategies.
Widgerow and colleagues have described a
patented process of applying a cream/gel
that contains antiscar active agents (Centella
asiatica, dimethicone, Bulbine frutescens) to
the surface of microporous tape.
This process has been used successfully for
scar management. Within 2 minutes, the
active agents in the gel are absorbed through
the tape and onto the scar tissue.
THANK YOU
You might also like
- Nordic Musculoskeletal Questionnaire Form PDFDocument1 pageNordic Musculoskeletal Questionnaire Form PDFkhaista bacha100% (4)
- Nordic Musculoskeletal Questionnaire Form PDFDocument1 pageNordic Musculoskeletal Questionnaire Form PDFkhaista bachaNo ratings yet
- Medicomat 39Document10 pagesMedicomat 39Ripro SurgNo ratings yet
- Excellent - MeaningDocument3 pagesExcellent - MeaningEmmanuel MahengeNo ratings yet
- From Transparent Dressings To Hydrogels, Wound Care Dressings You Use Every Day - WCEIDocument8 pagesFrom Transparent Dressings To Hydrogels, Wound Care Dressings You Use Every Day - WCEIDaniguedesNo ratings yet
- How To Choose The Appropriate DressingDocument4 pagesHow To Choose The Appropriate DressingDyan TD100% (1)
- Minor Veterinary SurgeryDocument14 pagesMinor Veterinary SurgeryLavinia JurcaNo ratings yet
- Medical DressingDocument9 pagesMedical DressingtokagheruNo ratings yet
- IPT AssignmentsDocument1 pageIPT AssignmentsRomana VayaniNo ratings yet
- Wound Dressing Types - OSCE Guide - Geeky MedicsDocument11 pagesWound Dressing Types - OSCE Guide - Geeky MedicsAnwar AlmahmodeNo ratings yet
- Wound DressingsDocument32 pagesWound DressingsAnnaiqaNo ratings yet
- How To Choose The Appropriate DressingDocument4 pagesHow To Choose The Appropriate DressingNinin ErniawatiNo ratings yet
- Surgical DressingDocument60 pagesSurgical DressingJeffri syaputraNo ratings yet
- Wound Coverage With Allogenic Skin: Ing and Biologic DressingsDocument9 pagesWound Coverage With Allogenic Skin: Ing and Biologic DressingskharemixNo ratings yet
- Dressing Selection in Chronic Wound ManagementDocument10 pagesDressing Selection in Chronic Wound ManagementFenni OktoberryNo ratings yet
- A Thoroughgoing Detail of Surgical Dressings PDFDocument17 pagesA Thoroughgoing Detail of Surgical Dressings PDFFortune JournalsNo ratings yet
- Wound Dressings VanessaDocument13 pagesWound Dressings VanessaMuhamad Sidik HasanudinNo ratings yet
- Advanced Wound DressingDocument14 pagesAdvanced Wound DressingGanga DharanNo ratings yet
- Wound DressingDocument3 pagesWound Dressingenojosa nhoelNo ratings yet
- Wound Care Essentials 5th Edition 2020-538-669 - CompressedDocument132 pagesWound Care Essentials 5th Edition 2020-538-669 - CompressedRomana VayaniNo ratings yet
- Suture MaterialsDocument36 pagesSuture Materialsdrhiwaomer100% (14)
- Types of Wound DressingsDocument8 pagesTypes of Wound DressingsDwayne GriffenNo ratings yet
- View Doc 635470672036959908Document6 pagesView Doc 635470672036959908abhishekbmcNo ratings yet
- Advanced Wound DressingsDocument32 pagesAdvanced Wound DressingskkmNo ratings yet
- Veterinary Clinics: Topical and Systemic Medications For WoundsDocument19 pagesVeterinary Clinics: Topical and Systemic Medications For WoundsLina Angarita Herrera100% (1)
- Cronic WoundsDocument11 pagesCronic WoundsAyline Araceli AlavaNo ratings yet
- Most Essential Learning CompetencyDocument6 pagesMost Essential Learning CompetencyPaolo OcampoNo ratings yet
- Burns DressingDocument4 pagesBurns DressingBalaMuruganNo ratings yet
- Wound and Skin Ulcer Management Care Guide PDFDocument21 pagesWound and Skin Ulcer Management Care Guide PDFAdriel Chandra AngNo ratings yet
- FINAL Copy Wound Management ProductsDocument21 pagesFINAL Copy Wound Management ProductsazilebongcloudinengenyiNo ratings yet
- Wound Dressings Update: Carolina Weller, Geoff SussmanDocument7 pagesWound Dressings Update: Carolina Weller, Geoff SussmanyodinheimNo ratings yet
