Professional Documents
Culture Documents
Chapter 24 Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders
Chapter 24 Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders
Uploaded by
سلطان محمد فوزي سلمانCopyright:
Available Formats
You might also like
- Print NCLEX Study - Mark Klimek Blue BookDocument17 pagesPrint NCLEX Study - Mark Klimek Blue Booklento1990100% (1)
- ATI Remediation ADocument3 pagesATI Remediation AChelsea PalmaNo ratings yet
- Mark Klimek Full Nclex ReviewerDocument30 pagesMark Klimek Full Nclex ReviewerAlex BellNo ratings yet
- Government College of Nursing: JodhpurDocument9 pagesGovernment College of Nursing: JodhpurpriyankaNo ratings yet
- Hesi Management of A Emergent Care UnitDocument5 pagesHesi Management of A Emergent Care UnitAna Bienne0% (1)
- LPN DELEGATION and PRIORITIZING AND MOREDocument38 pagesLPN DELEGATION and PRIORITIZING AND MOREDebra PowellNo ratings yet
- Thinking Like A NurseDocument3 pagesThinking Like A Nurseapi-519359726No ratings yet
- ATI Practice CodesDocument1 pageATI Practice Codesvanassa johnson100% (4)
- VATI Mental Health RemediationDocument2 pagesVATI Mental Health RemediationestberryNo ratings yet
- ISBAR Worksheet Olivia Jones Jasgou1752Document1 pageISBAR Worksheet Olivia Jones Jasgou1752Jasmyn Rose100% (1)
- NCLEX RN Review For Reduction of Risk PotentialDocument7 pagesNCLEX RN Review For Reduction of Risk Potentialpaulinatia100% (1)
- Sample Psychotherapy NoteDocument2 pagesSample Psychotherapy NoteRafael Sanchez100% (3)
- Adult1 27 - 28Document78 pagesAdult1 27 - 28Ahmed AbahraNo ratings yet
- Hinkle PPT CH 28Document34 pagesHinkle PPT CH 28Ahmed AbahraNo ratings yet
- A Nurse's Guide to Caring for Cardiac Intervention PatientsFrom EverandA Nurse's Guide to Caring for Cardiac Intervention PatientsNo ratings yet
- Mitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandMitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Chapter27-Assessment and Management of Patients With HypertensionDocument31 pagesChapter27-Assessment and Management of Patients With HypertensionAhmed 123No ratings yet
- Gastric and Duodenal Disorders - Test 4Document21 pagesGastric and Duodenal Disorders - Test 4Vickie BuckerNo ratings yet
- 1 - Yellow BookDocument49 pages1 - Yellow Booksushma.rayamajhi.bsc06No ratings yet
- Immunity 1Document6 pagesImmunity 1Tori RolandNo ratings yet
- Acute Kidney Injury NCLEXDocument21 pagesAcute Kidney Injury NCLEXSameerQadumi100% (1)
- NURS 460 Nursing Licensure Examination Course: Jv7@hawaii - EduDocument5 pagesNURS 460 Nursing Licensure Examination Course: Jv7@hawaii - EduJeffrey ViernesNo ratings yet
- Open Pediatric ArcherDocument84 pagesOpen Pediatric Archerbaharada1979No ratings yet
- Nursing ExamDocument8 pagesNursing ExamDa DungNo ratings yet
- Cad PPTDocument81 pagesCad PPTvaishnaviNo ratings yet
- CA RationaleDocument39 pagesCA RationaleSeirah Distor MartinezNo ratings yet
- Bsn-Rs-Careplan 2Document9 pagesBsn-Rs-Careplan 2api-520841770No ratings yet
- Renal & Urinary ATIDocument2 pagesRenal & Urinary ATIHelen Varela100% (1)
- The Client Should Be Instructed As Follows: Intravenous Pyelogram (IVP) Is An X-Ray of The Urinary SystemDocument25 pagesThe Client Should Be Instructed As Follows: Intravenous Pyelogram (IVP) Is An X-Ray of The Urinary SystemElizabeth SharmaNo ratings yet
- Final Study Guide 2Document4 pagesFinal Study Guide 2Nataraj LoganathanNo ratings yet
- Exam ReviewDocument4 pagesExam ReviewMya Thomas100% (1)
- Diet NclexDocument1 pageDiet NclexSoon ShinNo ratings yet
- Neurologic NCLEX Practice Test Part 1Document6 pagesNeurologic NCLEX Practice Test Part 1ojoj2206No ratings yet
- ADEX. MP Resume Template 0604.12 (NY) .6.24.15Document3 pagesADEX. MP Resume Template 0604.12 (NY) .6.24.15Mjay GuintoNo ratings yet
- Brain Dump NUR 213 FINALDocument37 pagesBrain Dump NUR 213 FINALkelsey jackson100% (1)
- Review Notes For NCLEX CGFNS - Aortic AneurysmsDocument2 pagesReview Notes For NCLEX CGFNS - Aortic Aneurysmswyndz100% (3)
- ATI Comprehensive Predictor: Study Online atDocument9 pagesATI Comprehensive Predictor: Study Online atVanessaMUellerNo ratings yet
- IV PDFDocument63 pagesIV PDFelbagouryNo ratings yet
- Dysrhythmia TestsDocument3 pagesDysrhythmia TestsKimberly WhitesideNo ratings yet
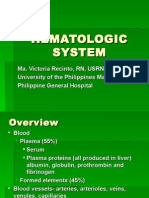
- Hematologic System2Document70 pagesHematologic System2Jesus Mario LopezNo ratings yet
- Fluids and Electrolytes: Irene L. Gardiner, MDDocument48 pagesFluids and Electrolytes: Irene L. Gardiner, MDGabriel Carlo FranciscoNo ratings yet
