Professional Documents
Culture Documents
Controlling Micriobial Growth
Controlling Micriobial Growth
Uploaded by
asiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Controlling Micriobial Growth
Controlling Micriobial Growth
Uploaded by
asiCopyright:
Available Formats
Burton's Microbiology
for the Health Sciences
Section IV.
Controlling the Growth of Microbes
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Burton's Microbiology
for the Health Sciences
Chapter 8.
Controlling Microbial Growth in Vitro
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Chapter 8 Outline
• Introduction
• Factors that Affect Microbial Growth
• Encouraging the Growth of Microbes in Vitro
• Inhibiting the Growth of Microbes in Vitro
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors That Affect Microbial Growth
• Availability of Nutrients
– All living organisms require nutrients to sustain life.
– Nutrients are energy sources. Organisms obtain
energy by breaking chemical bonds.
• Moisture
– Water is essential for life. It is needed to carry out
normal metabolic processes.
– Certain microbial stages (e.g., bacterial endospores
and protozoal cysts) can survive a drying process
(dessication).
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors That Affect Microbial Growth, cont.
• Temperature
– Every organism has an optimum growth
temperature.
– The temperature (and pH) ranges over which an
organism grows best are largely determined by its
enzymes.
– Thermophiles are microorganisms that grow best at
high temperatures.
– Mesophiles are microbes that grow best at moderate
temperatures (e.g., 37o C).
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors That Affect Microbial Growth, cont.
• Temperature, cont.
– Psychrophiles prefer cold temperatures (like deep
ocean water).
• Psychrotrophs, a particular group of psychrophiles,
prefer refrigerator temperature (4oC).
– Psychroduric organisms prefer warm temperatures,
but can endure very cold or even freezing
temperatures.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors That Affect Microbial Growth, cont.
• pH
– “pH” refers to the acidity or alkalinity of a solution.
– Most microorganisms prefer a neutral or slightly
alkaline growth medium (pH 7.0 - 7.4)
– Acidophiles prefer a pH of 2 to 5
– Alkaliphiles prefer a pH > 8.5
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors That Affect Microbial Growth, cont.
• Osmotic Pressure and Salinity
– Osmotic pressure is the pressure that is exerted on a
cell membrane by solutions both inside and outside
the cell.
– Osmosis is the movement of a solvent, through a
permeable membrane, from a lower concentration of
solutes (dissolved substances) to a higher
concentration of solutes.
– When the concentration of solutes in the external
environment of a cell is greater than that of solutes
inside the cell, the solution in which the cell is
suspended is said to be hypertonic.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors That Affect Microbial Growth, cont.
• Osmotic Pressure and Salinity, cont.
– Plasmolysis is a condition in which the cell membrane
and cytoplasm of a cell shrink away from the cell
wall; occurs when bacteria with rigid cell walls are
placed into a hypertonic solution.
– When the concentration of solutes outside a cell is
less than that of solutes inside a cell, the solution in
which the cell is suspended is said to be hypotonic.
– If a bacterial cell is placed into a hypotonic solution,
it may not burst (because of the rigid cell wall); if it
does burst, the cytoplasm escapes – this process is
known as plasmoptysis.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors That Affect Microbial Growth, cont.
• Osmotic Pressure and Salinity, cont.
– A solution is said to be isotonic when the
concentration of solutes outside a cell equals the
concentration of solutes inside the cell.
– Organisms that prefer to live in salty environments
are called halophilic organisms. Those that do not
prefer to live in salty environments, but which are
capable of surviving there (e.g., Staphylococcus
aureus) are called haloduric organisms.
• Barometric Pressure
– Microbes that can survive in high atmospheric
pressure (> 14.7 psi) are know as piezophiles.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Changes in Osmotic Pressure
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors That Affect Microbial Growth cont.
• Gaseous Atmosphere
– Microorganisms vary with respect to the type of
gaseous atmosphere that they require.
– Obligate aerobes prefer the same atmosphere that
humans do (~20-21% O2 and 78-79% N2, other
gases < 1%).
– Microaerophiles require reduced concentrations of
oxygen (~5% O2).
– Obligate anaerobes are killed by the presence of
oxygen.
– Capnophiles require increased concentrations of CO2
(5-10% CO2).
