Professional Documents
Culture Documents
HIV ENT Manifestation
HIV ENT Manifestation
Uploaded by
Ahmad fayaz0 ratings0% found this document useful (0 votes)
3 views33 pagesHIV infects and attacks CD4 T-lymphocytes, leading to immunosuppression. It is transmitted sexually, through blood/needles, or from mother to child. After initial infection, there is a latent asymptomatic period that can last 10+ years before advanced AIDS develops. ENT manifestations include opportunistic infections, cancers like Kaposi's sarcoma, and neurological issues. Diagnosis involves antibody tests and CD4 counts to assess immunosuppression.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentHIV infects and attacks CD4 T-lymphocytes, leading to immunosuppression. It is transmitted sexually, through blood/needles, or from mother to child. After initial infection, there is a latent asymptomatic period that can last 10+ years before advanced AIDS develops. ENT manifestations include opportunistic infections, cancers like Kaposi's sarcoma, and neurological issues. Diagnosis involves antibody tests and CD4 counts to assess immunosuppression.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
3 views33 pagesHIV ENT Manifestation
HIV ENT Manifestation
Uploaded by
Ahmad fayazHIV infects and attacks CD4 T-lymphocytes, leading to immunosuppression. It is transmitted sexually, through blood/needles, or from mother to child. After initial infection, there is a latent asymptomatic period that can last 10+ years before advanced AIDS develops. ENT manifestations include opportunistic infections, cancers like Kaposi's sarcoma, and neurological issues. Diagnosis involves antibody tests and CD4 counts to assess immunosuppression.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 33
HIV Infection/AIDS
and ENT Manifestations
Prepared By: Dr Fayaz Rajabzada
ACQUIRED IMMUNODEFICIENCY
SYNDROME) AIDS)
Acquired immunodeficiency syndrome is caused by
retroviruses.
Those infecting the human beings are of two types:
(i) HIV type I—which is the most common and very pathogenic
(ii) HIV type II—which is less common and less pathogenic.
Once virus enters the body, it attacks T-lymphocytes and other cells which
have CD4 surface marker.
CD4 T-lymphocytes are normally associated with helper-inducer function of
the immune system. With the fall in CD4 lymphocytes below 500 cells/mm3,
(normal 600–1500 cells/mm3), the immune system starts breaking down
with the appearance of opportunistic infections and unusual malignancies,
when it is called AIDS. When CD4-cell count falls below 200 cells/mm3,
death occurs within 2–3 years.
MODES OF TRANSMISSION
1. Sexual contact—homosexual or heterosexual.
2. Use of nonsterile needles, syringes or other
skin-piercing instruments.
3. Blood and blood products.
4. Infected mother to infant—During pregnancy,
during birth, and via breast milk.
High-risk Groups
(i) Heterosexually Promiscuous Individuals
(ii) Homosexuals
(iii)Prostitutes And Truck Drivers
(iv)IV Drug Users
(v) Recipients Of Blood And Blood Products
(Haemophilics, Thalassaemia Patients And
Those Undergoing Dialysis).
(vi)Children Born To Hiv Infected Mothers.
Major hazard to healthcare workers is from
blood and body fluids like amniotic, pleural,
peritoneal or pericardial fluid.
Risk of acquiring infection from the specimens
of urine, stool, saliva, sputum, tears, sweat and
vomitus is negligible unless they are visibly
bloody.
STRUCTURE OF HIV-I VIRION
1. Lipid membrane has two layers.
2. Envelope glycoproteins
(a) Glycoprotein 120 (helps virus to bind to host cell).
(b) Glycoprotein 41 (helps in fusion of viral and cellular membranes).
3. Viral core proteins
(a) Matrix protein p17
(b) Capsid protein p24
(c) Nucleocapsid protein p6, p7
(d) Single-stranded RNA: Two copies
(e) Viral enzymes
(i) Reverse transcriptase
(ii) Integrase
(iii) Protease
LIFE CYCLE OF HIV
1. Virus enters the body of an individual through various
modes of transmission. It binds to CD 4+ receptors situated on the surface of
helper T-cells and macrophages. Such receptors are also present on monocytes,
macrophages and CNS dendritic cells.
2. Fusion of virus to cell membrane allows the viral core to be injected into the
host cell.