- Hesi Management of A Medical UnitDocument2 pagesHesi Management of A Medical UnitAna Bienne100% (1)
- Hyperemesis Gravidarum: Bleeding Complications of PregnancyDocument6 pagesHyperemesis Gravidarum: Bleeding Complications of PregnancykirbsNo ratings yet
- NCLEX Quick FactsDocument7 pagesNCLEX Quick FactsMary Aurine FullanteNo ratings yet
- GuideDocument5 pagesGuideHu Tao100% (1)
- Ms Flash CardsDocument15 pagesMs Flash CardsMia MalazoNo ratings yet
- Medical Surgical Nursing - DiabetesDocument4 pagesMedical Surgical Nursing - Diabetestripj33100% (2)
- AdultDocument295 pagesAdultKen WonNo ratings yet
- HESI Medsurg V2Document26 pagesHESI Medsurg V2aasthabhattarai07No ratings yet
- 8 Essential Concepts 4 NCLEX RN-4Document6 pages8 Essential Concepts 4 NCLEX RN-4Jot grewalNo ratings yet
- Answers and Rationales For NCLEX Style Review QuestionsDocument12 pagesAnswers and Rationales For NCLEX Style Review QuestionsJacinth Florido Fedelin50% (2)
- Camporedondo, Bryan C. RLE8 - Group5 Emergency Drugs: Atropine SulfateDocument4 pagesCamporedondo, Bryan C. RLE8 - Group5 Emergency Drugs: Atropine SulfateIglesia Ni Cristo DoctorsNo ratings yet
- Remar WorkbookDocument60 pagesRemar Workbookharsimranr761100% (1)
- Entry To Practice RPNDocument20 pagesEntry To Practice RPNDivina D Galvez-BeronioNo ratings yet
- 7th Edition All NeuroDocument92 pages7th Edition All NeuroCrystal LynaeNo ratings yet
- Ignatavicius TOCDocument9 pagesIgnatavicius TOCjennaaahhhNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- Navigating Long-Term Care - A Practical Approach for NursesFrom EverandNavigating Long-Term Care - A Practical Approach for NursesNo ratings yet
- Registered Professional Nurse: Passbooks Study GuideFrom EverandRegistered Professional Nurse: Passbooks Study GuideNo ratings yet
- 7 - PainDocument22 pages7 - Painسلطان محمد فوزي سلمانNo ratings yet
- 10 - Care at The End of LifeDocument23 pages10 - Care at The End of Lifeسلطان محمد فوزي سلمانNo ratings yet
- 3 - Common Aging ChangesDocument41 pages3 - Common Aging Changesسلطان محمد فوزي سلمانNo ratings yet
- 4 NutritionDocument30 pages4 Nutritionسلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شـابـتـر ١٣?Document18 pagesتَـلـخـيـص شـابـتـر ١٣?سلطان محمد فوزي سلمانNo ratings yet
- Chapter 67 Management of Patients With Cerebrovascular DisordersDocument41 pagesChapter 67 Management of Patients With Cerebrovascular Disordersسلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شـابـتـر ١٤?Document21 pagesتَـلـخـيـص شـابـتـر ١٤?سلطان محمد فوزي سلمانNo ratings yet
- تَـلخـيـص شـابـتـر ٢٠?Document17 pagesتَـلخـيـص شـابـتـر ٢٠?سلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شـابـتـر ١٢?Document11 pagesتَـلـخـيـص شـابـتـر ١٢?سلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شَـابـتـر ٢٣?Document10 pagesتَـلـخـيـص شَـابـتـر ٢٣?سلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شَـابـتـر ٢٥?Document12 pagesتَـلـخـيـص شَـابـتـر ٢٥?سلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شـابـتـر ٢٦?Document15 pagesتَـلـخـيـص شـابـتـر ٢٦?سلطان محمد فوزي سلمانNo ratings yet
- Bundle Fundamentals of Nursing PDFDocument59 pagesBundle Fundamentals of Nursing PDFسلطان محمد فوزي سلمانNo ratings yet
- Weekly Objective Form - NEWDocument3 pagesWeekly Objective Form - NEWسلطان محمد فوزي سلمانNo ratings yet
- Medical Care Plan - NEWDocument4 pagesMedical Care Plan - NEWسلطان محمد فوزي سلمانNo ratings yet
- Infection and Infectious ProcessDocument44 pagesInfection and Infectious Processpandey omkarNo ratings yet
- Merrf Syndrome BeverlyDocument4 pagesMerrf Syndrome BeverlyQuezon D. Lerog Jr.No ratings yet
- Research in Public Health by Prof DR Rwamakuba ZephanieDocument120 pagesResearch in Public Health by Prof DR Rwamakuba ZephanieDr Zephanie RwamakubaNo ratings yet
- Mims Jpog August 2015 IdDocument70 pagesMims Jpog August 2015 IdDika MidbrainNo ratings yet
- Chakrabarti, 1986Document4 pagesChakrabarti, 1986Jessica VanyaNo ratings yet
- Mesna: Mesna, Sold Under The BrandDocument17 pagesMesna: Mesna, Sold Under The BrandAndry HamdaniNo ratings yet
- NeoBip Clinical Guide 2020.9.4Document11 pagesNeoBip Clinical Guide 2020.9.4TECHMED REPAIRS TECHMED SALESNo ratings yet
- ID Gambaran Histologik Hati Pada Kelinci Ya PDFDocument5 pagesID Gambaran Histologik Hati Pada Kelinci Ya PDFYudha Jrokolioli NostNo ratings yet
- New Vistas In: Fetal MedicineDocument2 pagesNew Vistas In: Fetal MedicineRaviraj TirukeNo ratings yet
- Liver Cirrhosis Case Study Polish Male 56 PDFDocument3 pagesLiver Cirrhosis Case Study Polish Male 56 PDFHlamin OoNo ratings yet