- Bandages Casts and External Support Equine WoundsDocument18 pagesBandages Casts and External Support Equine WoundsDanahe CastroNo ratings yet
- Dressing in First Aid KitDocument15 pagesDressing in First Aid KitEthNo ratings yet
- Presentation of Wound DressingDocument17 pagesPresentation of Wound DressingGafur TarniNo ratings yet
- The Wound Dressings and Their Applications in Wound Healing and ManagementDocument2 pagesThe Wound Dressings and Their Applications in Wound Healing and ManagementJohn FredNo ratings yet
- Dressing PDFDocument4 pagesDressing PDFIndika KarunamuniNo ratings yet
- Hydrogels+for+advanced+wound+management Revised+manuscript FinalDocument13 pagesHydrogels+for+advanced+wound+management Revised+manuscript FinalguedemclemenceNo ratings yet
- Dressing BedsoreDocument66 pagesDressing BedsoreGirish Waru100% (1)
- Surgical DressingDocument6 pagesSurgical DressingSania KanwalNo ratings yet
- 9 PDFDocument25 pages9 PDFDevina NawangsihNo ratings yet
- Modern Wound Dressing - pptx-1Document32 pagesModern Wound Dressing - pptx-1puvi.mayor2104No ratings yet
- Guide To Burn DressingsDocument4 pagesGuide To Burn DressingsjustanothergunnutNo ratings yet
- Cp201011 Practice Tools-363Document4 pagesCp201011 Practice Tools-363Shawn BNo ratings yet
- Dear Love 1996Document15 pagesDear Love 1996David Salomon Gomez AscencioNo ratings yet
- A - Pratic Guide Pediatric Wound CareDocument9 pagesA - Pratic Guide Pediatric Wound CareLicia GabrielleNo ratings yet
- Wound Dressings Update: Carolina Weller, Geoff SussmanDocument7 pagesWound Dressings Update: Carolina Weller, Geoff SussmanKevin AdrianNo ratings yet
- Dermafill Package Insert2014Document1 pageDermafill Package Insert2014api-253569358No ratings yet
- Eval of Hydrogels For Bio-Printing ApplicationsDocument14 pagesEval of Hydrogels For Bio-Printing ApplicationstaylortNo ratings yet
- Wound Management and Dressing SelectionDocument6 pagesWound Management and Dressing SelectionV15CERA FK UNAND100% (1)
- Management Open FractureDocument2 pagesManagement Open FracturecatharinamNo ratings yet
- Topical Agents and Dressings For Local Burn Wound CareDocument25 pagesTopical Agents and Dressings For Local Burn Wound CareViresh Upase Roll No 130. / 8th termNo ratings yet
- What Dressing For What Wound: Prudence Lennox National Clinical Leader Healthcare Rehabilitation LTDDocument37 pagesWhat Dressing For What Wound: Prudence Lennox National Clinical Leader Healthcare Rehabilitation LTDImafighter4HimNo ratings yet
- Wound Care Dressings and Their Uses: Carolyn Watts MSN, RN, CWON Vanderbilt University Medical Center Nashville, TNDocument34 pagesWound Care Dressings and Their Uses: Carolyn Watts MSN, RN, CWON Vanderbilt University Medical Center Nashville, TNSuciNo ratings yet
- 17 4Document5 pages17 4Gunawan SadewoNo ratings yet
- Sharma Et Al. (2014) - Third Generation Materials For Wound DressingsDocument13 pagesSharma Et Al. (2014) - Third Generation Materials For Wound DressingsxtraqrkyNo ratings yet
- Skin - Grafts by Madhuri GoreDocument112 pagesSkin - Grafts by Madhuri GoreAnonymous 8hVpaQdCtr100% (1)
- MEBO Moisture and Wound HealingDocument6 pagesMEBO Moisture and Wound HealingAnonymous 8hVpaQdCtr100% (2)
- Using Antimicrobial Foam DressingsDocument1 pageUsing Antimicrobial Foam DressingsRicardo BalauNo ratings yet
- Wound Dressing: Mengapa Luka Harus Dibalut?Document3 pagesWound Dressing: Mengapa Luka Harus Dibalut?Nur RowaidahNo ratings yet
- Procedure ON Surgical Dressing: Submitted ToDocument14 pagesProcedure ON Surgical Dressing: Submitted ToRaja60% (5)
- Pressure Ulcers and Hydrocolloids Made EasyDocument6 pagesPressure Ulcers and Hydrocolloids Made EasyJefferson AlexandreNo ratings yet
- EBSCOhost 3 PDFDocument27 pagesEBSCOhost 3 PDFWawan Febri RamdaniNo ratings yet
- Optigal’s Q & A for the CLRE: Contact Lens Registry Exam Questions Basic Certification - NCLEFrom EverandOptigal’s Q & A for the CLRE: Contact Lens Registry Exam Questions Basic Certification - NCLENo ratings yet
