Professional Documents
Culture Documents
Cardiovascular System - Structure of Heart
Cardiovascular System - Structure of Heart
Uploaded by
suresh0 ratings0% found this document useful (0 votes)
3 views66 pagesThe cardiovascular system includes the heart and blood vessels. The heart pumps blood into the blood vessels which circulate blood throughout the body. Blood transports oxygen and nutrients to tissues and removes carbon dioxide and waste. The heart has four chambers and pumps blood through two separate circuits. It is surrounded by membranes and composed of muscle tissue. Valves ensure blood flows in one direction. The actions of the heart include rate, force of contraction, conduction, and excitability which are regulated by nerves and hormones. Blood vessels include arteries, veins, and capillaries that vary in structure depending on their role in the circulatory system.
Original Description:
IT IS USEFULL FOR THE B.PHARM AND PHARM D AND MEDICAL STUDENTS
Original Title
CARDIOVASCULAR SYSTEM --STRUCTURE OF HEART
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe cardiovascular system includes the heart and blood vessels. The heart pumps blood into the blood vessels which circulate blood throughout the body. Blood transports oxygen and nutrients to tissues and removes carbon dioxide and waste. The heart has four chambers and pumps blood through two separate circuits. It is surrounded by membranes and composed of muscle tissue. Valves ensure blood flows in one direction. The actions of the heart include rate, force of contraction, conduction, and excitability which are regulated by nerves and hormones. Blood vessels include arteries, veins, and capillaries that vary in structure depending on their role in the circulatory system.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
3 views66 pagesCardiovascular System - Structure of Heart
Cardiovascular System - Structure of Heart
Uploaded by
sureshThe cardiovascular system includes the heart and blood vessels. The heart pumps blood into the blood vessels which circulate blood throughout the body. Blood transports oxygen and nutrients to tissues and removes carbon dioxide and waste. The heart has four chambers and pumps blood through two separate circuits. It is surrounded by membranes and composed of muscle tissue. Valves ensure blood flows in one direction. The actions of the heart include rate, force of contraction, conduction, and excitability which are regulated by nerves and hormones. Blood vessels include arteries, veins, and capillaries that vary in structure depending on their role in the circulatory system.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 66
CARDIOVASCULAR SYSTEM
SURESH BABU EMANDI M.Pharm
Department of Pharmacognosy
Vikas Institute of Pharmaceutical Sciences
Near Air Port, Rajahmundry, East Godavary Dist.
Andhrapradesh-533102.
Mail ID: emandi2008@gmail.com
8019115247
CARDIOVASCULAR SYSTEM
Cardiovascular system includes heart and blood
vessels.
Heart pumps blood into the blood vessels.
Blood vessels circulate the blood throughout the
body.
Blood transports nutrients and oxygen to the
tissues and removes carbon dioxide and waste
products from the tissues.
HEART
• Heart is a muscular organ
that pumps blood throughout
the circulatory system.
• It is situated in between two lungs in the mediastinum.
• It is made up of four chambers
• Two atria.
• Two ventricles.
• The musculature of ventricles is thicker than that of
atria.
• Force of contraction of heart depends upon the
muscles.
Pumping of blood
RIGHT SIDE OF THE HEART
• Right side of the heart has two chambers,
right atrium and right ventricle.
• Right atrium is a thin walled and low pressure
chamber.
• It has got the pacemaker known as sinoatrial
(SA node that produces cardiac impulses and
atrioventricular (AV) node that conducts the
impulses to the ventricles.
• Right atrium receives venous (deoxygenated)
blood via two large veins.
1. Superior vena cava
• 1. Superior vena cava that returns venous
blood from the head, neck and upper limbs
2. Inferior vena cava
• that returns venous blood from lower parts of the body.
• Right atrium communicates with right ventricle through
tricuspid valve.
• Wall of right ventricle is thick.
• Venous blood from the right atrium enters the right
ventricle through this valve.
• From the right ventricle, pulmonary artery arises.
• It carries the venous blood from right ventricle to lungs.
• In the lungs, the deoxygenated blood is oxygenated.
LEFT SIDE OF THE HEART
• Left side of the heart has two chambers, left
atrium and left ventricle.
• Left atrium is a thin walled and low pressure
chamber.
• It receives oxygenated blood from the lungs
through pulmonary veins.
• This is the only exception in the body, where an
artery carries venous blood and vein carries the
arterial blood.