- 1-Clinical ParasitologyDocument44 pages1-Clinical ParasitologyMohiedden M Abdul-FattahNo ratings yet
- Acute Renal Failure DR Kwaifa.2Document170 pagesAcute Renal Failure DR Kwaifa.2DICKSONNo ratings yet
- Expanded Program On Immunization (EPI) : Minimum Age at 1st Dose Number of Doses Dose Route SiteDocument2 pagesExpanded Program On Immunization (EPI) : Minimum Age at 1st Dose Number of Doses Dose Route SiteYana DugayNo ratings yet
- Department of Bio-Informatics 3 Semester (Morning) : Subject ImmunologyDocument10 pagesDepartment of Bio-Informatics 3 Semester (Morning) : Subject ImmunologyShaher Bano MirzaNo ratings yet
- Approach To A Child With Chronic Diarrhea: Parijat R. Tripathi Anshu SrivastavaDocument9 pagesApproach To A Child With Chronic Diarrhea: Parijat R. Tripathi Anshu SrivastavaTrọng PhướcNo ratings yet
- Eye Drops: Drug StudyDocument3 pagesEye Drops: Drug StudyChris PaguioNo ratings yet
- Pain Management Guide PDFDocument5 pagesPain Management Guide PDFPriydarshni KohliNo ratings yet
- Jurnal Penyakit Arteri PeriferDocument12 pagesJurnal Penyakit Arteri Perifereka saptaning windu fitriNo ratings yet
- Neurocritical CareDocument337 pagesNeurocritical Cares SNo ratings yet
- Neurogeriatria 2017 PDFDocument417 pagesNeurogeriatria 2017 PDFWilfredo DavilaNo ratings yet
- Atrial FibrillationDocument390 pagesAtrial FibrillationAlexandra Carmen100% (1)
- Sepsis Proposal1Document34 pagesSepsis Proposal1Appiah Peter OforiNo ratings yet
- Interpretation: L55 - PSC Indra Nagar Home Visit GRD FLR 197/A, Indra Nagar, Double ROAD, BANGALORE - 560080 BangaloreDocument2 pagesInterpretation: L55 - PSC Indra Nagar Home Visit GRD FLR 197/A, Indra Nagar, Double ROAD, BANGALORE - 560080 BangaloreDivyaSNo ratings yet
- Osha Rkforms Winstr - Fillable PDFDocument12 pagesOsha Rkforms Winstr - Fillable PDFBerhanu BedassaNo ratings yet
- Clinical Review Memo, August 23, 2021 - COMIRNATYDocument108 pagesClinical Review Memo, August 23, 2021 - COMIRNATYadrianoucamNo ratings yet
- Deep Vein Thrombosis in Pregnancy - Epidemiology, Pathogenesis, and Diagnosis - UpToDateDocument26 pagesDeep Vein Thrombosis in Pregnancy - Epidemiology, Pathogenesis, and Diagnosis - UpToDateCristinaCaprosNo ratings yet
- Narrative Pathophysiology of PregnancyDocument2 pagesNarrative Pathophysiology of PregnancyMarvin ChulyaoNo ratings yet
- Fat EmbolismDocument4 pagesFat EmbolismAmmar HasyimNo ratings yet
Chapter 24 Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders
Chapter 24 Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders
Uploaded by
سلطان محمد فوزي سلمانOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 24 Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders
Chapter 24 Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders
Uploaded by
سلطان محمد فوزي سلمانCopyright:
Available Formats
Chapter 24
Management of Patients With
Structural, Infectious, and
Inflammatory Cardiac Disorders
Learning Objectives
• The learner will be able to:
• Define valvular disorders of the heart and describe the
pathophysiology,
clinical manifestations, and management of patients with
mitral and aortic disorders.
• Describe types of cardiac valve repair and replacement
procedures used to treat valvular problems and care needed
by patients who undergo these procedures.
• Describe the pathophysiology, clinical manifestations, and
management of patients with cardiomyopathies.
• Describe the pathophysiology, clinical manifestations, and
management of
patients with infections of the heart.
• Use the nursing process as a framework of care for the
patient with a cardiomyopathy and the patient with
pericarditis.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Valvular Disorders
• Regurgitation: The valve does not close properly, and
blood backflows through the valve.
• Stenosis: The valve does not open completely, and
blood
flow through the valve is reduced.
• Valve prolapse: The stretching of an atrioventricular
valve leaflet into the atrium during diastole
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Valves of the Heart
Valves of the heart (aortic or semilunar, tricuspid, and mitral)
in closed positions.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Specific Valvular Disorders
• Mitral regurgitation
• Mitral stenosis
• In patients with mitral valve stenosis, the pulse is weak and
often irregular because of atrial fibrillation.
• The first symptom of mitral stenosis is often dyspnea on
exertion as a result of
pulmonary venous hypertension. Symptoms usually develop
after the valve opening is reduced by one-third to one-half
its usual size.
