Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
7 viewsOrgans of Head&neck
Organs of Head&neck
Uploaded by
raphaelyohana140The document discusses the anatomy of the nose and ear. It describes the skeletal structure of the nose including the nasal bones, maxillae and frontal bone. It discusses the vascular, lymphatic and nervous supply to the nose. It describes the nasal cavity and its functions. It then discusses the anatomy of the external, middle and inner ear. It describes the structures of the auricle, external acoustic meatus, tympanic membrane and middle ear bones. It provides clinical correlations regarding nosebleeds, sinusitis and ear infections.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You might also like
- Vent Modes ChartDocument1 pageVent Modes Chartladyhavocinc100% (1)
- Spice Rack Real Time Analysis of Speaker: Name NameDocument9 pagesSpice Rack Real Time Analysis of Speaker: Name NameFortuna Power TECHNOLOGYNo ratings yet
- Anatomy and Physiology of The Ear PDFDocument12 pagesAnatomy and Physiology of The Ear PDFDeshini Balasubramaniam83% (6)
- Anatomy and Physiology of The NoseDocument6 pagesAnatomy and Physiology of The NoseManveer DhaliwalNo ratings yet
- Anatomy of The External EarDocument28 pagesAnatomy of The External Earhama100% (1)
- Colon Cancer Pathophysiology PDFDocument2 pagesColon Cancer Pathophysiology PDFMaggieNo ratings yet
- Middle Ear - Earth's LabDocument1 pageMiddle Ear - Earth's Labmfk5p77t8mNo ratings yet
- By DR Manah Chandra Changmai MBBS MSDocument31 pagesBy DR Manah Chandra Changmai MBBS MSKalaivaany RamachandranNo ratings yet
- Ear Anatomy and PhysiologyDocument50 pagesEar Anatomy and Physiologyxj74fr4ddxNo ratings yet
- Parasinus AnatomyDocument6 pagesParasinus Anatomyalexandra663No ratings yet
- 1 RHINOLOGY NoseDocument116 pages1 RHINOLOGY NoseWai Kwong ChiuNo ratings yet
- Prof. DR - Mohamed Talaat ElghonemyDocument49 pagesProf. DR - Mohamed Talaat Elghonemyadel madanyNo ratings yet
- The EarDocument13 pagesThe EarOjambo FlaviaNo ratings yet
- Case Report CSOMDocument13 pagesCase Report CSOMNashria RusdhyNo ratings yet
- ورق مذاكره PDFDocument100 pagesورق مذاكره PDFsalamred100% (1)
- Anatomy of EarDocument17 pagesAnatomy of Earkresha solankiNo ratings yet
- Nasal AnatomyDocument23 pagesNasal AnatomyArchanaShenoyNo ratings yet
- Potongan CSOM Part 2Document12 pagesPotongan CSOM Part 2Athanasius WrinNo ratings yet
- Anatomy and Physiology of The Nose and Paranasal SinusesDocument2 pagesAnatomy and Physiology of The Nose and Paranasal SinusesNuardi YusufNo ratings yet
- Anatomy NoseDocument35 pagesAnatomy Noseضبيان فرحانNo ratings yet
- Anatomy Lec.1 Nasal Cavities and Paranasal SinusesDocument21 pagesAnatomy Lec.1 Nasal Cavities and Paranasal Sinusesزينب فؤاد موسىNo ratings yet
- PBL - THT HidungDocument35 pagesPBL - THT Hidungdian novitasariNo ratings yet
- NOSEDocument6 pagesNOSEAjigotto ubiq.No ratings yet
- Anatomy and Physiology of Ent-OrgansDocument52 pagesAnatomy and Physiology of Ent-OrgansdrghassanNo ratings yet
- Nose Dr. A. S. D' SouzaDocument18 pagesNose Dr. A. S. D' SouzaNariska CooperNo ratings yet
- Anatomy EarDocument20 pagesAnatomy EarRod HilalNo ratings yet
- Exterior and Middle EarDocument26 pagesExterior and Middle EarAndra BauerNo ratings yet
- Anatomy of External Ear, Middle Ear and MastoidDocument66 pagesAnatomy of External Ear, Middle Ear and Mastoiddebdeepbhattacharya411No ratings yet
- Otitis Media AkutDocument24 pagesOtitis Media AkutBethari K AbiantiNo ratings yet
- The Ear: Head & Neck Unit - مسعسلا ليلج رديح .دDocument20 pagesThe Ear: Head & Neck Unit - مسعسلا ليلج رديح .دStevanovic StojaNo ratings yet
- Lectures, WordDocument27 pagesLectures, Word9xymc5pcyzNo ratings yet
- 28 Temporal Bone (Done)Document7 pages28 Temporal Bone (Done)Ayah HyasatNo ratings yet
- Part 2 The Nose, Paranasal Sinuses and PharnyxDocument12 pagesPart 2 The Nose, Paranasal Sinuses and PharnyxLauraDernNo ratings yet
- AnatomyDocument15 pagesAnatomyAdeleye John AdebolaNo ratings yet
- 15-Sensory OrgansDocument23 pages15-Sensory OrgansMilad HabibiNo ratings yet
- Anatomy of The Nose and Paranasal SinusDocument5 pagesAnatomy of The Nose and Paranasal Sinusbayoe_pra100% (1)
- Demo Class of EarDocument54 pagesDemo Class of EarMegha BhengraNo ratings yet
- Good Afternoon EverybodyDocument131 pagesGood Afternoon EverybodyIhsan HanifNo ratings yet
- 12 - Anatomy of The NoseDocument32 pages12 - Anatomy of The Nosehanizulfani13No ratings yet
- Chronic Suppurative Otitis MediaDocument16 pagesChronic Suppurative Otitis MediaAndrei Rizqan AkmalNo ratings yet
- Anatomy of External EarDocument49 pagesAnatomy of External EarInderdeep AroraNo ratings yet
- Anatomy EarDocument44 pagesAnatomy Earrinaldy agungNo ratings yet
- EarDocument6 pagesEarDr.Mahesh kumar GuptaNo ratings yet
- Anatomy EarDocument44 pagesAnatomy Earrinaldy agungNo ratings yet
- Anatomy and Physiology THT - Dr. AriefDocument88 pagesAnatomy and Physiology THT - Dr. AriefGilbert Sterling OctaviusNo ratings yet
- Upper Respiratory Tract AnatomyDocument61 pagesUpper Respiratory Tract Anatomyيحيى اسماعيل الجميليNo ratings yet
- Presentation On Nasal ObstructionDocument111 pagesPresentation On Nasal Obstructionbatookhan100% (2)
- Anatomy, Physiology of ENT For Paramedics - Dr. Fuad RidhaDocument52 pagesAnatomy, Physiology of ENT For Paramedics - Dr. Fuad Ridhafuadredza100% (1)
- Eternal and Middle Ear AarogyaDocument66 pagesEternal and Middle Ear AarogyaAarooNo ratings yet
- The Vestibulocochlear Organ: China Medical UniversityDocument30 pagesThe Vestibulocochlear Organ: China Medical UniversityDONALD UNASHENo ratings yet
- Anatomy Physiology of The EarDocument8 pagesAnatomy Physiology of The EargheaastridgayatriNo ratings yet
- Middle EarDocument16 pagesMiddle EarproshishNo ratings yet
- 01.anatomy of The EarDocument52 pages01.anatomy of The EarJumanne Jay100% (2)
- Paranasal Sinus Anatomy - Overview, Gross Anatomy, Microscopic AnatomyDocument12 pagesParanasal Sinus Anatomy - Overview, Gross Anatomy, Microscopic AnatomyKienlevy100% (1)
- Special Senses 1 NDocument179 pagesSpecial Senses 1 Naoujahmed123456789010No ratings yet
- W2-7 Ear and Nose LectureDocument52 pagesW2-7 Ear and Nose LectureSAHIL AGARWALNo ratings yet
- G5 Nasal CavityDocument41 pagesG5 Nasal CavityGuo YageNo ratings yet
- B 22-Rs-Anatomy - Saq AnswersDocument22 pagesB 22-Rs-Anatomy - Saq Answersapi-516879364No ratings yet
- External EarDocument3 pagesExternal EarbarbacumlaudeNo ratings yet
- A Simple Guide to the Ear and Its Disorders, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to the Ear and Its Disorders, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Encyclopaedia Britannica, 11th Edition, Volume 13, Slice 2 "Hearing" to "Helmond"From EverandEncyclopaedia Britannica, 11th Edition, Volume 13, Slice 2 "Hearing" to "Helmond"No ratings yet
