Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
1 viewsMSC Med Micro Antimicrobial Agents 2
MSC Med Micro Antimicrobial Agents 2
Uploaded by
Shalini MThis document discusses various drug sensitivity tests that can be used to determine whether a microorganism is susceptible or resistant to antimicrobial agents. It describes methods such as antibiotic disc assays, test tube dilution tests, cylinder plate tests, E-tests, and molecular tests. Factors that can influence test results are temperature, incubation period, inoculum size, and medium used. The minimum inhibitory concentration (MIC) is discussed as the lowest drug concentration that prevents microbial growth. Assays can be performed directly on body fluids to determine susceptibility of pathogens. Probiotics and various probiotic strains and their therapeutic uses are also summarized.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You might also like
- Koji BiroreactorsDocument11 pagesKoji BiroreactorsShalini MNo ratings yet
- Antibiotic Sensitivity TestingDocument18 pagesAntibiotic Sensitivity TestingMeeJames100% (1)
- Anti Microbial Chemotherapy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDocument41 pagesAnti Microbial Chemotherapy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDr. Ashish JawarkarNo ratings yet
- Antibiotic Susceptibility Testing: A Review On Current PracticesDocument8 pagesAntibiotic Susceptibility Testing: A Review On Current PracticesAndriano Arie WibowoNo ratings yet
- Antibiotic Sensitivity TestDocument4 pagesAntibiotic Sensitivity TestAll new MovieshubNo ratings yet
- Biology Investigatory Project: The Study of Effects of Antibiotics On Micro-OrganismsDocument13 pagesBiology Investigatory Project: The Study of Effects of Antibiotics On Micro-OrganismsSamanwitha SharmaNo ratings yet
- Group 4 Antibiotic Sensitivity TestingDocument8 pagesGroup 4 Antibiotic Sensitivity TestingJe Michelle LoayonNo ratings yet
- Bacteriology: Principles of Antimicrobial ActionDocument35 pagesBacteriology: Principles of Antimicrobial ActionggemalynNo ratings yet
- Sensitivity TestDocument16 pagesSensitivity Testmarkwillaz100% (1)
- Antimicrobial Agents: Basic Principles of Antimicrobial TherapyDocument10 pagesAntimicrobial Agents: Basic Principles of Antimicrobial TherapyMarku LeeNo ratings yet
- Antibiotic Susceptibility TestsDocument18 pagesAntibiotic Susceptibility Testsمحمد رحيم حسن محمودNo ratings yet
- Introduction To Techniques in MicrobiologyDocument4 pagesIntroduction To Techniques in MicrobiologyYusnita Damayanti100% (1)
- Antibiotics: Rodel L. Saludares Mario S. Abendanio Hazel M. Dela Cruz Lea Diane Dela Cruz Jicka TagubaDocument51 pagesAntibiotics: Rodel L. Saludares Mario S. Abendanio Hazel M. Dela Cruz Lea Diane Dela Cruz Jicka TagubaVer Garcera TalosigNo ratings yet
- Medical Microbiology: Class: 2Document3 pagesMedical Microbiology: Class: 2S ANo ratings yet
- Presentation 1Document20 pagesPresentation 1Sneha BagulNo ratings yet
- A6 Antimicrobial AgentsDocument61 pagesA6 Antimicrobial AgentsSHIELOU LOMODNo ratings yet
- Antibiotic Susceptibility Testing: NotesDocument12 pagesAntibiotic Susceptibility Testing: NotesKania Putri D 113No ratings yet
- Antimicrobial Susceptibility Testing (AST)Document41 pagesAntimicrobial Susceptibility Testing (AST)summiya100% (1)
- Link Between MIC and Antimicrobial TherapyDocument8 pagesLink Between MIC and Antimicrobial TherapySahar WaqarNo ratings yet
- Antibiotic Susceptibility TestingDocument12 pagesAntibiotic Susceptibility TestingOsama BakheetNo ratings yet
- Microbiological AssaysDocument34 pagesMicrobiological Assayspradeepbawane60% (5)
- Laboratory 6 - AntimicrobialsDocument4 pagesLaboratory 6 - AntimicrobialsLuzzuvannaNo ratings yet
- Antimicrobial Susceptibilty TestingDocument47 pagesAntimicrobial Susceptibilty TestingpixholicNo ratings yet
- Lab Report Antimicrobial Susceptibility Testing MethodsDocument19 pagesLab Report Antimicrobial Susceptibility Testing MethodsAlyaa Athira100% (1)
- Mic, MBC and Mic Cutoff ValueDocument23 pagesMic, MBC and Mic Cutoff ValueDiksha DahalNo ratings yet
- تينقتلا طسولاا ثارفلا تعماج تفوك/ تيبطلاو تيحصلا ثاينقتلا تيلك تيبطلا ثاربتخملا ثاينقت مسق: ةدام Diagnostic Microbiology تعبارلا تلحرملاDocument19 pagesتينقتلا طسولاا ثارفلا تعماج تفوك/ تيبطلاو تيحصلا ثاينقتلا تيلك تيبطلا ثاربتخملا ثاينقت مسق: ةدام Diagnostic Microbiology تعبارلا تلحرملاAli M. AtshanNo ratings yet
- In Campus Micro Exp.6 2022Document17 pagesIn Campus Micro Exp.6 2022oking4831No ratings yet
- Biology Investigatory Project 2022-2023Document22 pagesBiology Investigatory Project 2022-2023Sneha Bagul50% (2)
- Biology Project XiiDocument14 pagesBiology Project XiiSagayaraniNo ratings yet
- Dokumen - Tips Biology Investigatory Project 561e79b91f5a0Document17 pagesDokumen - Tips Biology Investigatory Project 561e79b91f5a0Upendra LalNo ratings yet
- Ast Booklet GB Final PDFDocument19 pagesAst Booklet GB Final PDFAhmed GaberNo ratings yet
- Central AcademyDocument17 pagesCentral AcademyKartikey VermaNo ratings yet
- Antibiotic Sensitivity TestDocument2 pagesAntibiotic Sensitivity Testganesh2gigNo ratings yet
- Infectious Pharmacology 01Document19 pagesInfectious Pharmacology 01Arthur YanezNo ratings yet
- Biology Project ReportDocument15 pagesBiology Project ReportOmsai GarNo ratings yet
- Pharmacology Unit 2 Antimicrobial DrugsDocument62 pagesPharmacology Unit 2 Antimicrobial DrugsAsif Ali LashariNo ratings yet
- Fdocuments - in Biology Investigatory Project 561e79b91f5a0Document18 pagesFdocuments - in Biology Investigatory Project 561e79b91f5a0ASHOKNo ratings yet