3. Reverse transcriptase, an enzyme present in viral core, changes viral RNA to
DNA and the latter migrates to host genome.
4. Viral integrase helps viral DNA to integrate into host’s genome and the latter is
then called a provirus.
5. Provirus directs synthesis of new HIV particles.
6. During RNA transcription, there is also formation of
protein precursors or polyproteins which are cleaved by proteases to form
functional viral proteins. The latter increase the infectivity of the new virus
particles.
COURSE OF DISEASE
1. Initial viraemia. Primary infection with HIV,
first causes viraemia which produces mild
clinical disease like fever, headache, body aches
and pains, macular skin rash and lymph nodes
enlargement. This picture resembles infections
like mononucleosis and subsides in 1–2 weeks.
The virus is then taken up by lymphoid organs
like lymph nodes, tonsils, adenoids and spleen.
Initial plasma viraemia lasts for a few weeks.
COURSE OF DISEASE
2. Latent period. This is the asymptomatic period and may
last for a variable period, on an average 10 years. In up to 5–
10% of cases latent period may be 15 years or more.
They are called long-term survivors or long-term
nonprogressors.
In some cases, about 10%, latent period is short, nearly 3
years. They are called rapid progressors. During this period
no virus is detectable in plasma though it is replicating in the
lymphoid tissue and the CD4 T-helper cell number and
function is deteriorating. Antibody test becomes positive in
2–4 months of infection.
COURSE OF DISEASE
3. Advanced disease. It starts after several
years. The CD4 T-cell count falls below 200
cells/mm3 and patient becomes susceptible to
opportunistic infections. There are clinical signs
and symptoms of AIDS and death may occur
within 2 years.
ENT MANIFESTATIONS OF HIV INFECTION
Three types of lesions are seen:
1. Opportunistic infections
2. Unusual malignancies
3. Neurological disorders
Opportunistic infections
All types of infection can occur―viral, bacterial,
protozoal or mycobacterial. They can involve any
area of ear, nose and throat, head and neck, and
central nervous system.
Unusual malignancies
• Kaposi sarcoma (KS) and lymphomas are common.
KS can involve skin, mucous membranes or viscera.
KS may be seen in the skin of face (nose, ear or
external ear canal), neck or extremities.
• It can also occur in oral, nasal, nasopharyngeal,
oropharyngeal or laryngeal mucosa. KS causes
obstructive symptoms.
• Non-Hodgkin lymphoma can involve nodal and
extranodal sites. Hodgkin lymphoma is less
common.
Neurological disorders
They can be due to primary HIV infection or
opportunistic organisms. Primary HIV infection
of CNS can cause encephalopathy (AIDS
dementia complex), myelopathy, peripheral
neuropathy and cranial nerve involvement,
most often VIIth but occasionally Vth and VIIIth.
1. Ear:
Viral, bacterial or fungal infections which can
involve external, middle or internal ear are:
• Kaposi sarcoma
• Seborrhoeic dermatitis of external canal
• Malignant otitis externa
• Serous otitis media
• Acute otitis media
• Pseudomonas and candida infection of the
external and middle ear
• Mycobacterial infections
• Sensorineural hearing loss—due to viral
infection of auditory nerve or cochlea and
demyelination of CNS
• Herpes zoster
2. Nose and paranasal sinuses
• Herpetic lesions of nose
• Recurrent sinusitis
• Chronic sinus infection
• Fungal sinusitis
• Kaposi sarcoma
• Lymphomas–B cell type
• Burkitt lymphoma
3. Oral cavity and oropharynx
• Candidal infection of oral cavity can be thrush-like,
atrophic or hypertrophic forms of candidiasis. Candida infection also
involves oropharynx, hypopharynx or oesophagus. They cause difficulty and
painful swallowing.
• Herpetic lesions of palate, buccal mucosa, lips or gums.
Such lesion may form large ulcers
• Giant aphthous ulcers
• Adenotonsillar hypertrophy.
• Generalized lymphadenopathy
• Kaposi sarcoma of palate
• Non-Hodgkin lymphoma of tonsil or tongue
• Hairy leukoplakia
• Gingivitis
4. Larynx
• Laryngitis—fungal, viral (herpes simplex,
cytomegalovirus) or tubercular
• Kaposi sarcoma
• Non-Hodgkin lymphoma
5. Salivary Glands
• Parotitis
• Xerostomia (Dry mouth)
• Diffuse Parotid Enlargement
• Lymphoepithelial Cysts Of
Parotid. They Arise From
Parotid Nodes, Often On Both
Sides.