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Encouraging the Growth of
Microbes in Vitro
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
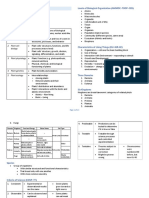
Culturing Bacteria in the Laboratory
Bacterial Growth
• Think of bacterial growth as an increase in the number of
organisms rather than an increase in their size.
• Bacteria divide by binary fission (one cell divides to
become two cells) when they reach their optimum size.
• Binary fission continues through many generations until a
colony is produced on solid culture medium.
• Binary fission continues for as long as there is a sufficient
supply of nutrients, water, and space.
• The time it takes for one cell to become two cells is called
the generation time (e.g., E. coli = 20 minutes).
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Binary fission of
staphylococci.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Culturing Bacteria in the Laboratory
Culture Media
• Media (sing., medium) are used in microbiology labs to
culture (i.e., grow) bacteria; media prepared in the lab
are referred to as artificial media or synthetic media.
• A chemically defined medium is one in which all
ingredients are known.
• Culture media can be liquid or solid.
• An enriched medium is a broth or solid containing a rich
supply of special nutrients that promote the growth of
fastidious organisms; example = chocolate agar.
• A selective medium has added inhibitors that discourage
growth of certain organisms while allowing the growth of
a desired organism; example = PEA agar.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Culturing Bacteria in the Laboratory
Culture Media, cont.
• A differential medium permits the differentiation of
organisms that grow on the medium; example =
MacConkey agar.
• The various categories of media are not mutually
exclusive; e.g., blood agar is enriched and differential.
• Thioglycollate broth (THIO) is a popular liquid medium in
bacteriology labs; it supports the growth of all categories
of bacteria from obligate aerobes to obligate anaerobes.
– How is that possible? There is a concentration
gradient of dissolved oxygen in the tube; organisms
grow only in that part of the broth where the oxygen
concentration meets their needs.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
A Thioglycollate (THIO)
Broth Tube
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Bacterial colonies on S. aureus on mannitol-
MacConkey agar (a salt agar (a selective &
selective & differential differential medium)
medium)
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Colonies of a β-hemolytic Streptococcus
species on a blood agar plate (in this case, the
blood agar is both enriched and differential)
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Culturing Bacteria in the Laboratory
Inoculation of Culture Media
• Culture media are inoculated
with clinical specimens (i.e.,
specimens collected from
patients with a suspected
infectious disease).
• Inoculation involves adding a
portion of a specimen to the
medium.
• Inoculation is accomplished
using a sterile inoculating
loop.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Culturing Bacteria in the Laboratory
Importance of Using “Aseptic Technique”
• Aseptic technique is practiced when it is necessary to
exclude microbes from a particular area (e.g., when
inoculating culture media).
• Unwanted organisms are referred to as contaminants;
the growth medium or plate is said to be contaminated.
• The sterility of the media must be maintained before
inoculation.
– Avoid touching the surface of the agar!
• Inoculating media within a biologic safety cabinet
minimizes contamination and protects the laboratorian.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Culturing Bacteria in the Laboratory
Incubation
• After media are inoculated, they must be placed into an
incubator which will maintain the appropriate
atmosphere, temperature, and moisture level; the
process is known as incubation.
• 3 types of incubators are used in clinical microbiology
laboratories:
– A CO2 incubator (contains 5-10% CO2)
– A non-CO2 incubator (contains room air)
– An anaerobic incubator (the atmosphere is devoid of
oxygen)
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Culturing Bacteria in the Laboratory
Bacterial Population Counts
• Microbiologists sometimes need to know how many
bacteria are present in a particular liquid at a given time
(e.g., to determine bacterial contamination of drinking
water).
– Can determine either the total number of bacterial
cells or the number of viable (living) cells
• A spectrophotometer can be used to determine growth by
measuring the turbidity of the medium.
• A viable plate count is used to determine the number of
viable bacteria in a liquid sample by making serial
dilutions of the liquid and inoculating onto nutrient agar;
after overnight incubation, the number of colonies is
counted.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Culturing Bacteria in the Laboratory
Bacterial Population Growth Curve
• A population growth curve for any particular species of
bacterium may be determined by growing a pure culture
of the organism in a liquid medium at a constant
temperature.
– Samples of the culture are collected at fixed intervals
to determine the number of viable organisms.
