Professional Documents
Culture Documents
CH 41
CH 41
Uploaded by
Pooja AcharyaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CH 41
CH 41
Uploaded by
Pooja AcharyaCopyright:
Available Formats
Chapter 41
Intraoral Radiography
Copyright 2003, Elsevier Science (USA).
All rights reserved. No part of this product may be reproduced or transmitted in any
form or by any means, electronic or mechanical, including input into or storage in any
information system, without permission in writing from the publisher.
PowerPoint® presentation slides may be displayed and may be reproduced in print
form for instructional purposes only, provided a proper copyright notice appears on
the last page of each print-out.
Produced in the United States of America
ISBN 0-7216-9770-4
Introduction
There are two basic techniques for obtaining periapical
radiographs:
• Paralleling technique.
• Bisection of the angle technique.
The American Academy of Oral and Maxillofacial
Radiology and the American Association of Dental
Schools recommend the use of the paralleling technique
because it provides the most accurate image.
In some situations the operator may have to use the
bisection technique.
Copyright 2003, Elsevier Science (USA). All rights reserved.
The Full Mouth Survey: FMX
An intraoral full mouth examination is composed of
both periapical and bite-wing projections.
This technique requires the use of intraoral film
that is placed inside of the mouth and is used to
examine the teeth and supporting structures.
On the average adult, a full mouth series consists
of 18 to 20 films. Generally, there are 14
periapicals and 4 to 6 bite-wings, but the number
may vary.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-2 Mounted full mouth series with eight anterior films using the
paralleling technique.
Fig. 41-2 B
Copyright 2003, Elsevier Science (USA). All rights reserved.
The Paralleling Technique: Basic Rules
Film placement: Position the film so that it will cover the
teeth.
Film position: Position the film parallel to the long axis of
the tooth. The film in the film holder must be placed away
from the teeth and toward the middle of the mouth.
Vertical angulation: Direct the central ray of the x-ray
beam perpendicular to the film and the long axis of the tooth.
Horizontal angulation: Direct the central ray of the x-ray
beam through the contact areas between the teeth.
Central ray: Center the x-ray beam on the film to ensure
that all areas of the film are exposed.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-5 Positions of the film teeth and central ray of the x-ray beam in the
paralleling technique.
Fig. 41-5
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-6 The x-rays pass through the contact areas of the premolars
because the central ray is directed through the contacts and perpendicular to
the film.
Fig. 41-6
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-7 This radiograph demonstrates a cone cut.
Fig. 41-7
Copyright 2003, Elsevier Science (USA). All rights reserved.
Exposure Sequence
When exposing radiographs, establish an
exposure sequence, or definite order for
periapical film placement.
Without an exposure sequence, there is a good
chance that you will omit an area or expose the
same area twice.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Anterior Exposure Sequence
When exposing periapical films with the paralleling
technique, always start with the anterior teeth
(canines and incisors) because:
• The number 1 size film used for anteriors is
small, less uncomfortable, and easier for the
patient to tolerate.
• It is easier for the patient to become
accustomed to the anterior film holder.
• The anterior film placements are less likely to
cause the patient to gag.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Anterior Exposure Sequence cont’d
Begin with the maxillary right canine (tooth #6).
Expose all of the maxillary anterior teeth from right to left.
End with the maxillary left canine (tooth #11).
Next, move to the mandibular arch.
Begin with the mandibular left canine (tooth #22).
Expose all of the mandibular anterior teeth from left to
right.
Finish with the mandibular right canine (tooth #27).
Copyright 2003, Elsevier Science (USA). All rights reserved.
Posterior Exposure Sequence
After completing the anterior teeth, begin the
posterior teeth.
Always expose the premolar film before the molar
film because:
• Premolar film placement is easier for the patient
to tolerate than molar film placement.
• Premolar exposure is less likely to evoke the gag
reflex.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Tips for Film Placement
The white side of the film always faces the teeth.
The anterior films are always placed vertically.
The posterior films are always placed horizontally.
The identification dot on the film is always placed in the
slot of the film holder (dot in the slot).
Always position the film holder away from the teeth and
toward the middle of the mouth.
Always center the film over the areas to be examined.
Always place the film parallel to the long axis of the teeth.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Preparation Before Seating the Patient
Prepare the operatory with all infection control barriers.