- SuperbugsDocument3 pagesSuperbugsMatei BuneaNo ratings yet
- The Roles and FunctionsDocument2 pagesThe Roles and Functionssyed hafizNo ratings yet
- INDEXDocument16 pagesINDEXayush rajeshNo ratings yet
- Antimicrobial Susceptibility Testing FK 2012Document32 pagesAntimicrobial Susceptibility Testing FK 2012Sheryl Elita100% (1)
- 6.1 Antibiotic Fermentation 1 PDFDocument26 pages6.1 Antibiotic Fermentation 1 PDFdenojsNo ratings yet
- Anti Micro Biii AlDocument7 pagesAnti Micro Biii AltimiiniyiiNo ratings yet
- The Role of Clinical Pharmacist in Combating Antibiotic ResistanceDocument4 pagesThe Role of Clinical Pharmacist in Combating Antibiotic ResistanceAnto BijuNo ratings yet
- Probiotik Mengurangi Resistensi AntibiotikDocument34 pagesProbiotik Mengurangi Resistensi AntibiotikviaNo ratings yet
- Biology ProjectDocument28 pagesBiology ProjectKanak MirpouriNo ratings yet
- Antimicrobial Susceptibility 4.3Document22 pagesAntimicrobial Susceptibility 4.3Maxwell C Jay KafwaniNo ratings yet
- Principles of Bacterial Infections and Anti-Infectives: Cause, Pathogenicity, and VirulenceDocument29 pagesPrinciples of Bacterial Infections and Anti-Infectives: Cause, Pathogenicity, and Virulencejheannie02100% (1)
- AntibioticsDocument49 pagesAntibioticsShriefElghazalyNo ratings yet
- Experiment 10Document2 pagesExperiment 10Mark Janssen CustodioNo ratings yet
- 2009-Antimicrobial SusceptilityDocument7 pages2009-Antimicrobial SusceptilityStephanie MurillejoNo ratings yet
- A6 Antimicrobial AgentsDocument61 pagesA6 Antimicrobial AgentsRIK HAROLD GATPANDANNo ratings yet
- Unit-II Lecture-IV Antibiotics by ZebDocument84 pagesUnit-II Lecture-IV Antibiotics by ZebImad khanNo ratings yet
- Unit 4, Pharmaceutical Engineering, B Pharmacy 3rd Sem, Carewell PharmaDocument4 pagesUnit 4, Pharmaceutical Engineering, B Pharmacy 3rd Sem, Carewell PharmaAjay KNo ratings yet
- Yuvraj BiologyDocument19 pagesYuvraj BiologyAnkit KashyapNo ratings yet
- Antibiotics Lloyd ADocument11 pagesAntibiotics Lloyd AAndrew Lloyd100% (1)
- Clinical Microbiology and ImmunologyDocument7 pagesClinical Microbiology and ImmunologyGwyn CervantesNo ratings yet
- Bacteriology - Chapter Six Antibiotics - Protein Synthesis, Nucleic Acid Synthesis and MetabolismDocument6 pagesBacteriology - Chapter Six Antibiotics - Protein Synthesis, Nucleic Acid Synthesis and MetabolismZeth MoturiNo ratings yet
- Presentation 1Document25 pagesPresentation 1Sneha BagulNo ratings yet
- Principles of Antimicrobial UseDocument5 pagesPrinciples of Antimicrobial Usegayleteguichan19No ratings yet
- Definitions:: Meaning of DelegationDocument9 pagesDefinitions:: Meaning of DelegationShalini MNo ratings yet
- Gibberellic AcidDocument17 pagesGibberellic AcidShalini MNo ratings yet
- Plant Growth RegulatorsDocument33 pagesPlant Growth RegulatorsShalini MNo ratings yet
- Patent - Laws and Procedure - Aneesh MarballiDocument29 pagesPatent - Laws and Procedure - Aneesh MarballiShalini MNo ratings yet
- Frankia SeminarDocument20 pagesFrankia SeminarShalini M100% (1)
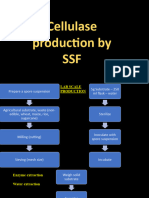
- Cellulase Production by SSFDocument9 pagesCellulase Production by SSFShalini MNo ratings yet
- Penicillin Production by Solid State FermentationDocument5 pagesPenicillin Production by Solid State FermentationShalini MNo ratings yet
- Barriers To EntreprenwurshipDocument7 pagesBarriers To EntreprenwurshipShalini MNo ratings yet
- eSTIMATION OF GROWTH in SSFDocument9 pageseSTIMATION OF GROWTH in SSFShalini MNo ratings yet
- Sterilization of Fermenter-1Document11 pagesSterilization of Fermenter-1Shalini M100% (1)
- SSF Bioreactor SystemsDocument26 pagesSSF Bioreactor SystemsShalini MNo ratings yet
- Biofertilizers (Microbial Inoculants)Document10 pagesBiofertilizers (Microbial Inoculants)Shalini MNo ratings yet
- Materi DR DR Ari Prayitno SpAK Typhoid Vaccine - Current and New PlatformDocument40 pagesMateri DR DR Ari Prayitno SpAK Typhoid Vaccine - Current and New PlatformMutiara UtiNo ratings yet
- The Immune SystemDocument29 pagesThe Immune SystemLalajimNo ratings yet
- Plant Vaccines: An Overview: Gaurav Kumar Karthik LoganathanDocument16 pagesPlant Vaccines: An Overview: Gaurav Kumar Karthik LoganathanMayank BahugunaNo ratings yet
- Global Manual Revised 12102015Document124 pagesGlobal Manual Revised 12102015Ishak Abdul GafarNo ratings yet
- Vaccines Science PharmaDocument30 pagesVaccines Science PharmaGanesh V GaonkarNo ratings yet
- Meningitis Bacteriana Aguda en El AdultoDocument12 pagesMeningitis Bacteriana Aguda en El AdultoJulian AlbarracínNo ratings yet
- Global Manual On Surveillance of AEFIDocument128 pagesGlobal Manual On Surveillance of AEFIHarold JeffersonNo ratings yet
- IMMUNOPROPHYLAXISDocument30 pagesIMMUNOPROPHYLAXISAli TARARNo ratings yet
- Impact of Pneumococcal Conjugate Vaccine in At-Risk Adults 2022Document48 pagesImpact of Pneumococcal Conjugate Vaccine in At-Risk Adults 2022Rosi AmaliaNo ratings yet
- Community Health Nursing Doh Related Programs: Epi - Types of VaccinesDocument32 pagesCommunity Health Nursing Doh Related Programs: Epi - Types of VaccinesAngelaNo ratings yet
- Immunization Manual For Medical and Nursing Students - Final Smaller PDFDocument296 pagesImmunization Manual For Medical and Nursing Students - Final Smaller PDFamit100% (3)
- Types of VaccinesDocument2 pagesTypes of VaccinesErika Bea PaculanangNo ratings yet
- IMUNOPROFILAKTIKDocument26 pagesIMUNOPROFILAKTIKSatriyo K. PalgunoNo ratings yet
- Biologics, Immunology and PharmacognosyDocument26 pagesBiologics, Immunology and PharmacognosyShereenNo ratings yet
