Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
6 viewsAneurysm HTN
Aneurysm HTN
Uploaded by
Reetu BaralAn aneurysm is an abnormal dilation of a blood vessel wall caused by weaknesses in the vessel from congenital defects, disease, trauma or atherosclerosis. Specific types of aneurysms include berry aneurysms of the brain which occur at arterial bifurcations and can rupture, and dissecting aneurysms associated with hypertension which involve blood entering the vessel wall. Complications of aneurysms include rupture, obstruction, embolism, and compression of surrounding structures. Hypertension is high blood pressure that can damage vessels and organs if untreated. It is classified as essential or secondary to conditions like chronic kidney disease or adrenal disorders. Untreated severe hypertension can lead to complications such as heart failure, stroke, and renal failure.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You might also like
- Pathophysiology of StrokeDocument3 pagesPathophysiology of StrokeAqeel Al-Mahdaly0% (1)
- Ischemic Heart Disease (IHD)Document55 pagesIschemic Heart Disease (IHD)rameshbmc100% (6)
- Cardiovascular System Pathology, MBCHBDocument18 pagesCardiovascular System Pathology, MBCHBSecret AgentNo ratings yet
- Disturbances in The Blood Flow1Document41 pagesDisturbances in The Blood Flow1ammar amerNo ratings yet
- Chapter 12 - The HeartDocument6 pagesChapter 12 - The HeartAgnieszka WisniewskaNo ratings yet
- Cardio-Vascular Disease: HypertensionDocument74 pagesCardio-Vascular Disease: HypertensionLijoNo ratings yet
- Clinical Medicine Hypertension: DR - Muhammad Nauman Senior Lecturer (DOVS) University of The LahoreDocument74 pagesClinical Medicine Hypertension: DR - Muhammad Nauman Senior Lecturer (DOVS) University of The LahoreNoman MunirNo ratings yet
- Oedema, Hemorrhages and ThrombosisDocument72 pagesOedema, Hemorrhages and ThrombosisTheBoss 20No ratings yet
- Hypertension: Alemwosen T. (MD, Asst Prof in Pathology)Document46 pagesHypertension: Alemwosen T. (MD, Asst Prof in Pathology)Amanuel MaruNo ratings yet
- HTN and CHFDocument29 pagesHTN and CHFkiflomNo ratings yet
- Elevated Arterial Pressure Is Called HypertensionDocument27 pagesElevated Arterial Pressure Is Called Hypertensionsaurabhv89No ratings yet
- Chemical Pathology of HypertensionDocument37 pagesChemical Pathology of Hypertensionp6hccq6jd7No ratings yet
- Hypertension PathoDocument13 pagesHypertension Pathowajehak40No ratings yet
- SEMINARDocument31 pagesSEMINARDeveshNo ratings yet
- Ipertensione Arteriosa PolmonareDocument33 pagesIpertensione Arteriosa PolmonareCarlo MaxiaNo ratings yet
- Pathology of The Cardiovascular System-2Document24 pagesPathology of The Cardiovascular System-2AZALEA SANIANONo ratings yet
- OEDEMADocument72 pagesOEDEMAAhmed NourNo ratings yet
- Pathology of Heart Failure and CardiomyopathiesDocument33 pagesPathology of Heart Failure and Cardiomyopathiesciyace7849No ratings yet
- باثو 2Document35 pagesباثو 2shahadkhaled171No ratings yet
- Peripheral-Vascular-Disease 2ndDocument84 pagesPeripheral-Vascular-Disease 2ndAb BabyNo ratings yet
- Cardiovascular PathologyDocument182 pagesCardiovascular PathologyPavan chowdaryNo ratings yet
- Diagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaDocument49 pagesDiagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaSiti rahmawatiNo ratings yet
- 1 Heart FailureDocument49 pages1 Heart FailureDammaqsaa W BiyyanaaNo ratings yet
- Hypertension For EMS ProvidersDocument35 pagesHypertension For EMS ProvidersPaulhotvw67100% (5)
- ShockDocument19 pagesShockirenekhatete1No ratings yet
- Chapter 5 HTDocument56 pagesChapter 5 HTtesfamichael mengistu100% (2)
