Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
11 viewsOsteoporosis: Dr. Lubna Dwerij
Osteoporosis: Dr. Lubna Dwerij
Uploaded by
Noor MajaliThis document discusses osteoporosis, including:
- It is the most prevalent bone disease and causes bone fractures. Peak bone mass is achieved between ages 18-25 and is affected by factors like nutrition and activity.
- Risk factors include small frame, menopause, medications, lack of exercise, and low calcium/vitamin D intake. Prevention focuses on optimal bone development and lifestyle modifications.
- It causes bone loss and increased fracture risk, especially of the spine, hip and wrist. Medical management includes calcium, vitamin D, bisphosphosphonates, exercise and lifestyle changes.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You might also like
- Abnormality in Little Miss SunshineDocument8 pagesAbnormality in Little Miss SunshineLaurie OuNo ratings yet
- OsteoporosisDocument33 pagesOsteoporosisCiptadi Permana Wijaya100% (1)
- The Fall by Albert CamusDocument1 pageThe Fall by Albert CamusWasi Ali0% (1)
- Total Soccer Fitness Juniors PDFDocument133 pagesTotal Soccer Fitness Juniors PDFAmelRahmanović100% (4)
- Reported by Nacito, Julie Ann T. & Tiongson, Annie Joy MDocument19 pagesReported by Nacito, Julie Ann T. & Tiongson, Annie Joy MTrixie Marie Sabile AbdullaNo ratings yet
- Osteoporosis: Done By: Dalal Hussain AlanaziDocument15 pagesOsteoporosis: Done By: Dalal Hussain AlanazidallasNo ratings yet
- OsteoporosisDocument9 pagesOsteoporosisRenuka Sivaram71% (7)
- OsteoporosisDocument16 pagesOsteoporosisDe Sesto Rhys CarloNo ratings yet
- Kelompok 6 OsteoporosisDocument10 pagesKelompok 6 OsteoporosisNur Indah FitrianaDewiNo ratings yet
- OsteoporosisDocument22 pagesOsteoporosisPrachi DSaNo ratings yet
- OsteoporosisDocument6 pagesOsteoporosiskingNo ratings yet
- OsteoporosisDocument6 pagesOsteoporosiskingNo ratings yet
- OsteoporosisDocument6 pagesOsteoporosiskingNo ratings yet
- OsteoporosisDocument6 pagesOsteoporosiskingNo ratings yet
- Dissertation OsteoporosisDocument5 pagesDissertation OsteoporosisWriteMyPaperFastCanada100% (1)
- OsteoporosisDocument11 pagesOsteoporosis906 SoNo ratings yet
- Bio Project File 2Document19 pagesBio Project File 2jiya singhNo ratings yet
- OsteoporosisDocument11 pagesOsteoporosisNisaar Jogi100% (1)
- OsteoporosisDocument6 pagesOsteoporosisabdulghaffarsp8No ratings yet
- Unit - 5 - Metabolic Bone DisordersDocument35 pagesUnit - 5 - Metabolic Bone Disorderskelemwork WaleNo ratings yet
- OsteoporosisDocument12 pagesOsteoporosisAzharul Islam ArjuNo ratings yet
- OsteoporosisDocument20 pagesOsteoporosisAsma NoreenNo ratings yet
- Osteoporosis: Causes, Incidence, and Risk FactorsDocument5 pagesOsteoporosis: Causes, Incidence, and Risk FactorsEmeka JusticeNo ratings yet
- OSTEOPOROSISDocument3 pagesOSTEOPOROSISHenry KaweesaNo ratings yet
- Osteoporosis Edited 100201092008 Phpapp02Document32 pagesOsteoporosis Edited 100201092008 Phpapp02Maya SwariNo ratings yet
- FPIDocument8 pagesFPIlloydjacksoNo ratings yet
- OsteoporosisDocument11 pagesOsteoporosisRiendraNo ratings yet
- OsteoporosisDocument43 pagesOsteoporosisMuna Hassan Mustafa100% (1)
- Osteoporosis: Signs and SymptomsDocument9 pagesOsteoporosis: Signs and SymptomschelseachoirNo ratings yet
- Sem Osteoporosis (Edit)Document31 pagesSem Osteoporosis (Edit)Rhomizal MazaliNo ratings yet
- Masculoskeletal Disorders PharmacotherapyDocument101 pagesMasculoskeletal Disorders PharmacotherapyWaaqoo Guutuu Waaqoo GuutuuNo ratings yet
- Menopause: Medical Author: Medical EditorDocument4 pagesMenopause: Medical Author: Medical EditorJanethcita SencaraNo ratings yet
- Osteoporosis: Prepared By: Md. Giash Uddin Lecturer, Dept. of Pharmacy University of ChittagongDocument30 pagesOsteoporosis: Prepared By: Md. Giash Uddin Lecturer, Dept. of Pharmacy University of Chittagongsamiul bashirNo ratings yet
- Osteoporosis Thesis PDFDocument6 pagesOsteoporosis Thesis PDFmonicabogdaneverett100% (2)