Determine the number and type of films to be exposed.
Label a paper cup with the patient's name and the date.
• This is the transfer cup for storing and moving exposed
films.
Turn on the x-ray machine and check the basic settings.
Wash and dry hands.
Dispense the desired number of films and store them
outside of the room in which the x-ray machine is being
used.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Positioning the Patient
Seat the patient comfortably in the dental chair, with the back
in an upright position and the head supported.
Ask the patient to remove eyeglasses and bulky earrings.
Have the patient remove any removable prosthetic appliances
from his or her mouth.
Position the patient with the occlusal plane of the jaw being
radiographed parallel to the floor when the mouth is in the
open position.
Drape the patient with a lead apron and thyroid collar.
Wash and dry hands and put on clean examination gloves.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Maxillary Cuspid Region
Insert the number 1 film packet vertically into the
anterior bite-block.
Position the film packet with the cuspid and first
premolar centered. Position film as far posterior as
possible.
With the film-holding instrument and film in place,
instruct the patient to close the mouth slowly but
firmly.
Position the localizing ring and positioning
indicating device (PID), and then expose the film.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-10 Assembling the XCP (Extension-Cone Paralleling Instruments),
Anterior Assembly.
Fig. 41-10
Copyright 2003, Elsevier Science (USA). All rights reserved.
Maxillary Central/Lateral Incisor Region
Insert the number 1 film packet vertically into the
anterior bite-block.
Center the film packet between the central and
lateral incisors and position the film as far posterior
as possible.
With the film-holding instrument and film in place,
instruct the patient to close the mouth slowly but
firmly.
Position the localizing ring and PID and then
expose the film.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-11 Assembling the XCP (Extension-Cone Paralleling Instruments),
Posterior Assembly.
Fig. 41-11
Copyright 2003, Elsevier Science (USA). All rights reserved.
Mandibular Cuspid Region
Insert the number 1 film packet vertically into the
anterior bite-block. Center the film on the cuspid.
Position the film as far in the lingual direction as
the patient’s anatomy will allow.
A cotton roll may be placed between the maxillary
teeth and bite-block to prevent rocking of the bite-
block on the cuspid tip and to increase patient
comfort.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-14 Mandibular cuspid region.
Fig. 41-14
Copyright 2003, Elsevier Science (USA). All rights reserved.
Mandibular Incisor Region
Insert the number 1 film packet vertically into the
anterior bite-block.
Center the film packet between the central and
lateral incisors and position the film as far in the
lingual direction as the patient's anatomy will allow.
With the instrument and film in place, instruct the
patient to close the mouth slowly but firmly.
Position the localizing ring and PID and then
expose the film.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig 41-15 Mandibular incisor region.
Fig. 41-15
Copyright 2003, Elsevier Science (USA). All rights reserved.
Maxillary Premolar Region
Insert the film packet horizontally into the posterior
bite-block, pushing the film packet all the way into
the slot.
Center the film packet on the second premolar.
Position film in the midpalate area.
With the instrument and film in place, instruct the
patient to close the mouth slowly but firmly.
Position the localizing ring and PID and then
expose the film.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-16 Maxillary premolar region.
Fig. 41-16
Copyright 2003, Elsevier Science (USA). All rights reserved.
Maxillary Molar Region
Insert the film packet horizontally into the posterior
bite-block.
Center the film packet on the second molar.
Position the film in the midpalate area.
With the instrument and film in place, instruct the
patient to close the mouth slowly but firmly.
Position the localizing ring and PID and then
expose the radiograph.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-17 Maxillary molar region
Fig. 41-17
Copyright 2003, Elsevier Science (USA). All rights reserved.
Mandibular Premolar Region
Insert the number 2 film horizontally into the posterior
bite-block.
Center the film on the contact point between the second
premolar and first molar. Position the film as far in the
lingual direction as the patient's anatomy will allow.
With the instrument and film in place, instruct the patient
to close the mouth slowly but firmly.
Slide the localizing ring down the indicator rod to the
patient's skin surface.
Position the localizing ring and PID and then expose the
film.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-18 Mandibular premolar region.
Fig. 41-18
Copyright 2003, Elsevier Science (USA). All rights reserved.