– A graph is prepared by plotting the logarithmic
number of viable organisms (on the vertical or Y-
axis) against the incubation time (on the horizontal
or X-axis).
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
A population growth curve of living organisms.
Stationary phase
Death phase
Logarithmic growth phase
Lag phase
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
A Chemostat is used
for continuous
cultures.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Culturing Obligate Intracellular Pathogens
in the Laboratory
• Obligate intracellular pathogens are microbes that can
only survive and multiply within living cells (called host
cells).
• Obligate intracellular pathogens include viruses and 2
groups of Gram-negative bacteria – rickettsias and
chlamydias.
• Culturing these organisms in the laboratory is a
challenge; they must be grown in embryonated chicken
eggs, lab animals, or cell cultures.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Culturing Fungi in the Laboratory
• Fungi (including yeasts, moulds and dimorphic fungi)
grow on and in a variety of solid and liquid culture media.
• There is no single medium that is best for all medically
important fungi.
• Examples of culture media for fungi include brain heart
infusion (BHI) agar, BHI with blood, and Sabouraud
dextrose agar (SDA); due to its low pH, SDA is selective
for fungi.
• Caution must be exercised when culturing fungi – some
are highly infectious!
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Culturing Protozoa in the Laboratory
• Most microbiology laboratories do not culture protozoa;
some research and reference labs do, however.
• Examples of protozoa that can be cultured in vitro are
amebae, Giardia lamblia, Leishmania spp., Toxoplasma
gondii, Trichomonas vaginalis and Trypanosoma cruzi.
• Due to the severity of diseases that they cause, it is of
greatest importance to culture amebae: Acanthamoeba
spp., Balamuthia spp. and Naegleria fowleri.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Inhibiting the Growth of
Microbes in Vitro
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Definition of Terms
• Sterilization is the complete destruction of all microbes,
including cells, spores, and viruses.
– Accomplished by dry heat, autoclaving (steam under
pressure), gas, various chemicals, and certain types
of radiation.
• Disinfection is the destruction or removal of pathogens
from nonliving objects by physical or chemical methods;
pasteurization is an example of a disinfection technique.
– Disinfectants are chemical substances that eliminate
pathogens on inanimate objects.
– Antiseptics are solutions used to disinfect skin and
other living tissues.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Definition of Terms, cont.
• The suffix –cide or –cidal refers to “killing.”
• Germicidal agents, biocidal agents, and microbicidal
agents are chemicals that kill microbes.
• Bactericidal agents are chemicals that specifically kill
bacteria, but not necessarily bacterial endospores.
– Sporicidal agents kill bacterial endospores.
– Fungicidal agents kill fungi, including fungal spores.
– Algicidal agents kill algae.
– Viricidal agents destroy viruses.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Definition of Terms (cont.)
• A microbistatic agent is a drug or chemical that inhibits
growth and reproduction of microbes.
• A bacteriostatic agent is one that specifically inhibits the
metabolism and reproduction of bacteria.
• Lyophilization is a process that combines dehydration
(drying) and freezing. This process is widely used in
industry to preserve foods, antibiotics, microorganisms,
and other biologic materials.
• Sepsis refers to the presence of pathogens in blood or
tissues, whereas asepsis means the absence of
pathogens.
• Antisepsis is the prevention of infection.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Using Physical Methods to Inhibit
Microbial Growth
• Heat
– 2 factors – temperature and time - determine the
effectiveness of heat for sterilization.
– The thermal death point (TDP) of any species is the
lowest temperature that will kill all of the organisms
in a standardized pure culture within a specified time.
• Types of Heat
– Dry heat – e.g., oven, electrical incinerator, or flame
– Moist heat – boiling or use of an autoclave
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Dry Heat Sterilization
Using a Bunsen Using an electrical
burner flame heating device
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Using Physical Methods to Inhibit
Microbial Growth, cont.
• The autoclave
– A large metal pressure cooker that uses steam under
pressure to completely destroy all microbial life.
– Increased pressure raises the temperature above the
temperature of boiling water (above 100oC) and
forces steam into materials being sterilized.
– Autoclaving at a pressure of 15 psi at 121.5oC for 20
minutes destroys vegetative microorganisms,
bacterial endospores, and viruses.