- Novartis Osteoporosis Slide KitDocument42 pagesNovartis Osteoporosis Slide KitShravanti SatyanandNo ratings yet
- Secondary Causes of OsteoporosisDocument6 pagesSecondary Causes of OsteoporosisJayaNo ratings yet
- OsteoporosisDocument11 pagesOsteoporosisAdine Jeminah LimonNo ratings yet
- Diseases and Disorders of The Skeletal SystemDocument32 pagesDiseases and Disorders of The Skeletal SystemPatrisha Georgia AmitenNo ratings yet
- What Is Osteoporosis?: Osteoposis Is A Disease ofDocument48 pagesWhat Is Osteoporosis?: Osteoposis Is A Disease ofTaruna GargNo ratings yet
- OsteoporosisDocument35 pagesOsteoporosisFarida Abo ElmagdNo ratings yet
- Blok 16 Endocrinology of OsteoporosisDocument14 pagesBlok 16 Endocrinology of OsteoporosisHasty WahyuniNo ratings yet
- OsteoporosisDocument6 pagesOsteoporosisKarla Mariana Gallegos P�rezNo ratings yet
- A. Pusey Murray (MRS) RN, Cert Psych Nursing & Nursing Admin, BSC (Hons), MPH, Dip. Ed. PHD (C)Document31 pagesA. Pusey Murray (MRS) RN, Cert Psych Nursing & Nursing Admin, BSC (Hons), MPH, Dip. Ed. PHD (C)okaciaNo ratings yet
- IbandronateDocument70 pagesIbandronateAmbreen AmirNo ratings yet
- Musculoskeletal SystemDocument60 pagesMusculoskeletal Systempetite_chien15No ratings yet
- Osteoporosis ThesisDocument5 pagesOsteoporosis Thesismaritzapetersonpaterson100% (2)
- Osteoporosis DR SawsawDocument19 pagesOsteoporosis DR SawsawNariman SternNo ratings yet
- Osteoporosis: Blondina Marpaung Rheumatology Division Internal Department Medical Faculty USU - MedanDocument47 pagesOsteoporosis: Blondina Marpaung Rheumatology Division Internal Department Medical Faculty USU - MedanFadhly SharimanNo ratings yet
- OsteomalaciaDocument28 pagesOsteomalaciaReginette Pisalbo ChanNo ratings yet
- OsteoporosisDocument33 pagesOsteoporosisNadya LiemNo ratings yet
- General - OsteoporosisDocument9 pagesGeneral - OsteoporosisAsma NazNo ratings yet
- Bone AbdallahDocument2 pagesBone Abdallahعبدالله بدرانNo ratings yet
- OsteoporosisDocument13 pagesOsteoporosisRuaa MalekNo ratings yet
- ORTHOPAEDICSDocument135 pagesORTHOPAEDICSJimmy MainaNo ratings yet
- Cooper C, Campion G, Melton LJ, 3rd. Hip Fractures in The Elderly: A World-Wide Projection. Osteoporosis Int. 1992 2 (6) :285-289Document5 pagesCooper C, Campion G, Melton LJ, 3rd. Hip Fractures in The Elderly: A World-Wide Projection. Osteoporosis Int. 1992 2 (6) :285-289Noor-E-Khadiza ShamaNo ratings yet
- Role of Exercise in Post-Menopausal WomenDocument15 pagesRole of Exercise in Post-Menopausal Womenapi-304463583No ratings yet
- TASK 1 (A)Document13 pagesTASK 1 (A)double keatNo ratings yet
- Osteoporosis Making Bones More Porous Than A Pumice StoneDocument5 pagesOsteoporosis Making Bones More Porous Than A Pumice Stoneapi-703723590No ratings yet
- Osteoporosis PDFDocument15 pagesOsteoporosis PDFعبدالرحمن علىNo ratings yet
- OsteoporosisDocument24 pagesOsteoporosisMousa SuhailNo ratings yet
- OsteoporosisDocument10 pagesOsteoporosisSandra Arely Rodriguez EscobarNo ratings yet
- Osteoporosis: How To Treat Osteoporosis: How To Prevent Osteoporosis: Along With Nutrition, Diet And Exercise For OsteoporosisFrom EverandOsteoporosis: How To Treat Osteoporosis: How To Prevent Osteoporosis: Along With Nutrition, Diet And Exercise For OsteoporosisNo ratings yet
- محاسبة 1Document37 pagesمحاسبة 1Noor MajaliNo ratings yet
- شاشات انجليزي 99 ادعولناDocument74 pagesشاشات انجليزي 99 ادعولناNoor MajaliNo ratings yet
- The Sound Patterns of LanguageDocument17 pagesThe Sound Patterns of LanguageNoor MajaliNo ratings yet
- شاشات عربي 99Document11 pagesشاشات عربي 99Noor MajaliNo ratings yet
- First Lecture - Nursing ProcessDocument57 pagesFirst Lecture - Nursing ProcessNoor MajaliNo ratings yet
- Management of Patients With Urinary Disorders: Dr. Lubna DwerijDocument74 pagesManagement of Patients With Urinary Disorders: Dr. Lubna DwerijNoor MajaliNo ratings yet
- Hepatic Cirrhosis and Hepatitis: Dr. Lubna DwerijDocument69 pagesHepatic Cirrhosis and Hepatitis: Dr. Lubna DwerijNoor MajaliNo ratings yet