- CHN211 Week 7 WORD - National Immunization ProgramDocument35 pagesCHN211 Week 7 WORD - National Immunization ProgramChesca DomingoNo ratings yet
- Pentaxim-Pi-Sg Pen 0118 Spc0914Document10 pagesPentaxim-Pi-Sg Pen 0118 Spc0914walkrogNo ratings yet
- IAS Exam Congress: IasecDocument22 pagesIAS Exam Congress: IasecNandita NanditaNo ratings yet
- VaccinesDocument17 pagesVaccinesYOGANANTH mscasNo ratings yet
- Immunosuppressants NotesDocument20 pagesImmunosuppressants NotesmadcalNo ratings yet
- Immunization CTP March 2021 4-Per-PageDocument71 pagesImmunization CTP March 2021 4-Per-PageAssal Al JanabiNo ratings yet
- Different Types of VaccinesDocument2 pagesDifferent Types of VaccinesBhuvaneshNo ratings yet
- Lab Technologist-3Document92 pagesLab Technologist-3AHAMED SHIFAAN100% (1)
- MODULE 2: Types of Vaccine and Adverse ReactionsDocument29 pagesMODULE 2: Types of Vaccine and Adverse ReactionsnandaNo ratings yet
- Immunization CTP July 2020 4-Per-PageDocument70 pagesImmunization CTP July 2020 4-Per-Pagejose carlos gonzalezNo ratings yet
- Types of VaccinesDocument3 pagesTypes of Vaccineshaddi awanNo ratings yet
- ImmunisationDocument42 pagesImmunisationDr. Ajeta GuptaNo ratings yet
- Immunological ProductsDocument19 pagesImmunological ProductsPharma 24No ratings yet
- Typbar TCV Package InsertDocument1 pageTypbar TCV Package Insertjossy123456No ratings yet
- 7) Preventive Health and EPIDocument51 pages7) Preventive Health and EPIDr. Zirwa AsimNo ratings yet
- Community Health Nursing Doh Related Programs: Epi - Types of VaccinesDocument32 pagesCommunity Health Nursing Doh Related Programs: Epi - Types of VaccinesAngelaNo ratings yet
MSC Med Micro Antimicrobial Agents 2
MSC Med Micro Antimicrobial Agents 2
Uploaded by
Shalini M0 ratings0% found this document useful (0 votes)
1 views35 pagesThis document discusses various drug sensitivity tests that can be used to determine whether a microorganism is susceptible or resistant to antimicrobial agents. It describes methods such as antibiotic disc assays, test tube dilution tests, cylinder plate tests, E-tests, and molecular tests. Factors that can influence test results are temperature, incubation period, inoculum size, and medium used. The minimum inhibitory concentration (MIC) is discussed as the lowest drug concentration that prevents microbial growth. Assays can be performed directly on body fluids to determine susceptibility of pathogens. Probiotics and various probiotic strains and their therapeutic uses are also summarized.
Original Description:
Original Title
MSc Med Micro Antimicrobial Agents 2
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses various drug sensitivity tests that can be used to determine whether a microorganism is susceptible or resistant to antimicrobial agents. It describes methods such as antibiotic disc assays, test tube dilution tests, cylinder plate tests, E-tests, and molecular tests. Factors that can influence test results are temperature, incubation period, inoculum size, and medium used. The minimum inhibitory concentration (MIC) is discussed as the lowest drug concentration that prevents microbial growth. Assays can be performed directly on body fluids to determine susceptibility of pathogens. Probiotics and various probiotic strains and their therapeutic uses are also summarized.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
1 views35 pagesMSC Med Micro Antimicrobial Agents 2
MSC Med Micro Antimicrobial Agents 2
Uploaded by
Shalini MThis document discusses various drug sensitivity tests that can be used to determine whether a microorganism is susceptible or resistant to antimicrobial agents. It describes methods such as antibiotic disc assays, test tube dilution tests, cylinder plate tests, E-tests, and molecular tests. Factors that can influence test results are temperature, incubation period, inoculum size, and medium used. The minimum inhibitory concentration (MIC) is discussed as the lowest drug concentration that prevents microbial growth. Assays can be performed directly on body fluids to determine susceptibility of pathogens. Probiotics and various probiotic strains and their therapeutic uses are also summarized.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 35
Antimicrobial Agents (Part 2)
MBH-301: Medical Microbiology
Drug Sensitivity Tests
Antibiotic Disc Assay
Kirby-Bauer Method
Drug Sensitivity Tests
Antibiotic Disc Assay
Stokes’ method tests sensitivity to an
antibiotic by using an inoculation of a
controlled organism on a part of the plate,
while the rest of the plate is coated with the
test organism. Discs placed at the interface
allow the comparison of the zones of
inhibition.
The type, pH, and volume of the medium
used for growing the culture, the age of the
culture, the size of the inoculums are all
important factors that have a bearing on the
results of the antibiotic assay test. Even the
temperature during incubation and the
period of incubation may affect the outcome
of a microbial antibiotic assay.
Drug Sensitivity Tests
The Test-tube Dilution
In the test tube dilution method, to check the sensitivity of a
microorganism to an antibiotic, a serial solution of the antibiotic
in a suitable medium is prepared. Each test tube with a different
concentration of the antibiotic is inoculated with a specific
number of microorganisms and incubated for a specified period
of time. The test tube with the lowest concentration of antibiotic,
which inhibits the growth of the microorganism as shown by the
absence of turbidity, is identified as the one with the minimal
inhibitory concentration.