- Encyclopaedia Britannica, 11th Edition, Volume 13, Slice 2 "Hearing" to "Helmond"From EverandEncyclopaedia Britannica, 11th Edition, Volume 13, Slice 2 "Hearing" to "Helmond"No ratings yet
- 4 - Protein SynthesisDocument66 pages4 - Protein Synthesisraphaelyohana140No ratings yet
- Muscles of Facial ExpressionDocument63 pagesMuscles of Facial Expressionraphaelyohana140No ratings yet
- 6 - NM2 Action PotentialDocument48 pages6 - NM2 Action Potentialraphaelyohana140No ratings yet
- Head AnatomyDocument66 pagesHead Anatomyraphaelyohana140No ratings yet
- H.anatomy IntroductionDocument60 pagesH.anatomy Introductionraphaelyohana140No ratings yet
- 16) Signaling Pathways That Control Gene ActivityDocument27 pages16) Signaling Pathways That Control Gene ActivityRNo ratings yet
- (Reviews in Mineralogy and Geochemistry'', 54) Patricia M. Dove, James J. de Yoreo, Steve Weiner-Biomineralization-Mineralogical Society of America (2003)Document377 pages(Reviews in Mineralogy and Geochemistry'', 54) Patricia M. Dove, James J. de Yoreo, Steve Weiner-Biomineralization-Mineralogical Society of America (2003)Karlii BasilioNo ratings yet
- L A Level Biology MS Jan 05Document180 pagesL A Level Biology MS Jan 05annakaranovaNo ratings yet
- Op Art and Visual PerceptionDocument26 pagesOp Art and Visual PerceptionFelipeCussenNo ratings yet
- Cklistskill 43 Oxygen AdministrationDocument3 pagesCklistskill 43 Oxygen AdministrationGalenn BarrionNo ratings yet
- Interactive National Vital Sign Chart July 2017Document2 pagesInteractive National Vital Sign Chart July 2017basheNo ratings yet
- Life ProcessesDocument12 pagesLife ProcessesJeevansh WadhwaNo ratings yet
- Niraamaya Spa MenuDocument35 pagesNiraamaya Spa MenuSanjeev HariharanNo ratings yet
- Sports Exercise and Health Science Paper 2 SL MarkschemeDocument21 pagesSports Exercise and Health Science Paper 2 SL Markschemegoingnow0001No ratings yet
- Maxillary Air Sinus Oral SurgeryDocument49 pagesMaxillary Air Sinus Oral SurgeryDentist Dina SamyNo ratings yet
- Foods That Cause Acne: SUNDAY, APRIL 8, 2012Document3 pagesFoods That Cause Acne: SUNDAY, APRIL 8, 2012FitriAndriyaniNo ratings yet
- Night Shifts Can Also Be TiringDocument2 pagesNight Shifts Can Also Be TiringMariccon Celestial PalmaNo ratings yet
- Amino Acids and Proteins ReviewerDocument11 pagesAmino Acids and Proteins ReviewerJohn-Karl JimenezNo ratings yet
- Saliva and Its Importance in Complete Denture ProsthodonticsDocument8 pagesSaliva and Its Importance in Complete Denture ProsthodonticsKrupali JainNo ratings yet
- SSGBIO1 - CM Week 1Document16 pagesSSGBIO1 - CM Week 1sgdick31No ratings yet
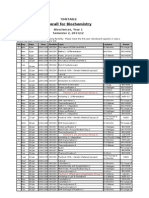
- Semester 2 Biochem TimetableDocument1 pageSemester 2 Biochem TimetablesophiecabNo ratings yet
- 11 - Head & Neck (Blood Vessels) (FF) - Part 1Document20 pages11 - Head & Neck (Blood Vessels) (FF) - Part 1checkmate100% (1)
- Kidney Problems and DialysisDocument3 pagesKidney Problems and DialysismarymakinNo ratings yet
- Review On Animal and Plant CellDocument3 pagesReview On Animal and Plant CellLadymae GalolaNo ratings yet
- HUBS1105 Bones and Joints of The Skull and FaceDocument5 pagesHUBS1105 Bones and Joints of The Skull and FaceChloe HeuchanNo ratings yet
- Pathophysiology Exam 4 - ReviewDocument18 pagesPathophysiology Exam 4 - ReviewWaqas GillNo ratings yet
- Staar g3 2016test Read FDocument33 pagesStaar g3 2016test Read FsatishNo ratings yet
- Special ArticlesDocument12 pagesSpecial ArticlesMichael Vincent MercadoNo ratings yet
- Life Processes Case Based QuestionsDocument21 pagesLife Processes Case Based Questionsvaibhav08112008No ratings yet
- Resume - Natalia MathesonDocument2 pagesResume - Natalia Mathesonapi-449546352No ratings yet
- A Whole Bouquet For YouDocument334 pagesA Whole Bouquet For YoujdgjhsbjhbsNo ratings yet
- Degradation of Cytokinins by Cytokinin Oxidases in PlantsDocument13 pagesDegradation of Cytokinins by Cytokinin Oxidases in PlantsRoikka HazarikaNo ratings yet
Organs of Head&neck
Organs of Head&neck
Uploaded by
raphaelyohana1400 ratings0% found this document useful (0 votes)
7 views143 pagesThe document discusses the anatomy of the nose and ear. It describes the skeletal structure of the nose including the nasal bones, maxillae and frontal bone. It discusses the vascular, lymphatic and nervous supply to the nose. It describes the nasal cavity and its functions. It then discusses the anatomy of the external, middle and inner ear. It describes the structures of the auricle, external acoustic meatus, tympanic membrane and middle ear bones. It provides clinical correlations regarding nosebleeds, sinusitis and ear infections.
Original Description:
Original Title
ORGANS OF HEAD&NECK
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses the anatomy of the nose and ear. It describes the skeletal structure of the nose including the nasal bones, maxillae and frontal bone. It discusses the vascular, lymphatic and nervous supply to the nose. It describes the nasal cavity and its functions. It then discusses the anatomy of the external, middle and inner ear. It describes the structures of the auricle, external acoustic meatus, tympanic membrane and middle ear bones. It provides clinical correlations regarding nosebleeds, sinusitis and ear infections.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
7 views143 pagesOrgans of Head&neck
Organs of Head&neck
Uploaded by
raphaelyohana140The document discusses the anatomy of the nose and ear. It describes the skeletal structure of the nose including the nasal bones, maxillae and frontal bone. It discusses the vascular, lymphatic and nervous supply to the nose. It describes the nasal cavity and its functions. It then discusses the anatomy of the external, middle and inner ear. It describes the structures of the auricle, external acoustic meatus, tympanic membrane and middle ear bones. It provides clinical correlations regarding nosebleeds, sinusitis and ear infections.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 143
ORGANS OF HEAD
Surface appearance of the nose.
Skeletal Structure
Bony component –Nasal bones, maxillae and
frontal bone.
Cartilaginous component –Two lateral
cartilages, two alar cartilages and one septal
cartilage.
Skin over the bony part of the nose is thin
That overlying the cartilaginous part is thicker
with many sebaceous glands.
Venous drainage is into the facial vein, and then
in turn into the internal jugular vein.
Lymphatic drainage from the external nose is
via superficial lymphatic vessels accompanying the
facial vein.
Then into deep cervical lymph nodes.