Mandibular Molar Region
Insert the number 2 film horizontally into the
posterior bite-block.
Center the film on the second molar. Position the
film as far in the lingual direction as the tongue will
allow. This position will be closer to the teeth than
that for the premolar and anterior views.
With the instrument and film in place, instruct the
patient to close the mouth slowly but firmly.
Position the localizing ring and PID and then
expose the film.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-19 Mandibular molar region.
Fig. 41-19
Copyright 2003, Elsevier Science (USA). All rights reserved.
The Bisecting Technique
The bisection of the angle technique is based on a
geometric principle of bisecting a triangle
(bisecting means dividing into two equal parts).
The angle formed by the long axis of the teeth and
the film is bisected, and the x-ray beam is directed
perpendicular to the bisecting line.
Perpendicular means at a right angle to the film.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-20 The bisecting technique.
Fig. 41-20
Copyright 2003, Elsevier Science (USA). All rights reserved.
Film Holders
Although you may see operators asking the patients
to hold the film with their fingers to stabilize the film
in the mouth, it is not recommended. This
practice exposes the patient's hand and finger to
unnecessary radiation.
The following are types of commercial film holders
that are available:
• Rinn BAI Instruments
• EEZEE-Grip Film Holder (Snap-A-Ray)
• Stabe Bite-Block (Rinn Corporation)
Copyright 2003, Elsevier Science (USA). All rights reserved.
PID Angulations: Bisecting Technique
In the bisecting technique, the angulation of the
PID is critical.
Angulation is a term used to describe the
alignment of the central ray of the x-ray beam in
the horizontal and vertical planes.
Angulation can be changed by moving the PID in
either a horizontal or vertical direction.
The bisecting angle instruments (BAI) with aiming
rings dictates the proper PID angulation.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Horizontal Angulation
Horizontal angulation refers to the positioning
of the tubehead and direction of the central ray in
a horizontal, or side-to-side, plane.
The horizontal angulation remains the same
whether you are using the paralleling or bisecting
technique.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-22 The arrows indicate movement in a horizontal direction.
Fig. 41-22
Copyright 2003, Elsevier Science (USA). All rights reserved.
Correct Horizontal Angulation
With correct horizontal angulation, the central ray
is directed perpendicular to the curvature of the
arch and through the contact areas of the teeth.
Incorrect horizontal angulation results in
overlapped (unopened) contact areas.
A film with overlapped contact areas cannot be
used to examine the interproximal areas of the
teeth.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-23 Correct horizontal angulation.
Fig. 41-23
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-24 Incorrect horizontal angulation.
Fig. 41-24
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-25 Overlapped contacts.
Fig. 41-25
Copyright 2003, Elsevier Science (USA). All rights reserved.
Vertical Angulation
Vertical angulation refers to the positioning of the PID
in a vertical, or up-and-down, plane.
The vertical angulation differs according to the
radiographic technique being used:
• With the paralleling technique, the vertical angulation
of the central ray is directed perpendicular to the film
and the long axis of the tooth.
• With the bisecting technique, the vertical angulation is
determined by the imaginary bisector; the central ray is
directed perpendicular to the imaginary bisector.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-26 Vertical angulation of the PID.
Fig. 41-26
Copyright 2003, Elsevier Science (USA). All rights reserved.
Correct Vertical Angulation
Correct vertical angulation results in a radiographic
image that is the same length as the tooth.
Incorrect vertical angulation results in an image
that is not the same length as the tooth being
radiographed.
The image appears either longer or shorter:
• Elongated
• Foreshortened
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-27 A, If the vertical angulation is to too steep, the image on the film
is shorter than the actual tooth. B, Foreshortened images.
Fig. 41-27 A & B
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-28 A, If the vertical angulation is to too flat, the image on the film is
longer than the actual tooth. B, Elongated images.
Fig. 41-28 A & B
Copyright 2003, Elsevier Science (USA). All rights reserved.
Film Size and Placement
In the bisection technique, the film is placed close
to the crowns of the teeth to be radiographed and
extends at an angle into the palate or floor of the
mouth.
The film packet should extend beyond the incisal
or occlusal aspect of the teeth by about 1/8 to 1/4
inch.