Drug Sensitivity Tests
Cylinder Plate Method
This test is used to determine the sensitivity of an organism. This
organism is usually isolated from a patient before the tests are
begun. This is a method in which the antibiotic solution is
diffused from a cylinder which is placed on an inoculated
surface. After incubation, the diameter of the inhibition zone is
measured. This diameter depends on the concentration of the
antibiotic used and its specific activity. This method is popular
and is therefore used in the commercial preparation of
antibiotics.
The result of such an assay can help a physician determine the
kind of drugs that need to be prescribed. If the organism is
susceptible to the antibiotic in this test, it is highly likely that it will
also be killed off when the antibiotics interact with the microbe in
the blood stream.
Drug Sensitivity Tests
E-Test
E-test (AB Biodisk, Solna, Sweden) is a
commercially available test that utilizes a
plastic test strip impregnated with a
gradually decreasing concentration of a
particular antibiotic. The strip also
displays a numerical scale that
corresponds to the antibiotic concentration
contained therein. This method provides
for a convenient quantitative test of
antibiotic resistance of a clinical isolate.
However, a separate strip is needed for
each antibiotic, and therefore the cost of
this method can be high.
Drug Sensitivity Tests
Antibiotic protection assay
It is another assay that might be done in order to check the
ability of the microbe to invade the epithelial cells and cause
harm. Such a test can help the doctors determine the course
that will be taken by a disease that is caused by microbes. It can
also help the doctors determine the kind of treatment that should
be given to the patient for the particular microbe. Additional tests
may be required with the antibiotic protection test.
Drug Sensitivity Tests
Molecular methods
Since resistance arises from genetic mutations, another
approach is to detect the mutations themselves. Many mutations
associated with resistance have been identified and molecular
tests to detect them have been developed. The advantages of
molecular methods of drug susceptibility testing include rapid
turnaround times, but the disadvantages include a low sensitivity
for some compounds, and a major issue is cost.
Drug Sensitivity Tests
In vivo
Mouse protection test
For chemotherapy studies, groups of mice are inoculated i.p. with
bacterial suspensions in mucin that contained about 100 ID50. Mice
are given graduated doses s.c. of antibiotics or saline 1 h later.
Mortality is determined after 48 h.
MIC
MIC: Minimum inhibitory concentration
The MIC is the lowest concentration of a drug that prevents
growth of a particular pathogen.
A drug must reach a concentration at the site of infection above
the pathogen’s MIC to be effective.
Broth Dilution Test:
A series of broth tubes (usually Mueller-Hinton broth) containing
antibiotic concentrations in the range of 0.1 to 128 g/ml is
prepared and inoculated with standard numbers of the test
organism.
The lowest concentration of the antibiotic resulting in no growth
after 16 to 20 hours of incubation is the MIC.
Agar Dilution Test:
Plates containing Mueller-Hinton agar and various amounts of
antibiotic are inoculated and examined for growth.
Antibiotic Assay in Body Fluids
The use of microtiter plates and automated inoculation
and reading systems makes the determination of MIC
feasible for use in the clinical laboratory.
MIC can even be performed on normally sterile body
fluids without isolating and identifying the pathogenic
microorganisms.
For example, blood or cerebrospinal fluid containing an infecting
microorganism can be added to tubes containing various
dilutions of an antibiotic and a suitable growth medium. An
increase in turbidity would indicate that the microorganism is
growing and that the antibiotic at that concentration was
ineffective in inhibiting microbial growth. Conversely, a lack of
growth would indicate that the pathogenic microorganisms were
susceptible to the antibiotic at the given concentration.
Swabs of body fluids for antibiotic assays
Probiotics: Introduction
Probiotics in the form of Streptococcus
thermophilus and Lactobacillus bulgaricus in fermented
milk have been ingested by humans for thousands of
years in the belief that they have health benefits.
Probiotics are defined as “live microorganisms that when
administered in adequate amounts confer a health
benefit on the host”.
Some of the best characterized probiotics have also
been shown to adhere strongly to intestinal epithelium in
both in vitro and in vivo studies.
Probiotics must also be resistant to gastric acid digestion
and to bile salts to reach the intestinal intact, and they
should be nonpathogenic.
( For more information, you can check: http://ajcn.nutrition.org/content/83/6/1256.full)
Probiotics: Strains
Most probiotics are strains of Bifidobacterium or
Lactobacillus species.
Some are derived from the intestinal microbiota of
healthy humans, and others are nonhuman strains used
in the fermentation of dairy products.
Species from other bacterial genera such
as Streptococcus, Bacillus, and Enterococcus have also
been used as probiotics.
There are concerns surrounding the safety of such probiotics
because these genera contain many pathogenic species,
particularly Enterococcus.
Nonbacterial microorganisms such as yeasts from the
genus Saccharomyces have also been used as
probiotics for many years.
Probiotics: Therapy
Probiotics have been advocated for the prevention and
treatment of a diverse range of disorders, from acute
gastroenteritis to intestinal neoplasia.
Some conditions for which probiotics can be used:
Irritable bowel syndrome
Inflammatory bowel disease (IBD)
Infectious diarrhea (caused by viruses, bacteria, or parasites)
Antibiotic-related diarrhea
There is also some research to show they ease the symptoms of
non-stomach-related problems. For example, some people say
they have helped with:
Skin conditions, like eczema
Urinary and vaginal health
Preventing allergies and colds
Oral health
Vaccines: Introduction
Refer to handout: Chapter 7 from Bacterial Pathogenesis
by Salyers and Whitt
Vaccines: Types
Scientists take many approaches to designing vaccines
against a microbe. These choices are typically based on
fundamental information about the microbe, such as how
it infects cells and how the immune system responds to
it, as well as practical considerations, such as regions of
the world where the vaccine would be used. Some
vaccine types include:
Live, attenuated vaccines
Inactivated vaccines
Subunit vaccines
Toxoid vaccines
Conjugate vaccines
DNA vaccines
Recombinant vector vaccines
Live, attenuated Vaccines
Live, attenuated vaccines contain a version of the living microbe that has
been weakened in the lab so it can’t cause disease. Because a live,
attenuated vaccine is the closest thing to a natural infection, these vaccines
are good “teachers” of the immune system: They elicit strong cellular and
antibody responses and often confer lifelong immunity with only one or two
doses.