• Patients are likely to show progressive fatigue as a
result of low cardiac output. The enlarged left atrium may
create pressure on the left bronchial
tree, resulting in a dry cough or wheezing. Patients may
expectorate blood
(i.e., hemoptysis) or experience palpitations, orthopnea,
paroxysmal nocturnal
dyspnea (PND), and repeated respiratory infections
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Specific Valvular Disorders
• Aortic regurgitation
• Blood to flow back from the aorta to the left ventricle
• Aortic regurgitation eventually causes left ventricular
hypertrophy. In aortic regurgitation, blood from the aorta
returns to the left ventricle during diastole in addition to
the blood normally delivered by the left atrium. The left
ventricle dilates, trying to accommodate the increased
volume of blood.
• Aortic stenosis
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Management: Valvular Heart
Disorders #1
• Patient education
• Monitor VS trends
• Monitor for complications
– Heart failure
– Dysrhythmias
– Other symptoms
• Medication schedule: education
• Daily weights: monitor for weight gain
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Management: Valvular Heart
Disorders #2
• Plan activity with rest periods
• Sleep with HOB elevated
• Patients with mitral stenosis are advised to avoid
strenuous activities, competitive sports, and pregnancy,
all of which increase heart rate.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Question #1
The nurse is providing education for a client diagnosed with
mitral valve prolapse (MVP). What should be included in
the teaching plan? (Select all that apply.)
A. MVP is not hereditary.
B. Caffeine is tolerated in small amounts.
C. Avoid alcohol.
D. Stop use of tobacco products.
E. Prophylactic antibiotics are not prescribed before dental
procedures.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Answer
C. Avoid alcohol.
D. Stop use of tobacco products.
E. Prophylactic antibiotics are not prescribed before dental
procedures.
Rationale: MVP is hereditary, and caffeine should be
avoided.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Surgical Management:
Valvular Heart Disorders
• Valvuloplasty • Valve replacement
– Commissurotomy – Mechanical
– Balloon valvuloplasty
– Annuloplasty
– Leaflet repair
– Chordoplasty
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Balloon Valvuloplasty
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Annuloplasty Ring Insertion
• Annuloplasty ring insertion.
A. Mitral valve regurgitation; leaflets do not close.
B. Insertion of an annuloplasty ring.
C. Completed valvuloplasty; leaflets close.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Valve Leaflet Resection and Repair With
Ring Annuloplasty
• Valve leaflet resection and repair with a ring
annuloplasty.
A. Mitral valve regurgitation; the section
indicated by dashed lines is excised.
B. Approximation of edges and suturing.
C. Completed valvuloplasty, leaflet repair,
and annuloplasty ring.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Valve Replacement
• Valve replacement. A. The native valve is trimmed, and the prosthetic valve
is sutured in place. B. Once all sutures are placed through the ring, the
surgeon slides the prosthetic valve down the sutures and into the natural
orifice. Sutures are then tied off and trimmed.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Management: Valvuloplasty and
Valve Replacement #1
• Balloon valvuloplasty
-For some patients, valvuloplasty can be done in a cardiac
catheterization laboratory.”
– Monitor for heart failure and emboli
– Assess heart sounds every 4 hours
– Same care as after cardiac catheterization
– After undergoing percutaneous balloon valvuloplasty, the patient
usually remains in the hospital for 24 to 48 hours.
• Surgical valvuloplasty or valve replacements
– Focus is hemodynamic stability and recovery from anesthesia
– Frequent assessments with attention to neurologic,
respiratory, and cardiovascular systems
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Management: Valvuloplasty and
Valve Replacement #2
• Patient education
– Mechanical valves necessitate long-term use of
required anticoagulants.
– Prevention of infective endocarditis
– Follow up
– Repeat echocardiograms
– Following mechanical valve replacement, antibiotic
prophylaxis is necessary before dental procedures
involving manipulation of gingival tissue, the
periapical area of the teeth or perforation of the oral
mucosa
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Management: Valvuloplasty and
Valve Replacement #3
• Patients who take warfarin (Coumadin) after valve
replacement have individualized target INRs; usually
between 2 and 3.5 for mitral valve replacement and 1.8
and 2.2 for aortic valve replacement.
• Possible complications of a balloon valvuloplasty include
aortic regurgitation, emboli, ventricular perforation,
rupture of the aortic valve annulus, ventricular
dysrhythmia, mitral valve damage, and bleeding
from the
catheter insertion sites.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Patient education
• In general, valves that undergo valvuloplasty function
longer than prosthetic valve replacements and patients
do not require continuous anticoagulation.
• Valvuloplasty carries a risk of infection, like all surgical
procedures, and it is not performed in a physician's
office.
• Antirejection drugs are unnecessary because foreign
tissue is not introduced.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Cardiomyopathy
• Cardiomyopathy is a series of progressive events that
culminates in impaired cardiac output and can lead to
heart failure, sudden death, or dysrhythmias.
• Types
– Dilated Cardiomyopathy(Dilated ventricles without
hypertrophy of the ventricles)
– The ventricles have elevated systolic and diastolic
volumes, but a decreased ejection fraction.
– Restrictive cardiomyopathy
– Hypertrophic cardiomyopathy (With HCM, cardiac arrest
(i.e.,
sudden cardiac death) may be the initial manifestation in
young
people, including athletes).
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Cardiomyopathies That Lead to
Congestive Heart Failure
Copyright © 2022 Wolters Kluwer · All Rights Reserved
diagnostic tool for cardiomyopathy
• diagnostic tool would be most helpful in diagnosing
cardiomyopathy is the echocardiogram
• the echocardiogram is one of the most helpful diagnostic
tools because the structure and function of the ventricles
can be observed easily
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Question #2
What is the main electrolyte involved in cardiomyopathy?