• Blood from left atrium enters the left ventricle
through mitral valve (bicuspid valve).
• Wall of the left ventricle is very thick.
• Left ventricle pumps the arterial blood to
different parts of the body through systemic
aorta.
SEPTA OF THE HEART
• Right and left atria are separated from one
another by a fibrous septum called interatrial
septum.
• Right and left ventricles are separated from
one another by interventricular septum.
• The upper part of this septum is a
membranous structure, whereas the lower
part of it is muscular in nature
LAYERS OF WALL OF THE HEART
• Heart is made up of three layers of tissues:
• 1. Outer pericardium
• 2. Middle myocardium
• 3. Inner endocardium
PERICARDIUM
• Pericardium is the outer covering of the heart.
It is made up of two layers:
• i. Outer parietal pericardium
• ii. Inner visceral pericardium.
• The space between the two layers is called
pericardial cavity or pericardial space and it
contains a thin film of fluid.
i. Outer Parietal
• Pericardium
• Parietal pericardium forms a strong protective
sac for the heart.
• It helps also to anchor the heart within the
mediastinum.
• Parietal pericardium is made up two layers:
Outer fibrous layer
Inner serous layer.
• Fibrous layer Fibrous layer of the parietal
pericardium is formed by thick fibrous
connective tissue.
• It is attached to the diaphragm and it is
continuous with tunica adventitia (outer wall)
of the blood vessels, entering and leaving the
heart.
• It is attached with diaphragm below. Because
of the fibrous nature, it protects the heart
from over stretching.
Serous layer
• Serous layer is formed by mesothelium,
together with a small amount of connective
tissue.
• Mesothelium contains squamous epithelial
cells which secrete a small amount of fluid,
which lines the pericardial space.
• This fluid prevents friction and allows free
movement of heart within pericardium, when
it contracts and relaxes.
• The total volume of this fluid is only about 25
to 35 mL
i. Inner Visceral Pericardium
• Inner visceral pericardium lines the surface of
myocardium.
• It is made up of flattened epithelial cells.
• This layer is also known as epicardium.
MYOCARDIUM
• Myocardium is the middle layer of wall of the
heart and it is formed by cardiac muscle fibers
or cardiac myocytes.
• Myocardium forms the bulk of the heart and it
is responsible for pumping action of the heart.
• Unlike skeletal muscle fibers, the cardiac
muscle fibers are involuntary in nature.
Myocardium layers
• Myocardium has three types of muscle fibers:
i. Muscle fibers which form contractile unit of heart
ii. Muscle fibers which form pacemaker
iii. Muscle fibers which form conductive system.
ii. Inner Visceral Pericardium
• Inner visceral pericardium lines the surface of
myocardium.
• It is made up of flattened epithelial cells.
• This layer is also known as epicardium.
ENDOCARDIUM
• Endocardium is the inner most layer of heart
wall.
• It is a thin, smooth and glistening membrane.
It is formed by a single layer of endothelial
cells, lining the inner surface of the heart.
• Endocardium continues as endothelium of
the blood vessels.
VALVES OF THE HEART
• There are four valves in human heart. Two
valves are in between atria and the ventricles
called atrioventricular valves.
• Other two are the semilunar valves, placed at
the opening of blood vessels arising from
ventricles, namely systemic aorta and
pulmonary artery.
• Valves of the heart permit the flow of blood
through heart in only one direction.
Valves of the heart
• Atrioventricular
Valves Left
atrioventricular valve
is otherwise known
as mitral valve or
bicuspid valve.
• It is formed by two
valvular cusps or
flaps. Right
atrioventricular valve
is known as tricuspid
valve and it is
formed by three
cusps
• Brim of the atrioventricular valves is attached
to atrioventricular ring, which is the fibrous
connection between the atria and ventricles.
• Cusps of the valves are attached to papillary
muscles by means of chordae tendineae.
• Papillary muscles arise from inner surface of
the ventricles.
• Papillary muscles play an important role in
closure of the cusps and in preventing the
back flow of blood from ventricle to atria
during ventricular contraction. Atrioventricular
valves open only towards ventricles and
prevent the backflow of blood into atria.
Semilunar Valves
• Semilunar valves are present at the openings
of systemic aorta and pulmonary artery and
are known as aortic valve and pulmonary
valve respectively. half moon shape, these two
valves are called semilunar valves.