- Reduced Renal Sodium Excretion: Forced Through A Narrow LumenDocument5 pagesReduced Renal Sodium Excretion: Forced Through A Narrow LumenFlowerNo ratings yet
- ENDOCRINE HYPERTENSION. A Number of Hormonal Secretions May Produce Secondary HyDocument5 pagesENDOCRINE HYPERTENSION. A Number of Hormonal Secretions May Produce Secondary HyIsak ShatikaNo ratings yet
- RENAL VASCULAR DISEASES UpdatedDocument97 pagesRENAL VASCULAR DISEASES UpdatedgibreilNo ratings yet
- 1.congestive Heart FailureDocument8 pages1.congestive Heart FailureJarda julie DacuagNo ratings yet
- Heart Failure and Pulmonary EdemaDocument60 pagesHeart Failure and Pulmonary EdemaYosra —No ratings yet
- SHOCK DiscussionDocument22 pagesSHOCK DiscussionNavpreet Kaur100% (1)
- Antihypertensives Part 1Document15 pagesAntihypertensives Part 1alizwaxabanisa8No ratings yet
- Diseases of Blood Vessels Dr. Fe A. Bartolome, Maed, FpasmapDocument15 pagesDiseases of Blood Vessels Dr. Fe A. Bartolome, Maed, FpasmapJayesh MahajanNo ratings yet
- Cerebrovascular Accident/Brain Attack: Gideon Gachihi Associate Faculty, MKUDocument52 pagesCerebrovascular Accident/Brain Attack: Gideon Gachihi Associate Faculty, MKUElvisNo ratings yet
- Patofisiologi HipertensiDocument18 pagesPatofisiologi HipertensiZebyyNo ratings yet
- Heart Failure and CardiomyopathiesDocument26 pagesHeart Failure and Cardiomyopathieslionel andreaNo ratings yet
- Cerebrovascular CVADocument19 pagesCerebrovascular CVAmmkavitha98No ratings yet
- 5 - Pathology of CADDocument58 pages5 - Pathology of CADregeti bhargavNo ratings yet
- Infective Endocarditis: Akriti DahalDocument79 pagesInfective Endocarditis: Akriti DahalAkriti100% (1)
- Neoplasm: - TermsDocument125 pagesNeoplasm: - Termsferina steffiNo ratings yet
- Cerebrovascular Disease and Coronary Artery Disease: DR Masona-MutitiDocument28 pagesCerebrovascular Disease and Coronary Artery Disease: DR Masona-MutitiShaun MazorodzeNo ratings yet
- 5th Chapter DDDocument36 pages5th Chapter DDRameen RizviNo ratings yet
- HF & ShockDocument18 pagesHF & ShockSahar YousifNo ratings yet
- Congestive Heart Failure LathaDocument68 pagesCongestive Heart Failure LathaLatha GhanesanNo ratings yet
- 1-3 Haemodinamicpart1 PDFDocument64 pages1-3 Haemodinamicpart1 PDFSetiawan SukmadjaNo ratings yet
- Hypertensive Encephalopathy: By:hasmawaty BasirDocument78 pagesHypertensive Encephalopathy: By:hasmawaty BasirLexyArungTikuNo ratings yet
- Hypertension: Nucleus Medical MediaDocument17 pagesHypertension: Nucleus Medical Mediakrish oswalNo ratings yet
- Hypertension: MedicineDocument6 pagesHypertension: Medicineapi-3829364No ratings yet
- Hemodynamic Disorders: By: Dr. SL RasonableDocument59 pagesHemodynamic Disorders: By: Dr. SL RasonableJenneth Marquez JoloNo ratings yet
- Hypertensive Emergencies: Sulaiman Usaid G. MBCHB V Facilatator: DR Jack TDocument44 pagesHypertensive Emergencies: Sulaiman Usaid G. MBCHB V Facilatator: DR Jack TUsaid SulaimanNo ratings yet
- Diagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaDocument51 pagesDiagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaHilmaNo ratings yet
- Tatalaksana Hipertensi KrisisDocument39 pagesTatalaksana Hipertensi KrisisImron RosyadiNo ratings yet
- Cardiomyopathy: Restrictive Heart DiseaseDocument18 pagesCardiomyopathy: Restrictive Heart DiseaseMitch GabuyaNo ratings yet
- Acute Vascular Insufficiency (OSN)Document18 pagesAcute Vascular Insufficiency (OSN)Zeyad HassanNo ratings yet
- Antianginal DrugsDocument92 pagesAntianginal DrugsSarthak DubeyNo ratings yet
- Shock: DR Ahmed MohDocument60 pagesShock: DR Ahmed MohSalman KhanNo ratings yet
- Inflammatory and Valvular DisordersDocument43 pagesInflammatory and Valvular DisordersRifqi Hary ZulfikarNo ratings yet
- 11.sudden Natural Death 3Document55 pages11.sudden Natural Death 3Hasabo AwadNo ratings yet