– Can use pressure-sensitive tape or spore strips or
solutions as a quality control measure to ensure
proper autoclaving.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
A large, built-in autoclave.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Pressure-sensitive autoclave tape showing dark
stripes after sterilization.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Biological Indicators for Monitoring the
Effectiveness of Steam Sterilization
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Using Physical Methods to Inhibit
Microbial Growth, cont.
• Cold; most microorganisms are not killed, but their
metabolic activities are slowed.
• Desiccation; many dried microorganisms remain viable,
but they cannot reproduce.
• Radiation; an ultra-violet (UV) lamp is useful for reducing
the number of microbes in the air.
• Ultrasonic waves; used in hospitals and medical and
dental clinics to clean equipment.
• Filters; used to separate cells/microbes from liquids or
gases.
• Gaseous atmosphere; can be altered to inhibit growth.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Using Chemical Agents to Inhibit Microbial
Growth
• Chemical disinfection refers to the use of chemical agents
to inhibit the growth of pathogens, either temporarily or
permanently.
• Disinfectants are affected by:
– Prior cleaning of the object or surface
– The organic load (e.g., feces, blood, pus)
– The bioburden; types and numbers of microbes
– Concentration of the disinfectant
– Contact time
– Physical nature of the object being disinfected
– Temperature and pH
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Using Chemical Agents to Inhibit Microbial
Growth, cont.
Characteristics of an ideal chemical antimicrobial agent:
• Should have a broad • Soluble in water and easy to
antimicrobial spectrum apply
• Fast acting • Inexpensive and easy to
prepare
• Not affected by the presence
of organic matter • Stable as both a concentrate
and a working solution
• Nontoxic to human tissues
and noncorrosive • Odorless
• Should leave a residual
antimicrobial film on surface
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Using Chemical Agents to Inhibit Microbial
Growth (cont.)
• Antiseptics
– May safely be used on human tissues.
– Reduce the number of organisms on the surface of
the skin; do not penetrate pores and hair follicles.
• Antiseptic soaps and scrubbing are used by
healthcare personnel to remove organisms
lodged in pores or folds of the skin.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Inhibiting the Growth of Pathogens in Our
Kitchens (from the CD-ROM)
• Many foods brought into our kitchens are contaminated
with pathogens; examples = E. coli O157:H7, Salmonella
and Campylobacter spp. on poultry and ground beef.
• Problems arise when handling foods before cooking.
• Remain aware of pathogens when preparing foods.
• Wash hands frequently.
• Thoroughly clean plates and counter tops that have had
poultry or meat on them with hot soapy water
• The use of antibacterial kitchen sprays is controversial.
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
Controversies Relating to the Use of
Antimicrobial Agents in Animal Feed and
Household Products
• 40% of the antibiotics manufactured in the U.S. are used
in animal feed; microorganisms resistant to these
antibiotics survive!
– Drug resistant organisms are transmitted in animal
feces and in food products.
– Efforts are underway to eliminate or reduce the
practice of adding antibiotics to animal feed.
• Use of antimicrobial agents is widespread in toys, cutting
boards, in hand soaps, and many other household
products; resistant microorganisms survive!
• Controversy: Should children be exposed to all sorts of
microorganisms for their immune systems to develop
properly?
Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins
You might also like
- Chapter 09 Controlling Microbial Growth in Vivo Using Antimicrobial AgentsDocument49 pagesChapter 09 Controlling Microbial Growth in Vivo Using Antimicrobial AgentsSherinne Jane Cariazo100% (1)
- Week 1 - Burton'S - LWW Introduction To MicrobiologyDocument21 pagesWeek 1 - Burton'S - LWW Introduction To MicrobiologyCathy Lago100% (1)
- Burton's Microbiology For The Health Sciences: Chapter 2. Viewing The Microbial WorldDocument23 pagesBurton's Microbiology For The Health Sciences: Chapter 2. Viewing The Microbial WorldMrkTrstn99No ratings yet
- Chapter 6Document22 pagesChapter 6Marlop CasicasNo ratings yet
- Burton's Microbiology Ch1Document38 pagesBurton's Microbiology Ch1Carl Elexer Cuyugan Ano91% (11)
- CHAPTER 1 Microbial World and YouDocument4 pagesCHAPTER 1 Microbial World and YouAsther MantuaNo ratings yet
- Chapter 1 PPT CRLDocument40 pagesChapter 1 PPT CRLRozel EncarnacionNo ratings yet
- Microbiology As A ScienceDocument41 pagesMicrobiology As A ScienceAlexander DontonNo ratings yet
- Burton's Microbiology For The Health Sciences: Nonspecific Host Defense MechanismsDocument26 pagesBurton's Microbiology For The Health Sciences: Nonspecific Host Defense MechanismsMarlop Casicas100% (1)
- Burton's Microbiology For The Health Sciences: Chapter 10. Microbial Ecology and Microbial BiotechnologyDocument20 pagesBurton's Microbiology For The Health Sciences: Chapter 10. Microbial Ecology and Microbial BiotechnologyKenj PereñaNo ratings yet
- Chapter 7 Microbial Physiology and GeneticsDocument47 pagesChapter 7 Microbial Physiology and GeneticsJhane Kimberly A. RustiaNo ratings yet
- Microbiology For The Health Sciences: Section II. Introduction To MicroorganismsDocument48 pagesMicrobiology For The Health Sciences: Section II. Introduction To MicroorganismsHashim Ghazo100% (1)
- 14 Fungal and Parasitic Infections of Integumentary CNS and Sense OrgansDocument30 pages14 Fungal and Parasitic Infections of Integumentary CNS and Sense OrgansNea Therese AmbidaNo ratings yet
- Burton's Microbiology For The Health Sciences: Section II. Introduction To Microbes and Cellular BiologyDocument41 pagesBurton's Microbiology For The Health Sciences: Section II. Introduction To Microbes and Cellular BiologyAlexander Donton100% (1)
- Micropara Lec Unit 1 LaDocument1 pageMicropara Lec Unit 1 LaGrace HernandezNo ratings yet
- Controlling Microbial Growth in VitroDocument5 pagesControlling Microbial Growth in VitroLady DanielleNo ratings yet
- 1.overview of The Microbial World, Origins andDocument50 pages1.overview of The Microbial World, Origins andSamuel BandaNo ratings yet
- Chapter 4: Microbial Diversity: Part 1: Acelluar and Prokaryotic MicrobesDocument48 pagesChapter 4: Microbial Diversity: Part 1: Acelluar and Prokaryotic MicrobesMudarab AliNo ratings yet
- Prelims Micropara LecDocument14 pagesPrelims Micropara LecBSN1F- JACILDO, KUH KYLA C.No ratings yet
- Microbiology CHapter 1Document66 pagesMicrobiology CHapter 1cj barias100% (4)
- Chapter11Epidemiology and Public Health RevisedDocument45 pagesChapter11Epidemiology and Public Health Revisedbaku narsNo ratings yet
- Lecture - Microbial Diversity The Eukaryotic Microbes - Chapter 4 - BSEDDocument5 pagesLecture - Microbial Diversity The Eukaryotic Microbes - Chapter 4 - BSEDMaden betoNo ratings yet
- 1microbiology PRELIM-merged PDFDocument134 pages1microbiology PRELIM-merged PDFHelping HandsNo ratings yet
- Biochemical ActivitiesDocument9 pagesBiochemical ActivitiesPeter Hong Leong CheahNo ratings yet
- Chapter 6 The Biochemical Basis of LifeDocument54 pagesChapter 6 The Biochemical Basis of LifeJhane Kimberly A. Rustia100% (1)