A. Calcium
B. Phosphorus
C. Potassium
D. Sodium
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Answer
D. Sodium
Rationale: Sodium is the major electrolyte involved with
cardiomyopathy. Cardiomyopathy often leads to heart
failure, which develops, in part, from fluid overload.
Fluid
overload is often associated with elevated sodium
levels.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Process: The Patient With
Cardiomyopathy (Assessment)
• History (predisposing factors, family history)
• Chest pain
• Review of diet (Na reduction, vitamin supplements)
• Psychosocial history: impact on family, stressors,
depression
• Physical assessment: VS pulse pressure; pulsus
paradoxus; weight gain or loss; PMI; murmurs; S3 or S4;
pulmonary auscultation for crackles, JVD, and edema
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Process: The Patient with
Cardiomyopathy (Nursing Diagnosis)
• Decreased cardiac output
• Risk for ineffective cardiac, cerebral, peripheral, and
renal tissue perfusion
• Impaired gas exchange
• Activity intolerance
• Anxiety
• Powerlessness
• Noncompliance with medication and diet therapies
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Collaborative Problems and Potential
Complications
• Heart failure
• Ventricular dysrhythmias
• Atrial dysrhythmias
• Cardiac conduction defects
• Pulmonary or cerebral embolism
• Valvular dysfunction
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Process: The Patient With
Cardiomyopathy (Planning and Goals)
Goals
– Improvement or maintenance of cardiac output
– Increased activity tolerance
– Reduction of anxiety
– Adherence to the self-care program
– Increased sense of power with decision making
– Absence of complications
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Process: The Patient With
Cardiomyopathy (Nursing Interventions) #1
• Improve cardiac output and peripheral blood flow
– The priority nursing diagnosis of a patient with
cardiomyopathy would include improved or maintained
cardiac output
– Rest, positioning (legs down), supplemental O2,
– medications, low Na diet, avoid dehydration
• Increase activity tolerance and improving gas exchange
– Cycle rest and activity, ensure patient recognizes
symptoms that indicate the need for rest
• Reduce anxiety
– Eradicate or alleviate perceived stressors, educate family
about diagnosis, assist with anticipatory grieving
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Process: The Patient With
Cardiomyopathy (Nursing Interventions) #2
• Decrease the sense of powerlessness
– Assist patients in identifying things that have been
lost (i.e., ability to play sports), assist patients in
identifying amount of control they still have left
• Promote home- and community-based care
– Educate patients about ways to balance lifestyle and
work while accomplishing therapeutic activities
– Assess patient and family and their adjustment to
lifestyle changes, educate family about CPR and
AEDs, establish trust
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Process: The Patient With
Cardiomyopathy (Evaluation) #1
• Maintain or improve cardiac function
– HR and RR WNL, decreased dyspnea and increased
comfort, maintain or improve gas exchange, absence
of weight gain, maintain or improve peripheral blood
flow
• Maintain or increase activity tolerance
– Carry out activities of daily living (e.g., brush teeth,
feed self), reports increased tolerance to activity
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Nursing Process: The Patient With
Cardiomyopathy (Evaluation) #2
• Reduce anxiety
– Discusses prognosis, verbalizes fears and concerns,
participates in support groups, demonstrates
appropriate coping mechanisms
• Decrease sense of powerlessness
– Identifies emotional response to diagnosis, discusses
control that he or she has
• Adhere to self-care program
– Takes medications as prescribed, modifies diet to
accommodate sodium and fluid recommendations,
modifies lifestyle, identifies S&S to be reported
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Cardiomyopathy
• When heart failure progresses and medical treatment is
no longer effective, surgical intervention, including heart
transplantation, is considered.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Infectious Diseases of the Heart
• Any of the layers of the heart may be affected by an
infectious process.
• Diseases are named by the layer of the heart that is
affected.
• Diagnosis is made by patient symptoms and
echocardiogram.
• Blood cultures may be used to identify the infectious
agent and to monitor therapy.
• Treatment is with appropriate antimicrobial therapy.
Patients require teaching to complete the course of
appropriate antimicrobial therapy and require teaching
for infection prevention and health promotion.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Types of Infectious Disease of the Heart
• Rheumatic endocarditis
– Occurs most often in school-age children after group A beta-hemolytic
streptococcal pharyngitis; need to promptly recognize and treat “strep”
throat to prevent rheumatic fever
• Infective endocarditis
– Usually develops in people with prosthetic heart valves or structural
cardiac defects; also occurs in patients who are IV drug abusers and in
those with debilitating diseases, indwelling catheters, or prolonged IV
therapy
– The physician's choice of antibiotics would be primarily based on Blood
cultures
– Group A streptococcus can cause rheumatic heart fever, resulting in
rheumatic endocarditis. Being aware of signs and symptoms of
streptococcal infections, identifying them quickly, and treating them
promptly, are the best preventative techniques for rheumatic
endocarditis
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Types of Infectious Disease of the Heart
• Pericarditis
– Inflammation of the pericardium; many causes; potential complications:
pericardial effusion and cardiac tamponade
– The most characteristic symptom of pericarditis is chest pain, although
pain also may be located beneath the clavicle, in the neck, or in the left
trapezius (scapula) region. The pain or discomfort usually remains fairly
constant, but it may worsen with deep inspiration and when lying down
or turning. A pericardial friction rub is diagnostic of pericarditis
• Myocarditis
– An inflammatory process involving the myocardium; most common
pathogens involved in myocarditis tend to be viral; in endocarditis, they
tend to be bacterial; complications: cardiomyopathy and heart failure
– The most common symptoms of myocarditis are flulike symptoms
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Clinical Manifestations: Infectious
Diseases of the Heart
Fever
New heart murmur, friction rub at left lower sternal
border (pericarditis)
Osler nodes, Janeway lesions, Roth spots, and splinter
hemorrhages in nailbeds (Rheumatic)
Cardiomegaly, heart failure, tachycardia, splenomegaly
Fatigue, dyspnea, syncope, palpitations, chest pain
(myocarditis)
Diagnostic tools: blood cultures, echocardiogram, CBC,
rheumatoid factor, ESR, CRP, urinalysis, ECG, cardiac
catheterization, TEE, CT scan
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Prevention
• Antibiotic prophylaxis before certain procedures .