Despite the advantages of live, attenuated vaccines, there are some
downsides. It is the nature of living things to change, or mutate, and the
organisms used in live, attenuated vaccines are no different. The remote
possibility exists that an attenuated microbe in the vaccine could revert to a
virulent form and cause disease. Also, not everyone can safely receive live,
attenuated vaccines. For their own protection, people who have damaged or
weakened immune systems—because they’ve undergone chemotherapy or
have HIV, for example—cannot be given live vaccines.
Another limitation is that live, attenuated vaccines usually need to be
refrigerated to stay potent. If the vaccine needs to be shipped overseas and
stored by healthcare workers in developing countries that lack widespread
refrigeration, a live vaccine may not be the best choice.
Live, attenuated Vaccines
Live, attenuated vaccines are relatively easy to create for certain viruses.
Vaccines against measles, mumps, and chickenpox, for example, are made
by this method. Viruses are simple microbes containing a small number of
genes, and scientists can therefore more readily control their characteristics.
Viruses often are attenuated through a method of growing generations of
them in cells in which they do not reproduce very well. This hostile
environment takes the fight out of viruses: As they evolve to adapt to the
new environment, they become weaker with respect to their natural host,
human beings.
Live, attenuated vaccines are more difficult to create for bacteria. Bacteria
have thousands of genes and thus are much harder to control. Scientists
working on a live vaccine for a bacterium, however, might be able to use
recombinant DNA technology to remove several key genes. This approach
has been used to create a vaccine against the bacterium that causes
cholera, Vibrio cholerae, although the live cholera vaccine has not been
licensed in the United States.
Inactivated Vaccines
Scientists produce inactivated vaccines by killing the disease-causing
microbe with chemicals, heat, or radiation. Such vaccines are more stable
and safer than live vaccines: The dead microbes can’t mutate back to their
disease-causing state. Inactivated vaccines usually don’t require
refrigeration, and they can be easily stored and transported in a freeze-dried
form, which makes them accessible to people in developing countries.
Most inactivated vaccines, however, stimulate a weaker immune system
response than do live vaccines. So it would likely take several additional
doses, or booster shots, to maintain a person’s immunity. This could be a
drawback in areas where people don’t have regular access to health care
and can’t get booster shots on time.
Subunit Vaccines
Instead of the entire microbe, subunit vaccines include only the antigens
that best stimulate the immune system. In some cases, these vaccines use
epitopes—the very specific parts of the antigen that antibodies or T cells
recognize and bind to. Because subunit vaccines contain only the essential
antigens and not all the other molecules that make up the microbe, the
chances of adverse reactions to the vaccine are lower.
Subunit vaccines can contain anywhere from 1 to 20 or more antigens. Of
course, identifying which antigens best stimulate the immune system is a
tricky, time-consuming process. Once scientists do that, however, they can
make subunit vaccines in one of two ways:
They can grow the microbe in the laboratory and then use chemicals to break it apart and
gather the important antigens.
They can manufacture the antigen molecules from the microbe using recombinant DNA
technology. Vaccines produced this way are called “recombinant subunit vaccines.”
A recombinant subunit vaccine has been made for the hepatitis B virus.
Scientists inserted hepatitis B genes that code for important antigens into
common baker’s yeast. The yeast then produced the antigens, which the
scientists collected and purified for use in the vaccine. Research is
continuing on a recombinant subunit vaccine against hepatitis C virus.
Toxoid Vaccines
For bacteria that secrete toxins, or harmful chemicals, a toxoid vaccine
might be the answer. These vaccines are used when a bacterial toxin is the
main cause of illness. Scientists have found that they can inactivate toxins
by treating them with formalin, a solution of formaldehyde and sterilized
water. Such “detoxified” toxins, called toxoids, are safe for use in vaccines.
When the immune system receives a vaccine containing a harmless toxoid,
it learns how to fight off the natural toxin. The immune system produces
antibodies that lock onto and block the toxin. Vaccines against diphtheria
and tetanus are examples of toxoid vaccines.
Conjugate Vaccines
If a bacterium possesses an outer coating of sugar molecules called
polysaccharides, as many harmful bacteria do, researchers may try making
a conjugate vaccine for it. Polysaccharide coatings disguise a bacterium’s
antigens so that the immature immune systems of infants and younger
children can’t recognize or respond to them. Conjugate vaccines, a special
type of subunit vaccine, get around this problem.
When making a conjugate vaccine, scientists link antigens or toxoids from a
microbe that an infant’s immune system can recognize to the
polysaccharides. The linkage helps the immature immune system react to
polysaccharide coatings and defend against the disease-causing bacterium.
The vaccine that protects against Haemophilus influenzae type B (Hib) is a
conjugate vaccine.
DNA Vaccines
Once the genes from a microbe have been analyzed, scientists could
attempt to create a DNA vaccine against it.
Still in the experimental stages, these vaccines show great promise, and
several types are being tested in humans. DNA vaccines take immunization
to a new technological level. These vaccines dispense with both the whole
organism and its parts and get right down to the essentials: the microbe’s
genetic material. In particular, DNA vaccines use the genes that code for
those all-important antigens.
Researchers have found that when the genes for a microbe’s antigens are
introduced into the body, some cells will take up that DNA. The DNA then
instructs those cells to make the antigen molecules. The cells secrete the
antigens and display them on their surfaces. In other words, the body’s own
cells become vaccine-making factories, creating the antigens necessary to
stimulate the immune system.
DNA Vaccines
A DNA vaccine against a microbe would evoke a strong antibody response
to the free-floating antigen secreted by cells, and the vaccine also would
stimulate a strong cellular response against the microbial antigens displayed
on cell surfaces. The DNA vaccine couldn’t cause the disease because it
wouldn’t contain the microbe, just copies of a few of its genes. In addition,
DNA vaccines are relatively easy and inexpensive to design and produce.
So-called naked DNA vaccines consist of DNA that is administered directly
into the body. These vaccines can be administered with a needle and
syringe or with a needle-less device that uses high-pressure gas to shoot
microscopic gold particles coated with DNA directly into cells. Sometimes,
the DNA is mixed with molecules that facilitate its uptake by the body’s cells.
Naked DNA vaccines being tested in humans include those against the
viruses that cause influenza and herpes.
Recombinant Vector Vaccines
Recombinant vector vaccines are experimental vaccines similar to DNA
vaccines, but they use an attenuated virus or bacterium to introduce
microbial DNA to cells of the body. “Vector” refers to the virus or bacterium
used as the carrier.