- Secondary Hypertension: S Ystolic-Diastolic Arterial HypetrtensionDocument9 pagesSecondary Hypertension: S Ystolic-Diastolic Arterial HypetrtensionvifawuduNo ratings yet
- The ASCOD Phenotyping of Ischemic Stroke (Updated ASCO Phenotyping)Document5 pagesThe ASCOD Phenotyping of Ischemic Stroke (Updated ASCO Phenotyping)Jose Algomas KnorecuerdoNo ratings yet
- Types of Stroke: Stroke - CVA Cerebral Vascular Accident Ischemic Cerebrovascular DiseaseDocument7 pagesTypes of Stroke: Stroke - CVA Cerebral Vascular Accident Ischemic Cerebrovascular DiseaseMarrylane GamisNo ratings yet
- Acute Coronary Syndrome: An Essential & Practical ApproachDocument35 pagesAcute Coronary Syndrome: An Essential & Practical ApproachGinawidiyastutiNo ratings yet
- Pathophysiology HypertensionDocument4 pagesPathophysiology HypertensionKimberly BautistaNo ratings yet
- Management of Hypertensive Crisis (Diskusi RSUD)Document20 pagesManagement of Hypertensive Crisis (Diskusi RSUD)Kia AgusputraNo ratings yet
- Aninditha. Buku Ajar Neurologi. Jakarta: Departemen Neurologi Fakultas Kedokteran Universitas Indonesia RS Cipto Mangunkusumo. 2017Document2 pagesAninditha. Buku Ajar Neurologi. Jakarta: Departemen Neurologi Fakultas Kedokteran Universitas Indonesia RS Cipto Mangunkusumo. 2017pelangiNo ratings yet
- Stroke Pathophysiology 1Document5 pagesStroke Pathophysiology 1Jeco ValdezNo ratings yet
- Ait Nejm 2020Document9 pagesAit Nejm 2020Ahmed JallouliNo ratings yet
- Hridroga SampraptiDocument39 pagesHridroga SampraptiGAURAVNo ratings yet
- Yejvs - 7432Document9 pagesYejvs - 7432Francisco Álvarez MarcosNo ratings yet
- Burr Hole Washout Versus Craniotomy For Chronic Subdural Hematoma: Patient Outcome and Cost AnalysisDocument1 pageBurr Hole Washout Versus Craniotomy For Chronic Subdural Hematoma: Patient Outcome and Cost AnalysisCelia WijayaNo ratings yet
- Unit 4b Drugs Affecting CVS, Antianginal DrugsDocument17 pagesUnit 4b Drugs Affecting CVS, Antianginal DrugsالدتادتغدتعدNo ratings yet
- Stroke/Cerebrovascular Accident: Transient Ischemic AttacksDocument5 pagesStroke/Cerebrovascular Accident: Transient Ischemic AttacksCraigNo ratings yet
- ANEURYSMDocument39 pagesANEURYSMIvan Roque100% (1)
- Secondary Stroke PreventionDocument54 pagesSecondary Stroke PreventionHùng Phạm Lý ChíNo ratings yet
- Thromboangiitis ObliteransDocument17 pagesThromboangiitis Obliteransmu_crNo ratings yet
- LeukemiaDocument5 pagesLeukemiaNourie BerawiNo ratings yet
- Critical Limb IschemiaDocument11 pagesCritical Limb IschemiaAmalia Hendar PangestutiNo ratings yet
- 3-5 Slides Primary Prophylaxis For Esophageal Varices in Cirrhosis PDFDocument4 pages3-5 Slides Primary Prophylaxis For Esophageal Varices in Cirrhosis PDFBhavin DalalNo ratings yet
- Journal StrokeDocument5 pagesJournal StrokeRika Sartyca IlhamNo ratings yet
- Antianginal Drugs: Dr. Jim AmisiDocument11 pagesAntianginal Drugs: Dr. Jim AmisiMike AnnisNo ratings yet
- Coronary Heart Disease 3Document47 pagesCoronary Heart Disease 3Silvia RNo ratings yet
- Epidemiological Aspects On Abdominal Aortic Aneurysms (AAA)Document17 pagesEpidemiological Aspects On Abdominal Aortic Aneurysms (AAA)Janey Ceniza تNo ratings yet
- Tia Abcd2 Tool 1Document2 pagesTia Abcd2 Tool 1Siti RahmahNo ratings yet
- Carotid Stenosis (Carotid Artery Disease)Document5 pagesCarotid Stenosis (Carotid Artery Disease)Pieter SteenkampNo ratings yet
- NF100 E76 Blood Supply Brain AnnotatedDocument40 pagesNF100 E76 Blood Supply Brain AnnotatedShashiNo ratings yet
- AneurysmDocument7 pagesAneurysmLillabinNo ratings yet
- Woc AcsDocument5 pagesWoc AcsMuhammad Alvin Fuzail IyazNo ratings yet
- Icha Marissa Sofyan c11108318 UAPDocument24 pagesIcha Marissa Sofyan c11108318 UAPIcha Marissa SofyanNo ratings yet