Film holders for the bisection of the angle
technique, including some with alignment
indicators, are available commercially.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Beam Alignment
The x-ray beam is directed to pass between the contacts
of the teeth being radiographed in the horizontal
dimension, just as it does in the paralleling technique.
The vertical angle, however, must be directed at 90 o to
the imaginary bisecting line.
Too much vertical angulation will produce images that
are foreshortened.
Too little vertical angulation will result in images that are
elongated.
The beam must be centered to avoid cone cutting.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-29 C, D, Maxillary canine exposure.
Fig. 41-29 C & D
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-30 C, D, Maxillary incisor exposure.
Fig. 41-30 C & D
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-31 C, D, Mandibular canine exposure.
Fig. 41-31 C & D
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-32 C, D, Mandibular incisor exposure.
Fig. 41-32 C & D
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-33 A, D, Maxillary premolar exposure.
Fig. 41-33 A & D
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-34 C, D, Maxillary molar exposure.
Fig. 41-34 A & D
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-35 C, D, Mandibular premolar exposure.
Fig. 41-35 A & D
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-36 C&D, Mandibular molar exposure.
Fig. 41-36 A & D
Copyright 2003, Elsevier Science (USA). All rights reserved.
Bite-wing Examinations
A bite-wing radiograph shows the crowns and
interproximal areas of the maxillary and
mandibular teeth and the areas of crestal bone on
one film.
Bite-wing radiographs are used to detect
interproximal caries (tooth decay) and are
particularly useful in detecting early carious lesions
that are not clinically evident.
Bite-wing radiographs are also useful in examining
the crestal bone levels between the teeth.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Basic Principles of the Bite-wing Technique
The film is placed in the mouth parallel to the
crowns of both the upper and lower teeth.
The film is stabilized when the patient bites on the
bite-wing tab or bite-wing film holder.
The central ray of the x-ray beam is directed
through the contacts of the teeth, using a +10˚
vertical angulation.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-37 A +10˚ vertical angulation is used to compensate for the slight bend of the
upper portion of the film and the tilt of the maxillary teeth.
Fig. 41-37
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-38 Bite-wing tab and film-holder.
Fig. 41-38
Copyright 2003, Elsevier Science (USA). All rights reserved.
BWX Film Placement
The film is positioned (with either a bite tab or a
film-holding device) parallel to the crowns of both
upper and lower teeth, and the central ray is
directed perpendicular to the film.
The premolar bite-wing radiograph should
include the distal half of the crowns of the
cuspids, both premolars, and often the first molars
on both the maxillary and mandibular arches.
The molar film should be centered over the
second molars.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-39 Premolar bite-wing. A, Film placement. B, Resultant radiograph.
Fig. 41-39
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-42 The molar-bite-wing. A, Film placement. B, Resultant radiograph.
Fig. 41-42 A, B
Copyright 2003, Elsevier Science (USA). All rights reserved.
The Occlusal Technique
The occlusal technique is used to examine large
areas of the upper or lower jaw.
In the occlusal technique, size-4 intraoral film is
used. The film is so named because the patient
bites, or “occludes,” on the entire film.
In adults, size-4 film is used in the occlusal
examination.
In children, size-2 film can be used.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Basic Principles of the Occlusal Technique
The film is positioned with the white side facing
the arch being exposed.
The film is placed in the mouth between the
occlusal surfaces of the maxillary and mandibular
teeth.
The film is stabilized when the patient gently bites
on the surface of the film.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-44 A, The central ray (CR) is directed at +65˚ to the plane of the film. B,
Relationship of film and position-indicator device. C, Maxillary occlusal radiographic
projection.
Fig. 41-44 A,B,C
Copyright 2003, Elsevier Science (USA). All rights reserved.
Patients with Special Needs
Radiographic examination techniques must often
be modified to accommodate patients with special
needs.
The dental radiographer must be competent in
altering radiographic technique to meet the specific
diagnostic need of the individual patient.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Physical Disabilities
A person with a physical disability may have
problems with vision, hearing, or mobility.
You must make every effort to meet the individual
needs of such patients.
In many cases, a family member or caretaker
accompanies the person with a physical disability
to the dental office.
You can ask the caretaker to assist you with
communicating concerning the physical needs of
the patient.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-45 Wheelchair bound patient receiving x-rays.