Clinical Relevance: Danger Triangle of the Face
The venous drainage of the nose and surrounding
area has communication between the facial
vein and cavernous sinus, via the ophthalmic
vein.
Innervation
Sensory innervation - trigeminal nerve (CN V).
The external nasal nerve, (CN V1), supplies the
skin of the dorsum of nose, nasal alae and nasal
vestibule.
The lateral aspects of the nose are supplied by
the infrorbital nerve, (CN v2).
Motor innervation to the nasal muscles of facial
expression is via the facial nerve (CN VII).
The nasal cavity has four functions:
Warms and humidifies the inspired air.
Removes and traps pathogens and particulate
matter from the inspired air.
Responsible for sense of smell.
Drains and clears the paranasal sinuses and
lacrimal ducts.
DIVISIONS OF NASAL CAVITY
Sagittal section of the nasal cavity. Conchae are present
on the lateral walls
Coronal section of the anterior nasal cavity. The spheno-
ethmoidal recess is located posteriorly, and not visible
on this diagram.
Openings into the Nasal Cavity
The paranasal sinuses -The frontal, maxillary
and anterior ethmoidal sinuses open into the
middle meatus.
The sphenoid sinus drains onto the posterior
roof.
Nasolacrimal duct – acts to drain tears from the
eye and opens into the inferior meatus.
Auditory (Eustachian) tube – opens into the
nasopharynx at the level of the inferior meatus and
allows the middle ear to equalize with the
atmospheric air pressure.
Clinical Relevance: Spread of Infection
As the auditory tube connects the middle ear and
upper respiratory tract, it is a path by
which infection can spread from the upper
respiratory tract to the ear.
Infection of the auditory tube causes swelling of
the mucous linings, and the tube becomes blocked.
This results in diminished hearing.
The conchae have been removed, showing the various
openings on the lateral wall of the nasal cavity.
Gateways to the Nasal Cavity
The cribriform plate part of the ethmoid bone,
allowing fibres of the olfactory nerve to enter and
exit
At superior meatus, the sphenopalatine
foramen allows communication between the nasal
cavity and the pterygopalatine fossa.
The sphenopalatine artery, nasopalatine and
superior nasal nerves pass through here.
The incisive canal is a pathway between the nasal
cavity and the incisive fossa of the oral cavity.
It transmits the nasopalatine nerve and greater
palatine artery.
Opening of the pterygopalatine fossa (circled in red).
Vasculature
The nose receives blood from both the internal
and external carotid arteries:
Internal carotid branches:
Anterior ethmoidal artery
Posterior ethmoidal artery
They descend into the nasal cavity through the
cribriform plate
External carotid branches:
Sphenopalatine artery
Greater palatine artery
Superior labial artery
Lateral nasal arteries
Divisions of Maxillary artery:
3 parts by lateral pterygoid
1st part (Mandibular part): winds around deep
to neck of mandible
2nd part (Pterygoid part): travels between 2
heads of lateral pterygoid
3rd part (Pterygopalatine part): enters
pterygopalatine fossa containing
pterygopalatine ganglion
Branches of maxillary Artery
FIRST PART(DAMIA)
5Ms(Meatus (External auditory meatus),Meninges and
mater (duramater),Meckel’s cave, Mandible, Membrane
(tympanic membrane)
Deep auricular artery: External acoustic
meatus
Anterior tympanic artery: Tympanic
membrane
Middle meningeal artery: Dura mater and
Skull bones
Inferior alveolar artery: Mandible
Accessory meningeal artery: Middle fossa -
dura mater and Meckel’s cave (trigeminal
ganglion)
SECOND PART(MUSCLES OF
MASTICATION)
Anterior and Posterior Deep temporal artery:
Temporalis
Pterygoid artery: Lateral and medial pterygoids
Masseteric artery: Masseter
Buccal of Buccinator artery: Buccinator
THIRD PART( FIVE Ps + I)
Posterior superior alveolar artery: Maxilla
Pterygoid canal artery: Upper part of pharynx
and tympanic cavity
Palatine – Descending palatine artery: Gives off
greater and lesser palatine artery and supplies
hard and soft palate respectively
Palatine – Sphenopalatine or Nasopalatine
artery: Supplies nasal cavity
Pharyngeal artery: Pharynx
Infraorbital artery which gives off Anterior and
Middle Superior Alveolar Artery.
Little’s area and the arterial supply to the nose.
Clinical Relevance: Epistaxis
Epistaxis is the medical term for a nosebleed.
Due to the rich blood supply of the nose, this is a
common occurrence.
It is most likely to occur in the anterior third of the
nasal cavity – this area is known as
the Kiesselbach area.
The cause can be local (such as trauma),
or systemic (such as hypertension).
Innervation
Special sensory innervation is carried out by
the olfactory nerves.
General sensory innervation to the septum and
lateral walls is delivered by the nasopalatine
nerve (branch of maxillary nerve) and
the nasociliary nerve (branch of the ophthalmic
nerve).
Innervation to the external skin of the nose is
supplied by the trigeminal nerve.
Lateral view of the nasal septum. Note the close
relationship of the olfactory bulb and cribriform plate
Clinical Relevance: Cribriform Plate Fracture
A fractured cribriform plate can penetrate
the meningeal linings of the brain, causing
leakage of cerebro-spinal fluid.
Exposing the brain to the outside environment
like this increases the risks of meningitis,
encephalitis and cerebral abscesses.
The olfactory bulb lies on the cribriform plate
and can be damaged irreversibly by the fracture.
In this case, the patient may present
with anosmia (loss of smell).
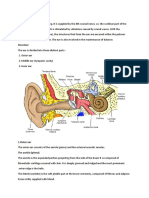
The ear
Divided into three parts; external, middle
and inner
The external ear
Divided functionally and structurally into two
parts; the auricle (or pinna), and the external
acoustic meatus – which ends at the tympanic
membrane.
Overview of the ear
Auricle
Captures and direct sound waves towards the
external acoustic meatus.
The cartilaginous part of the auricle forms an
outer curvature, known as the helix.
A second innermost curvature runs in parallel
with the helix – the antihelix.
The antihelix divides into two cura; the
inferoanterior crus, and the superoposterior crus.
In the middle of the auricle is a hollow depression,
called the concha.
Anterior surface of the auricle of the
external ear.
AURICULAR HAEMATOMA
External Acoustic Meatus
A sigmoid shaped tube that extends from the deep
part of the concha to the tympanic membrane.
The walls of the external 1/3 are formed by
cartilage, whereas the inner 2/3 are formed by the
temporal bone.
Tympanic Membrane
Translucent and middle ear structures can be
observed during otoscopy.
On its inner surface, the handle of malleus
attaches to it, at a point called the umbo
The tympanic membrane of the ear.
Clinical Relevance: Perforation of the Tympanic
Membrane
An infection of the middle ear (otitis media) causes
pus and fluid to build up behind the tympanic
membrane.
This causes an increase in pressure within the middle
ear, and eventually the eardrum can rupture.
Vasculature
The external ear is supplied by branches of
the external carotid artery:
Posterior auricular artery
Superficial temporal artery
Occipital artery
Maxillary artery (deep auricular branch) –
supplies the deep aspect of the external acoustic
meatus and tympanic membrane only.
Venous follows the arteries listed above.
Innervation
The skin of the auricle is by
Greater auricular nerve (branch of the cervical
plexus) – innervates the skin of the auricle
Lesser occipital nerve (branch of the cervical
plexus) – innervates the skin of the auricle
Auriculotemporal nerve (branch of the
mandibular nerve) – innervates the skin of the
auricle and external auditory meatus.
INNERVATION OF THE FACE
Branches of the facial and Vagus nerves –
innervates the deeper aspect of the auricle and
external auditory meatus
Involuntary cough when cleaning ears is due to
stimulation of the auricular branch of the Vagus
nerve
Lymphatics
The lymphatic drainage of the external ear is to
the superficial parotid, mastoid, upper deep
cervical and superficial cervical nodes.