Aneurysm HTN
Aneurysm HTN
Uploaded by
Reetu Baral0 ratings0% found this document useful (0 votes)
6 views20 pagesAn aneurysm is an abnormal dilation of a blood vessel wall caused by weaknesses in the vessel from congenital defects, disease, trauma or atherosclerosis. Specific types of aneurysms include berry aneurysms of the brain which occur at arterial bifurcations and can rupture, and dissecting aneurysms associated with hypertension which involve blood entering the vessel wall. Complications of aneurysms include rupture, obstruction, embolism, and compression of surrounding structures. Hypertension is high blood pressure that can damage vessels and organs if untreated. It is classified as essential or secondary to conditions like chronic kidney disease or adrenal disorders. Untreated severe hypertension can lead to complications such as heart failure, stroke, and renal failure.
Original Description:
Class for MBBS I
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAn aneurysm is an abnormal dilation of a blood vessel wall caused by weaknesses in the vessel from congenital defects, disease, trauma or atherosclerosis. Specific types of aneurysms include berry aneurysms of the brain which occur at arterial bifurcations and can rupture, and dissecting aneurysms associated with hypertension which involve blood entering the vessel wall. Complications of aneurysms include rupture, obstruction, embolism, and compression of surrounding structures. Hypertension is high blood pressure that can damage vessels and organs if untreated. It is classified as essential or secondary to conditions like chronic kidney disease or adrenal disorders. Untreated severe hypertension can lead to complications such as heart failure, stroke, and renal failure.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
6 views20 pagesAneurysm HTN
Aneurysm HTN
Uploaded by
Reetu BaralAn aneurysm is an abnormal dilation of a blood vessel wall caused by weaknesses in the vessel from congenital defects, disease, trauma or atherosclerosis. Specific types of aneurysms include berry aneurysms of the brain which occur at arterial bifurcations and can rupture, and dissecting aneurysms associated with hypertension which involve blood entering the vessel wall. Complications of aneurysms include rupture, obstruction, embolism, and compression of surrounding structures. Hypertension is high blood pressure that can damage vessels and organs if untreated. It is classified as essential or secondary to conditions like chronic kidney disease or adrenal disorders. Untreated severe hypertension can lead to complications such as heart failure, stroke, and renal failure.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 20
Aneurysm
Hypertension
Prof Dr Reetu Baral MD (Pathology)
Department of Pathology
Nobel Medical College Teaching Hospital
ANEURYSM
An abnormal local dilation or out-pouching of a vessel
wall or cardiac chamber
Caused by weakened vessel wall from:
Congenital defect
Systemic disease
Atherosclerosis
Infection
Trauma
Dr. Reetu Baral
Berry
aneurysm
Involve cerebral arteries at
bifurcations
Probably arise at congenital
points of weakness in wall
Can rupture and result in
subarachnoid hemorrhage
Clinically:
Headache
Stiff neck (meningeal irritation)
Death
Dr. Reetu Baral
Dissecting aneurysm
• Entry of blood into wall & extension
along the length of the vessel
• Form of hematoma, also called dissecting
hematoma
• Associated with:
• Hypertension
• Marfan’s syndrome
Dr. Reetu Baral
Aneurysm: Complications
Rupture
Obstruction
Embolism
Compression
Ureter
Spine
Mass effect
Dr. Reetu Baral
Hypertension
Hypertension
• Hypotension: Low blood pressure results in:
• Inadequate organ perfusion
• Organ dysfunction
• Sometimes tissue death.