- Screenshot 2023-10-04 at 11.54.40 AMnDocument9 pagesScreenshot 2023-10-04 at 11.54.40 AMnkhaista bachaNo ratings yet
- AUP Template NNDocument20 pagesAUP Template NNkhaista bachaNo ratings yet
- Timetable - SynergyDocument1 pageTimetable - Synergykhaista bachaNo ratings yet
- How To Pray The Rosary in 8 Easy StepsDocument7 pagesHow To Pray The Rosary in 8 Easy Stepstroylemaire100% (10)
- Impact of Orthodontic Treatment On Oral Health-Related Quality of Life in The Slovak Republic: A Cross-Sectional StudyDocument10 pagesImpact of Orthodontic Treatment On Oral Health-Related Quality of Life in The Slovak Republic: A Cross-Sectional StudyKornist BufuNo ratings yet
- NIT03 WAR Museurm PDFDocument78 pagesNIT03 WAR Museurm PDFDeepak SinghNo ratings yet
- (Q2) - Improving The Experience For Software-Measurement System End-UsersDocument25 pages(Q2) - Improving The Experience For Software-Measurement System End-UserscheikhNo ratings yet
- CB of JapanDocument11 pagesCB of JapanHema GolaniNo ratings yet
- Revision Units 4-6 Going For GoldDocument2 pagesRevision Units 4-6 Going For GoldZsuzsa StuparNo ratings yet
- 1992 - Purpose - of - Signs - and - Wonders DACARSON PDFDocument16 pages1992 - Purpose - of - Signs - and - Wonders DACARSON PDFDavid CameiraNo ratings yet
- 8 Ways To Defeat Persistent Unwanted ThoughtsDocument2 pages8 Ways To Defeat Persistent Unwanted ThoughtsE-consulting NigeriaNo ratings yet
- ADL Project TemplateDocument6 pagesADL Project TemplateOm JiNo ratings yet
- This Study Resource Was: AnswerDocument1 pageThis Study Resource Was: AnswerJoel DufaleNo ratings yet
- Lecture Notes NanomaterialsDocument34 pagesLecture Notes NanomaterialsEsther Yesudasan67% (3)
- Conjunctions: Coordinating Conjunctions Subordinating ConjunctionsDocument4 pagesConjunctions: Coordinating Conjunctions Subordinating ConjunctionsRokiah ShukerNo ratings yet
- PerDev Learning ActivityDocument4 pagesPerDev Learning ActivitydwacindyfjNo ratings yet
- Ipw WRDocument176 pagesIpw WRMay FaroukNo ratings yet
- Political Science and The Study of Politics: Presented byDocument14 pagesPolitical Science and The Study of Politics: Presented byxXUncle DrueXxNo ratings yet
- Rabagia - MatenTertiary Tectonic and Sedimentological Evolution of The South Carpathians Foredeep: Tectonic Versus Eustatic Controlco (1999)Document22 pagesRabagia - MatenTertiary Tectonic and Sedimentological Evolution of The South Carpathians Foredeep: Tectonic Versus Eustatic Controlco (1999)Lex AlexaNo ratings yet
- Shangla Girls School: Summer Camp 2019Document5 pagesShangla Girls School: Summer Camp 2019Moyz RahmanNo ratings yet
- UNIT 1 Eng FORM 5Document4 pagesUNIT 1 Eng FORM 5leonal neevedthanNo ratings yet
- No Strings AttachedDocument7 pagesNo Strings AttachedTrallo Fewdays ChibweNo ratings yet
- MTB-Lesson 3Document4 pagesMTB-Lesson 3Clavillas GrachelleNo ratings yet
- 3.6.b Relational Databases and NormalisationDocument10 pages3.6.b Relational Databases and Normalisationne002No ratings yet
- Proof by Induction - FactorialsDocument1 pageProof by Induction - FactorialsejlflopNo ratings yet
- SSRN Id4029217Document31 pagesSSRN Id4029217BAMS WIDODONo ratings yet
- R. Molski, Polish Antitrust Law in Its Fight Against Cartels - Awaiting A BreakthroughDocument28 pagesR. Molski, Polish Antitrust Law in Its Fight Against Cartels - Awaiting A Breakthroughcsair1No ratings yet
- Unit-1-Handouts LIFE 3 UNIT 1 Handout 2Document2 pagesUnit-1-Handouts LIFE 3 UNIT 1 Handout 2sanchezskiaraNo ratings yet
- EDU Development of Malaysian EducationDocument47 pagesEDU Development of Malaysian EducationNabilFikriChumiNo ratings yet
- Powerpoint By: Mohamad Sepehri, Ph.D. Jacksonville UniversityDocument31 pagesPowerpoint By: Mohamad Sepehri, Ph.D. Jacksonville UniversityNilesh DhakeNo ratings yet
- Selected Bibliography On Islam and SomaliaDocument9 pagesSelected Bibliography On Islam and SomaliaDr. Abdurahman M. Abdullahi ( baadiyow)No ratings yet