Professional Documents
Culture Documents
Paediatric AIDS
Paediatric AIDS
Uploaded by
vijayasree bavireddy0 ratings0% found this document useful (0 votes)
16 views52 pagesThis document discusses HIV and AIDS. It covers the discovery of HIV, its classification and taxonomy. It describes the two strains of HIV (HIV-1 and HIV-2) and how HIV-1 is further divided into groups and subtypes. It discusses HIV's structure, genome, and the genes it contains. It also summarizes the various modes of transmission of HIV and approaches to diagnosing HIV infection, including tests of viral load and CD4 count. Finally, it outlines the stages of HIV infection from primary infection to AIDS.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses HIV and AIDS. It covers the discovery of HIV, its classification and taxonomy. It describes the two strains of HIV (HIV-1 and HIV-2) and how HIV-1 is further divided into groups and subtypes. It discusses HIV's structure, genome, and the genes it contains. It also summarizes the various modes of transmission of HIV and approaches to diagnosing HIV infection, including tests of viral load and CD4 count. Finally, it outlines the stages of HIV infection from primary infection to AIDS.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
16 views52 pagesPaediatric AIDS
Paediatric AIDS
Uploaded by
vijayasree bavireddyThis document discusses HIV and AIDS. It covers the discovery of HIV, its classification and taxonomy. It describes the two strains of HIV (HIV-1 and HIV-2) and how HIV-1 is further divided into groups and subtypes. It discusses HIV's structure, genome, and the genes it contains. It also summarizes the various modes of transmission of HIV and approaches to diagnosing HIV infection, including tests of viral load and CD4 count. Finally, it outlines the stages of HIV infection from primary infection to AIDS.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 52
HIV-AIDS
Dr. Mohammed Faraaz Khan
Dr. Mohammed Adil Ali
Introduction
Human Immunodeficiency Virus (HIV), was first isolated in
the year 1983 by two scientists separately, namely Robert
Gallo at the National Cancer Institute and Luc Montagnier
alongwith Francoise Barre Sinoussi at the Pasteur Institute.
Paris.
AIDS as a condition was first identified in patients suffering
from Pneumocystis jirovecii pneumonia in 1981. The doubt
arised as the infection occurs only in very
immunocompromised patients. As the first identified cases
were in homosexuals, the condition was initially called Gay
Related Immune Deficiency (GRID).
Introduction
Later it was realized that the condition was not confined to
homosexuals alone which resulted in the condition being
renamed as Acquired Immuno-Deficiency Syndrome
(AIDS).
In 2008, Luc Montagnier and Francoise Barre Sinnousi were
awarded the Nobel prize for their discovery of HIV.
Taxonomy
HIV belongs to the order Ortervirales and the family
Retroviridae belonging to the genus Lentivirus.
The other members of the genus are animal based and infect
animals. They include Caprine arthritis encephalitis virus
which infects sheep and Simian Immuno-deficiency Virus
which infects primate monkeys.
The viruses under this genus generally tend to cause long-
lasting chronic conditions associated with lymphoproliferative
discrepancies such as causing the death of T-lymphocytes
over a period of time.
Classification
HIV has two distinct strains namely, HIV-1 and HIV-2. Infection
with one strain does not confer immunity against the other as the
genetic sequential differences are nearly more than 55% between
the two viruses.
HIV-1 is further divided into three groups ; M (Major), O
(Outlier) and N (Non- major, non-outlier) based on minor genetic
variability.
Group M is further divided into nine subtypes : A,B.C.D.F.G.H.J
and K.
The high mutation rate of HIV is characterized by the high
number of recombinant subtypes leading to a difficulty in
effective HIV management. The aim is to hence find a common
yet feasible antigen which can be successfully targeted.
HIV-1 and HIV-2
HIV-1 HIV-2
Highly virulent Less virulent
Worldwide distribution Restricted to parts of Africa
Associated with chimpanzees Associated with sooty
mangabeys
Regulator gene vpu is present Regulator gene vpx is present
Gp36 is absent Gp36 is present
Morphology
Genomic structure
HIV consists of three main structural genes (gag, pol and env)
and six regulatory genes ( rev, tat, nef, vpr, vpu and vif ).
The gag gene codes for the capsid protein p24 and the matrix
protein p17.
The env gene codes for the envelope glycoproteins such as
gp120 and gp41.