Parts of the Middle Ear
Tympanic cavity
It contains three small bones known as the
auditory Ossicles: the malleus, incus and stapes.
They transmit sound vibrations through the
middle ear.
Epitympanic recess – a space superior to the
tympanic cavity, which lies next to the mastoid air
cells.
The malleus and incus partially extend upwards
into the epitympanic recess.
The middle ear. The two main parts of the middle ear
have been labelled.
Bones
They are connected in a chain-like manner,
linking the tympanic membrane to the oval
window of the internal ear
Sound vibrations cause a movement in the
tympanic membrane which then creates
movement, or oscillation, in the auditory ossicles.
This movement helps to transmit the sound waves
from the tympanic membrane of external ear to the
oval window of the internal ear.
The malleus-Largest and most lateral of the ear
bones, attaching to the tympanic membrane, via the
handle of malleus.
Incus – Consists of a body and two limbs.
The body articulates with the malleus, the short limb
attaches to the posterior wall of the middle ear, and the
long limb joins the stapes.
The stapes- Smallest bone in the human body.
It joins the incus to the oval window of the inner ear.
The head articulates with the incus, and the base joins
the oval window.
Bones of the middle ear.
Muscles
Two: Tensor tympani and stapedius. And are
protective
They contract in response to loud noise
protecting the inner ear
This action is known as the acoustic reflex.
The tensor tympani originates from the auditory
tube and attaches to the handle of malleus, pulling
it medially when contracting.
It is innervated by the tensor tympani nerve, a
branch of the mandibular nerve.
The stapedius muscle attaches to the stapes, and
is innervated by the facial nerve.
Auditory Tube
The auditory tube (eustachian tube) is
a cartilaginous and bony tube that connects the
middle ear to the nasopharynx.
It acts to equalise the pressure of the middle ear
to that of the external auditory meatus.
An upper respiratory infection can spread into the
middle ear.
Clinical Relevance: Otitis Media with Effusion
Otitis media with effusion is commonly known
as glue ear.
It arises from persistent dysfunction of the
auditory tube.
If the auditory tube is unable to equalize middle
ear pressure (due to blockage, inflammation,
genetic mutation), a negative pressure develops
inside the middle ear
This negative pressure draws out
a transudate from the mucosa of the middle ear,
creating an environment suitable for pathogens to
replicate and cause infection.
The eardrum is inverted, with fluid visible inside
the ear in OM with effusion.
Mastoiditis
Middle ear infections (otitis media) can spread to
the mastoid air cells.
Due to their porous nature, they are a suitable site
for pathogenic replication.
The mastoid process infection, can spread to
the middle cranial fossa, and into the brain,
causing meningitis.
In mastoiditis, Pus must be drained from the air
cells taking care of nearby facial nerve.
Mastoiditis
The inner ear
Innermost part of the ear, and houses the
vestibulocochlear organs.
It has two main functions:
To convert mechanical signals from the middle
ear into electrical signals, which can transfer
information to the auditory pathway in the brain.
To maintain balance
detecting position and motion.
The inner ear is located within the petrous part of
the temporal bone
The inner ear has two main components
Bony labyrinth
Series of bony cavities within the petrous part of
the temporal bone.
It is composed of the cochlea, vestibule and
three semi-circular canals.
All these structures are lined internally with
periosteum and contain a fluid called perilymph.
Membranous labyrinth
lies within the bony labyrinth.
It consists of the cochlear duct, semi-circular
ducts, utricle and the saccule.
The membranous labyrinth is filled with fluid
called endolymph.
The inner ear has two openings into the middle
ear, both covered by membranes.
The oval window lies between the middle ear and
the vestibule(central part of the bony
labyrinth)
The round window separates the middle ear
from the scala tympani (part of the cochlear duct).
Bony Labyrinth
It consists of three parts – the cochlea, vestibule
and the three semi-circular canals.
Vestibule
The central part of the bony labyrinth.
It is separated from the middle ear by the oval
window, and communicates anteriorly with the
cochlea and posteriorly with the semi-circular
canals.
Two parts of the membranous labyrinth;
the saccule and utricle, are located within the
vestibule.
Cochlea
The cochlea houses the cochlea duct of the
membranous labyrinth – the auditory part of
the inner ear.
It twists upon itself around a central portion of
bone called the modiolus.
Branches from the cochlear portion of
the vestibulocochlear (VIII) nerve are found at
the base of the modiolus.
Extending from the modiolus is a ledge of bone
known as spiral lamina, which attaches to the
cochlear duct, holding it in position.
The three parts of the bony labyrinth.
The presence of the cochlear duct creates two
perilymph-filled chambers above and below:
Scala vestibuli: Located superiorly to the
cochlear duct. As its name suggests, it is
continuous with the vestibule.
Scala tympani: Located inferiorly to the cochlear
duct. It terminates at the round window.
Semi-circular Canals
There are three semi-circular canals: anterior,
lateral and posterior.
They contain the semi-circular ducts, which are
responsible for balance (along with the utricle and
saccule).
Membranous Labyrinth
A continuous system of ducts filled
with endolymph.
Lies within the bony labyrinth, surrounded by
perilymph.
It is composed of the cochlear duct, three semi-
circular ducts, saccule and the utricle.
The cochlear duct is situated within the cochlea
and is the organ of hearing.
The semi-circular ducts, saccule and utricle are
the organs of balance (also known as
the vestibular apparatus).
Cochlear Duct
Located within the bony scaffolding of the
cochlea.
It is held in place by the spiral lamina.
The presence of the duct creates two canals above
and below it – the scala vestibuli and scala
tympani respectively.
The cochlear duct is triangular in shape:
Lateral wall – Formed by thickened periosteum,
known as the spiral ligament.
Roof – Formed by a membrane which separates
the cochlear duct from the scala vestibuli, known as
the Reissner’s membrane.
Floor – Formed by a membrane which separates
the cochlear duct from the scala tympani, known as
the basilar membrane.
The basilar membrane houses the epithelial
cells of hearing – the Organ of Corti.
Saccule and Utricle
Two membranous sacs located in the vestibule.
They are organs of balance which detect
movement of the head in the vertical and
horizontal planes, respectively.
The utricle -larger of the two, receives the three
semi-circular ducts.
The saccule is globular in shape and receives the
cochlear duct.
Endolymph drains from the saccule and utricle
into the endolymphatic duct.
The duct travels through the vestibular
aqueduct to the posterior aspect of the petrous
part of the temporal bone.
Here, the duct expands to a sac where endolymph
can be secreted and absorbed.
Semi-circular Ducts
The semi-circular ducts are located within the
semi-circular canals, and share their orientation.
On movement of the head, the flow
of endolymph within the ducts changes speed
and/or direction.
Sensory receptors in the ampullae of the semi-
circular canals detect this change, and send signals
to the brain, allowing for the processing of balance.
The components of the membranous
labyrinth.
VASCULATURE
The bony labyrinth receives its blood supply from
three arteries, which also supply the surrounding
temporal bone:
Anterior tympanic branch (from maxillary
artery).
Petrosal branch (from middle meningeal artery).
Stylomastoid branch (from posterior auricular
artery).
The membranous labyrinth is supplied by
the labyrinthine artery, a branch of the inferior
cerebellar artery (or, occasionally, the basilar
artery).
It divides into three branches:
Cochlear branch – supplies the cochlear duct.
Vestibular branches (x2) – supply the vestibular
apparatus.
Venous drainage of the inner ear is through
the labyrinthine vein, which empties into the
sigmoid sinus or inferior petrosal sinus.
BRANCHES OF INTERNAL CAROTID
Innervation
The inner ear is innervated by
the vestibulocochlear nerve (CN VIII)
It enters the inner ear via the internal acoustic
meatus, where it divides into the vestibular
nerve (responsible for balance) and the cochlear
nerve (responsible for hearing):
The facial nerveCN VII, passes through the inner
ear, but does not innervate any of the structures
present.