- Autoimmune Processes: Dr. Lubna DwerijDocument46 pagesAutoimmune Processes: Dr. Lubna DwerijNoor MajaliNo ratings yet
- Citation 323943933Document1 pageCitation 323943933Noor MajaliNo ratings yet
- Sublingual RouteDocument5 pagesSublingual RouteRiani Dwi HastutiNo ratings yet
- Complementary Therapies in Clinical PracticeDocument8 pagesComplementary Therapies in Clinical PracticeSeva Ikhsan PambudiNo ratings yet
- Research ProposalDocument45 pagesResearch ProposalAaliyah Marie AbaoNo ratings yet
- Managing Heat StressDocument14 pagesManaging Heat StressMuhammad Aliff100% (1)
- Hye Doun Jan Feb March 08 PSDocument12 pagesHye Doun Jan Feb March 08 PSanrcinfoNo ratings yet
- Omega-3 Fatty Acid Supplements and Recurrent Miscarriage A Perspective On Potential Mechanisms and Clinical EvidenceDocument12 pagesOmega-3 Fatty Acid Supplements and Recurrent Miscarriage A Perspective On Potential Mechanisms and Clinical EvidenceRaqqi PujatmikoNo ratings yet
- EASA Mod 9A BK 1 Human Factors 1 PDFDocument75 pagesEASA Mod 9A BK 1 Human Factors 1 PDFRam C HumagainNo ratings yet
- Kenyon, E W Jesus The Healer PDFDocument1 pageKenyon, E W Jesus The Healer PDFChester Schmitz100% (1)
- Community Acquired PneumoniaDocument17 pagesCommunity Acquired PneumoniaDaniel Puentes SánchezNo ratings yet
- Degenerative Spinal DisordersDocument2 pagesDegenerative Spinal DisordersjabolbolNo ratings yet
- Prostho SR 2015Document34 pagesProstho SR 2015Arjun NarangNo ratings yet
- Ntruhs Thesis FormatDocument8 pagesNtruhs Thesis Formatheatherharveyanchorage100% (1)
- Polyphenols Health Benefits PDFDocument10 pagesPolyphenols Health Benefits PDFfather.mckenzie.twitterNo ratings yet
- Causes of Pharyngitis: Pharyngitis: A Case StudyDocument2 pagesCauses of Pharyngitis: Pharyngitis: A Case StudyRiadi riadiNo ratings yet
- Age in A Graying America: Numbers, Profiles, Trends: Nicholas Collins PA-C With Thanks To Diana Koin, M.DDocument42 pagesAge in A Graying America: Numbers, Profiles, Trends: Nicholas Collins PA-C With Thanks To Diana Koin, M.DVidya BalaNo ratings yet
- New England Journal Medicine: The ofDocument9 pagesNew England Journal Medicine: The ofalibakirNo ratings yet
- MSDS RO1 enDocument5 pagesMSDS RO1 enTito Prastyo RNo ratings yet
- MR Pulse SequencesDocument125 pagesMR Pulse SequencesdrphducNo ratings yet
- Safety and Health Protocols On Covid-19Document7 pagesSafety and Health Protocols On Covid-19Marie I. RosalesNo ratings yet
- Fundamentals of Nursing DrillDocument6 pagesFundamentals of Nursing DrillHassen Zabala100% (1)
- Tugas DR Vanda Covid 19 in Scuba DivingDocument2 pagesTugas DR Vanda Covid 19 in Scuba Divingfrd2c456ydNo ratings yet
- Tle - He (Cookery 10) Quarter 4 - Module 5 Storing MeatDocument9 pagesTle - He (Cookery 10) Quarter 4 - Module 5 Storing MeatAdine Jeminah Limon100% (1)
- Full Ebook of Cardiology Secrets 6Th Edition Glenn N Levine Online PDF All ChapterDocument69 pagesFull Ebook of Cardiology Secrets 6Th Edition Glenn N Levine Online PDF All Chaptermelaavablable100% (7)
- Pesticide PoisoningDocument34 pagesPesticide PoisoningJasmin Venus Padua100% (2)
- Validation of The Amyotrophic Lateral Sclerosis Assessment Questionnaire (ALSAQ-40) Scale in The Portuguese LanguageDocument4 pagesValidation of The Amyotrophic Lateral Sclerosis Assessment Questionnaire (ALSAQ-40) Scale in The Portuguese LanguageMCPF1No ratings yet
- Global Idiopathic Pulmonary Fibrosis Treatment MarketDocument3 pagesGlobal Idiopathic Pulmonary Fibrosis Treatment MarketiHealthcareAnalyst, Inc.No ratings yet
- Ritme Sirkadian: Suyasning HIDocument44 pagesRitme Sirkadian: Suyasning HIDedek SumantaraNo ratings yet
Osteoporosis: Dr. Lubna Dwerij
Osteoporosis: Dr. Lubna Dwerij
Uploaded by
Noor Majali0 ratings0% found this document useful (0 votes)
11 views26 pagesThis document discusses osteoporosis, including:
- It is the most prevalent bone disease and causes bone fractures. Peak bone mass is achieved between ages 18-25 and is affected by factors like nutrition and activity.