The pol gene codes for the viral enzymes such as reverse
transcriptase , integrase and protease.
The six regulatory genes influence various parts of the virus
replication and its production of viral proteins.
Modes of transmission
HIV can be transmitted by sexual contact, blood transfusion,
sharing of needles , in utero from an infected mother to her
baby , during delivery and even via breastfeeding.
Globally the most common route of transmission is
heterosexual in which anal intercourse has the highest risk of
HIV transmission compared to vaginal or oral.
Development of antigen and antibody tests to screen HIV
infected blood has virtually eliminated blood transfusion as a
mode of infection but the WHO estimates that because of the
lack of adequate screening facilities in resource poor
countries, 5-10% of transfusions globally are with HIV
infected blood.
Modes of transmission
Unlike adults, >95 % of HIV infections in children are
acquired as perinatal transmission from their mothers.
Rare horizontal modes of infection in children include blood
transfusions as in thalassemics and haemophiliacs, sexual
child abuse and very rarely, intravenous drug abuse in
adolescents.
Perinatal transmission
Peripartum infection (60%) during the passage of the baby
through the infected vaginal canal is the commonest mode of
infection, specially in instrumental deliveries.
Transplacental transmission (25%) is rare till 20 weeks of
gestation and usually occurs in the last trimester due to
degenerative changes in the placenta
Postpartum infection (15%) via breastfeeding usually occurs
in early stages of breastfeeding when breast/ nipple problems
are common.
Delta 32 mutation
1% of the European population possesses a mutation known
as delta 32 mutation which results in a change in the structure
of the CCR5 receptor present on the macrophages thus
preventing HIV from binding and entering the cell and
rendering the person immune to HIV infection.
The mutation is autosomal recessive and homozygosity is
required for total immunity. Heterozygous individuals have an
enhanced resistance to the virus though they are not
completely immune and take many years more than normal
individuals to progress to AIDS.
Diagnosis
As of now, the trend is towards universal HIV testing rather than
selective screening.
The diagnosis is carried out by performing ELISA to detect antibodies
to both HIV-1 and HIV-2.
In case of a positive result, confirmation should be obtained by a
Western blot.
However a positive antibody test from two different immunoassays
is sufficient to confirm infection.
But in some cases such as infants who carry maternal antibodies and
patients in whom a diagnosis is required before the formation of
antibodies, detection of p24 capsid antigen is the test of choice as it is
cheaper than nucleic acid assays.
If available, a nucleic acid assay such as a Reverse Transcriptase
PCR is superior to p24 capsid antigen detection.
Diagnostic criteria for HIV infection in
children (WHO 2006)
< 18 months of age: A positive virological test (DNA-PCR)
after at least 4 weeks of birth, re-confirmed on a second
sample.
> 18 months of age:
1) A positive virological test (DNA-PCR), re-confirmed on a
second sample.
2) Two positive HIV antibody tests with different principles in
a symptomatic case.
3) Three positive HIV antibody tests with different principles
in an asymptomatic case.
CD4 count and viral load
The normal CD4 counts in a person are always above 500
cells per mm3. CD4 counts are always determined by the
technique of flow cytometry.
The CD4 count is used together with the clinical staging
chart to decide when to begin anti-retroviral therapy and
prophylaxis against opportunistic infections.
However viral load measurement is the test of choice for
monitoring response to treatment.
The issue is the lack of routine viral load monitoring
facilities in the resource poor countries which poses
difficulty in effectively monitoring the response to
treatment.
Immunological classification (WHO
2006)
Categories < 11 months 12-35 >36-59 > 5 years
months months
Not >35% >30% >25% >500
significant
Mild 30-35% 25-30% 20-25% 350-499
Advanced 25-30% 20-25% 15-20% 200-349
Severe <25% or <20% or <15% or <15% or
<1500 <750 <350 <200
Stages of infection
Primary infection: This is the first stage following
inoculation. After an incubation period of usually 2
weeks, the patient presents with a viral fever like
illness complete with fever, headache , malaise,
lymphadenopathy, pharyngitis, diarrhoea and a
maculopapular rash. The differential diagnosis should
be infectious mononucleosis, toxoplasmosis,
cytomegalovirus infection, influenza, rubella and even
secondary syphilis. P24 antigen detection and PCR are
useful to diagnose the infection in this stage and
antibody formation takes at least 2 weeks.