Clinical Relevance: Meniere’s Disease
Meniere’s disease is a disorder of the inner ear,
characterised by episodes of vertigo, low-pitched
tinnitus, and hearing loss.
The symptoms are thought to be caused by an
excess accumulation of endolymph within the
membranous labyrinth, causing progressive
distension of the ducts.
The resulting pressure fluctuations damage the
thin membranes of the ear that detect balance and
sound.
The eyeball
Lies in the bony orbit
It is divided into three parts –
fibrous, vascular and inner layers.
Layers of the Eyeball
Fibrous
Outermost layer consisting of sclera and cornea,
which are continuous with each other.
They provide shape to the eye and support the
deeper structures.
The sclera comprises the majority of the fibrous
layer (approximately 85%).
It provides attachment to the extraocular
muscles these muscles are responsible for the
movement of the eye.
It is visible as the white part of the eye.
The cornea is transparent and Light entering the
eye is refracted by the cornea.
The cornea and sclera of the eye.
Vascular
Lies underneath the fibrous layer.
It consists of the choroid, ciliary body and iris:
Choroid – layer of connective tissue and blood
vessels that provides nourishment to the outer layers
of the retina.
Ciliary body – comprised of two parts – the ciliary
smooth muscles that are attached to the lens of the
eye by the ciliary processes.
The ciliary body controls the shape of the lens, and
contributes to the formation of aqueous humor
Iris – circular structure, with an aperture in the
centre (the pupil).
The diameter of the pupil is altered by smooth
muscle fibres within the iris, which are innervated
by the autonomic nervous system.
It is situated between the lens and the cornea.
The vascular layer of the eye.
Inner
Formed by the retina; its light detecting
component.
The retina is composed of two layers:
Pigmented (outer) layer – formed by a single
layer of cells.
It is attached to the choroid and supports the
choroid in absorbing light (preventing scattering of
light within the eyeball).
It continues around the whole inner surface of the
eye.
Neural (inner) layer – consists of
photoreceptors, the light detecting cells of the
retina located posteriorly and laterally in the eye.
Anteriorly, the pigmented layer continues but the
neural layer does not – this is part is known as
the non-visual retina.
Posteriorly and laterally, both layers of the retina
are present.
This is the optic part of the retina that can be
viewed during ophthalmoscopy.
The centre of the retina is marked by an area
known as the macula( yellowish and highly
pigmented).
The macula contains a depression called the fovea
centralis, which has a high concentration of light
detecting cells.
It is the area responsible for high acuity vision.
The area that the optic nerve enters the retina is
known as the optic disc and has no light detecting
cells.
Structures of the Eyeball
Vitreous Body
A transparent gel which fills the posterior segment
of the eyeball (the area posterior to the lens).
It is marked by a narrow fetal remnant canal
which runs from the optic disc to the lens –
the hyaloid canal.
The vitreous body has three main functions:
Magnifying power of the eye
Supports the lens
Holds the layers of the retina in place
Lens
Its between the vitreous humor and the pupil.
The shape of the lens is altered by the ciliary
body, altering its refractive power.
In old age, the lens can become opaque – a
condition known as a cataract.
Anterior and Posterior Chambers
There are two fluid filled areas in the eye – known
as the anterior(between cornea and
iris) and posterior chambers (between iris and
ciliary processes).
The chambers are filled with aqueous humor – a
clear plasma-like fluid that nourishes and protects
the eye.
The Humor is produced constantly, and drains via
the trabecular meshwork, an area of tissue at the
base of the cornea, near the anterior chamber.
If the drainage of aqueous humor is obstructed, a
condition known as glaucoma can result.
Anterior and posterior chambers of the
eye.
Vasculature
The eyeball receives arterial blood via
the ophthalmic artery that gives rise to the
central artery of the retina supplying the internal
surface of the retina.
Occlusion of this artery will quickly result in
blindness.
Venous drainage of the eyeball is
by superior and inferior ophthalmic veins.
These drain into the cavernous sinus.
Clinical Relevance: Glaucoma
These are eye diseases that damage the optic nerve.
Open angle glaucoma –Due to diminished
drainage
Causes a gradual reduction of the peripheral vision,
Closed angle glaucoma –The iris is forced against
the trabecular meshwork, preventing any drainage of
aqueous humor.
It is an ophthalmic emergency, which can rapidly
lead to blindness.
Clinical Relevance: Papilloedema
Swelling of the optic disc secondary to
raised intracranial pressure.
The optic disc is the area of the retina where the
optic nerve enters and can be visualised using an
ophthalmoscope.
The high pressure within the cranium resists venous
return from the eye.
This causes fluid to extravasate from blood vessels
and collect in the retina, producing a swollen optic
disc.
The fundus (interior surface) of the eye.
The eyelids
Thin, mobile folds that cover the eyeball
anteriorly.
They offer protection and distributing tears over
the surface of the eyeball.
The upper and lower portions meet at the medial
and lateral canthi of the eye.
The opening between the two eyelids is called
the palpebral aperture or opening.
The upper and lower eyelid.
Layers of the Eyelid
The eyelid consists of five main layers (superficial
to deep):
Skin and subcutaneous tissue
Orbicularis oculi
Tarsal plates
Levator apparatus
Conjunctiva
The levator palpebrae superioris and superior
tarsal muscles both act to open the eyelid.
They are only present in the upper eyelid.
Sagittal section of the orbit with the layers
of the eyelid.
Tarsal Plates
The tarsal plates are deep to the palpebral region
of the orbicularis oculi muscle.
They form the scaffolding of the eyelid
The superior tarsus also acts as the attachment site
of the levator palpebrae superioris.
In the tarsal plates lie the Meibomian
glands (also known as tarsal glands).
The Meibomian glands secretes an oily
substance onto the eye to slow the evaporation of
the eye’s tear film.
The oily substance also prevents the eyelids from
sticking together when closed.
Clinical Relevance: Styes and Chalazion
A stye is an infection of a hair follicle or Meibomian
glands around the eyelash.
If affecting the hair follicles, they are described
as external, and if they affect the Meibomian glands
they are classified as internal.
They are self-limiting, although they can be drained
by removing the hair from the affected follicle.
A chalazion is a painless granuloma of the
Meibomian glands distinguished from a stye by the
absence of pain in a chalazion, whereas styes are
normally painful.
Attachment of the levator palpebrae
superiors to the superior tarsal plate.
Conjunctiva
The palpebral conjunctiva forms the deepest
layer of the eyelid.
It is a thin mucous membrane, which is reflected
onto the sclera of the eyeball (bulbar conjunctiva).
Vasculature
Ophthalmic artery – lacrimal, medial palpebral,
supraorbital, dorsal nasal and supratrochlear
arteries.
Facial artery – angular branch.
Superficial temporal artery – transverse facial
artery branch.
Venous drainage
Medially, blood drains via the medial palpebral
vein into the angular and ophthalmic veins.
Laterally, blood drains into the superficial
temporal vein from the lateral palpebral vein.
Innervation
Ophthalmic nerve (V1) – upper eyelid.
Supraorbital, supratrochlear, infratrochlear and
lacrimal branches.
Maxillary nerve (V2) – lower eyelid.
Infraorbital and zygomaticofacial branches.
The oral cavity,
Major functions:
Digestion – receives food, preparing it for
digestion in the stomach and small intestine.
Communication – modifies the sound produced
in the larynx to create a range of sounds.
Breathing – acts as an air inlet in addition to the
nasal cavity.
Divisions of the Oral Cavity
The oral cavity spans between the oral
fissure and the oropharyngeal isthmus
The two divisions of the oral cavity are the vestibule
and oral cavity proper.
Mouth Proper
The mouth proper lies posteriorly to the vestibule.
It is bordered by a roof, a floor, and the cheeks. The
tongue fills a large proportion of the cavity of the
mouth proper.
Roof
The roof of the mouth proper consists of the hard
and soft palates.