• Semilunar valves are made up of three flaps.
ACTIONS OF THE HEART
• Actions of the heart are classified into four types:
1. Chronotropic action
2. Inotropic action
3. Dromotropic action
4. Bathmotropic action.
CHRONOTROPIC ACTION
• Chronotropic action is the frequency of heart
beat or heart rate.
• It is of two types:
i. Tachycardia or increase in heart rate
ii. Bradycardia or decrease in heart rate.
DROMOTROPIC ACTION
• Dromotropic action is the conduction of
impulse through heart.
It is of two types:
i.Positive dromotropic action or increase in the
velocity of conduction
ii. Negative dromotropic action or decrease in
the velocity of conduction.
Regulation of Actions of Heart
• All the actions of heart are continuously
regulated.
• It is essential for the heart to cope up with the
needs of the body.
• All the actions are altered by stimulation of
nerves supplying the heart or some hormones
or hormonal substances secreted in the body.
BATHMOTROPIC ACTION
• Bathmotropic action is the excitability of
cardiac muscle.
• It is also of two types:
i. Positive bathmotropic action or increase in the
excitability of cardiac muscle
ii. Negative bathmotropic action or decrease in
the excitability of cardiac muscle.
INOTROPIC ACTION
• Force of contraction of heart is called inotropic
action.
• It is of two types:
• i. Positive inotropic action or increase in the
force of contraction
• ii. Negative inotropic action or decrease in the
force of contraction.
BLOOD VESSELS
• Vessels of circulatory
system are the aorta,
arteries, arterioles,
capillaries, venules,
veins and venae cavae.
• Structural differences
between different
blood.
ARTERIAL SYSTEM
• Arterial system comprises the aorta, arteries
and arterioles.
• Walls of the aorta and arteries are formed by
three layers:
1. Outer tunica adventitia
2. Middle tunica media
3. Inner tunica intima
1. Outer-Tunica adventitia, which is made up of
connective tissue layer.
It is the continuation of fibrous layer of parietal
pericardium
2. Middle- Tunica media, which is formed by
smooth muscles
3. Inner-Tunica intima, which is made up of
endothelium.
It is the continuation of endocardium
• Aorta, arteries and arterioles have two
laminae of elastic tissues:
• i. External elastic lamina between tunica
adventitia and tunica media
• ii. Internal elastic lamina between tunica
media and tunica intima.
• Aorta and arteries have more elastic tissues.
• The arterioles have more smooth muscles.
• Arterial branches become narrower and their
walls become thinner while reaching the
periphery.
• Aorta has got the maximum diameter of about
25 mm.
• Diameter of the arteries is gradually
decreased and at the end arteries.
• It is about 4 mm.
• It further decreases to 30 µ in the arterioles
and ends up with 10 µ in the terminal
arterioles.
Arterioles
• Arterioles are continued
as capillaries, which are
small, thin walled vessels
having a diameter of
about 5 to 8 µ.
• Capillaries are
functionally very
important because, the
exchange of materials
between the blood and
the tissues occurs
through these vessels
VENOUS SYSTEM
• From the capillaries, venous system starts and it
includes venules, veins and venae cavae.
• Capillaries end in venules, which are the smaller
vessels with thin muscular wall than the arterioles.
• Diameter of the venules is about 20 µ.
• At a time, a large quantity of blood is held in
venules and hence the venules are called
capacitance vessels.
• Venules are continued as veins, which have the
diameter of 5 mm.
• Veins form superior and inferior venae cavae,
which have a diameter of about 30 mm.
• Walls of the veins and venae cavae are made
up of inner endothelium, elastic tissues,
smooth muscles and outer connective tissue
layer.
• In the veins and venae cavae, the elastic tissue
is less but the smooth muscle fibers are more.
Structural and dimensional differences between
different blood vessel walls
DIVISIONS OF CIRCULATION
Blood flows through
two divisions of
circulatory system:
1. Systemic
circulation
2. Pulmonary
circulation.
SYSTEMIC CIRCULATION
• Systemic circulation is otherwise known as
greater circulation.
• Blood pumped from left ventricle passes
through a series of blood vessels, arterial
system and reaches the tissues.
• Exchange of various substances between
blood and the tissues occurs at the capillaries..
• After exchange of materials, blood enters the
venous system and returns to right atrium of
the heart.