Window period: This is a period of prolonged clinical latency
wherein there are no symptoms and the viral load is
maintained at a plateau phase within 3 months with slow
increase over a matter of years. Antibody tests are positive for
the virus In this stage.
Minor associated HIV disorders: A wide range of disorders
indicating some impairment of cellular immunity occur in
most patients before they develop AIDS.
AIDS: AIDS is defined by the development of specified
opportunistic infections, cancers and severe manifestations o
HIV itself. CDC category C is the most widely used definition
of AIDS.
Natural course of perinatal infection in children Is different
from adult infection due to:
1) Higher viral load due to sustained exposure in intrauterine,
peripartum and postnatal period.
2) Large and expanding CD-4 cell pool in a growing baby
facilitating viral multiplication.
3) Relative immaturity of HIV specific immune responses to
limit the infection.
Presenting problems in HIV infection
Mucocutaneous involvement is the most common
presentation of HIV infection in general practice
(Candidiasis, herpes zoster, Kaposi’s sarcoma)
However Pneumocystis jirovecii pneumonia is the most
common presentation in AIDS patients.
CNS conditions of prime importance common in AIDS
include progressive multifocal leukoencephalopathy, cerebral
toxoplasmosis and primary CNS lymphoma. Meningitis is
mostly Cryptococcal or tubercular in nature. Space occupying
lesions such as cryptococcoma and tuberculoma are often a
result of the former meningitis.
Failure to thrive
This is the commonest clinical presentation in Indian children,
defined as:
1) Weight <5th percentile
2) Weight loss> 10% than earlier record or
3) Weight loss crossing at least 2 major percentiles on growth
curves.
HIV wasting syndrome as seen in adults is not as common in
children and diagnosis requires presence of three features
namely: a) Failure to thrive, b) chronic diarrhoea/ enteropathy
and c) prolonged pyrexia
Mucocutaneous disease
The common conditions included, but are not restricted to, are
Herpes simplex infection, Herpes zoster, mucocutaneous
candidiasis and Kaposi’s sarcoma.
Herpes simplex and Herpes Zoster tend to get reactivated
easily as the immunity has fallen.
Candidiasis is usually one of the first conditions seen and is
generally seen first in the mouth.
Skin infections occur very easily in these patients even with
minor trauma.
Kaposi’s sarcoma
This is a spindle cell tumor of lympho endothelial origin seen
more frequently in AIDS patients though the incidence in
India is lower than the European countries.
Kaposi’s sarcoma has four types:
1) Classic KS
2) Endemic form
3) AIDS associated
4) Immunosuppressant associated
However, while it is common in adults, Kaposi’s sarcoma is
extremely rare in children.
Respiratory disease
Pneumocystis jirovecii pneumonia is the most common
respiratory complication in high income countries while
Tuberculosis is the most common in middle and low income
countries.
Bacterial pneumonia has an incidence which is increased
about 100 fold in HIV infection.
The most common organisms are Streptococcus pneumoniae,
Haemophilus influenzae, Klebsiella pneumoniae and
Staphylococcus aureus. Other causes could include Nocardia
species as well.
Pneumocystis jirovecii
Pneumocystis jirovecii pneumonia tends to occur when the
CD4 cells have fallen below 200 cells/mm3.
The onset is with progressive breathlessness, dry cough and
fever.
X-ray is useful in the diagnosis which reveals bilateral
interstitial infiltrates usually involving the lower lobes of the
lungs.
The sputum can be analysed by PCR or methenamine silver
stain to confirm the diagnosis. The organism cannot be
cultured on culture media.
Treatment is with co-trimoxazole for 21 days or pentamidine
otherwise.
Gastrointestinal system
Chronic diarrhoea is the most common GIT manifestation and
may be due to Cryptosporidium,Isospora, bacterial infections,
Giardiasis or even HIV enteropathy.
Candidiasis, the most common opportunistic infection of the
GIT presents as:
1) Persistent oral or esophageal thrush
2) Dysphagia due to esophageal candidiasis
3) Chronic diarrhoea due to intestinal candidiasis
Central nervous system
HIV causes three types of neurological disorders namely
cognitive disorders, space occupying lesions and meningitis.
Progressive multifocal leukoencephalopathy caused by the JC
virus is the most important cognitive disorder.