The hard palate separates the nasal cavity from
the oral cavity.
It is covered superiorly by respiratory mucosa
(ciliated pseudostratified columnar epithelium)
and inferiorly by oral mucosa (stratified squamous
epithelium).
The soft palate is a muscular structure.
It acts as a valve that can lower to close the
oropharyngeal isthmus, and elevate to separate the
nasopharynx from the oropharynx.
Cheeks
The cheeks are formed by the buccinator muscle,
which is lined internally by the oral mucous
membrane.
Floor
The floor of the oral cavity consists of several
structures:
Muscular diaphragm – comprised of the
bilateral mylohyoid muscles. It pulls the larynx
forward during swallowing.
Geniohyoid muscles – pull the larynx forward
during swallowing.
Tongue – connected to the floor by the frenulum
of the tongue, a fold of oral mucosa.
Salivary glands and ducts.
Structures of the oral cavity floor.
Innervation
The hard palate is innervated by the greater
palatine and nasopalatine nerves, both of which
are branches of the maxillary nerve (CN V2).
The soft palate is innervated by lesser
palatine nerve, branch of the maxillary nerve.
The floor is innervated by lingual nerve – a
branch of the mandibular (V3)
The tongue is innervated by special fibres for taste
from the chorda tympani, a branch of the facial
nerve (CN VII).
The cheeks are innervated by the buccal nerve a
branch of the mandibular
The lingual nerve provides sensory
innervation to the tongue.
Clinical relevance: The Gag Reflex
The gag reflex is protective against foreign bodies
touching the posterior aspects of the oral cavity,
which are most innervated by
the glossopharyngeal nerve (CN IX).
When stimulated, a reflex arc leads to contraction
of the pharyngeal musculature and the elevation of
the soft palate.
The efferent nerve in this case is the Vagus
nerve(CN X).
The lacrimal glands
Serous and Exocrine and secrete lacrimal fluid
onto the surfaces of the conjunctiva and cornea of
the eye.
Lacrimal fluid clean, nourish and lubricate the
eyes.
It forms tears when produced in excess.
The lacrimal gland is located anteriorly in the
superolateral aspect of the orbit, within the
lacrimal fossa – a depression in the orbital plate of
the frontal bone.
Its anatomical relations include:
Superior – zygomatic process of frontal bone
Anterior – orbital septum
Posterior – orbital fat
Inferolateral – lateral rectus muscle
The anatomical position of the lacrimal
gland.
The lacrimal gland has two main parts:
Orbital – larger and sits on the lateral margin of
the levator palpabrae superioris muscle.
Palprebral – smaller and is located along the
inner surface of the eyelid.
The lacrimal fluid is secreted into excretory ducts,
which empty into the superior conjunctival
fornix.
The fluid is then ‘spread’ over the cornea by the
process of blinking.
Lacrimal Apparatus
After secretion, lacrimal fluid circulates across the
eye, and accumulates in the lacrimal lake –
located in the medial canthus of the eye.
From here, it drains into the lacrimal sac via a
series of canals.
The lacrimal sac is the dilated end of
the nasolacrimal duct, and is located in a groove
formed by the lacrimal bone and frontal process of
the maxilla.
Lacrimal fluid drains down the nasolacrimal duct
and empties into the inferior meatus of the nasal
cavity.
The lacrimal apparatus of the eye.
Vasculature
The lacrimal artery,
Venous drainage is via the superior ophthalmic
vein, and ultimately empties into the cavernous
sinus.
Lymphatic drainage is to the superficial parotid
lymph nodes.
They empty into the superior deep cervical nodes.
Innervation
The sensory innervation to the lacrimal gland is
via the lacrimal nerve(ophthalmic nerve)
The lacrimal gland also receives autonomic nerve
fibres:
Parasympathetic:
Preganglionic fibres are carried in the greater
petrosal nerve (branch of the facial nerve) and
then the nerve of pterygoid canal, before
synapsing at the pterygopalatine ganglion.
Postganglionic fibres travel with the maxillary
nerve, and finally the zygomatic nerve.
Stimulates fluid secretion from the lacrimal
gland
Sympathetic
Fibres originate from the superior cervical
ganglion, and are carried by the internal carotid
plexus and deep petrosal nerve.
They join with the parasympathetic fibres in the
nerve of pterygoid canal, and follow the same
route to supply the gland.
Inhibits fluid secretion from the lacrimal gland
Clinical Relevance: Dacryoadenitis
Inflammation of the lacrimal glands.
Acute dacryoadenitis –Due to viral and bacterial
infection such as mumps, Epstein-Barr virus,
staphylococcus and gonococcus.
Chronic dacryoadenitis – Due to a non-
infectious inflammatory condition such as thyroid
eye disease associated with Grave’s disease.
Clinical features include swelling, pain
and excess tear production.
The swelling can lead to visual impairment,
secondary to pressure on the eye.
Treat the underlying cause.
SALIVARY GLANDS
The parotid gland
A bilateral salivary gland located in the face.
It produces serous saliva, a watery solution rich
in enzymes.
It is divided into deep and superficial lobes,
which are separated by the facial nerve.
The parotid region is bounded as follows:
Superiorly – Zygomatic arch.
Inferiorly – Inferior border of the mandible.
Anteriorly – Masseter muscle.
Posteriorly – External ear and
sternocleidomastoid.
The secretions of the parotid gland are
transported to the oral cavity by the Stensen duct.
It pierces the buccinator, moving medially.
It opens out into the oral cavity near the second
upper molar.
Position of the parotid gland and borders
of the parotid region.
Important neurovascular structures pass
through the gland:
The facial nerve
It gives rise to five terminal branches within the
parotid gland.
These branches innervate the muscles of facial
expression.
The external carotid artery
It ascends through the parotid gland.
Within the gland, it gives rise to the posterior
auricular artery.
The ECA then divides into its two terminal
branches – the maxillary artery and superficial
temporal artery.
The retromandibular vein is formed within the
parotid gland by the convergence of the
superficial temporal and maxillary veins.
The branches of the facial nerve . The parotid gland has
been removed to show their anatomical course.
Vasculature
Blood is supplied by the posterior
auricular and superficial temporal arteries.
Venous drainage is via the retromandibular
vein. Innervation
Receives sensory and autonomic innervation.
The autonomic innervation controls the rate of
saliva production.
Sensory innervation is via auriculotemporal
nerve (gland) and the great auricular
nerve (fascia).
Path of the parasympathetic fibres to the
parotid gland.
Clinical Relevance: Disorders of the Parotid
Gland
Parotid Gland Tumours
Usually benign, such as an adenolymphoma.
Tumours of the submandibular and sublingual
glands are less common, but more likely to
be malignant.
Treatment usually involves surgical excision of the
tumour and parotid gland, known as
a parotidectomy.
Parotitis
Parotitis refers to inflammation of the parotid
gland, usually as a result of an infection.
The parotid gland is enclosed in a tough fibrous
capsule.
This limits swelling of the gland, producing pain.
The pain produced can be referred to the external
ear.
This is because the auriculotemporal
nerve provides sensory innervation to the parotid
gland and the external ear.
The sublingual glands
Smallest of the three paired salivary glands and
the most deeply situated.
Produces mixed secretions which are mucous
They are found below the tongue, bordered
laterally by the mandible and medially by
genioglossus muscle of the tongue.
The submandibular duct and lingual
nerve pass alongside the medial aspect of the
sublingual gland.
The sublingual gland, viewed from the
right side
Vasculature
Via the sublingual and submental
arteries which arise from the lingual and facial
arteries respectively
Venous drainage- sublingual and submental
veins which drain into the lingual and facial veins
respectively; both then draining into the internal
jugular vein.
Innervation
Autonomic innervation is via parasympathetic
and sympathetic fibres, which directly and
indirectly regulate salivary secretions respectively.
Innervation to the sublingual gland, via
the submandibular ganglion.