• From right atrium, blood enters the right
ventricle. Thus, through systemic circulation,
oxygenated blood is supplied from heart to
the tissues and venous blood returns to the
heart from tissues
PULMONARY CIRCULATION
• Pulmonary circulation is otherwise called lesser
circulation.
• Blood is pumped from right ventricle to lungs
through pulmonary artery.
• Exchange of gases occurs between blood and alveoli
of the lungs at pulmonary capillaries.
• Oxygenated blood returns to left atrium through
the pulmonary veins.
• Thus, left side of the heart contains oxygenated or
arterial blood and the right side of the heart
contains deoxygenated or venous blood.
Properties of Cardiac Muscle
• EXCITABILITY
Excitability is defined as the ability of a living
tissue to give response to a stimulus.
In all the tissues, initial response to a stimulus is
electrical activity in the form of action
potential.
It is followed by mechanical activity in the form
of contraction, secretion, etc.
Action Potential
• Action potential in cardiac muscle is different
from that of other tissues such as skeletal
muscle, smooth muscle and nervous tissue.
Duration of the action potential in cardiac
muscle is 250 to 350 msec (0.25 to 0.35 sec).
Phases of action potential
• Action potential in a single cardiac muscle
fiber occurs in four phases:
1. Initial depolarization
2. Initial repolarization
3. A plateau or final depolarization
4. Final repolarization.
1. Initial Depolarization
• Initial depolarization is very rapid and it lasts
for about 2 msec (0.002 sec).
• Amplitude of depolarization is about + 20 mV
2. Initial Repolarization
• Immediately after depolarization, there is an
initial rapid repolarization for a short period of
about 2 msec.
• The end of rapid repolarization is represented
by a notch
3. Plateau or Final Depolarization
• Afterwards, the muscle fiber remains in depolarized
state for sometime before further repolarization.
• It forms the plateau (stable period) in action
potential curve.
• The plateau lasts for about 200 msec in atrial
muscle fibers and for about 300 msec in ventricular
muscle fibers.
• Due to long plateau in action potential, the
contraction time is also longer in cardiac muscle by
5 to 15 times than in skeletal muscle.
4. Final Repolarization
• Final repolarization occurs after the plateau.
• It is a slow process and it lasts for about 50 to
80 msec before the re-establishment of
resting membrane potential.
Cardiac cycle
• Cardiac cycle is defined as the succession of
(sequence of) coordinated events taking place
in the heart during each beat.
• Each heartbeat consists of two major periods
called systole and diastole.
• During systole, heart contracts and pumps the
blood through arteries.
• During diastole, heart relaxes and blood is
filled in the heart.
• All these changes are repeated during every
heartbeat, in a cyclic manner.
EVENTS OF CARDIAC CYCLE
• Events of cardiac cycle are classified into two:
• 1. Atrial events
• 2. Ventricular events.
Cardiac cycle Events
DIVISIONS AND DURATION OF CARDIAC CYCLE
• When the heart beats at a normal rate of
72/minute.
• Duration of each cardiac cycle is about 0.8
second.
ATRIAL EVENTS
• Atrial events are divided into two divisions:
• 1. Atrial systole = 0.11 (0.1) sec
• 2. Atrial diastole = 0.69 (0.7) sec.