Cerebral toxoplasmosis, primary CNS lymphoma (PCNSL),
tuberculoma and cryptococcoma are the usual space
occupying lesions.
Meningitis is frequently caused by Streptococcus pneumoniae,
Cryptococcus neoformans and Mycobacterium tuberculosis.
Unlike adults, cryptococcal meningitis and CNS tumours are
less common in HIV infected children.
HIV encephalopathy
HIV encephalopathy develops in about 40% survivors beyond
infancy due to direct viral infection and cytopathic damage to
neuronal cells.
Clinical manifestations usually begin in the second year of life
characterised by a) Regression of milestones/ cognitive
function b) microcephaly c) progressive symmetrical spastic
paresis with gait abnormalities.
Important CT/MRI findings include cerebral atrophy with
venticular dilatation and basal ganglia calcifications.
Anti-retroviral therapy (ART)
ART refers to the treatment provided to HIV positive patients
in order to combat the virus using a variety of drugs.
The most commonly used classes of drugs include:
1) Nucleoside reverse transcriptase inhibitors (NRTI’s) :
Abacavir, Lamivudine, Zidovudine, Emtricitabine, Tenofovir.
2)Non-nucleoside reverse transcriptase inhibitors(NNRTI’s):
Efavirenz, Etravirine, Nevirapine.
3) Protease inhibitors: Darunavir, Lopinavir, Ritonavir.
4) Integrase inhibitors: Raltegravir
5) CCR5 receptor antagonist: Maraviroc
When to start ART?
ART is indicated in all cases with confirmed HIV infection.
However, ART should be deferred until acute infections are
treated, if possible.
In cases with HIV-TB co-infection, anti-tubercular therapy is
the priority and ART should be started after 2-6 weeks.
Monitoring efficacy
For monitoring the efficacy, viral load measurement is the test
of choice and not CD4 cell count.
A baseline viral load should be obtained prior to starting ART.
After that, the viral load should be checked once after 4-8
weeks.
After 6 months, the viral load should be suppressed to an
undetectable level which is usually less than 50 copies per
mL.
Failure of the ART regimen is indicated by a viral load
between 400-1000 copies/mL and warrants a change in the
ART regimen.
1st line regimen
The standard first line regimen is a combination of two
NRTI’s and one NNRTI.
The WHO prefers NNRTI’s as the first line choice of drugs as
they are cheaper than and better tolerated than Protease
inhibitors.
The usual combinations include Emtricitabine and Tenofovir
with an NNRTI such as Nevirapine.
WHO regimens
WHO recommended preferred regimens are as follows:
Age <3 years : Abacavir / Zidovudine + Lamivudine+
Lopinavir
Age 3-10 years: Abacavir+ Lamivudine + Efavirenz
Age > 10 years: Tenofovir + Lammivudine+ Efavirenz
Dosages
Zidovudine: 240 mg/m2
Lamivudine: 4mg/kg BD
Abacavir: 8mg/kg BD
Tenofovir: 300 mg OD ( >10 years of age)
Nevirapine: 120-200mg/m2 OD
Efavirenz: 200-600 mg OD ( not for children <3 years)
Lopinavir: 225 mg/m2 BD
Ritonavir: 400 mg/m2 BD (>2 years)
2nd line regimen
When failure has been indicated by means of virological load
testing, the switchover to the second line drugs should be
carried out which consists of dual NRTI’s with a Ritonavir
boosted Protease inhibitor such as Darunavir or Lopinavir.
Ritonavir is toxic in therapeutic doses but is given in a low
dose along with other Protease inhibitors as it increases their
half life and reduces elimination.
A regimen called TRIO has successfully achieved more than
90% reduction rates in several patients. It consists of
Darunavir, Raltegravir and Etravirine.
Side effects
1) Immune Reconstitution Inflammatory syndrome : IRIS is a
fairly common complication of ART characterized by
worsening of the disease and opportunistic infections. The
treatment is purely supportive and consists of continuing ART
and treating the infection completely.
2) Lipodystrophy: Changes in body fat distribution such as
subcutaneous fat loss and fat gain are commonly observed in
patients on long term ART.
3) Rashes: Commonly observed with NNRTI’s, they are
minor and do not constitute a major problem. If the rash
worsens or systemic features develop, the drug is
discontinued.