Amoxicillin is the drug of choice.
• Ongoing oral hygiene
• Female patients are advised NOT to use IUDs
• Meticulous care should be taken in patients “at risk”
who have catheters
• Catheters should be removed as soon as they are no
longer needed
• Immunizations
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Question #3
A patient with restrictive cardiomyopathy taking digoxin
presents with symptoms of anorexia, nausea, vomiting,
headache, and malaise. What should the nurse expect to
be included in the plan of care for this patient?
A. The patient’s digoxin will be changed to nifedipine.
B. The patient’s digoxin dose will be decreased.
C. Nothing; these are signs of restrictive cardiomyopathy
that are expected.
D. The patient will be admitted to an ICU.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
Answer
B. The patient’s digoxin dose will be
decreased.
Rationale: Patients with restrictive cardiomyopathy are
sensitive to digitalis. Nurses must closely monitor these
patients for digitalis toxicity, which is evidenced by
dysrhythmia, anorexia, nausea, vomiting, headache,
and
malaise. This patient presents with symptoms of digoxin
toxicity, so a decrease in dosage should be anticipated.
These patients should avoid nifedipine, and they do not
need to be admitted to the ICU.
Copyright © 2022 Wolters Kluwer · All Rights Reserved
You might also like
- Print NCLEX Study - Mark Klimek Blue BookDocument17 pagesPrint NCLEX Study - Mark Klimek Blue Booklento1990100% (1)
- ATI Remediation ADocument3 pagesATI Remediation AChelsea PalmaNo ratings yet
- Mark Klimek Full Nclex ReviewerDocument30 pagesMark Klimek Full Nclex ReviewerAlex BellNo ratings yet
- Government College of Nursing: JodhpurDocument9 pagesGovernment College of Nursing: JodhpurpriyankaNo ratings yet
- Hesi Management of A Emergent Care UnitDocument5 pagesHesi Management of A Emergent Care UnitAna Bienne0% (1)
- LPN DELEGATION and PRIORITIZING AND MOREDocument38 pagesLPN DELEGATION and PRIORITIZING AND MOREDebra PowellNo ratings yet
- Thinking Like A NurseDocument3 pagesThinking Like A Nurseapi-519359726No ratings yet
- ATI Practice CodesDocument1 pageATI Practice Codesvanassa johnson100% (4)
- VATI Mental Health RemediationDocument2 pagesVATI Mental Health RemediationestberryNo ratings yet
- ISBAR Worksheet Olivia Jones Jasgou1752Document1 pageISBAR Worksheet Olivia Jones Jasgou1752Jasmyn Rose100% (1)
- NCLEX RN Review For Reduction of Risk PotentialDocument7 pagesNCLEX RN Review For Reduction of Risk Potentialpaulinatia100% (1)
- Sample Psychotherapy NoteDocument2 pagesSample Psychotherapy NoteRafael Sanchez100% (3)
- Adult1 27 - 28Document78 pagesAdult1 27 - 28Ahmed AbahraNo ratings yet
- Hinkle PPT CH 28Document34 pagesHinkle PPT CH 28Ahmed AbahraNo ratings yet
- A Nurse's Guide to Caring for Cardiac Intervention PatientsFrom EverandA Nurse's Guide to Caring for Cardiac Intervention PatientsNo ratings yet
- Mitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandMitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Chapter27-Assessment and Management of Patients With HypertensionDocument31 pagesChapter27-Assessment and Management of Patients With HypertensionAhmed 123No ratings yet
- Gastric and Duodenal Disorders - Test 4Document21 pagesGastric and Duodenal Disorders - Test 4Vickie BuckerNo ratings yet
- 1 - Yellow BookDocument49 pages1 - Yellow Booksushma.rayamajhi.bsc06No ratings yet
- Immunity 1Document6 pagesImmunity 1Tori RolandNo ratings yet
- Acute Kidney Injury NCLEXDocument21 pagesAcute Kidney Injury NCLEXSameerQadumi100% (1)
- NURS 460 Nursing Licensure Examination Course: Jv7@hawaii - EduDocument5 pagesNURS 460 Nursing Licensure Examination Course: Jv7@hawaii - EduJeffrey ViernesNo ratings yet
- Open Pediatric ArcherDocument84 pagesOpen Pediatric Archerbaharada1979No ratings yet
- Nursing ExamDocument8 pagesNursing ExamDa DungNo ratings yet
- Cad PPTDocument81 pagesCad PPTvaishnaviNo ratings yet
- CA RationaleDocument39 pagesCA RationaleSeirah Distor MartinezNo ratings yet
- Bsn-Rs-Careplan 2Document9 pagesBsn-Rs-Careplan 2api-520841770No ratings yet
- Renal & Urinary ATIDocument2 pagesRenal & Urinary ATIHelen Varela100% (1)