- MicrobiologyDocument5 pagesMicrobiologyreg speckNo ratings yet
- Pathogenesis and Host Defense Mechanism: Instructor: Bertha Escobar-Poni, MDDocument32 pagesPathogenesis and Host Defense Mechanism: Instructor: Bertha Escobar-Poni, MDGelvia AwaehNo ratings yet
- Biochem Lab Act PrelimDocument20 pagesBiochem Lab Act PrelimcharlesNo ratings yet
- Micro paraDocument7 pagesMicro paraAj MillanNo ratings yet
- Tissues ReviewerDocument5 pagesTissues ReviewerJoannah MarieNo ratings yet
- Anaphy Topic 1Document15 pagesAnaphy Topic 1RAYNE CHLOIE LASTANo ratings yet
- Streak Plate Technique For Isolating BacteriaDocument3 pagesStreak Plate Technique For Isolating BacteriaHimanshu tripathiNo ratings yet
- MICROBIODocument158 pagesMICROBIOJoyce VillanuevaNo ratings yet
- Microbiology and Parasitology Presentation by W KakumuraDocument14 pagesMicrobiology and Parasitology Presentation by W KakumurahamiltonNo ratings yet
- Micropara Lab NotesDocument34 pagesMicropara Lab NotesShyenNo ratings yet
- Micro Zoubi PDFDocument73 pagesMicro Zoubi PDFVims BatchNo ratings yet
- Chapter 10Document5 pagesChapter 10Apryll DarlineNo ratings yet
- Controlling Microbial Growth in VitroDocument30 pagesControlling Microbial Growth in VitroJhon Lapuz100% (1)
- Immunity PDFDocument22 pagesImmunity PDFAlelie HerreraNo ratings yet
- Bacte Lec - Prelim ExamDocument84 pagesBacte Lec - Prelim ExamDanielle Anne LambanNo ratings yet
- Control of Microbial GrowthDocument35 pagesControl of Microbial GrowthVincent ManganaanNo ratings yet
- 5enzymes and Vitamins PDFDocument48 pages5enzymes and Vitamins PDFRomelyn AngelNo ratings yet
- Microbiology For The Health Sciences: Chapter 2. MicrosDocument23 pagesMicrobiology For The Health Sciences: Chapter 2. MicrosHashim Ghazo100% (1)
- Prelims - LectureDocument19 pagesPrelims - LectureKaecee WongNo ratings yet
- Enzyme Classification Nomenclature PDFDocument11 pagesEnzyme Classification Nomenclature PDFramsrivatsan100% (1)
- Topic 6. BASIC CONCEPTS ON LABORATORY BIOSAFETY AND BIOSECURITY PDFDocument6 pagesTopic 6. BASIC CONCEPTS ON LABORATORY BIOSAFETY AND BIOSECURITY PDFSophia GarciaNo ratings yet
- Microbial World: VirusDocument18 pagesMicrobial World: VirusShyenNo ratings yet
- Module 1 - PSTMLSDocument53 pagesModule 1 - PSTMLSArvie Karl NabiNo ratings yet
- 5559 Chapter 12Document36 pages5559 Chapter 12Abdallah Essam Al-ZireeniNo ratings yet
- Drugs For Immune SystemDocument75 pagesDrugs For Immune SystemDhonat FlashNo ratings yet
- Bacteriology PRELIMS PDFDocument225 pagesBacteriology PRELIMS PDFRichell Villacarlos100% (1)
- Bacteriology PDFDocument19 pagesBacteriology PDFDarshana Juvekar0% (1)
- Biochemistry Lec - Prelim TransesDocument20 pagesBiochemistry Lec - Prelim TransesLOUISSE ANNE MONIQUE L. CAYLONo ratings yet
- Virus Structure and ReplicationDocument64 pagesVirus Structure and ReplicationLawrence RemuloNo ratings yet
- Hema Lesson 1Document64 pagesHema Lesson 1fleur harrisonNo ratings yet
- Cilia and Flagella: Structure and Function in EukaryotesDocument10 pagesCilia and Flagella: Structure and Function in EukaryotesEr Purushottam PalNo ratings yet
- Microbiology NotesDocument1 pageMicrobiology NotesGlecy Ann MagnoNo ratings yet
- Principles in Medical Laboratory Science 2Document2 pagesPrinciples in Medical Laboratory Science 2lai cruzNo ratings yet
- A MLS Biochemistry Intro 2020 Lec 1Document25 pagesA MLS Biochemistry Intro 2020 Lec 1نجوي عبدالوهاب100% (1)
- The politics of hunger: Protest, poverty and policy in England, <i>c.</i> 1750–<i>c.</i> 1840From EverandThe politics of hunger: Protest, poverty and policy in England, <i>c.</i> 1750–<i>c.</i> 1840No ratings yet