In nature, viruses latch on to cells and inject their genetic material into them.
In the lab, scientists have taken advantage of this process. They have
figured out how to take the roomy genomes of certain harmless or
attenuated viruses and insert portions of the genetic material from other
microbes into them. The carrier viruses then ferry that microbial DNA to
cells. Recombinant vector vaccines closely mimic a natural infection and
therefore do a good job of stimulating the immune system.
Attenuated bacteria also can be used as vectors. In this case, the inserted
genetic material causes the bacteria to display the antigens of other
microbes on its surface. In effect, the harmless bacterium mimics a harmful
microbe, provoking an immune response.
Researchers are working on both bacterial and viral-based recombinant
vector vaccines for HIV, rabies, and measles.
Immunization Schedules
Immunization is an important and effective health intervention for
children. Over the course of history, it has helped keep millions of
children protected against infectious and life-threatening diseases.
Vaccines have been so effective that some diseases that were once
feared are now either eradicated or easily manageable. Yet, in the
recent past many new diseases are emerging too. This makes
immunization of a child even more important.
Vaccines are most effective when they are administered to children
at the right age and with the recommended dosage as children are
susceptible to certain diseases at certain ages. As an example, polio
occurs most frequently in children below the age of 5. Because of
this, polio vaccines are given to children of those ages to prevent
harm caused by the disease. A child who isn't vaccinated or isn't
vaccinated on time remains unprotected and has increased chances
of getting seriously ill.
Passive Immunization
SEMINAR
Refer to handout: Chapter 7 from Bacterial Pathogenesis
by Salyers and Whitt
Interferons
Refer to handout: Basic Virology by Wagner and Hewlett
Pages 102-106
Interferons
Interferons (IFNs) are a group of signaling proteins made
and released by host cells in response to the presence
of pathogens, such as viruses, bacteria, parasites, or
tumor cells.
In a typical scenario, a virus-infected cell will release interferons
causing nearby cells to heighten their anti-viral defenses.
IFNs also have various other functions: they activate immune cells,
such as natural killer cells and macrophages; they increase host
defenses by up-regulating antigen presentation by virtue of
increasing the expression of major histocompatibility
complex (MHC) antigens. Certain symptoms of infections, such
as fever, muscle pain and "flu-like symptoms", are also caused by
the production of IFNs and other cytokines.
Types of Interferons
Based on the type of receptor through which they signal,
human interferons have been classified into three major types:
Interferon type I:
All type I IFNs bind to a specific cell surface receptor complex known as the
IFN-α/β receptor .
The type I interferons present in humans are IFN-α, IFN-β, IFN-ε, IFN-
κ and IFN-ω.
In general, type I interferons are produced when the body recognizes a
virus has invaded it.
They are produced by fibroblasts and monocytes.
However, the production of type I IFN-α is prohibited by another cytokine
known as Interleukin-10.
Once activated, type I interferons will create molecules which prevent the
virus from producing and replicating its RNA and DNA.
Overall, IFN-α can be used to treat hepatitis B and C infections, while IFN-β
can be used to treat multiple sclerosis
Types of Interferons
Interferon type II:
This is also known as immune interferon and is activated by IL-12.
Furthermore, type II interferons are released by T helper cells, type 1
specifically. However, they block the proliferation of T helper cells type 2.
The previous results in an inhibition of Th2 immune response and a further
induction of Th1 immune response, which leads to the development of
debilitating diseases such as multiple sclerosis.
IFN type II binds to IFNGR, which consists of IFNGR1 and IFNGR2 chains
and has a different receptor than type I IFN. In humans this is known
as IFN-γ.
Interferon type III:
Signal through a receptor complex consisting of IL10R2 (also called CRF2-
4) and IFNLR1 (also called CRF2-12).
Although discovered more recently than type I and type II IFNs, recent
information demonstrates the importance of Type III IFNs in some types of
virus infections.
Effects of Interferons in Humans
(dsRNA-dependent)
Effects of Interferons in Humans
(dsRNA-independent)
You might also like
- Koji BiroreactorsDocument11 pagesKoji BiroreactorsShalini MNo ratings yet
- Antibiotic Sensitivity TestingDocument18 pagesAntibiotic Sensitivity TestingMeeJames100% (1)
- Anti Microbial Chemotherapy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDocument41 pagesAnti Microbial Chemotherapy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDr. Ashish JawarkarNo ratings yet
- Antibiotic Susceptibility Testing: A Review On Current PracticesDocument8 pagesAntibiotic Susceptibility Testing: A Review On Current PracticesAndriano Arie WibowoNo ratings yet
- Antibiotic Sensitivity TestDocument4 pagesAntibiotic Sensitivity TestAll new MovieshubNo ratings yet
- Biology Investigatory Project: The Study of Effects of Antibiotics On Micro-OrganismsDocument13 pagesBiology Investigatory Project: The Study of Effects of Antibiotics On Micro-OrganismsSamanwitha SharmaNo ratings yet