Clinical Relevance: Ranula
A ranula is a type of mucocele (mucous cyst) that
occurs in the floor of the mouth inferior to the
tongue.
The most common disorder linked with the
sublingual glands due to their
higher mucin content in secretions compared to
other salivary glands.
Ranulas can be caused by trauma to the delicate
sublingual gland ducts causing them to rupture,
with mucin then collecting within the connective
tissues to form a cyst.
Cervical Ranulas rarely exist
A right sided ranula.
The submandibular glands
Bilateral salivary glands located in the face with
mixed serous and mucous salivary secretions
The submandibular gland is located in anterior
part of the submandibular triangle.
The boundaries of this triangle are:
Superiorly: Inferior body of the mandible.
Anteriorly: Anterior belly of the digastric muscle.
Posteriorly: Posterior belly of the digastric
muscle.
Secretions from the submandibular glands travel
into the oral cavity via the submandibular
duct (Wharton’s duct).
It emerges anteromedially from the deep arm of
the gland between the mylohyoid, hypoglossus and
genioglossus muscles.
The duct ascends on its course to open as 1-3
orifices on a small sublingual papilla (caruncle)
at the base of the lingual frenulum bilaterally.
The sublingual folds and papillae.
The submandibular triangle of the neck.
The superficial arm of the submandibular
gland.
Relationship with Nerves
lingual nerve, hypoglossal nerve and facial
nerve (marginal mandibular branch).
Lingual nerve: Beginning lateral to the
submandibular duct to provide general somatic
afferent innervation to the mucus membrane of the
anterior two-thirds of the tongue.
Hypoglossal nerve: Lies deep to the
submandibular gland and runs superficial to
hyoglossus and deep to digastric muscle.
Facial nerve (marginal mandibular
branch): Exits the anterior-inferior portion of the
parotid gland at the angle of the jaw
Clinical Relevance: Submandibular Gland
Excision
Submandibular gland excision is a common
surgical procedure indicated for conditions such as
submandibular gland neoplasia or recurrent
calculi.
The anatomical course of the hypoglossal
nerve.
Vasculature
The submental artery (branch of facial artery)
and sublingual artery (branch of lingual artery).
Its venous drainage is by two vessels:
Facial vein – empties directly into the internal
jugular vein.
Sublingual vein – drains into the lingual vein and
then internal jugular vein.
Innervation
The submandibular glands receive autonomic
innervation through parasympathetic and
sympathetic fibres,
Clinical Relevance: Salivary Duct Calculi
A calculus or sialolith is a calcified deposit which
can block the lumen of a duct.
The submandibular duct is the most susceptible to
calculi out of all the salivary ducts; accounting for
approximately 80% of cases.
This is thought to be due to torturous length of
the duct
Ascending secretory pathway
Nature of salivary secretion
The submandibular glands and the patency of the
ducts can be examined by direct injection of a
contrast medium.
This is known as a sialogram, which is a special
type of radiograph.
A calculus may present radiographically as a
stricture or complete occlusion of the duct.
You might also like
- Vent Modes ChartDocument1 pageVent Modes Chartladyhavocinc100% (1)
- Spice Rack Real Time Analysis of Speaker: Name NameDocument9 pagesSpice Rack Real Time Analysis of Speaker: Name NameFortuna Power TECHNOLOGYNo ratings yet
- Anatomy and Physiology of The Ear PDFDocument12 pagesAnatomy and Physiology of The Ear PDFDeshini Balasubramaniam83% (6)
- Anatomy and Physiology of The NoseDocument6 pagesAnatomy and Physiology of The NoseManveer DhaliwalNo ratings yet
- Anatomy of The External EarDocument28 pagesAnatomy of The External Earhama100% (1)
- Colon Cancer Pathophysiology PDFDocument2 pagesColon Cancer Pathophysiology PDFMaggieNo ratings yet
- Middle Ear - Earth's LabDocument1 pageMiddle Ear - Earth's Labmfk5p77t8mNo ratings yet
- By DR Manah Chandra Changmai MBBS MSDocument31 pagesBy DR Manah Chandra Changmai MBBS MSKalaivaany RamachandranNo ratings yet
- Ear Anatomy and PhysiologyDocument50 pagesEar Anatomy and Physiologyxj74fr4ddxNo ratings yet
- Parasinus AnatomyDocument6 pagesParasinus Anatomyalexandra663No ratings yet
- 1 RHINOLOGY NoseDocument116 pages1 RHINOLOGY NoseWai Kwong ChiuNo ratings yet
- Prof. DR - Mohamed Talaat ElghonemyDocument49 pagesProf. DR - Mohamed Talaat Elghonemyadel madanyNo ratings yet
- The EarDocument13 pagesThe EarOjambo FlaviaNo ratings yet
- Case Report CSOMDocument13 pagesCase Report CSOMNashria RusdhyNo ratings yet
- ورق مذاكره PDFDocument100 pagesورق مذاكره PDFsalamred100% (1)
- Anatomy of EarDocument17 pagesAnatomy of Earkresha solankiNo ratings yet
- Nasal AnatomyDocument23 pagesNasal AnatomyArchanaShenoyNo ratings yet
- Potongan CSOM Part 2Document12 pagesPotongan CSOM Part 2Athanasius WrinNo ratings yet
- Anatomy and Physiology of The Nose and Paranasal SinusesDocument2 pagesAnatomy and Physiology of The Nose and Paranasal SinusesNuardi YusufNo ratings yet
- Anatomy NoseDocument35 pagesAnatomy Noseضبيان فرحانNo ratings yet
- Anatomy Lec.1 Nasal Cavities and Paranasal SinusesDocument21 pagesAnatomy Lec.1 Nasal Cavities and Paranasal Sinusesزينب فؤاد موسىNo ratings yet
- PBL - THT HidungDocument35 pagesPBL - THT Hidungdian novitasariNo ratings yet
- NOSEDocument6 pagesNOSEAjigotto ubiq.No ratings yet
- Anatomy and Physiology of Ent-OrgansDocument52 pagesAnatomy and Physiology of Ent-OrgansdrghassanNo ratings yet
- Nose Dr. A. S. D' SouzaDocument18 pagesNose Dr. A. S. D' SouzaNariska CooperNo ratings yet
- Anatomy EarDocument20 pagesAnatomy EarRod HilalNo ratings yet
- Exterior and Middle EarDocument26 pagesExterior and Middle EarAndra BauerNo ratings yet
- Anatomy of External Ear, Middle Ear and MastoidDocument66 pagesAnatomy of External Ear, Middle Ear and Mastoiddebdeepbhattacharya411No ratings yet
- Otitis Media AkutDocument24 pagesOtitis Media AkutBethari K AbiantiNo ratings yet
- The Ear: Head & Neck Unit - مسعسلا ليلج رديح .دDocument20 pagesThe Ear: Head & Neck Unit - مسعسلا ليلج رديح .دStevanovic StojaNo ratings yet
- Lectures, WordDocument27 pagesLectures, Word9xymc5pcyzNo ratings yet
- 28 Temporal Bone (Done)Document7 pages28 Temporal Bone (Done)Ayah HyasatNo ratings yet
- Part 2 The Nose, Paranasal Sinuses and PharnyxDocument12 pagesPart 2 The Nose, Paranasal Sinuses and PharnyxLauraDernNo ratings yet
- AnatomyDocument15 pagesAnatomyAdeleye John AdebolaNo ratings yet
- 15-Sensory OrgansDocument23 pages15-Sensory OrgansMilad HabibiNo ratings yet
- Anatomy of The Nose and Paranasal SinusDocument5 pagesAnatomy of The Nose and Paranasal Sinusbayoe_pra100% (1)