Post exposure prophylaxis
Post exposure prophylaxis is recommended to anyone who
has a significant risk of acquiring the infection after an
exposure.
The first dose should be given as soon as possible, preferably
within 6-8 hours. There is no point in administering PEP 72
hours after exposure.
The usual regimen consists of dual NRTI’s with a PI or
Efavirenz in high risk exposures.
HIV antibody testing should be performed at 6, 12 and 24
weeks after exposure.
Prevention
There is no vaccine for HIV. Prevention relies on behavioral
change in the form of:
1) Safer sex practices
2) Screening of blood and blood products before transfusion
3) Avoidance of needle sharing especially amongst
intravenous drug abusers.
4) Post exposure prophylaxis
5) Male circumcision
6) Treatment of pregnant mothers to reduce vertical
transmission
Prevention of perinatal transmission
Routine opt out antenatal HIV testing.
ART to HIV infected mothers:- Zidovudine administration
starting at 28 weeks of gestation and bolstered by single dose
Nevirapine at delivery is the standard regimen used in
resource limited nations. Though it is cost effective, it is less
effective than other options, does not cover the risk of HIV
transmission during breastfeeding and adds to the risk of
acquiring Nevirapine resistance.
It is recommended that all pregnant and breastfeeding women
living with HIV undertake lifelong ART regardless of CD4
count or clinical stage.
Early LSCS delivery:- Early LSCS delivery has been fund to
reduce the risk of transmission to the fetus by shortening the
exposure time. However it is associated with a risk of pre-term
infants. Moreover, the mode of delivery does not impact
infectivity to the fetus if the viral load was suppressed
beforehand on ART.
Early infant feeding:- Exclusive breastfeeding is recommended
in resource limited settings for the 12 month duration with
supplementary feeding from 6 months of age.
If replacement feeding is sought, it must fulfill the AFASS
criteria ( acceptable, feasible, affordable, sustainable and safe).
Mixed feeds are totally contraindicated during the first 6
months.
The HIV gallery
Freddie Mercury Howard Ashman
(1946-1991) (1950-1991)
Singer, songwriter and lead Playwright, lyricist and winner
vocalist for the band Queen Of two Oscars for best original
Song for the movies; Beauty and
The Beast and The Little Mermaid
The HIV gallery
Anthony Perkins
(1930-1992) Charlie Sheen
Actor best known for playing ‘Norman Bates’ (Born 1965)
in Alfred Hitchcock’s 1960 movie Psycho Actor known for
the series ‘Two and a half men’
You might also like
- JJAU BookletFinal 20150927 LQDocument5 pagesJJAU BookletFinal 20150927 LQYasuhito NumamuraNo ratings yet
- Kimutai N Gideon Dennis Mutiso Moderator DR Songok 07 FEB 2011Document56 pagesKimutai N Gideon Dennis Mutiso Moderator DR Songok 07 FEB 2011drgiddie7640No ratings yet
- HivDocument29 pagesHivSUTHAN100% (2)
- HIV and Related InfectionsDocument50 pagesHIV and Related InfectionsHassan.shehriNo ratings yet
- Hiv AidsDocument9 pagesHiv Aidschuramarak23No ratings yet
- HIVDocument79 pagesHIVMehiella SatchiNo ratings yet
- Case 17 HIV-1Document19 pagesCase 17 HIV-1ngNo ratings yet
- Immune Deficinecy: By: Kirk Odrey O. Jimenez R.NDocument51 pagesImmune Deficinecy: By: Kirk Odrey O. Jimenez R.NKirk08No ratings yet
- Hiv Aids FNLDocument68 pagesHiv Aids FNLMelesNo ratings yet