VENTRICULAR EVENTS
• Ventricular events are divided into two divisions:
• 1. Ventricular systole = 0.27 (0.3) sec
• 2. Ventricular diastole = 0.53 (0.5) sec
You might also like
- CVS Up To Cardiac Output-1Document198 pagesCVS Up To Cardiac Output-1mokshachapaneriNo ratings yet
- Introduction To CVSDocument24 pagesIntroduction To CVSKjoNo ratings yet
- Circulatory SystemDocument96 pagesCirculatory SystemuzumakiyashNo ratings yet
- Cardiovascular PhysiologyDocument99 pagesCardiovascular Physiologyredhat56964No ratings yet
- Cardiovascular SystemDocument26 pagesCardiovascular SystemGaurav SinghNo ratings yet
- Cardiovascular Physiology For University Students: S. I. Ogungbemi Department of Physiology University of LagosDocument136 pagesCardiovascular Physiology For University Students: S. I. Ogungbemi Department of Physiology University of LagosTeeNo ratings yet
- المحاضرة الثانية عشر - مادة التشريح العام - المرحلة الاولىDocument10 pagesالمحاضرة الثانية عشر - مادة التشريح العام - المرحلة الاولىAbdullah TheNo ratings yet
- Anatomy and Physiology Ii-Dm Cardiovascular Sys-1Document64 pagesAnatomy and Physiology Ii-Dm Cardiovascular Sys-1Mathews showsNo ratings yet
- Cardio NewDocument204 pagesCardio NewHaleema SaadiaNo ratings yet
- 11 The Cardiovascular SystemDocument27 pages11 The Cardiovascular SystemHarshika KDGNo ratings yet
- Lymphatic SystemDocument30 pagesLymphatic SystemWijesiri D WNo ratings yet
- The Cardiovascular To MhsDocument25 pagesThe Cardiovascular To MhsikuwageNo ratings yet
- Cardiovascular System: - HeartDocument58 pagesCardiovascular System: - HeartFaraz AhmedNo ratings yet
- Cardiovascular SystemDocument18 pagesCardiovascular SystemDeep RoyNo ratings yet
- Circulatory Syst Ana 241Document34 pagesCirculatory Syst Ana 241giftabumere54No ratings yet
- Osup TTDocument23 pagesOsup TTKIM EUNHANo ratings yet
- Cardiovascular SystemDocument18 pagesCardiovascular SystemBinta Elsa JohnNo ratings yet
- Cardio 2Document24 pagesCardio 2Myz TogannNo ratings yet
- Cardiovascular System: by DR Saad ZafarDocument154 pagesCardiovascular System: by DR Saad Zafarkhalidtalal8000No ratings yet
- Anaphy HeartDocument8 pagesAnaphy HeartVivien LancinNo ratings yet
- The Cardiovascular SystemDocument57 pagesThe Cardiovascular Systemkrmgxc8p4fNo ratings yet
- Alterations in Oxygenation 1Document15 pagesAlterations in Oxygenation 1alejandrino_leoaugustoNo ratings yet
- Anatomy of Heart: Mr. Binu Babu MBA, M.Sc. (N) Asst. Professor Mrs. Jincy Ealias M.Sc. (N) LecturerDocument71 pagesAnatomy of Heart: Mr. Binu Babu MBA, M.Sc. (N) Asst. Professor Mrs. Jincy Ealias M.Sc. (N) Lecturerjyoti kunduNo ratings yet
- Circulatory SystemDocument67 pagesCirculatory SystemLiswani MuyatwaNo ratings yet
- Grade 7 CH 4.05 The HeartDocument12 pagesGrade 7 CH 4.05 The HeartMunmun AfnanNo ratings yet
- Anatomy and Physiology Ii-Dm Cardiovascular SysDocument43 pagesAnatomy and Physiology Ii-Dm Cardiovascular SysMathews showsNo ratings yet
- Cardiovascular System: Prepared by Samjhana GautamDocument71 pagesCardiovascular System: Prepared by Samjhana GautamSamjhana GautamNo ratings yet
- The Cardiovascular System: A. KabweDocument117 pagesThe Cardiovascular System: A. KabwePeter ChipatelaNo ratings yet
- Sistem Kardio 2022Document51 pagesSistem Kardio 2022Silyas KhanNo ratings yet
- 1 Cardiovascular SystemDocument51 pages1 Cardiovascular SystemChryzl JoyNo ratings yet
- 1.5 Heart & DiseasesDocument9 pages1.5 Heart & DiseasesRayonesh RayanaNo ratings yet
- Null 1Document37 pagesNull 1Esdras DountioNo ratings yet
- Cardiovascular System PDFDocument149 pagesCardiovascular System PDFGayathri SNo ratings yet