• Hypertension: High blood pressure causes:
• Vessel and end-organ damage
• Blood pressure is a function of cardiac output and peripheral
vascular resistance
• Cardiac output is a function of stroke volume and heart rate
(CO=SVxHR)
HYPERTENSIVE VASCULAR DISEASE
• “Essential hypertension”:
• Hypertension: BP>140/90 mmHg
• General population >25% are hypertensive
• Death may be due to (Untreated cases):
• Ischemic heart disease (IHD)
• Congestive heart failure
• Stroke
• Malignant hypertension: 200/120 mmHg
• Associated with Renal failure / Retinal hemorrhage with or without
papilledema
• Death within 1-2 years if untreated
Types and Essential Hypertension
causes of • Accounts for 90-95% cases
hypertension Secondary Hypertension
Renal
• Acute glomerulonephritis
• Chronic renal disease
• Polycystic disease
• Renal artery stenosis
Endocrine
• Adrenocortical hyperfunction (Cushing syndrome)
• Exogenous hormones (glucocorticoids, estrogen)
• Pheochromocytoma
Types and causes Cardiovascular
of hypertension
• Coarctation of the aorta
• Polyarteritis nodosa
Neurologic
• Psychogenic
• Increased ICP
• Sleep apnea
• Acute stress, including surgery
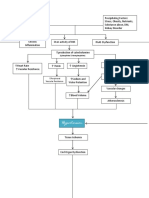
Pathogenesis: HTN
• HTN may be:
• Primary (idiopathic)
• Secondary to an identifiable underlying condition.
• In close to 95% of cases hypertension is idiopathic or “essential”.
• Secondary hypertension are due:
• Primary renal disease
• Renal artery narrowing (reno-vascular hypertension)
• Adrenal disorders
• Essential hypertension is compatible with long life unless:
• Myocardial infarction
• Stroke
• Prognosis of secondary hypertension depends on adequate
treatment of the underlying cause.
• Genetic disorders affecting blood pressure is:
• Gene defects in enzymes involved in aldosterone metabolism
• Mutations in proteins that affect sodium resorption
Pathogenesis: Hypertension
• Reduced renal sodium excretion:
• Decreased sodium excretion causes increase in fluid
volume and increased cardiac output - elevating blood
pressure
• At the new higher blood pressure, the kidneys excrete
additional sodium.
• Thus, a new steady state of sodium excretion is achieved,
but at the expense of an elevated blood pressure.
• Increased vascular resistance due to :
• Increased vascular resistance due to vasoconstriction
because of structural changes in vessel walls
• Genetic factors:
• Familial clustering – as evidenced by monozygotic twins
• Environmental factors can modify the impact of genetic
determinants:
• Stress
• Obesity
• Smoking
• Physical inactivity
• High levels of salt consumption
Morphology
1. HTN accelerates atherogenesis
2. Can lead to aortic dissection
and cerebrovascular
hemorrhage.
Morphology --- Contd.
• Small blood vessel disease related to
hypertension:
1. Hyaline arteriolosclerosis:
• Homogeneous, pink hyaline thickening
of the arteriolar walls
• Loss of underlying structural detail
• Luminal narrowing
• Leakage of plasma components across
injured ECs into vessel - increased ECM
production by SMCs
• In Kidney: Nephrosclerosis
2. Hyperplastic arteriolosclerosis:
• Seen in severe hypertension
• Vessels exhibit “onion skin,”
concentric, laminated thickening of
arteriolar walls and luminal narrowing
• The laminations consist of SMCs and
thickened, reduplicated basement
membrane.
• In malignant hypertension, these
changes are accompanied by fibrinoid
deposits and vessel wall necrosis
(necrotizing arteriolitis) - kidney.