- Red - Book - ® - Atlas - of - Pediatric - Infectious - Diseases - 4TH - EDITION - Copy (1) - 325-333Document9 pagesRed - Book - ® - Atlas - of - Pediatric - Infectious - Diseases - 4TH - EDITION - Copy (1) - 325-333jessica mezaNo ratings yet
- Hiv AidsDocument86 pagesHiv AidsLady AngodNo ratings yet
- Presented By: DR - Biswajeeta Saha (1 Yr PG) Moderator: Dr. N. Sahu, Dept of Pathology, Kims, BBSRDocument43 pagesPresented By: DR - Biswajeeta Saha (1 Yr PG) Moderator: Dr. N. Sahu, Dept of Pathology, Kims, BBSRBiswajeeta SahaNo ratings yet
- RetrovirusesDocument7 pagesRetroviruseseluardpaul37No ratings yet
- Human Immunodeficiency Virus HIVDocument14 pagesHuman Immunodeficiency Virus HIVAdam ChungNo ratings yet
- Gen Patho AIDSDocument22 pagesGen Patho AIDSJireh MejinoNo ratings yet
- HIV Patient Case - StudentDocument11 pagesHIV Patient Case - StudentNancy FNo ratings yet
- Gulu Cohes Hiv Nelly MDDocument68 pagesGulu Cohes Hiv Nelly MDYIKI ISAACNo ratings yet
- Pertemuan Ke-2 REPRODocument74 pagesPertemuan Ke-2 REPROAbi Surya MandalaNo ratings yet
- AIDSDocument32 pagesAIDSJuwairia tariqNo ratings yet
- Presentation - AIDSDocument14 pagesPresentation - AIDSPuguNo ratings yet
- Perio2000 2007 MTYinDocument27 pagesPerio2000 2007 MTYinmin moongNo ratings yet
- VirusDocument51 pagesVirusBatool SherbiniNo ratings yet
- 3 HIV PresentationDocument22 pages3 HIV PresentationMaiCAlmanzorNo ratings yet
- Virus 7 LastDocument50 pagesVirus 7 LastBatool SherbiniNo ratings yet
- Hiv/Aids: by Aisha MansurDocument34 pagesHiv/Aids: by Aisha MansurMpanso Ahmad AlhijjNo ratings yet
- Hiv AidsDocument7 pagesHiv Aidsandirio7486No ratings yet
- Prepared By: Dr. Brian Gilbert Fernandez, DPCOMDocument28 pagesPrepared By: Dr. Brian Gilbert Fernandez, DPCOMShivani GauswamiNo ratings yet
- Biology Ip XiiDocument8 pagesBiology Ip XiiSugumaran MageshNo ratings yet
- Teachers' Topics The Pharmacotherapy of The Modern Day Epidemic Infection With Human Immunodeficiency Virus (HIV)Document9 pagesTeachers' Topics The Pharmacotherapy of The Modern Day Epidemic Infection With Human Immunodeficiency Virus (HIV)amin2002No ratings yet
- Inrauterine InfectionsDocument83 pagesInrauterine Infectionsahmad aminNo ratings yet
- Aids HivDocument43 pagesAids Hivjoemarie SalduaNo ratings yet
- Herpesvirus Infections in Immunocompromised Patients: An OverviewDocument29 pagesHerpesvirus Infections in Immunocompromised Patients: An OverviewAyioKunNo ratings yet
- The HIV AIDS QuestionDocument98 pagesThe HIV AIDS Questionbadboy6.868510No ratings yet
- Human Immunodeficiency Virus Case AnalysisDocument5 pagesHuman Immunodeficiency Virus Case AnalysisAllen Bugarin CabadingNo ratings yet
- NPGMC Revision Course HIV in Pregnancy, Sept 2005 FinalDocument51 pagesNPGMC Revision Course HIV in Pregnancy, Sept 2005 Finalapi-3705046No ratings yet
- AIDSDocument71 pagesAIDSapi-19916399No ratings yet
- What Is HIV?Document8 pagesWhat Is HIV?Quan ThieuNo ratings yet
- Presented By: Marlene Lombi C T SiviaDocument19 pagesPresented By: Marlene Lombi C T SiviaVanlal RemruatiNo ratings yet
- Serology Chapter 24 WorksheetDocument3 pagesSerology Chapter 24 WorksheetRikkiNo ratings yet
- Abubaker SikyDocument6 pagesAbubaker SikyAbubaker sikyNo ratings yet
- Text Book of Microbiology (221-330)Document110 pagesText Book of Microbiology (221-330)Jamila ridaNo ratings yet
- Cytomegalovirus (CMV) HepatitisDocument3 pagesCytomegalovirus (CMV) HepatitisN NwekeNo ratings yet
- HIV SeminarDocument111 pagesHIV SeminarRakshaNo ratings yet