- The Client Should Be Instructed As Follows: Intravenous Pyelogram (IVP) Is An X-Ray of The Urinary SystemDocument25 pagesThe Client Should Be Instructed As Follows: Intravenous Pyelogram (IVP) Is An X-Ray of The Urinary SystemElizabeth SharmaNo ratings yet
- Final Study Guide 2Document4 pagesFinal Study Guide 2Nataraj LoganathanNo ratings yet
- Exam ReviewDocument4 pagesExam ReviewMya Thomas100% (1)
- Diet NclexDocument1 pageDiet NclexSoon ShinNo ratings yet
- Neurologic NCLEX Practice Test Part 1Document6 pagesNeurologic NCLEX Practice Test Part 1ojoj2206No ratings yet
- ADEX. MP Resume Template 0604.12 (NY) .6.24.15Document3 pagesADEX. MP Resume Template 0604.12 (NY) .6.24.15Mjay GuintoNo ratings yet
- Brain Dump NUR 213 FINALDocument37 pagesBrain Dump NUR 213 FINALkelsey jackson100% (1)
- Review Notes For NCLEX CGFNS - Aortic AneurysmsDocument2 pagesReview Notes For NCLEX CGFNS - Aortic Aneurysmswyndz100% (3)
- ATI Comprehensive Predictor: Study Online atDocument9 pagesATI Comprehensive Predictor: Study Online atVanessaMUellerNo ratings yet
- IV PDFDocument63 pagesIV PDFelbagouryNo ratings yet
- Dysrhythmia TestsDocument3 pagesDysrhythmia TestsKimberly WhitesideNo ratings yet
- Hematologic System2Document70 pagesHematologic System2Jesus Mario LopezNo ratings yet
- Fluids and Electrolytes: Irene L. Gardiner, MDDocument48 pagesFluids and Electrolytes: Irene L. Gardiner, MDGabriel Carlo FranciscoNo ratings yet
- Hesi Management of A Medical UnitDocument2 pagesHesi Management of A Medical UnitAna Bienne100% (1)
- Hyperemesis Gravidarum: Bleeding Complications of PregnancyDocument6 pagesHyperemesis Gravidarum: Bleeding Complications of PregnancykirbsNo ratings yet
- NCLEX Quick FactsDocument7 pagesNCLEX Quick FactsMary Aurine FullanteNo ratings yet
- GuideDocument5 pagesGuideHu Tao100% (1)
- Ms Flash CardsDocument15 pagesMs Flash CardsMia MalazoNo ratings yet
- Medical Surgical Nursing - DiabetesDocument4 pagesMedical Surgical Nursing - Diabetestripj33100% (2)
- AdultDocument295 pagesAdultKen WonNo ratings yet
- HESI Medsurg V2Document26 pagesHESI Medsurg V2aasthabhattarai07No ratings yet
- 8 Essential Concepts 4 NCLEX RN-4Document6 pages8 Essential Concepts 4 NCLEX RN-4Jot grewalNo ratings yet
- Answers and Rationales For NCLEX Style Review QuestionsDocument12 pagesAnswers and Rationales For NCLEX Style Review QuestionsJacinth Florido Fedelin50% (2)
- Camporedondo, Bryan C. RLE8 - Group5 Emergency Drugs: Atropine SulfateDocument4 pagesCamporedondo, Bryan C. RLE8 - Group5 Emergency Drugs: Atropine SulfateIglesia Ni Cristo DoctorsNo ratings yet
- Remar WorkbookDocument60 pagesRemar Workbookharsimranr761100% (1)
- Entry To Practice RPNDocument20 pagesEntry To Practice RPNDivina D Galvez-BeronioNo ratings yet
- 7th Edition All NeuroDocument92 pages7th Edition All NeuroCrystal LynaeNo ratings yet
- Ignatavicius TOCDocument9 pagesIgnatavicius TOCjennaaahhhNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- Navigating Long-Term Care - A Practical Approach for NursesFrom EverandNavigating Long-Term Care - A Practical Approach for NursesNo ratings yet
- Registered Professional Nurse: Passbooks Study GuideFrom EverandRegistered Professional Nurse: Passbooks Study GuideNo ratings yet
- 7 - PainDocument22 pages7 - Painسلطان محمد فوزي سلمانNo ratings yet
- 10 - Care at The End of LifeDocument23 pages10 - Care at The End of Lifeسلطان محمد فوزي سلمانNo ratings yet
- 3 - Common Aging ChangesDocument41 pages3 - Common Aging Changesسلطان محمد فوزي سلمانNo ratings yet
- 4 NutritionDocument30 pages4 Nutritionسلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شـابـتـر ١٣?Document18 pagesتَـلـخـيـص شـابـتـر ١٣?سلطان محمد فوزي سلمانNo ratings yet
- Chapter 67 Management of Patients With Cerebrovascular DisordersDocument41 pagesChapter 67 Management of Patients With Cerebrovascular Disordersسلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شـابـتـر ١٤?Document21 pagesتَـلـخـيـص شـابـتـر ١٤?سلطان محمد فوزي سلمانNo ratings yet
- تَـلخـيـص شـابـتـر ٢٠?Document17 pagesتَـلخـيـص شـابـتـر ٢٠?سلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شـابـتـر ١٢?Document11 pagesتَـلـخـيـص شـابـتـر ١٢?سلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شَـابـتـر ٢٣?Document10 pagesتَـلـخـيـص شَـابـتـر ٢٣?سلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شَـابـتـر ٢٥?Document12 pagesتَـلـخـيـص شَـابـتـر ٢٥?سلطان محمد فوزي سلمانNo ratings yet