Complications of Hypertension
• Cardiac hypertrophy
• Heart failure
• Aortic dissection
• Multi-infarct dementia
• Renal failure
• The end
• Next Class
• Infective endocarditis
You might also like
- Pathophysiology of StrokeDocument3 pagesPathophysiology of StrokeAqeel Al-Mahdaly0% (1)
- Ischemic Heart Disease (IHD)Document55 pagesIschemic Heart Disease (IHD)rameshbmc100% (6)
- Cardiovascular System Pathology, MBCHBDocument18 pagesCardiovascular System Pathology, MBCHBSecret AgentNo ratings yet
- Disturbances in The Blood Flow1Document41 pagesDisturbances in The Blood Flow1ammar amerNo ratings yet
- Chapter 12 - The HeartDocument6 pagesChapter 12 - The HeartAgnieszka WisniewskaNo ratings yet
- Cardio-Vascular Disease: HypertensionDocument74 pagesCardio-Vascular Disease: HypertensionLijoNo ratings yet
- Clinical Medicine Hypertension: DR - Muhammad Nauman Senior Lecturer (DOVS) University of The LahoreDocument74 pagesClinical Medicine Hypertension: DR - Muhammad Nauman Senior Lecturer (DOVS) University of The LahoreNoman MunirNo ratings yet
- Oedema, Hemorrhages and ThrombosisDocument72 pagesOedema, Hemorrhages and ThrombosisTheBoss 20No ratings yet
- Hypertension: Alemwosen T. (MD, Asst Prof in Pathology)Document46 pagesHypertension: Alemwosen T. (MD, Asst Prof in Pathology)Amanuel MaruNo ratings yet
- HTN and CHFDocument29 pagesHTN and CHFkiflomNo ratings yet
- Elevated Arterial Pressure Is Called HypertensionDocument27 pagesElevated Arterial Pressure Is Called Hypertensionsaurabhv89No ratings yet
- Chemical Pathology of HypertensionDocument37 pagesChemical Pathology of Hypertensionp6hccq6jd7No ratings yet
- Hypertension PathoDocument13 pagesHypertension Pathowajehak40No ratings yet
- SEMINARDocument31 pagesSEMINARDeveshNo ratings yet
- Ipertensione Arteriosa PolmonareDocument33 pagesIpertensione Arteriosa PolmonareCarlo MaxiaNo ratings yet
- Pathology of The Cardiovascular System-2Document24 pagesPathology of The Cardiovascular System-2AZALEA SANIANONo ratings yet
- OEDEMADocument72 pagesOEDEMAAhmed NourNo ratings yet
- Pathology of Heart Failure and CardiomyopathiesDocument33 pagesPathology of Heart Failure and Cardiomyopathiesciyace7849No ratings yet
- باثو 2Document35 pagesباثو 2shahadkhaled171No ratings yet
- Peripheral-Vascular-Disease 2ndDocument84 pagesPeripheral-Vascular-Disease 2ndAb BabyNo ratings yet
- Cardiovascular PathologyDocument182 pagesCardiovascular PathologyPavan chowdaryNo ratings yet
- Diagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaDocument49 pagesDiagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaSiti rahmawatiNo ratings yet
- 1 Heart FailureDocument49 pages1 Heart FailureDammaqsaa W BiyyanaaNo ratings yet
- Hypertension For EMS ProvidersDocument35 pagesHypertension For EMS ProvidersPaulhotvw67100% (5)
- ShockDocument19 pagesShockirenekhatete1No ratings yet
- Chapter 5 HTDocument56 pagesChapter 5 HTtesfamichael mengistu100% (2)
- Reduced Renal Sodium Excretion: Forced Through A Narrow LumenDocument5 pagesReduced Renal Sodium Excretion: Forced Through A Narrow LumenFlowerNo ratings yet
- ENDOCRINE HYPERTENSION. A Number of Hormonal Secretions May Produce Secondary HyDocument5 pagesENDOCRINE HYPERTENSION. A Number of Hormonal Secretions May Produce Secondary HyIsak ShatikaNo ratings yet
- RENAL VASCULAR DISEASES UpdatedDocument97 pagesRENAL VASCULAR DISEASES UpdatedgibreilNo ratings yet
- 1.congestive Heart FailureDocument8 pages1.congestive Heart FailureJarda julie DacuagNo ratings yet