- Risk factors include small frame, menopause, medications, lack of exercise, and low calcium/vitamin D intake. Prevention focuses on optimal bone development and lifestyle modifications.
- It causes bone loss and increased fracture risk, especially of the spine, hip and wrist. Medical management includes calcium, vitamin D, bisphosphosphonates, exercise and lifestyle changes.
Original Description:
Original Title
4_5848042670122864095
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses osteoporosis, including:
- It is the most prevalent bone disease and causes bone fractures. Peak bone mass is achieved between ages 18-25 and is affected by factors like nutrition and activity.
- Risk factors include small frame, menopause, medications, lack of exercise, and low calcium/vitamin D intake. Prevention focuses on optimal bone development and lifestyle modifications.
- It causes bone loss and increased fracture risk, especially of the spine, hip and wrist. Medical management includes calcium, vitamin D, bisphosphosphonates, exercise and lifestyle changes.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
11 views26 pagesOsteoporosis: Dr. Lubna Dwerij
Osteoporosis: Dr. Lubna Dwerij
Uploaded by
Noor MajaliThis document discusses osteoporosis, including:
- It is the most prevalent bone disease and causes bone fractures. Peak bone mass is achieved between ages 18-25 and is affected by factors like nutrition and activity.
- Risk factors include small frame, menopause, medications, lack of exercise, and low calcium/vitamin D intake. Prevention focuses on optimal bone development and lifestyle modifications.
- It causes bone loss and increased fracture risk, especially of the spine, hip and wrist. Medical management includes calcium, vitamin D, bisphosphosphonates, exercise and lifestyle changes.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 26
OSTEOPOROSIS
Dr. Lubna Dwerij
OSTEOPOROSIS
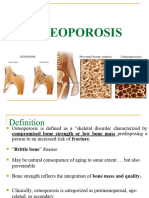
Osteoporosis is the most prevalent bone disease in the
world.
The consequence of osteoporosis is bone fracture.
Peak adult bone mass is achieved between the ages of 18
and 25 years in both females and males and is affected by
genetic factors.
Bone mass during these years is affected by nutrition,
physical activity, medications, endocrine status, and
general health.
Risk factors for osteoporosis and their effects on bone
remodeling and maintenance
Prevention
Primary osteoporosis occurs in women after menopause
(usually between the ages of 45 and 55 years) and in men
later in life, but it is not merely a consequence of aging.
Failure to develop optimal peak bone mass during
childhood, adolescence, and young adulthood contributes
to the development of osteoporosis.
Early identification of at-risk teenagers and young adults,
increased calcium intake, participation in regular weight-
bearing exercise, and modification of lifestyle (eg,
reduced use of caffeine, cigarettes, carbonated soft
drinks, and alcohol) are interventions that decrease the
risk of osteoporosis, fractures, and associated disability
later in life.
Prevention
Secondary osteoporosis is the result of medications or
other conditions and diseases that affect bone
metabolism.
The degree of osteoporosis is related to the duration of
medication therapy.
When the therapy is discontinued or the metabolic
problem is corrected, the progression of osteoporosis is
halted, but restoration of lost bone mass usually does not
occur.
Pathophysiology
Osteoporosis is characterized by reduced bone
mass, deterioration of bone matrix, and diminished
bone architectural strength.
Normal homeostatic bone turnover is altered; the
rate of bone resorption that is maintained by
osteoclasts is greater than the rate of bone
formation that is maintained by osteoblasts,
resulting in a reduced total bone mass.
The bones become progressively porous, brittle,
and fragile; they fracture easily under stresses that
would not break normal bone.
Pathophysiology
These increase susceptibility to fracture, which occur
most commonly as compression fractures of the thoracic
and lumbar spine, hip fractures, and Colles’ fractures of
the wrist.
These fractures may be the first clinical manifestation of
osteoporosis
Pathophysiology
The gradual collapse of a vertebra may be
asymptomatic; it is observed as progressive kyphosis.
With the development of kyphosis ,there is an
associated loss of height.
Women develop osteoporosis more frequently and more
extensively than men because of lower peak bone mass
and the effect of estrogen loss during menopause.
The withdrawal of estrogens at menopause or with
oophorectomy causes an accelerated bone resorption
Risk Factors
Small-framed, nonobese Caucasian women are at greatest
risk for osteoporosis.
Asian women of slight build are at risk for low peak BMD.
African American women, who have a greater bone mass
than Caucasian women, are less susceptible to
osteoporosis.
Men have a greater peak bone mass and do not experience
sudden estrogen reduction.
As a result, osteoporosis occurs in men at a lower rate and
at an older age (about one decade later).
It is believed that testosterone and estrogen are important
in achieving and maintaining bone mass in men.
Risk Factors
Nutritional factors contribute to the development of
osteoporosis.
A diet that includes adequate calories and nutrients
needed to maintain bone, calcium, and vitamin D must be
consumed.
Vitamin D is necessary for calcium absorption and for
normal bone mineralization.
Dietary calcium and vitamin D must be adequate to
maintain bone remodeling and body functions.