- Topic 10. Cardiovascular SystemDocument17 pagesTopic 10. Cardiovascular SystemJanine Jerica JontilanoNo ratings yet
- Cardiovascular System SonDocument36 pagesCardiovascular System SonsmilingjudgeNo ratings yet
- Introduction To Cardiovascular SystemDocument10 pagesIntroduction To Cardiovascular Systemtewogbadeomobuwajo005No ratings yet
- Circulatory System in AnimalsDocument42 pagesCirculatory System in AnimalsAlaina SmithNo ratings yet
- PHA618 Ex 31 Revised PDFDocument20 pagesPHA618 Ex 31 Revised PDFPATRICIA ROSE SORIANONo ratings yet
- Circulatory System:, ,,, and The and That and Through The Body. - ,, andDocument62 pagesCirculatory System:, ,,, and The and That and Through The Body. - ,, andBlister CountNo ratings yet
- Anatomyoftheheart 141215104035 Conversion Gate02Document27 pagesAnatomyoftheheart 141215104035 Conversion Gate02shahera rosdiNo ratings yet
- Circulatory System:, ,,, and The and That and Through The Body. - ,, andDocument62 pagesCirculatory System:, ,,, and The and That and Through The Body. - ,, andBlister Count100% (1)
- Chapter 7. CirculationDocument54 pagesChapter 7. CirculationankurbiologyNo ratings yet
- Mammalian CirculationDocument54 pagesMammalian Circulationron971No ratings yet
- PHS 205 Cardiovascular SystemDocument33 pagesPHS 205 Cardiovascular Systemdivineraymond34No ratings yet
- Cardiovascular SystemDocument77 pagesCardiovascular SystemAyesha100% (1)
- General Anatomy 5.thoracic Cavity (Intro To Cardivascular and Respiratory)Document49 pagesGeneral Anatomy 5.thoracic Cavity (Intro To Cardivascular and Respiratory)amrokhalefa21No ratings yet
- Cardiovascular System (2015 - 06 - 09 22 - 21 - 55 Utc)Document89 pagesCardiovascular System (2015 - 06 - 09 22 - 21 - 55 Utc)DiazNo ratings yet
- Anatomia Del CorazonDocument21 pagesAnatomia Del CorazonAndrea OrtizNo ratings yet
- Unit 4 Word Circulatory SystemDocument26 pagesUnit 4 Word Circulatory SystemChandan Shah100% (2)
- Cardiovascular System Heart ModuleDocument19 pagesCardiovascular System Heart Modulebadodong700No ratings yet
- Cardiovascular System: Shoaib AlamDocument28 pagesCardiovascular System: Shoaib AlamUzma KhanNo ratings yet
- Circulatory SystemDocument15 pagesCirculatory Systemrafaelarmildez02No ratings yet
- Cardiovascular System HistologyDocument58 pagesCardiovascular System HistologyDeniz asmazNo ratings yet
- Anatomy and Physiology Ii SMS 1224: Norhayati Ismail NOV 2011Document50 pagesAnatomy and Physiology Ii SMS 1224: Norhayati Ismail NOV 2011Shirley LourdesNo ratings yet
- Cardiovascular SystemDocument53 pagesCardiovascular SystemPelin OktayNo ratings yet
- Hear Structure NotesDocument27 pagesHear Structure NotesRaifa FathimaNo ratings yet
- Special Cardiobascular SystemDocument24 pagesSpecial Cardiobascular SystemBijay Kumar MahatoNo ratings yet
- Histology of Circulatory SystemDocument156 pagesHistology of Circulatory SystemErmiyas BeletewNo ratings yet
- Kuliah The Heart, Pericardium, and Coronary VesselsDocument62 pagesKuliah The Heart, Pericardium, and Coronary VesselsRafianza AkbarNo ratings yet
- Hai-I SyllabusDocument3 pagesHai-I SyllabussureshNo ratings yet
- Formation of HemoglobinDocument13 pagesFormation of HemoglobinsureshNo ratings yet
- Blood Properties and FunctionsDocument13 pagesBlood Properties and FunctionssureshNo ratings yet
- Blood DisordersDocument10 pagesBlood DisorderssureshNo ratings yet
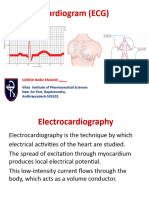
- Ecg or Electro Cardiogram and ElectrocardiographDocument20 pagesEcg or Electro Cardiogram and ElectrocardiographsureshNo ratings yet
- Cardiac CycleDocument24 pagesCardiac CyclesureshNo ratings yet