Fig. 41-45
Copyright 2003, Elsevier Science (USA). All rights reserved.
Patients With Special Dental Needs
Reasons for radiographs on the edentulous patient:
• To detect the presence of root tips, impacted
teeth, and lesions (cysts, tumors).
• To identify objects embedded in bone.
• To observe the quantity and quality of bone that
is present.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Exposure Techniques for the
Edentulous Patient
The radiographic examination of an edentulous patient
may include a panoramic radiograph, periapical
radiographs, or a combination of occlusal and
periapical radiographs.
Radiographic images must be made in all teeth-bearing
areas of the mouth whether or not teeth are present.
For edentulous patients, either the bisection of the
angle or the paralleling technique may be used.
Because there are no teeth present, the distortion
inherent in the bisecting technique does not interfere
with the diagnostic intrabony conditions.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-46 Mixed occlusal-periapical edentulous survey.
Fig. 41-46
Copyright 2003, Elsevier Science (USA). All rights reserved.
Radiographs for the Pediatric Patient
In children, radiographs are useful for detecting
conditions of the teeth and bones, for showing changes
related to caries and trauma, and for evaluating growth
and development.
Explain the radiographic procedures you are about to
perform in terms that the child can easily understand.
For example, you can refer to the tubehead as a camera,
the lead apron as a coat and the radiograph as a picture.
Exposure factors (milliamperage, kilovoltage, time) must
be reduced because of the smaller size of the pediatric
patient.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 41-47 The XCP instruments can also be used for the pediatric patient,
but the exposure time is reduced.
Fig. 41-47
Copyright 2003, Elsevier Science (USA). All rights reserved.
The Patient Who Gags
To help prevent the gag reflex, you must convey a
confident attitude.
For the patient who has a hypersensitive gag reflex, you
should expose the maxillary molars last.
When you place films in the maxillary posterior, do not slide
them along the palate.
There may be times when you will encounter a patient with
an uncontrollable gag reflex.
When this occurs, you must use extraoral radiographs such
as panoramic or lateral jaw radiographs.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Normal Anatomic Landmarks
To correctly mount dental radiographs, the
dental assistant must be able to recognize the
normal anatomic landmarks on intraoral
radiographs.
Copyright 2003, Elsevier Science (USA). All rights reserved.
Maxillary Anterior Landmarks
Median palatine suture
Incisive foramen
Anterior nasal spine
Nasal septum
Nasal fossa
Copyright 2003, Elsevier Science (USA). All rights reserved.
Landmarks of the Mandible
Genial tubercules
Lingual foramen
Nutrient canals
Mental foramen
Mandibular canal
Coronoid process
Mylohyoid ridge
External oblique ridge
Mental ridge
Copyright 2003, Elsevier Science (USA). All rights reserved.
Tips for Mounting Radiographs
Handle films only by the edges.
Label and date the film mount before mounting the
films.
Include the patient’s full name and date of
exposure and the dentist’s name.
Use clean and dry hands.
Use a definite order for mounting films.
Use the “smile” line to mount bite-wing
radiographs (BWXs).
Copyright 2003, Elsevier Science (USA). All rights reserved.
Radiographs for the Endodontic Patient
It often is difficult to obtain accurate radiographs
during endodontic (root canal) treatment because
of the rubber dam clamp, endodontic instruments,
or filling material extending from the tooth.
The EndoRay II film holder can be used to aid in
positioning the film during this portion of the root
canal procedure.
This holder fits around a rubber dam clamp and
allows space for endodontic instruments and filling
materials to protrude from the tooth.
Copyright 2003, Elsevier Science (USA). All rights reserved.