The best source of calcium and vitamin D is fortified milk.
A cup of milk or calcium-fortified orange juice contains
about 300 mg of calcium.
Risk Factors
The recommended adequate intake (RAI) level of calcium
for all individuals is 1000 to 1200 mg daily
The recommended vitamin D intake for adults 50 years of
age and older is 800 to 1000 international units (IU) daily.
Bone formation is enhanced by the stress of weight and
muscle activity. Resistance and impact exercises are most
beneficial in developing and maintaining bone mass.
Immobility contributes to the development of
osteoporosis.
When immobilized by casts, general inactivity, paralysis,
or other disability, the bone is resorbed faster than it is
formed, and osteoporosis results.
Assessment and Diagnostic Findings
Osteoporosis may be undetectable on routine x-rays until
there has been 25% to 40% demineralization.
Osteoporosis is diagnosed by dual-energy x-ray
absorptiometry (DXA), which provides information about
bone mineral density (BMD) at the spine and hip.
BMD testing is recommended for:
All women older than 65 years of age.
For all men older than 70 years of age.
For postmenopausal women and men older than 50 years
of age with osteoporosis risk factors, and
For all people who have had a fracture thought to occur as
a consequence of osteoporosis
Assessment and Diagnostic Findings
Laboratory studies (eg, serum calcium, serum phosphate,
serum alkaline phosphatase, urine calcium excretion,
urinary hydroxyproline excretion, hematocrit, erythrocyte
sedimentation rate [ESR]) and x-ray studies are used to
exclude other possible disorders (eg, multiple myeloma,
osteomalacia, hyperparathyroidism, malignancy) that
contribute to bone loss.
Medical Management
A diet rich in calcium and vitamin D throughout life, with
an increased calcium intake during adolescence, young
adulthood, and the middle years, protects against skeletal
demineralization.
Regular weight-bearing exercise promotes bone formation.
From 20 to 30 minutes of aerobic exercise (eg, walking), 3
days or more a week, is recommended.
Medical Management
Pharmacologic Therapy
The first-line medications used to treat and prevent
osteoporosis include calcium and vitamin D supplements
and bisphosphonates.
Common side effects of calcium supplements are
abdominal distention and constipation.
Other medications that might be prescribed after these
medications are tried include calcitonin, selective
estrogen receptor modulators, and anabolic agents.
Medical Management
Pharmacologic Therapy
Bisphosphonates increase bone mass and decrease bone
loss by inhibiting osteoclast function.
These medications have demonstrated cost-effectiveness
in preventing osteoporotic-related fractures.
Adequate calcium and vitamin D intake is needed for
maximum effect, but these supplements should not be
taken at the same time of day as bisphosphonates.
Side effects of bisphosphonates include gastrointestinal
symptoms (eg, dyspepsia, nausea, flatulence, diarrhea,
constipation).
Medical Management
Pharmacologic Therapy
Some patients may develop esophageal ulcers, gastric
ulcers, or osteonecrosis of the jaw related to
bisphosphonate use.
Patients who take oral bisphosphonates must take these
medications on an empty stomach on arising in the
morning with a full glass of water and must sit upright for
30 to 60 minutes after their administration.
Medical Management
Pharmacologic Therapy
Calcitonin (Miacalcin) directly inhibits osteoclasts, thereby
reducing bone loss and increasing BMD.
Calcitonin is administered by nasal spray or by
subcutaneous or intramuscular injection.
It should not be prescribed for patients with seafood
allergies.
Medical Management
Fracture Management
Fractures of the hip that occur as a consequence of
osteoporosis are managed surgically by joint replacement
or by closed or open reduction with internal fixation.
Patients need to be evaluated for osteoporosis and
treated, as indicated, in order to prevent additional
fractures.
Pharmacologic and dietary treatments are aimed at
increasing vertebral bone density.
NURSING PROCESS
Assessment
Health promotion, identification of people at risk for
osteoporosis, and recognition of problems associated with
osteoporosis form the basis for nursing assessment.
The health history includes questions focuses on:
Family history, previous fractures, dietary consumption of
calcium.
Exercise patterns, onset of menopause.
Use of corticosteroids as well as alcohol, smoking, and
caffeine intake.
Physical examination may disclose a fracture, kyphosis of
the thoracic spine, or shortened stature.
Nursing Diagnoses
Deficient knowledge about the osteoporotic process and
treatment regimen
Acute pain related to fracture and muscle spasm.
Risk for constipation related to immobility or development
of ileus (intestinal obstruction).
Risk for injury: additional fractures related to
osteoporosis.
Nursing Interventions
Promoting Understanding of Osteoporosis and the
Treatment Regimen
Patient teaching focuses on factors influencing the
development of osteoporosis, interventions to arrest or
slow the process, and measures to relieve symptoms.
It is emphasized that all people continue to need
sufficient calcium, vitamin D, and weight-bearing exercise
to slow the progression of osteoporosis.
Patient teaching related to medication therapy is
important.
Nursing Interventions
Relieving Pain
Relief of back pain resulting from compression fracture
may be accomplished by resting in bed in a supine or side-
lying position several times a day.