- Heart Failure and Pulmonary EdemaDocument60 pagesHeart Failure and Pulmonary EdemaYosra —No ratings yet
- SHOCK DiscussionDocument22 pagesSHOCK DiscussionNavpreet Kaur100% (1)
- Antihypertensives Part 1Document15 pagesAntihypertensives Part 1alizwaxabanisa8No ratings yet
- Diseases of Blood Vessels Dr. Fe A. Bartolome, Maed, FpasmapDocument15 pagesDiseases of Blood Vessels Dr. Fe A. Bartolome, Maed, FpasmapJayesh MahajanNo ratings yet
- Cerebrovascular Accident/Brain Attack: Gideon Gachihi Associate Faculty, MKUDocument52 pagesCerebrovascular Accident/Brain Attack: Gideon Gachihi Associate Faculty, MKUElvisNo ratings yet
- Patofisiologi HipertensiDocument18 pagesPatofisiologi HipertensiZebyyNo ratings yet
- Heart Failure and CardiomyopathiesDocument26 pagesHeart Failure and Cardiomyopathieslionel andreaNo ratings yet
- Cerebrovascular CVADocument19 pagesCerebrovascular CVAmmkavitha98No ratings yet
- 5 - Pathology of CADDocument58 pages5 - Pathology of CADregeti bhargavNo ratings yet
- Infective Endocarditis: Akriti DahalDocument79 pagesInfective Endocarditis: Akriti DahalAkriti100% (1)
- Neoplasm: - TermsDocument125 pagesNeoplasm: - Termsferina steffiNo ratings yet
- Cerebrovascular Disease and Coronary Artery Disease: DR Masona-MutitiDocument28 pagesCerebrovascular Disease and Coronary Artery Disease: DR Masona-MutitiShaun MazorodzeNo ratings yet
- 5th Chapter DDDocument36 pages5th Chapter DDRameen RizviNo ratings yet
- HF & ShockDocument18 pagesHF & ShockSahar YousifNo ratings yet
- Congestive Heart Failure LathaDocument68 pagesCongestive Heart Failure LathaLatha GhanesanNo ratings yet
- 1-3 Haemodinamicpart1 PDFDocument64 pages1-3 Haemodinamicpart1 PDFSetiawan SukmadjaNo ratings yet
- Hypertensive Encephalopathy: By:hasmawaty BasirDocument78 pagesHypertensive Encephalopathy: By:hasmawaty BasirLexyArungTikuNo ratings yet
- Hypertension: Nucleus Medical MediaDocument17 pagesHypertension: Nucleus Medical Mediakrish oswalNo ratings yet
- Hypertension: MedicineDocument6 pagesHypertension: Medicineapi-3829364No ratings yet
- Hemodynamic Disorders: By: Dr. SL RasonableDocument59 pagesHemodynamic Disorders: By: Dr. SL RasonableJenneth Marquez JoloNo ratings yet
- Hypertensive Emergencies: Sulaiman Usaid G. MBCHB V Facilatator: DR Jack TDocument44 pagesHypertensive Emergencies: Sulaiman Usaid G. MBCHB V Facilatator: DR Jack TUsaid SulaimanNo ratings yet
- Diagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaDocument51 pagesDiagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaHilmaNo ratings yet
- Tatalaksana Hipertensi KrisisDocument39 pagesTatalaksana Hipertensi KrisisImron RosyadiNo ratings yet
- Cardiomyopathy: Restrictive Heart DiseaseDocument18 pagesCardiomyopathy: Restrictive Heart DiseaseMitch GabuyaNo ratings yet
- Acute Vascular Insufficiency (OSN)Document18 pagesAcute Vascular Insufficiency (OSN)Zeyad HassanNo ratings yet
- Antianginal DrugsDocument92 pagesAntianginal DrugsSarthak DubeyNo ratings yet
- Shock: DR Ahmed MohDocument60 pagesShock: DR Ahmed MohSalman KhanNo ratings yet
- Inflammatory and Valvular DisordersDocument43 pagesInflammatory and Valvular DisordersRifqi Hary ZulfikarNo ratings yet
- 11.sudden Natural Death 3Document55 pages11.sudden Natural Death 3Hasabo AwadNo ratings yet
- Secondary Hypertension: S Ystolic-Diastolic Arterial HypetrtensionDocument9 pagesSecondary Hypertension: S Ystolic-Diastolic Arterial HypetrtensionvifawuduNo ratings yet