You might also like
- All On 4Document50 pagesAll On 4Juan Jose Stuven RodriguezNo ratings yet
- Bitewing and Occlusal 2021Document47 pagesBitewing and Occlusal 2021Khadyjah RashidNo ratings yet
- Intraoral Radiographic ExaminationDocument79 pagesIntraoral Radiographic Examinationغلاها عبدوNo ratings yet
- Occlusal RadiografiDocument8 pagesOcclusal RadiografiFatma MahechiNo ratings yet
- Intraoral Radiographic TechniqueDocument29 pagesIntraoral Radiographic Techniqueabdullah aliNo ratings yet
- Periapical RadiographDocument4 pagesPeriapical RadiographAnggreta AuriadiniNo ratings yet
- Intraoral 20radiographic 20technique 20ii 140507115114 Phpapp02Document60 pagesIntraoral 20radiographic 20technique 20ii 140507115114 Phpapp02An AnNo ratings yet
- Intraoral Radiographic Technique IiDocument50 pagesIntraoral Radiographic Technique IiAn AnNo ratings yet
- Kashvee Vashishtha (BDS 3rd Year)Document15 pagesKashvee Vashishtha (BDS 3rd Year)pooja sharmaNo ratings yet
- Radiographic Technique of The BisectrizDocument72 pagesRadiographic Technique of The BisectrizScribdTranslationsNo ratings yet
- Intraoral Projection and Quality Evaluation - Kel 1Document35 pagesIntraoral Projection and Quality Evaluation - Kel 1alzayyanauroraNo ratings yet
- Intraoral Periapical Radiographic Techniques: Second Academic Year DENT214Document116 pagesIntraoral Periapical Radiographic Techniques: Second Academic Year DENT2143bdullah al3yuni100% (1)
- Radiography Bisecting AngleDocument17 pagesRadiography Bisecting Anglerabee_tomehNo ratings yet
- Need of Lntraoral Periapical Radiographs: 5. Post Extraction Radiographs For Root Fragments and Other Co-Lateral DamagesDocument6 pagesNeed of Lntraoral Periapical Radiographs: 5. Post Extraction Radiographs For Root Fragments and Other Co-Lateral DamagesRifky Al ThariqNo ratings yet
- Occlusal RadDocument3 pagesOcclusal RadAhmedFouadNo ratings yet
- Panoramic RadiographyDocument52 pagesPanoramic RadiographyPuspita Wulansari100% (1)
- Chapter 16 - Oral Radiography (Essentials of Dental Assisting)Document96 pagesChapter 16 - Oral Radiography (Essentials of Dental Assisting)mussanteNo ratings yet
- OcclusalDocument10 pagesOcclusalFATIHAH SYAFINAZ BINTI KAMARUL ZAMANNo ratings yet
- DA220 Ch1Document32 pagesDA220 Ch1Anne DavisNo ratings yet
- Successful Panoramic Radiography PDFDocument27 pagesSuccessful Panoramic Radiography PDFDivyanshBansalNo ratings yet
- Intraoral Radiographic Pararel and Bitewing 2015Document54 pagesIntraoral Radiographic Pararel and Bitewing 2015EuginiaNo ratings yet
- Cephalometric SrachaelDocument130 pagesCephalometric Srachaelابو العزNo ratings yet
- Intraoral Radiographic Techniques ǁ: by Dr. WajnaaDocument32 pagesIntraoral Radiographic Techniques ǁ: by Dr. WajnaaALI abd-alamamNo ratings yet
- Cieszynski' Rule of IsometryDocument5 pagesCieszynski' Rule of Isometrynishant_tewari_1No ratings yet
- Intra-Oral Radio Graphs For The Pediatric Dental Patient PedoDocument44 pagesIntra-Oral Radio Graphs For The Pediatric Dental Patient PedoFourthMolar.comNo ratings yet
- Radiology Practical PartDocument75 pagesRadiology Practical PartLisa FUzelieNo ratings yet
- Vertical and Horizontal AngulationDocument7 pagesVertical and Horizontal Angulationjoanadiasalves1234No ratings yet
- 4 Intraoral Radiographic TechniquesDocument35 pages4 Intraoral Radiographic TechniquesDan 04100% (1)
- Canine Dental Radiology - Radiographic Technic, Development, and Anatomy of The TeethDocument9 pagesCanine Dental Radiology - Radiographic Technic, Development, and Anatomy of The TeethFernanda PérezNo ratings yet