- BHF CVD Statistics Uk FactsheetDocument21 pagesBHF CVD Statistics Uk FactsheetUme Aimen Hussain Akhtar Year 12No ratings yet
- 4-Pulp Vessels FactoidDocument4 pages4-Pulp Vessels FactoidmoffittajNo ratings yet
- Part4 - CIE IGCSE Biology 9 RN - SampleDocument2 pagesPart4 - CIE IGCSE Biology 9 RN - SampleJun ZheNo ratings yet
- Phosphodiesterase Inhibitors - AMBOSSDocument3 pagesPhosphodiesterase Inhibitors - AMBOSSRuva Oscass JimmyNo ratings yet
- Microsoft Word Cardiac Medications 1231855169882073 2Document1 pageMicrosoft Word Cardiac Medications 1231855169882073 2api-19824701No ratings yet
- Takayasu's ArteritisDocument2 pagesTakayasu's ArteritisJuan Pablo Zuluaga CastañoNo ratings yet
- MyocarditisDocument52 pagesMyocarditis7337man100% (1)
- Abstrak IsicamDocument22 pagesAbstrak IsicambgusjklNo ratings yet
- EmbolismDocument11 pagesEmbolismSubhrajyoti RoyNo ratings yet
- CirculatorySystemSE - Anthony HernandezDocument5 pagesCirculatorySystemSE - Anthony HernandezAnthony Hernandez100% (1)
- Sensus Icvcu 29.06.2022Document2 pagesSensus Icvcu 29.06.2022raka JantungunsNo ratings yet
- Hypertensive CrisisDocument13 pagesHypertensive CrisisJoanna TaylanNo ratings yet
- Main Principles of Varicose Disease Surgical Treatment A. Conservative TherapyDocument3 pagesMain Principles of Varicose Disease Surgical Treatment A. Conservative TherapyManushi HenadeeraNo ratings yet
- Student Exploration: Circulatory SystemDocument6 pagesStudent Exploration: Circulatory SystemAmir SadeghiNo ratings yet
- New Microsoft Word DocumentDocument18 pagesNew Microsoft Word Documentapi-427712934No ratings yet
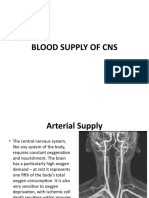
- NEUROANATOMY Lecture # 07 (BLOOD SUPPLY OF CNS)Document26 pagesNEUROANATOMY Lecture # 07 (BLOOD SUPPLY OF CNS)MISS. COMNo ratings yet
- Histology of The Cardiovascular System-t22-HDocument22 pagesHistology of The Cardiovascular System-t22-HSekry EyaNo ratings yet
- Atherosclerosis and ArteriosclerosisDocument50 pagesAtherosclerosis and ArteriosclerosisApril Carter100% (1)
- 2022 The Intensive Care Management of Acute Ischaemic StrokeDocument9 pages2022 The Intensive Care Management of Acute Ischaemic StrokeOmar Alejandro Agudelo ZuluagaNo ratings yet
- Door To Unload: A New Paradigm For The Management of Cardiogenic ShockDocument8 pagesDoor To Unload: A New Paradigm For The Management of Cardiogenic ShockAttilio Del RossoNo ratings yet
- Lab Activity 2 HeartDocument5 pagesLab Activity 2 HeartRaraNo ratings yet
- Rajivgandhi University of Health Sciences, Karnataka: 1. Name of The Candidate and AddressDocument29 pagesRajivgandhi University of Health Sciences, Karnataka: 1. Name of The Candidate and Addresssr.kumariNo ratings yet
- Cerebrovascular AccidentDocument12 pagesCerebrovascular AccidentMarvie JOiz AnteNo ratings yet
- Laporan SP3 LB1 2021 DMDocument1 pageLaporan SP3 LB1 2021 DMfitra rezaNo ratings yet
- CVS Examination PSC2021Document2 pagesCVS Examination PSC2021علي 707No ratings yet
- Ecocardiografia NeonatalDocument10 pagesEcocardiografia NeonatalRonald MHNo ratings yet
- (Board Review Series) Kyung Won Chung - BRS Gross Anatomy (2004, Lippincott Williams - Wilkins) - Libgen - LiDocument17 pages(Board Review Series) Kyung Won Chung - BRS Gross Anatomy (2004, Lippincott Williams - Wilkins) - Libgen - LiSalifyanji SimpambaNo ratings yet
- Question Nbns2213 Hematology and Cardiology NursingDocument11 pagesQuestion Nbns2213 Hematology and Cardiology Nursingdicky chongNo ratings yet
- Chronic Adaptations To Training: Liveitup2Document20 pagesChronic Adaptations To Training: Liveitup2dvenumohanNo ratings yet
- Atherosclerosis and Its Complications-2Document59 pagesAtherosclerosis and Its Complications-2Kelly YeowNo ratings yet