The mattress should be firm.
Knee flexion increases comfort by relaxing back muscles.
Intermittent local heat and back rubs promote muscle
relaxation.
The nurse encourages good posture and teaches body
mechanics.
When the patient is assisted out of bed, a trunk orthosis
(eg, lumbosacral corset) may be worn for temporary
support and immobilization.
Nursing Interventions
Improving Bowel Elimination
Constipation is a problem related to immobility and
medications. Early institution of a high-fiber diet,
increased fluids, and the use of prescribed stool softeners
help prevent or minimize constipation.
If the vertebral collapse involves the T10–L2 vertebrae,
the patient may develop a paralytic ileus.
The nurse therefore monitors the patient’s intake, bowel
sounds, and bowel activity.
Reference
Hinkle, J. L., & Cheever, K. H. (2014). Brunner & Suddarth's textbook of
medical-surgical nursing (Edition 13.). Wolters Kluwer Health/Lippincott
Williams & Wilkins.
You might also like
- Abnormality in Little Miss SunshineDocument8 pagesAbnormality in Little Miss SunshineLaurie OuNo ratings yet
- OsteoporosisDocument33 pagesOsteoporosisCiptadi Permana Wijaya100% (1)
- The Fall by Albert CamusDocument1 pageThe Fall by Albert CamusWasi Ali0% (1)
- Total Soccer Fitness Juniors PDFDocument133 pagesTotal Soccer Fitness Juniors PDFAmelRahmanović100% (4)
- Reported by Nacito, Julie Ann T. & Tiongson, Annie Joy MDocument19 pagesReported by Nacito, Julie Ann T. & Tiongson, Annie Joy MTrixie Marie Sabile AbdullaNo ratings yet
- Osteoporosis: Done By: Dalal Hussain AlanaziDocument15 pagesOsteoporosis: Done By: Dalal Hussain AlanazidallasNo ratings yet
- OsteoporosisDocument9 pagesOsteoporosisRenuka Sivaram71% (7)
- OsteoporosisDocument16 pagesOsteoporosisDe Sesto Rhys CarloNo ratings yet
- Kelompok 6 OsteoporosisDocument10 pagesKelompok 6 OsteoporosisNur Indah FitrianaDewiNo ratings yet
- OsteoporosisDocument22 pagesOsteoporosisPrachi DSaNo ratings yet
- OsteoporosisDocument6 pagesOsteoporosiskingNo ratings yet
- OsteoporosisDocument6 pagesOsteoporosiskingNo ratings yet
- OsteoporosisDocument6 pagesOsteoporosiskingNo ratings yet
- OsteoporosisDocument6 pagesOsteoporosiskingNo ratings yet
- Dissertation OsteoporosisDocument5 pagesDissertation OsteoporosisWriteMyPaperFastCanada100% (1)
- OsteoporosisDocument11 pagesOsteoporosis906 SoNo ratings yet
- Bio Project File 2Document19 pagesBio Project File 2jiya singhNo ratings yet
- OsteoporosisDocument11 pagesOsteoporosisNisaar Jogi100% (1)
- OsteoporosisDocument6 pagesOsteoporosisabdulghaffarsp8No ratings yet
- Unit - 5 - Metabolic Bone DisordersDocument35 pagesUnit - 5 - Metabolic Bone Disorderskelemwork WaleNo ratings yet
- OsteoporosisDocument12 pagesOsteoporosisAzharul Islam ArjuNo ratings yet
- OsteoporosisDocument20 pagesOsteoporosisAsma NoreenNo ratings yet
- Osteoporosis: Causes, Incidence, and Risk FactorsDocument5 pagesOsteoporosis: Causes, Incidence, and Risk FactorsEmeka JusticeNo ratings yet
- OSTEOPOROSISDocument3 pagesOSTEOPOROSISHenry KaweesaNo ratings yet
- Osteoporosis Edited 100201092008 Phpapp02Document32 pagesOsteoporosis Edited 100201092008 Phpapp02Maya SwariNo ratings yet
- FPIDocument8 pagesFPIlloydjacksoNo ratings yet
- OsteoporosisDocument11 pagesOsteoporosisRiendraNo ratings yet
- OsteoporosisDocument43 pagesOsteoporosisMuna Hassan Mustafa100% (1)
- Osteoporosis: Signs and SymptomsDocument9 pagesOsteoporosis: Signs and SymptomschelseachoirNo ratings yet
- Sem Osteoporosis (Edit)Document31 pagesSem Osteoporosis (Edit)Rhomizal MazaliNo ratings yet
- Masculoskeletal Disorders PharmacotherapyDocument101 pagesMasculoskeletal Disorders PharmacotherapyWaaqoo Guutuu Waaqoo GuutuuNo ratings yet
- Menopause: Medical Author: Medical EditorDocument4 pagesMenopause: Medical Author: Medical EditorJanethcita SencaraNo ratings yet