- Bitewing RadiographyDocument20 pagesBitewing Radiographyanon_66676758No ratings yet
- Schropp Et Al (2005) Immediate Vs Delayed IJOMI PDFDocument9 pagesSchropp Et Al (2005) Immediate Vs Delayed IJOMI PDFAlla MushkeyNo ratings yet
- Schropp Et Al (2005) Immediate Vs Delayed IJOMIDocument9 pagesSchropp Et Al (2005) Immediate Vs Delayed IJOMIAlla MushkeyNo ratings yet
- Intraoral ProjectionsDocument73 pagesIntraoral ProjectionsrespikNo ratings yet
- Tilted or Parallel Implant Placement inDocument7 pagesTilted or Parallel Implant Placement in朱嘉琪No ratings yet
- Mermigos 11 01Document4 pagesMermigos 11 01Sankurnia HariwijayadiNo ratings yet
- Radiology in Pediatric Dentistry 2Document44 pagesRadiology in Pediatric Dentistry 2Aima Cuba100% (1)
- Bitewing Radiography PDFDocument39 pagesBitewing Radiography PDFMarianaBsvNo ratings yet
- Partial Odontectomy 2007Document7 pagesPartial Odontectomy 2007Yoga ChrisnugrohoNo ratings yet
- Panoramic Imaging & Cone Beam Computed TomographyDocument54 pagesPanoramic Imaging & Cone Beam Computed TomographyMenna KhNo ratings yet
- Radio Graphic Techniques-Bisecting and OcclusalDocument66 pagesRadio Graphic Techniques-Bisecting and OcclusalFourthMolar.comNo ratings yet
- Cephalometric Radiography 101Document48 pagesCephalometric Radiography 101Rabeea KittaniNo ratings yet
- Self Study Bisecting Occlusal RX TechniqueDocument64 pagesSelf Study Bisecting Occlusal RX TechniqueMihnea BuiaNo ratings yet
- RadiologyDocument55 pagesRadiologySuganya MurugaiahNo ratings yet
- Management of Impacted Canine1Document88 pagesManagement of Impacted Canine1Saumya Singh100% (1)
- Lec 8 Cep Halo MetricDocument12 pagesLec 8 Cep Halo MetricHuda AljaderiNo ratings yet
- Endodontic Radiography Lec.18: Al-Mustansiriya University College of Dentistry Endodontics LecturesDocument9 pagesEndodontic Radiography Lec.18: Al-Mustansiriya University College of Dentistry Endodontics Lecturesmariamalobeidi53No ratings yet
- 2005 Laster Width Distraction OsteogenesisDocument7 pages2005 Laster Width Distraction Osteogenesislisal1saNo ratings yet
- Shetye 2017Document7 pagesShetye 2017Evgeniya KocherginaNo ratings yet
- Dental Radiology Related To Pedodontics: Dept. of Pediatric & Preventive DentistryDocument43 pagesDental Radiology Related To Pedodontics: Dept. of Pediatric & Preventive DentistryHebah NawafNo ratings yet
- Extraoral 2018Document14 pagesExtraoral 2018sanyengereNo ratings yet
- Lee2016 Usar EsseDocument9 pagesLee2016 Usar EsseMr OdontologiaNo ratings yet
- 10 1111@edt 12575Document44 pages10 1111@edt 12575gbaez.88No ratings yet
- Intraoral Tech عمليDocument28 pagesIntraoral Tech عمليAbdullah EmadNo ratings yet
- Bisecting and Parelling TechniqueDocument32 pagesBisecting and Parelling TechniqueArka Saha100% (1)
- X-Ray: Oral Radiographic Techniques: - IntraDocument21 pagesX-Ray: Oral Radiographic Techniques: - Intraمحمد عماد علي احمدNo ratings yet
- PanoramikDocument38 pagesPanoramikStephanie Victoria100% (1)
- CH 50Document19 pagesCH 502oclockNo ratings yet
- Impacted Maxillary Canines-A Review. - American Journal of Orthodontics and Dentofacial Orthopedics, 101-159, 1992 PDFDocument13 pagesImpacted Maxillary Canines-A Review. - American Journal of Orthodontics and Dentofacial Orthopedics, 101-159, 1992 PDFPia ContrerasNo ratings yet
- Fundamentals of Oral and Maxillofacial RadiologyFrom EverandFundamentals of Oral and Maxillofacial RadiologyRating: 4 out of 5 stars4/5 (1)