- Group 4 Antibiotic Sensitivity TestingDocument8 pagesGroup 4 Antibiotic Sensitivity TestingJe Michelle LoayonNo ratings yet
- Bacteriology: Principles of Antimicrobial ActionDocument35 pagesBacteriology: Principles of Antimicrobial ActionggemalynNo ratings yet
- Sensitivity TestDocument16 pagesSensitivity Testmarkwillaz100% (1)
- Antimicrobial Agents: Basic Principles of Antimicrobial TherapyDocument10 pagesAntimicrobial Agents: Basic Principles of Antimicrobial TherapyMarku LeeNo ratings yet
- Antibiotic Susceptibility TestsDocument18 pagesAntibiotic Susceptibility Testsمحمد رحيم حسن محمودNo ratings yet
- Introduction To Techniques in MicrobiologyDocument4 pagesIntroduction To Techniques in MicrobiologyYusnita Damayanti100% (1)
- Antibiotics: Rodel L. Saludares Mario S. Abendanio Hazel M. Dela Cruz Lea Diane Dela Cruz Jicka TagubaDocument51 pagesAntibiotics: Rodel L. Saludares Mario S. Abendanio Hazel M. Dela Cruz Lea Diane Dela Cruz Jicka TagubaVer Garcera TalosigNo ratings yet
- Medical Microbiology: Class: 2Document3 pagesMedical Microbiology: Class: 2S ANo ratings yet
- Presentation 1Document20 pagesPresentation 1Sneha BagulNo ratings yet
- A6 Antimicrobial AgentsDocument61 pagesA6 Antimicrobial AgentsSHIELOU LOMODNo ratings yet
- Antibiotic Susceptibility Testing: NotesDocument12 pagesAntibiotic Susceptibility Testing: NotesKania Putri D 113No ratings yet
- Antimicrobial Susceptibility Testing (AST)Document41 pagesAntimicrobial Susceptibility Testing (AST)summiya100% (1)
- Link Between MIC and Antimicrobial TherapyDocument8 pagesLink Between MIC and Antimicrobial TherapySahar WaqarNo ratings yet
- Antibiotic Susceptibility TestingDocument12 pagesAntibiotic Susceptibility TestingOsama BakheetNo ratings yet
- Microbiological AssaysDocument34 pagesMicrobiological Assayspradeepbawane60% (5)
- Laboratory 6 - AntimicrobialsDocument4 pagesLaboratory 6 - AntimicrobialsLuzzuvannaNo ratings yet
- Antimicrobial Susceptibilty TestingDocument47 pagesAntimicrobial Susceptibilty TestingpixholicNo ratings yet
- Lab Report Antimicrobial Susceptibility Testing MethodsDocument19 pagesLab Report Antimicrobial Susceptibility Testing MethodsAlyaa Athira100% (1)
- Mic, MBC and Mic Cutoff ValueDocument23 pagesMic, MBC and Mic Cutoff ValueDiksha DahalNo ratings yet
- تينقتلا طسولاا ثارفلا تعماج تفوك/ تيبطلاو تيحصلا ثاينقتلا تيلك تيبطلا ثاربتخملا ثاينقت مسق: ةدام Diagnostic Microbiology تعبارلا تلحرملاDocument19 pagesتينقتلا طسولاا ثارفلا تعماج تفوك/ تيبطلاو تيحصلا ثاينقتلا تيلك تيبطلا ثاربتخملا ثاينقت مسق: ةدام Diagnostic Microbiology تعبارلا تلحرملاAli M. AtshanNo ratings yet
- In Campus Micro Exp.6 2022Document17 pagesIn Campus Micro Exp.6 2022oking4831No ratings yet
- Biology Investigatory Project 2022-2023Document22 pagesBiology Investigatory Project 2022-2023Sneha Bagul50% (2)
- Biology Project XiiDocument14 pagesBiology Project XiiSagayaraniNo ratings yet
- Dokumen - Tips Biology Investigatory Project 561e79b91f5a0Document17 pagesDokumen - Tips Biology Investigatory Project 561e79b91f5a0Upendra LalNo ratings yet
- Ast Booklet GB Final PDFDocument19 pagesAst Booklet GB Final PDFAhmed GaberNo ratings yet
- Central AcademyDocument17 pagesCentral AcademyKartikey VermaNo ratings yet
- Antibiotic Sensitivity TestDocument2 pagesAntibiotic Sensitivity Testganesh2gigNo ratings yet
- Infectious Pharmacology 01Document19 pagesInfectious Pharmacology 01Arthur YanezNo ratings yet
- Biology Project ReportDocument15 pagesBiology Project ReportOmsai GarNo ratings yet
- Pharmacology Unit 2 Antimicrobial DrugsDocument62 pagesPharmacology Unit 2 Antimicrobial DrugsAsif Ali LashariNo ratings yet
- Fdocuments - in Biology Investigatory Project 561e79b91f5a0Document18 pagesFdocuments - in Biology Investigatory Project 561e79b91f5a0ASHOKNo ratings yet
- SuperbugsDocument3 pagesSuperbugsMatei BuneaNo ratings yet
- The Roles and FunctionsDocument2 pagesThe Roles and Functionssyed hafizNo ratings yet
- INDEXDocument16 pagesINDEXayush rajeshNo ratings yet
- Antimicrobial Susceptibility Testing FK 2012Document32 pagesAntimicrobial Susceptibility Testing FK 2012Sheryl Elita100% (1)
- 6.1 Antibiotic Fermentation 1 PDFDocument26 pages6.1 Antibiotic Fermentation 1 PDFdenojsNo ratings yet
- Anti Micro Biii AlDocument7 pagesAnti Micro Biii AltimiiniyiiNo ratings yet
- The Role of Clinical Pharmacist in Combating Antibiotic ResistanceDocument4 pagesThe Role of Clinical Pharmacist in Combating Antibiotic ResistanceAnto BijuNo ratings yet
- Probiotik Mengurangi Resistensi AntibiotikDocument34 pagesProbiotik Mengurangi Resistensi AntibiotikviaNo ratings yet
- Biology ProjectDocument28 pagesBiology ProjectKanak MirpouriNo ratings yet
- Antimicrobial Susceptibility 4.3Document22 pagesAntimicrobial Susceptibility 4.3Maxwell C Jay KafwaniNo ratings yet
- Principles of Bacterial Infections and Anti-Infectives: Cause, Pathogenicity, and VirulenceDocument29 pagesPrinciples of Bacterial Infections and Anti-Infectives: Cause, Pathogenicity, and Virulencejheannie02100% (1)
- AntibioticsDocument49 pagesAntibioticsShriefElghazalyNo ratings yet
- Experiment 10Document2 pagesExperiment 10Mark Janssen CustodioNo ratings yet
- 2009-Antimicrobial SusceptilityDocument7 pages2009-Antimicrobial SusceptilityStephanie MurillejoNo ratings yet
- A6 Antimicrobial AgentsDocument61 pagesA6 Antimicrobial AgentsRIK HAROLD GATPANDANNo ratings yet
- Unit-II Lecture-IV Antibiotics by ZebDocument84 pagesUnit-II Lecture-IV Antibiotics by ZebImad khanNo ratings yet