- The ASCOD Phenotyping of Ischemic Stroke (Updated ASCO Phenotyping)Document5 pagesThe ASCOD Phenotyping of Ischemic Stroke (Updated ASCO Phenotyping)Jose Algomas KnorecuerdoNo ratings yet
- Types of Stroke: Stroke - CVA Cerebral Vascular Accident Ischemic Cerebrovascular DiseaseDocument7 pagesTypes of Stroke: Stroke - CVA Cerebral Vascular Accident Ischemic Cerebrovascular DiseaseMarrylane GamisNo ratings yet
- Acute Coronary Syndrome: An Essential & Practical ApproachDocument35 pagesAcute Coronary Syndrome: An Essential & Practical ApproachGinawidiyastutiNo ratings yet
- Pathophysiology HypertensionDocument4 pagesPathophysiology HypertensionKimberly BautistaNo ratings yet
- Management of Hypertensive Crisis (Diskusi RSUD)Document20 pagesManagement of Hypertensive Crisis (Diskusi RSUD)Kia AgusputraNo ratings yet
- Aninditha. Buku Ajar Neurologi. Jakarta: Departemen Neurologi Fakultas Kedokteran Universitas Indonesia RS Cipto Mangunkusumo. 2017Document2 pagesAninditha. Buku Ajar Neurologi. Jakarta: Departemen Neurologi Fakultas Kedokteran Universitas Indonesia RS Cipto Mangunkusumo. 2017pelangiNo ratings yet
- Stroke Pathophysiology 1Document5 pagesStroke Pathophysiology 1Jeco ValdezNo ratings yet
- Ait Nejm 2020Document9 pagesAit Nejm 2020Ahmed JallouliNo ratings yet
- Hridroga SampraptiDocument39 pagesHridroga SampraptiGAURAVNo ratings yet
- Yejvs - 7432Document9 pagesYejvs - 7432Francisco Álvarez MarcosNo ratings yet
- Burr Hole Washout Versus Craniotomy For Chronic Subdural Hematoma: Patient Outcome and Cost AnalysisDocument1 pageBurr Hole Washout Versus Craniotomy For Chronic Subdural Hematoma: Patient Outcome and Cost AnalysisCelia WijayaNo ratings yet
- Unit 4b Drugs Affecting CVS, Antianginal DrugsDocument17 pagesUnit 4b Drugs Affecting CVS, Antianginal DrugsالدتادتغدتعدNo ratings yet
- Stroke/Cerebrovascular Accident: Transient Ischemic AttacksDocument5 pagesStroke/Cerebrovascular Accident: Transient Ischemic AttacksCraigNo ratings yet
- ANEURYSMDocument39 pagesANEURYSMIvan Roque100% (1)
- Secondary Stroke PreventionDocument54 pagesSecondary Stroke PreventionHùng Phạm Lý ChíNo ratings yet
- Thromboangiitis ObliteransDocument17 pagesThromboangiitis Obliteransmu_crNo ratings yet
- LeukemiaDocument5 pagesLeukemiaNourie BerawiNo ratings yet
- Critical Limb IschemiaDocument11 pagesCritical Limb IschemiaAmalia Hendar PangestutiNo ratings yet
- 3-5 Slides Primary Prophylaxis For Esophageal Varices in Cirrhosis PDFDocument4 pages3-5 Slides Primary Prophylaxis For Esophageal Varices in Cirrhosis PDFBhavin DalalNo ratings yet
- Journal StrokeDocument5 pagesJournal StrokeRika Sartyca IlhamNo ratings yet
- Antianginal Drugs: Dr. Jim AmisiDocument11 pagesAntianginal Drugs: Dr. Jim AmisiMike AnnisNo ratings yet
- Coronary Heart Disease 3Document47 pagesCoronary Heart Disease 3Silvia RNo ratings yet
- Epidemiological Aspects On Abdominal Aortic Aneurysms (AAA)Document17 pagesEpidemiological Aspects On Abdominal Aortic Aneurysms (AAA)Janey Ceniza تNo ratings yet
- Tia Abcd2 Tool 1Document2 pagesTia Abcd2 Tool 1Siti RahmahNo ratings yet
- Carotid Stenosis (Carotid Artery Disease)Document5 pagesCarotid Stenosis (Carotid Artery Disease)Pieter SteenkampNo ratings yet
- NF100 E76 Blood Supply Brain AnnotatedDocument40 pagesNF100 E76 Blood Supply Brain AnnotatedShashiNo ratings yet
- AneurysmDocument7 pagesAneurysmLillabinNo ratings yet
- Woc AcsDocument5 pagesWoc AcsMuhammad Alvin Fuzail IyazNo ratings yet
- Icha Marissa Sofyan c11108318 UAPDocument24 pagesIcha Marissa Sofyan c11108318 UAPIcha Marissa SofyanNo ratings yet