- Demo Class of EarDocument54 pagesDemo Class of EarMegha BhengraNo ratings yet
- Good Afternoon EverybodyDocument131 pagesGood Afternoon EverybodyIhsan HanifNo ratings yet
- 12 - Anatomy of The NoseDocument32 pages12 - Anatomy of The Nosehanizulfani13No ratings yet
- Chronic Suppurative Otitis MediaDocument16 pagesChronic Suppurative Otitis MediaAndrei Rizqan AkmalNo ratings yet
- Anatomy of External EarDocument49 pagesAnatomy of External EarInderdeep AroraNo ratings yet
- Anatomy EarDocument44 pagesAnatomy Earrinaldy agungNo ratings yet
- EarDocument6 pagesEarDr.Mahesh kumar GuptaNo ratings yet
- Anatomy EarDocument44 pagesAnatomy Earrinaldy agungNo ratings yet
- Anatomy and Physiology THT - Dr. AriefDocument88 pagesAnatomy and Physiology THT - Dr. AriefGilbert Sterling OctaviusNo ratings yet
- Upper Respiratory Tract AnatomyDocument61 pagesUpper Respiratory Tract Anatomyيحيى اسماعيل الجميليNo ratings yet
- Presentation On Nasal ObstructionDocument111 pagesPresentation On Nasal Obstructionbatookhan100% (2)
- Anatomy, Physiology of ENT For Paramedics - Dr. Fuad RidhaDocument52 pagesAnatomy, Physiology of ENT For Paramedics - Dr. Fuad Ridhafuadredza100% (1)
- Eternal and Middle Ear AarogyaDocument66 pagesEternal and Middle Ear AarogyaAarooNo ratings yet
- The Vestibulocochlear Organ: China Medical UniversityDocument30 pagesThe Vestibulocochlear Organ: China Medical UniversityDONALD UNASHENo ratings yet
- Anatomy Physiology of The EarDocument8 pagesAnatomy Physiology of The EargheaastridgayatriNo ratings yet
- Middle EarDocument16 pagesMiddle EarproshishNo ratings yet
- 01.anatomy of The EarDocument52 pages01.anatomy of The EarJumanne Jay100% (2)
- Paranasal Sinus Anatomy - Overview, Gross Anatomy, Microscopic AnatomyDocument12 pagesParanasal Sinus Anatomy - Overview, Gross Anatomy, Microscopic AnatomyKienlevy100% (1)
- Special Senses 1 NDocument179 pagesSpecial Senses 1 Naoujahmed123456789010No ratings yet
- W2-7 Ear and Nose LectureDocument52 pagesW2-7 Ear and Nose LectureSAHIL AGARWALNo ratings yet
- G5 Nasal CavityDocument41 pagesG5 Nasal CavityGuo YageNo ratings yet
- B 22-Rs-Anatomy - Saq AnswersDocument22 pagesB 22-Rs-Anatomy - Saq Answersapi-516879364No ratings yet
- External EarDocument3 pagesExternal EarbarbacumlaudeNo ratings yet
- A Simple Guide to the Ear and Its Disorders, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to the Ear and Its Disorders, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Encyclopaedia Britannica, 11th Edition, Volume 13, Slice 2 "Hearing" to "Helmond"From EverandEncyclopaedia Britannica, 11th Edition, Volume 13, Slice 2 "Hearing" to "Helmond"No ratings yet
- Encyclopaedia Britannica, 11th Edition, Volume 13, Slice 2 "Hearing" to "Helmond"From EverandEncyclopaedia Britannica, 11th Edition, Volume 13, Slice 2 "Hearing" to "Helmond"No ratings yet
- 4 - Protein SynthesisDocument66 pages4 - Protein Synthesisraphaelyohana140No ratings yet
- Muscles of Facial ExpressionDocument63 pagesMuscles of Facial Expressionraphaelyohana140No ratings yet
- 6 - NM2 Action PotentialDocument48 pages6 - NM2 Action Potentialraphaelyohana140No ratings yet
- Head AnatomyDocument66 pagesHead Anatomyraphaelyohana140No ratings yet
- H.anatomy IntroductionDocument60 pagesH.anatomy Introductionraphaelyohana140No ratings yet
- 16) Signaling Pathways That Control Gene ActivityDocument27 pages16) Signaling Pathways That Control Gene ActivityRNo ratings yet
- (Reviews in Mineralogy and Geochemistry'', 54) Patricia M. Dove, James J. de Yoreo, Steve Weiner-Biomineralization-Mineralogical Society of America (2003)Document377 pages(Reviews in Mineralogy and Geochemistry'', 54) Patricia M. Dove, James J. de Yoreo, Steve Weiner-Biomineralization-Mineralogical Society of America (2003)Karlii BasilioNo ratings yet
- L A Level Biology MS Jan 05Document180 pagesL A Level Biology MS Jan 05annakaranovaNo ratings yet
- Op Art and Visual PerceptionDocument26 pagesOp Art and Visual PerceptionFelipeCussenNo ratings yet
- Cklistskill 43 Oxygen AdministrationDocument3 pagesCklistskill 43 Oxygen AdministrationGalenn BarrionNo ratings yet
- Interactive National Vital Sign Chart July 2017Document2 pagesInteractive National Vital Sign Chart July 2017basheNo ratings yet
- Life ProcessesDocument12 pagesLife ProcessesJeevansh WadhwaNo ratings yet
- Niraamaya Spa MenuDocument35 pagesNiraamaya Spa MenuSanjeev HariharanNo ratings yet
- Sports Exercise and Health Science Paper 2 SL MarkschemeDocument21 pagesSports Exercise and Health Science Paper 2 SL Markschemegoingnow0001No ratings yet
- Maxillary Air Sinus Oral SurgeryDocument49 pagesMaxillary Air Sinus Oral SurgeryDentist Dina SamyNo ratings yet
- Foods That Cause Acne: SUNDAY, APRIL 8, 2012Document3 pagesFoods That Cause Acne: SUNDAY, APRIL 8, 2012FitriAndriyaniNo ratings yet
- Night Shifts Can Also Be TiringDocument2 pagesNight Shifts Can Also Be TiringMariccon Celestial PalmaNo ratings yet
- Amino Acids and Proteins ReviewerDocument11 pagesAmino Acids and Proteins ReviewerJohn-Karl JimenezNo ratings yet
- Saliva and Its Importance in Complete Denture ProsthodonticsDocument8 pagesSaliva and Its Importance in Complete Denture ProsthodonticsKrupali JainNo ratings yet
- SSGBIO1 - CM Week 1Document16 pagesSSGBIO1 - CM Week 1sgdick31No ratings yet
- Semester 2 Biochem TimetableDocument1 pageSemester 2 Biochem TimetablesophiecabNo ratings yet
- 11 - Head & Neck (Blood Vessels) (FF) - Part 1Document20 pages11 - Head & Neck (Blood Vessels) (FF) - Part 1checkmate100% (1)
- Kidney Problems and DialysisDocument3 pagesKidney Problems and DialysismarymakinNo ratings yet
- Review On Animal and Plant CellDocument3 pagesReview On Animal and Plant CellLadymae GalolaNo ratings yet
- HUBS1105 Bones and Joints of The Skull and FaceDocument5 pagesHUBS1105 Bones and Joints of The Skull and FaceChloe HeuchanNo ratings yet
- Pathophysiology Exam 4 - ReviewDocument18 pagesPathophysiology Exam 4 - ReviewWaqas GillNo ratings yet
- Staar g3 2016test Read FDocument33 pagesStaar g3 2016test Read FsatishNo ratings yet
- Special ArticlesDocument12 pagesSpecial ArticlesMichael Vincent MercadoNo ratings yet
- Life Processes Case Based QuestionsDocument21 pagesLife Processes Case Based Questionsvaibhav08112008No ratings yet
- Resume - Natalia MathesonDocument2 pagesResume - Natalia Mathesonapi-449546352No ratings yet
- A Whole Bouquet For YouDocument334 pagesA Whole Bouquet For YoujdgjhsbjhbsNo ratings yet
- Degradation of Cytokinins by Cytokinin Oxidases in PlantsDocument13 pagesDegradation of Cytokinins by Cytokinin Oxidases in PlantsRoikka HazarikaNo ratings yet