- 7-Human Immunodeficiency Virus (HIV)Document6 pages7-Human Immunodeficiency Virus (HIV)TᕼE FᗩᗪEᗪ ᔕOᑌᒪNo ratings yet
- Cquired Mmune Eficiency Yndrome : A I D S AidsDocument41 pagesCquired Mmune Eficiency Yndrome : A I D S AidsprinceejNo ratings yet
- Human Immunodeficency VirusDocument58 pagesHuman Immunodeficency VirusRandy BerryNo ratings yet
- Secondary ImmunodeficiencyDocument26 pagesSecondary ImmunodeficiencyHira.S Faisal (Hiradr)No ratings yet
- HIV DiagnosisDocument47 pagesHIV DiagnosisDharaneedhar AdepuNo ratings yet
- HIV DISEASE - Physiotherapy ClassDocument32 pagesHIV DISEASE - Physiotherapy ClassPraveen RajNo ratings yet
- Hiv Infection and AidsDocument51 pagesHiv Infection and Aidspokhara gharipatanNo ratings yet
- Current Perioperative Management of The Patient With Hiv A B, H M, C R, A G, A K e A.M. FDocument12 pagesCurrent Perioperative Management of The Patient With Hiv A B, H M, C R, A G, A K e A.M. FPrashant SinghNo ratings yet
- From Wikipedia, The Free Encyclopedia: Classification and External ResourcesDocument25 pagesFrom Wikipedia, The Free Encyclopedia: Classification and External ResourcesLismir DushajNo ratings yet
- Hiv/Aids: Mariano Marcos State University College of Health Sciences Department of Nursing Batac City, Ilocos NorteDocument10 pagesHiv/Aids: Mariano Marcos State University College of Health Sciences Department of Nursing Batac City, Ilocos NorteEyySiEffVee100% (1)
- Pertemuan Ke-2 REPRODocument74 pagesPertemuan Ke-2 REPROMohamad Rheza F ZamzamiNo ratings yet
- REVIEWER - Management of Patients With Immune Deficiency DisordersDocument2 pagesREVIEWER - Management of Patients With Immune Deficiency DisordersRaquel HatulanNo ratings yet
- Anesthesia For The Pregnant HIV PatientDocument17 pagesAnesthesia For The Pregnant HIV PatientrolandoanestesiaNo ratings yet
- 2 AidsDocument99 pages2 AidsSazzad JoyNo ratings yet
- Pertemuan Ke-2 REPRODocument74 pagesPertemuan Ke-2 REPROAdi Joyo NegoroNo ratings yet
- Hiv Aids in PediatricsDocument60 pagesHiv Aids in Pediatricsmy Lord JesusNo ratings yet
- HerpesvirusesDocument54 pagesHerpesvirusessameera ruffaiNo ratings yet
- Feline Immunodeficiency Virus: From Diagnosis to Well-being for Cats with FIVFrom EverandFeline Immunodeficiency Virus: From Diagnosis to Well-being for Cats with FIVNo ratings yet
- Newer Vaccines June 2023 Pravi Bhuvi MamDocument13 pagesNewer Vaccines June 2023 Pravi Bhuvi Mamvijayasree bavireddyNo ratings yet
- Sample Collection and TransportDocument64 pagesSample Collection and Transportvijayasree bavireddyNo ratings yet
- Jbacter00724 0040Document6 pagesJbacter00724 0040vijayasree bavireddyNo ratings yet
- Praveen Stool Concentration Methods June 24Document34 pagesPraveen Stool Concentration Methods June 24vijayasree bavireddyNo ratings yet
- Human Leukocyte Antigens: Dr. B.Vijayasree 1 Year Post-Graduate Department of MicrobiologyDocument30 pagesHuman Leukocyte Antigens: Dr. B.Vijayasree 1 Year Post-Graduate Department of Microbiologyvijayasree bavireddyNo ratings yet
- Moraxella: DR - Vijayasree 2 Year Post-GraduateDocument6 pagesMoraxella: DR - Vijayasree 2 Year Post-Graduatevijayasree bavireddyNo ratings yet
- ROLE OF A MICROBIOLOGIST IN PREVENTION OF HEALTHCARE-ASSOCIATED INFECTIONS - v3Document12 pagesROLE OF A MICROBIOLOGIST IN PREVENTION OF HEALTHCARE-ASSOCIATED INFECTIONS - v3vijayasree bavireddyNo ratings yet