- Manual 2 PDFDocument442 pagesManual 2 PDFSebastian CoraisacaNo ratings yet
- Presentation 2Document5 pagesPresentation 2TechLakeNo ratings yet
- Raising Permit: Office of The Building OfficialDocument2 pagesRaising Permit: Office of The Building OfficialJc JüsäyänNo ratings yet
- Seal Gas FlowDocument2 pagesSeal Gas FlowoluwasolNo ratings yet
- Learning & Teaching MethodologyDocument17 pagesLearning & Teaching MethodologyVaidya Gautham M33% (6)
- Embedded Controlled Drip Irrigation SystemDocument5 pagesEmbedded Controlled Drip Irrigation SystemInternational Journal of Application or Innovation in Engineering & ManagementNo ratings yet
- Missing Women of PartitionDocument30 pagesMissing Women of PartitionSaya Augustin100% (1)
- Coitus ReservatusDocument4 pagesCoitus ReservatusTrà Thanh NguyễnNo ratings yet
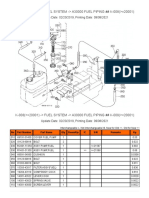
- K-008 ( 20001) - Fuel System - A30000 Fuel Piping ## K-008 ( 20001)Document2 pagesK-008 ( 20001) - Fuel System - A30000 Fuel Piping ## K-008 ( 20001)Martin LindbergNo ratings yet
- Application FormDocument8 pagesApplication FormCrystal KleistNo ratings yet
- Ctu (Zuuu) PDFDocument45 pagesCtu (Zuuu) PDFchang woo yunNo ratings yet
- Combined Cellulitis - FinalDocument78 pagesCombined Cellulitis - Finalsaru_patel0% (1)
- What Are The Expected Tasks You Have Successfully AccomplishedDocument1 pageWhat Are The Expected Tasks You Have Successfully AccomplishedImmortality Realm67% (18)
- Basic Facts About ESOPs2Document20 pagesBasic Facts About ESOPs2Quant TradingNo ratings yet
- Transverse Lie : Predisposing Factors, Maternal and Perinatal OutcomeDocument4 pagesTransverse Lie : Predisposing Factors, Maternal and Perinatal OutcomeErlangga DayudNo ratings yet
- Exercise 4:: Organic Components: CarbohydratesDocument20 pagesExercise 4:: Organic Components: CarbohydratespikachuzingungaNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care Planalexander abasNo ratings yet
- LV Panel ReportDocument71 pagesLV Panel ReportMudassirNo ratings yet
- TirupathiDocument14 pagesTirupathiEkta Adlakha100% (1)
- Interactive Schematic: This Document Is Best Viewed at A Screen Resolution of 1024 X 768Document13 pagesInteractive Schematic: This Document Is Best Viewed at A Screen Resolution of 1024 X 768maquinariakypcon100% (2)
- نموذج ميزانية تدريبDocument2 pagesنموذج ميزانية تدريبعمولةNo ratings yet
- Beer & Wine Osd PresDocument18 pagesBeer & Wine Osd PresAnand100% (1)
- Chemistry Ibdp Exam Syle QuestionsDocument37 pagesChemistry Ibdp Exam Syle QuestionsGEORGE MATTHEWNo ratings yet
- Wastewater Characteristics: Table 7.1.5 Table 7.1.6Document4 pagesWastewater Characteristics: Table 7.1.5 Table 7.1.6Amin EnviroNo ratings yet
- Acquaintance Games: Morning Games Team Building Activity: The Boat Is SinkingDocument3 pagesAcquaintance Games: Morning Games Team Building Activity: The Boat Is SinkingAnonymous iZJv305rNo ratings yet
- The Food Chain Consists of Four Main PartsDocument3 pagesThe Food Chain Consists of Four Main PartskoiaitraazNo ratings yet
- Chapter 2 Lesson 21 Animals That Live On LandDocument17 pagesChapter 2 Lesson 21 Animals That Live On LandRoxan S. Pumphrey0% (1)
- Acute Rheumatic Fever - Clinical Manifestations and Diagnosis - UpToDateDocument15 pagesAcute Rheumatic Fever - Clinical Manifestations and Diagnosis - UpToDateDannyGutierrezNo ratings yet
- B 17Document15 pagesB 17Rochdi SahliNo ratings yet
- Focus Level 3 Table of Contents PDFDocument2 pagesFocus Level 3 Table of Contents PDFDaria KudosLamNo ratings yet