- تَـلـخـيـص شـابـتـر ٢٦?Document15 pagesتَـلـخـيـص شـابـتـر ٢٦?سلطان محمد فوزي سلمانNo ratings yet
- Bundle Fundamentals of Nursing PDFDocument59 pagesBundle Fundamentals of Nursing PDFسلطان محمد فوزي سلمانNo ratings yet
- Weekly Objective Form - NEWDocument3 pagesWeekly Objective Form - NEWسلطان محمد فوزي سلمانNo ratings yet
- Medical Care Plan - NEWDocument4 pagesMedical Care Plan - NEWسلطان محمد فوزي سلمانNo ratings yet
- Infection and Infectious ProcessDocument44 pagesInfection and Infectious Processpandey omkarNo ratings yet
- Merrf Syndrome BeverlyDocument4 pagesMerrf Syndrome BeverlyQuezon D. Lerog Jr.No ratings yet
- Research in Public Health by Prof DR Rwamakuba ZephanieDocument120 pagesResearch in Public Health by Prof DR Rwamakuba ZephanieDr Zephanie RwamakubaNo ratings yet
- Mims Jpog August 2015 IdDocument70 pagesMims Jpog August 2015 IdDika MidbrainNo ratings yet
- Chakrabarti, 1986Document4 pagesChakrabarti, 1986Jessica VanyaNo ratings yet
- Mesna: Mesna, Sold Under The BrandDocument17 pagesMesna: Mesna, Sold Under The BrandAndry HamdaniNo ratings yet
- NeoBip Clinical Guide 2020.9.4Document11 pagesNeoBip Clinical Guide 2020.9.4TECHMED REPAIRS TECHMED SALESNo ratings yet
- ID Gambaran Histologik Hati Pada Kelinci Ya PDFDocument5 pagesID Gambaran Histologik Hati Pada Kelinci Ya PDFYudha Jrokolioli NostNo ratings yet
- New Vistas In: Fetal MedicineDocument2 pagesNew Vistas In: Fetal MedicineRaviraj TirukeNo ratings yet
- Liver Cirrhosis Case Study Polish Male 56 PDFDocument3 pagesLiver Cirrhosis Case Study Polish Male 56 PDFHlamin OoNo ratings yet
- 1-Clinical ParasitologyDocument44 pages1-Clinical ParasitologyMohiedden M Abdul-FattahNo ratings yet
- Acute Renal Failure DR Kwaifa.2Document170 pagesAcute Renal Failure DR Kwaifa.2DICKSONNo ratings yet
- Expanded Program On Immunization (EPI) : Minimum Age at 1st Dose Number of Doses Dose Route SiteDocument2 pagesExpanded Program On Immunization (EPI) : Minimum Age at 1st Dose Number of Doses Dose Route SiteYana DugayNo ratings yet
- Department of Bio-Informatics 3 Semester (Morning) : Subject ImmunologyDocument10 pagesDepartment of Bio-Informatics 3 Semester (Morning) : Subject ImmunologyShaher Bano MirzaNo ratings yet
- Approach To A Child With Chronic Diarrhea: Parijat R. Tripathi Anshu SrivastavaDocument9 pagesApproach To A Child With Chronic Diarrhea: Parijat R. Tripathi Anshu SrivastavaTrọng PhướcNo ratings yet
- Eye Drops: Drug StudyDocument3 pagesEye Drops: Drug StudyChris PaguioNo ratings yet
- Pain Management Guide PDFDocument5 pagesPain Management Guide PDFPriydarshni KohliNo ratings yet
- Jurnal Penyakit Arteri PeriferDocument12 pagesJurnal Penyakit Arteri Perifereka saptaning windu fitriNo ratings yet
- Neurocritical CareDocument337 pagesNeurocritical Cares SNo ratings yet
- Neurogeriatria 2017 PDFDocument417 pagesNeurogeriatria 2017 PDFWilfredo DavilaNo ratings yet
- Atrial FibrillationDocument390 pagesAtrial FibrillationAlexandra Carmen100% (1)
- Sepsis Proposal1Document34 pagesSepsis Proposal1Appiah Peter OforiNo ratings yet
- Interpretation: L55 - PSC Indra Nagar Home Visit GRD FLR 197/A, Indra Nagar, Double ROAD, BANGALORE - 560080 BangaloreDocument2 pagesInterpretation: L55 - PSC Indra Nagar Home Visit GRD FLR 197/A, Indra Nagar, Double ROAD, BANGALORE - 560080 BangaloreDivyaSNo ratings yet
- Osha Rkforms Winstr - Fillable PDFDocument12 pagesOsha Rkforms Winstr - Fillable PDFBerhanu BedassaNo ratings yet
- Clinical Review Memo, August 23, 2021 - COMIRNATYDocument108 pagesClinical Review Memo, August 23, 2021 - COMIRNATYadrianoucamNo ratings yet
- Deep Vein Thrombosis in Pregnancy - Epidemiology, Pathogenesis, and Diagnosis - UpToDateDocument26 pagesDeep Vein Thrombosis in Pregnancy - Epidemiology, Pathogenesis, and Diagnosis - UpToDateCristinaCaprosNo ratings yet
- Narrative Pathophysiology of PregnancyDocument2 pagesNarrative Pathophysiology of PregnancyMarvin ChulyaoNo ratings yet
- Fat EmbolismDocument4 pagesFat EmbolismAmmar HasyimNo ratings yet