- Bacterial Cell Wall: Dr. B.Vijayasree 1 Year Post-Graduate SMC, VjaDocument42 pagesBacterial Cell Wall: Dr. B.Vijayasree 1 Year Post-Graduate SMC, Vjavijayasree bavireddyNo ratings yet
- 10 Question Related To InheritanceDocument4 pages10 Question Related To InheritancePrashant kumarNo ratings yet
- Sizing of Current TransformerDocument6 pagesSizing of Current TransformerAhmed SeddikNo ratings yet
- Background Medical CountermeasuresDocument7 pagesBackground Medical Countermeasuresapi-246003035No ratings yet
- Sample School Report CardDocument12 pagesSample School Report CardMuradxan NovruzovNo ratings yet
- A Case Study of Huawei: Strategic and Environment Analysis: August 2021Document8 pagesA Case Study of Huawei: Strategic and Environment Analysis: August 2021Khaled WalidNo ratings yet
- FrootiDocument5 pagesFrootiRachel MonisNo ratings yet
- Integrated InveterDocument24 pagesIntegrated InveterDoan Anh TuanNo ratings yet
- (Toni) TX MS W Chinese Scalp AcupDocument16 pages(Toni) TX MS W Chinese Scalp AcupAngelaNo ratings yet
- Nikole Hannah-Jones - Twitter Search TwitterDocument1 pageNikole Hannah-Jones - Twitter Search TwitterLindsay LooperNo ratings yet
- Posse. Analecta Vaticana. 1878.Document240 pagesPosse. Analecta Vaticana. 1878.Patrologia Latina, Graeca et OrientalisNo ratings yet
- Ad 630Document12 pagesAd 630rafaelfialhoNo ratings yet
- Cloze Test PowerPointDocument14 pagesCloze Test PowerPointsetdangNo ratings yet
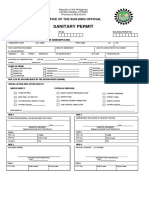
- Sanitary Permit (Front)Document1 pageSanitary Permit (Front)Darwin CustodioNo ratings yet
- Fifth Year Quiz 2021 EndoDocument6 pagesFifth Year Quiz 2021 Endohoho2019kuNo ratings yet
- Amazon Cognito PrinciplesDocument3 pagesAmazon Cognito PrinciplesHaider HadiNo ratings yet
- Lesson 4 - History of Development Economics (First Part)Document12 pagesLesson 4 - History of Development Economics (First Part)Rose RaboNo ratings yet
- Backup Types and Methods in NetbackupDocument9 pagesBackup Types and Methods in NetbackupSrinivas KumarNo ratings yet
- L-s1 Specification For Low Voltage Internal Electrical InstallationDocument154 pagesL-s1 Specification For Low Voltage Internal Electrical InstallationKW LeeNo ratings yet
- The Pathophysiology of Peptic UlcerDocument15 pagesThe Pathophysiology of Peptic UlcerKike Meneses100% (1)
- When Do We Use The Infinitive or - INGDocument2 pagesWhen Do We Use The Infinitive or - INGMarioNo ratings yet
- Pros & Cons Impacts of Social MediaDocument2 pagesPros & Cons Impacts of Social MediaWan NursyakirinNo ratings yet
- Brkipm-2011 - Multicast MplsDocument106 pagesBrkipm-2011 - Multicast MplsmatarakiNo ratings yet
- Effect On The PerformanceDocument11 pagesEffect On The Performancehanna abadiNo ratings yet
- Tutorial Letter 101/0/2022: Programming: Contemporary ConceptsDocument12 pagesTutorial Letter 101/0/2022: Programming: Contemporary Concepts33822018No ratings yet
- CVS 4150 & 4160 Pressure Controller July 2012Document12 pagesCVS 4150 & 4160 Pressure Controller July 2012Zts MksNo ratings yet
- Scus 942.54Document4 pagesScus 942.54Leeyo DesuNo ratings yet
- Chapter 7 Linear Momentum and Collisions - CompressDocument30 pagesChapter 7 Linear Momentum and Collisions - Compressdeez IINo ratings yet
- CRMDocument9 pagesCRMJITESH KHURANANo ratings yet
- School: Grade: Teacher: Learning Area: Date & Time: Quarter: SecondDocument3 pagesSchool: Grade: Teacher: Learning Area: Date & Time: Quarter: SecondJhen MendozaNo ratings yet