- Unit 4, Pharmaceutical Engineering, B Pharmacy 3rd Sem, Carewell PharmaDocument4 pagesUnit 4, Pharmaceutical Engineering, B Pharmacy 3rd Sem, Carewell PharmaAjay KNo ratings yet
- Yuvraj BiologyDocument19 pagesYuvraj BiologyAnkit KashyapNo ratings yet
- Antibiotics Lloyd ADocument11 pagesAntibiotics Lloyd AAndrew Lloyd100% (1)
- Clinical Microbiology and ImmunologyDocument7 pagesClinical Microbiology and ImmunologyGwyn CervantesNo ratings yet
- Bacteriology - Chapter Six Antibiotics - Protein Synthesis, Nucleic Acid Synthesis and MetabolismDocument6 pagesBacteriology - Chapter Six Antibiotics - Protein Synthesis, Nucleic Acid Synthesis and MetabolismZeth MoturiNo ratings yet
- Presentation 1Document25 pagesPresentation 1Sneha BagulNo ratings yet
- Principles of Antimicrobial UseDocument5 pagesPrinciples of Antimicrobial Usegayleteguichan19No ratings yet
- Definitions:: Meaning of DelegationDocument9 pagesDefinitions:: Meaning of DelegationShalini MNo ratings yet
- Gibberellic AcidDocument17 pagesGibberellic AcidShalini MNo ratings yet
- Plant Growth RegulatorsDocument33 pagesPlant Growth RegulatorsShalini MNo ratings yet
- Patent - Laws and Procedure - Aneesh MarballiDocument29 pagesPatent - Laws and Procedure - Aneesh MarballiShalini MNo ratings yet
- Frankia SeminarDocument20 pagesFrankia SeminarShalini M100% (1)
- Cellulase Production by SSFDocument9 pagesCellulase Production by SSFShalini MNo ratings yet
- Penicillin Production by Solid State FermentationDocument5 pagesPenicillin Production by Solid State FermentationShalini MNo ratings yet
- Barriers To EntreprenwurshipDocument7 pagesBarriers To EntreprenwurshipShalini MNo ratings yet
- eSTIMATION OF GROWTH in SSFDocument9 pageseSTIMATION OF GROWTH in SSFShalini MNo ratings yet
- Sterilization of Fermenter-1Document11 pagesSterilization of Fermenter-1Shalini M100% (1)
- SSF Bioreactor SystemsDocument26 pagesSSF Bioreactor SystemsShalini MNo ratings yet
- Biofertilizers (Microbial Inoculants)Document10 pagesBiofertilizers (Microbial Inoculants)Shalini MNo ratings yet
- Materi DR DR Ari Prayitno SpAK Typhoid Vaccine - Current and New PlatformDocument40 pagesMateri DR DR Ari Prayitno SpAK Typhoid Vaccine - Current and New PlatformMutiara UtiNo ratings yet
- The Immune SystemDocument29 pagesThe Immune SystemLalajimNo ratings yet
- Plant Vaccines: An Overview: Gaurav Kumar Karthik LoganathanDocument16 pagesPlant Vaccines: An Overview: Gaurav Kumar Karthik LoganathanMayank BahugunaNo ratings yet
- Global Manual Revised 12102015Document124 pagesGlobal Manual Revised 12102015Ishak Abdul GafarNo ratings yet
- Vaccines Science PharmaDocument30 pagesVaccines Science PharmaGanesh V GaonkarNo ratings yet
- Meningitis Bacteriana Aguda en El AdultoDocument12 pagesMeningitis Bacteriana Aguda en El AdultoJulian AlbarracínNo ratings yet
- Global Manual On Surveillance of AEFIDocument128 pagesGlobal Manual On Surveillance of AEFIHarold JeffersonNo ratings yet
- IMMUNOPROPHYLAXISDocument30 pagesIMMUNOPROPHYLAXISAli TARARNo ratings yet
- Impact of Pneumococcal Conjugate Vaccine in At-Risk Adults 2022Document48 pagesImpact of Pneumococcal Conjugate Vaccine in At-Risk Adults 2022Rosi AmaliaNo ratings yet
- Community Health Nursing Doh Related Programs: Epi - Types of VaccinesDocument32 pagesCommunity Health Nursing Doh Related Programs: Epi - Types of VaccinesAngelaNo ratings yet
- Immunization Manual For Medical and Nursing Students - Final Smaller PDFDocument296 pagesImmunization Manual For Medical and Nursing Students - Final Smaller PDFamit100% (3)
- Types of VaccinesDocument2 pagesTypes of VaccinesErika Bea PaculanangNo ratings yet
- IMUNOPROFILAKTIKDocument26 pagesIMUNOPROFILAKTIKSatriyo K. PalgunoNo ratings yet
- Biologics, Immunology and PharmacognosyDocument26 pagesBiologics, Immunology and PharmacognosyShereenNo ratings yet
- CHN211 Week 7 WORD - National Immunization ProgramDocument35 pagesCHN211 Week 7 WORD - National Immunization ProgramChesca DomingoNo ratings yet
- Pentaxim-Pi-Sg Pen 0118 Spc0914Document10 pagesPentaxim-Pi-Sg Pen 0118 Spc0914walkrogNo ratings yet
- IAS Exam Congress: IasecDocument22 pagesIAS Exam Congress: IasecNandita NanditaNo ratings yet
- VaccinesDocument17 pagesVaccinesYOGANANTH mscasNo ratings yet
- Immunosuppressants NotesDocument20 pagesImmunosuppressants NotesmadcalNo ratings yet
- Immunization CTP March 2021 4-Per-PageDocument71 pagesImmunization CTP March 2021 4-Per-PageAssal Al JanabiNo ratings yet
- Different Types of VaccinesDocument2 pagesDifferent Types of VaccinesBhuvaneshNo ratings yet
- Lab Technologist-3Document92 pagesLab Technologist-3AHAMED SHIFAAN100% (1)
- MODULE 2: Types of Vaccine and Adverse ReactionsDocument29 pagesMODULE 2: Types of Vaccine and Adverse ReactionsnandaNo ratings yet
- Immunization CTP July 2020 4-Per-PageDocument70 pagesImmunization CTP July 2020 4-Per-Pagejose carlos gonzalezNo ratings yet
- Types of VaccinesDocument3 pagesTypes of Vaccineshaddi awanNo ratings yet
- ImmunisationDocument42 pagesImmunisationDr. Ajeta GuptaNo ratings yet
- Immunological ProductsDocument19 pagesImmunological ProductsPharma 24No ratings yet
- Typbar TCV Package InsertDocument1 pageTypbar TCV Package Insertjossy123456No ratings yet
- 7) Preventive Health and EPIDocument51 pages7) Preventive Health and EPIDr. Zirwa AsimNo ratings yet
- Community Health Nursing Doh Related Programs: Epi - Types of VaccinesDocument32 pagesCommunity Health Nursing Doh Related Programs: Epi - Types of VaccinesAngelaNo ratings yet