- Cellular Structure and FunctionDocument4 pagesCellular Structure and Functionsalmasadiq2008No ratings yet
- 7-Drug Delivery Systems 3Document26 pages7-Drug Delivery Systems 3Ibrahim Al ShantiNo ratings yet
- Syaidatul Annisha Sarum - LAB 3 - MOVEMENT THROUGH MEMBRANESDocument4 pagesSyaidatul Annisha Sarum - LAB 3 - MOVEMENT THROUGH MEMBRANESSyaidatulNo ratings yet
- Principles of Irrigation & Water Harvesting TechnologyDocument63 pagesPrinciples of Irrigation & Water Harvesting TechnologyHamud Husein Du'aleNo ratings yet
- Diffusion and Osmosis Worksheet: D O D D DDocument4 pagesDiffusion and Osmosis Worksheet: D O D D DDorothy AtilanoNo ratings yet
- Biology - Principles and Processes - Roberts, Reiss and Monger-1993Document2 pagesBiology - Principles and Processes - Roberts, Reiss and Monger-1993Kannamai PriyaNo ratings yet
- Chapter 7 Membrane Structure and FunctionDocument7 pagesChapter 7 Membrane Structure and FunctionIrish Jem BantolinoNo ratings yet
- Of Cac03: Inhibition Scaling in Reverse Osmosis System by Zinc IonDocument6 pagesOf Cac03: Inhibition Scaling in Reverse Osmosis System by Zinc IondonsombreroNo ratings yet
- BIO LE1 ReviewerDocument13 pagesBIO LE1 ReviewerMark JimenezNo ratings yet
- SCIENCE WorksheetsDocument53 pagesSCIENCE WorksheetsHsje GhaNo ratings yet
- On-Level Cell Transport WebquestDocument3 pagesOn-Level Cell Transport WebquestHaley OsbornNo ratings yet
- AS Biology-SOL Unit 1 Topic 2Document43 pagesAS Biology-SOL Unit 1 Topic 2Israa JaboNo ratings yet
- Expt 1 The Membrane Transport Worksheet and QFRsDocument5 pagesExpt 1 The Membrane Transport Worksheet and QFRsTRISHA KATE MEDINANo ratings yet
- Low Salinity Water FloodingDocument39 pagesLow Salinity Water FloodingSunny Bba100% (1)
- Anatomy & Physiology of CellsDocument53 pagesAnatomy & Physiology of CellsMika ForwardNo ratings yet
- Final Reverse Osmosis Lit ReviewDocument9 pagesFinal Reverse Osmosis Lit ReviewJoycelyn AryeeNo ratings yet
- Lab Report ESE Exp 3Document10 pagesLab Report ESE Exp 3LogaSaeran0% (1)
- Cell Biology: Science Explorer - Cells and HeredityDocument242 pagesCell Biology: Science Explorer - Cells and HeredityZeinab ElkholyNo ratings yet
- Pure Water Production - An Overview ScienceDirecDocument14 pagesPure Water Production - An Overview ScienceDirecoffyNo ratings yet
- Review On Osmotically Controlled Drug Delivery SystemDocument5 pagesReview On Osmotically Controlled Drug Delivery SystemEditor IJTSRDNo ratings yet
- PaintDocument21 pagesPaintPRAVEEN VARMANo ratings yet
- Bab 3 ObjektifDocument11 pagesBab 3 ObjektifNoor Hidayah IbrahimNo ratings yet
- Lesson #7 - Transporting Materials Across CellsDocument37 pagesLesson #7 - Transporting Materials Across CellsMaya AwadNo ratings yet
- Chemical Engineering Journal: Sherub Phuntsho, Soleyman Sahebi, Tahir Majeed, Fezeh Lotfi, Jung Eun Kim, Ho Kyong ShonDocument13 pagesChemical Engineering Journal: Sherub Phuntsho, Soleyman Sahebi, Tahir Majeed, Fezeh Lotfi, Jung Eun Kim, Ho Kyong Shonsaad arabNo ratings yet
- Chapter 1 CELL ORGANELLES AND MACROMOLECULESDocument23 pagesChapter 1 CELL ORGANELLES AND MACROMOLECULESAdelette Delos ReyesNo ratings yet
- Unit 1 Chemistry SASTRA University Water TreatmentDocument6 pagesUnit 1 Chemistry SASTRA University Water Treatmentstar100% (1)
- Lab Case Study Final PaperDocument5 pagesLab Case Study Final Paperapi-308850922No ratings yet
- Lec Activity3 The Cell Structure and Their Functions-1Document4 pagesLec Activity3 The Cell Structure and Their Functions-1Miss VinaNo ratings yet
- Membrane and TransportDocument25 pagesMembrane and TransportHafsa JalisiNo ratings yet
- Fluid, Electrolyte, and Acid-Base BalanceDocument50 pagesFluid, Electrolyte, and Acid-Base BalanceBRI KUNo ratings yet