- Osteoporosis: Prepared By: Md. Giash Uddin Lecturer, Dept. of Pharmacy University of ChittagongDocument30 pagesOsteoporosis: Prepared By: Md. Giash Uddin Lecturer, Dept. of Pharmacy University of Chittagongsamiul bashirNo ratings yet
- Osteoporosis Thesis PDFDocument6 pagesOsteoporosis Thesis PDFmonicabogdaneverett100% (2)
- Novartis Osteoporosis Slide KitDocument42 pagesNovartis Osteoporosis Slide KitShravanti SatyanandNo ratings yet
- Secondary Causes of OsteoporosisDocument6 pagesSecondary Causes of OsteoporosisJayaNo ratings yet
- OsteoporosisDocument11 pagesOsteoporosisAdine Jeminah LimonNo ratings yet
- Diseases and Disorders of The Skeletal SystemDocument32 pagesDiseases and Disorders of The Skeletal SystemPatrisha Georgia AmitenNo ratings yet
- What Is Osteoporosis?: Osteoposis Is A Disease ofDocument48 pagesWhat Is Osteoporosis?: Osteoposis Is A Disease ofTaruna GargNo ratings yet
- OsteoporosisDocument35 pagesOsteoporosisFarida Abo ElmagdNo ratings yet
- Blok 16 Endocrinology of OsteoporosisDocument14 pagesBlok 16 Endocrinology of OsteoporosisHasty WahyuniNo ratings yet
- OsteoporosisDocument6 pagesOsteoporosisKarla Mariana Gallegos P�rezNo ratings yet
- A. Pusey Murray (MRS) RN, Cert Psych Nursing & Nursing Admin, BSC (Hons), MPH, Dip. Ed. PHD (C)Document31 pagesA. Pusey Murray (MRS) RN, Cert Psych Nursing & Nursing Admin, BSC (Hons), MPH, Dip. Ed. PHD (C)okaciaNo ratings yet
- IbandronateDocument70 pagesIbandronateAmbreen AmirNo ratings yet
- Musculoskeletal SystemDocument60 pagesMusculoskeletal Systempetite_chien15No ratings yet
- Osteoporosis ThesisDocument5 pagesOsteoporosis Thesismaritzapetersonpaterson100% (2)
- Osteoporosis DR SawsawDocument19 pagesOsteoporosis DR SawsawNariman SternNo ratings yet
- Osteoporosis: Blondina Marpaung Rheumatology Division Internal Department Medical Faculty USU - MedanDocument47 pagesOsteoporosis: Blondina Marpaung Rheumatology Division Internal Department Medical Faculty USU - MedanFadhly SharimanNo ratings yet
- OsteomalaciaDocument28 pagesOsteomalaciaReginette Pisalbo ChanNo ratings yet
- OsteoporosisDocument33 pagesOsteoporosisNadya LiemNo ratings yet
- General - OsteoporosisDocument9 pagesGeneral - OsteoporosisAsma NazNo ratings yet
- Bone AbdallahDocument2 pagesBone Abdallahعبدالله بدرانNo ratings yet
- OsteoporosisDocument13 pagesOsteoporosisRuaa MalekNo ratings yet
- ORTHOPAEDICSDocument135 pagesORTHOPAEDICSJimmy MainaNo ratings yet
- Cooper C, Campion G, Melton LJ, 3rd. Hip Fractures in The Elderly: A World-Wide Projection. Osteoporosis Int. 1992 2 (6) :285-289Document5 pagesCooper C, Campion G, Melton LJ, 3rd. Hip Fractures in The Elderly: A World-Wide Projection. Osteoporosis Int. 1992 2 (6) :285-289Noor-E-Khadiza ShamaNo ratings yet
- Role of Exercise in Post-Menopausal WomenDocument15 pagesRole of Exercise in Post-Menopausal Womenapi-304463583No ratings yet
- TASK 1 (A)Document13 pagesTASK 1 (A)double keatNo ratings yet
- Osteoporosis Making Bones More Porous Than A Pumice StoneDocument5 pagesOsteoporosis Making Bones More Porous Than A Pumice Stoneapi-703723590No ratings yet
- Osteoporosis PDFDocument15 pagesOsteoporosis PDFعبدالرحمن علىNo ratings yet
- OsteoporosisDocument24 pagesOsteoporosisMousa SuhailNo ratings yet
- OsteoporosisDocument10 pagesOsteoporosisSandra Arely Rodriguez EscobarNo ratings yet
- Osteoporosis: How To Treat Osteoporosis: How To Prevent Osteoporosis: Along With Nutrition, Diet And Exercise For OsteoporosisFrom EverandOsteoporosis: How To Treat Osteoporosis: How To Prevent Osteoporosis: Along With Nutrition, Diet And Exercise For OsteoporosisNo ratings yet
- محاسبة 1Document37 pagesمحاسبة 1Noor MajaliNo ratings yet
- شاشات انجليزي 99 ادعولناDocument74 pagesشاشات انجليزي 99 ادعولناNoor MajaliNo ratings yet
- The Sound Patterns of LanguageDocument17 pagesThe Sound Patterns of LanguageNoor MajaliNo ratings yet
- شاشات عربي 99Document11 pagesشاشات عربي 99Noor MajaliNo ratings yet
- First Lecture - Nursing ProcessDocument57 pagesFirst Lecture - Nursing ProcessNoor MajaliNo ratings yet
- Management of Patients With Urinary Disorders: Dr. Lubna DwerijDocument74 pagesManagement of Patients With Urinary Disorders: Dr. Lubna DwerijNoor MajaliNo ratings yet
- Hepatic Cirrhosis and Hepatitis: Dr. Lubna DwerijDocument69 pagesHepatic Cirrhosis and Hepatitis: Dr. Lubna DwerijNoor MajaliNo ratings yet
- Autoimmune Processes: Dr. Lubna DwerijDocument46 pagesAutoimmune Processes: Dr. Lubna DwerijNoor MajaliNo ratings yet
- Citation 323943933Document1 pageCitation 323943933Noor MajaliNo ratings yet
- Sublingual RouteDocument5 pagesSublingual RouteRiani Dwi HastutiNo ratings yet
- Complementary Therapies in Clinical PracticeDocument8 pagesComplementary Therapies in Clinical PracticeSeva Ikhsan PambudiNo ratings yet
- Research ProposalDocument45 pagesResearch ProposalAaliyah Marie AbaoNo ratings yet
- Managing Heat StressDocument14 pagesManaging Heat StressMuhammad Aliff100% (1)
- Hye Doun Jan Feb March 08 PSDocument12 pagesHye Doun Jan Feb March 08 PSanrcinfoNo ratings yet
- Omega-3 Fatty Acid Supplements and Recurrent Miscarriage A Perspective On Potential Mechanisms and Clinical EvidenceDocument12 pagesOmega-3 Fatty Acid Supplements and Recurrent Miscarriage A Perspective On Potential Mechanisms and Clinical EvidenceRaqqi PujatmikoNo ratings yet
- EASA Mod 9A BK 1 Human Factors 1 PDFDocument75 pagesEASA Mod 9A BK 1 Human Factors 1 PDFRam C HumagainNo ratings yet
- Kenyon, E W Jesus The Healer PDFDocument1 pageKenyon, E W Jesus The Healer PDFChester Schmitz100% (1)
- Community Acquired PneumoniaDocument17 pagesCommunity Acquired PneumoniaDaniel Puentes SánchezNo ratings yet
- Degenerative Spinal DisordersDocument2 pagesDegenerative Spinal DisordersjabolbolNo ratings yet
- Prostho SR 2015Document34 pagesProstho SR 2015Arjun NarangNo ratings yet
- Ntruhs Thesis FormatDocument8 pagesNtruhs Thesis Formatheatherharveyanchorage100% (1)
- Polyphenols Health Benefits PDFDocument10 pagesPolyphenols Health Benefits PDFfather.mckenzie.twitterNo ratings yet
- Causes of Pharyngitis: Pharyngitis: A Case StudyDocument2 pagesCauses of Pharyngitis: Pharyngitis: A Case StudyRiadi riadiNo ratings yet
- Age in A Graying America: Numbers, Profiles, Trends: Nicholas Collins PA-C With Thanks To Diana Koin, M.DDocument42 pagesAge in A Graying America: Numbers, Profiles, Trends: Nicholas Collins PA-C With Thanks To Diana Koin, M.DVidya BalaNo ratings yet
- New England Journal Medicine: The ofDocument9 pagesNew England Journal Medicine: The ofalibakirNo ratings yet
- MSDS RO1 enDocument5 pagesMSDS RO1 enTito Prastyo RNo ratings yet
- MR Pulse SequencesDocument125 pagesMR Pulse SequencesdrphducNo ratings yet
- Safety and Health Protocols On Covid-19Document7 pagesSafety and Health Protocols On Covid-19Marie I. RosalesNo ratings yet
- Fundamentals of Nursing DrillDocument6 pagesFundamentals of Nursing DrillHassen Zabala100% (1)
- Tugas DR Vanda Covid 19 in Scuba DivingDocument2 pagesTugas DR Vanda Covid 19 in Scuba Divingfrd2c456ydNo ratings yet
- Tle - He (Cookery 10) Quarter 4 - Module 5 Storing MeatDocument9 pagesTle - He (Cookery 10) Quarter 4 - Module 5 Storing MeatAdine Jeminah Limon100% (1)
- Full Ebook of Cardiology Secrets 6Th Edition Glenn N Levine Online PDF All ChapterDocument69 pagesFull Ebook of Cardiology Secrets 6Th Edition Glenn N Levine Online PDF All Chaptermelaavablable100% (7)
- Pesticide PoisoningDocument34 pagesPesticide PoisoningJasmin Venus Padua100% (2)
- Validation of The Amyotrophic Lateral Sclerosis Assessment Questionnaire (ALSAQ-40) Scale in The Portuguese LanguageDocument4 pagesValidation of The Amyotrophic Lateral Sclerosis Assessment Questionnaire (ALSAQ-40) Scale in The Portuguese LanguageMCPF1No ratings yet
- Global Idiopathic Pulmonary Fibrosis Treatment MarketDocument3 pagesGlobal Idiopathic Pulmonary Fibrosis Treatment MarketiHealthcareAnalyst, Inc.No ratings yet
- Ritme Sirkadian: Suyasning HIDocument44 pagesRitme Sirkadian: Suyasning HIDedek SumantaraNo ratings yet