• Kaposi Sarcoma
• Non-hodgkin Lymphoma
6. Neck
• Lymphadenopathy. It could be only a follicular
hyperplasia or due to a disease such as
tuberculosis, histoplasmosis, toxoplasmosis or
non-Hodgkin or Hodgkin lymphoma.
KAPOSI SARCOMA
• It is a multicentric neoplasm which may involve any part of the
skin, mucosa or the viscera.
• There is excessive proliferation of spindle cells of vascular
origin. It is noninvasive and respects the fascial planes.
• In the oral cavity, Kaposi sarcoma is mostly seen in the palate,
but may occur on the tongue or gingiva or on the posterior
wall of the pharynx.
• It appears purplish in colour and may need to be
differentiated from angioma or pyogenic granuloma.
• It can occur at any stage of HIV infection, even in those with
normal CD4 counts.
• Size of the tumour may vary from a few mm to several
centimetres.
• Diagnosis is based on biopsy which may show
proliferation of spindle cells, endothelial cells, extravasation of
red blood cells and haemosiderin-laden macrophages.
• Treatment includes localized radiation, intralesional
vinblastine or cryotherapy. Systemic chemotherapy may be
given in those with multiple lesions.
NON-HODGKIN LYMPHOMA
• HIV patients have high incidence of lymphomas.
• B-cell lymphomas are more common (90%) and many
are due to Epstein–Barr virus.
• Risk of lymphomas increases as disease progresses
generally in patient with CD4+ count less than
200/mm3.
• CNS lymphomas occur in late stages of the disease
while systemic ones can occur early.
• Both nodal and extranodal sites can be involved; the
latter include nose and paranasal sinuses, tonsils,
nasopharynx, tongue, orbit and larynx.
• They also involve gastrointestinal tract, lung and
bone marrow.
• Cervical lymphadenopathy can occur.
• Hodgkin lymphoma is less common.
HAIRY LEUKOPLAKIA
• It is a white, vertically corrugated lesions on the
anterior part of the lateral border of tongue.
• Caused by epstein–barr virus.
• It develops early and gives clue to hiv infection.
• Aids develops in 50% of such patients in 16
months or 80% in 30 months.
• Differential diagnosis includes leukoplakia,
carcinoma in situ, hypertrophic candidiasis or
lichen planus.
• Biopsy should be done to confirm.
DIAGNOSTIC TESTS
• Diagnostic tests are based on identification of
antibodies or viral antigens.
• Antibodies are formed within 3 months (2
weeks–12 weeks) of infection.
1. ELISA test (enzyme-linked immunosorbent
assay). It is a very sensitive test (sensitivity
more than 95.5%).
2. Western blot. It is a confirmatory test and
specific for HIV antibodies.
DIAGNOSTIC TESTS...
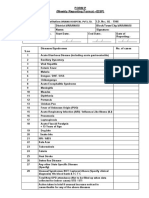
3. CD4 count. Normal count is 600–1500/mm3. Disease has
been classified according to CD4 counts such as
(i) less than 500 cells/mm3;
(ii) 200–499 cells/mm3
(iii) less than 200 cells/mm3; AIDS-defining illnesses appear
when CD4 count fall below 200/mm3.
4. p24 antigen assay. It detects p24 core protein of HIV.
The test is positive even prior to seroconversion. High levels
of p24 antigen are present before development of
antibodies and are useful in those suspected of acute HIV
syndrome.
5. PCR tests. They determine HIV-RNA. Two
important tests are reverse transcriptase PCR
and branched DNA assay. They determine
number of copies of RNA per millilitre of plasma
and indicate viral load.
UNIVERSAL PRECAUTIONS
• Wash hands before and after patient or specimen contact.
• Handle the blood of all patients as potentially infectious.
• Wear gloves for potential contact with blood and body fluids. All sharps like blades, needles,
etc. to be put in impermeable container and destroyed.
• During operation, knife to be passed to the surgeon in a tray.
• Place used syringes immediately in a nearby impermeable container; DO NOT recap, bend or
manipulate needle in anyway!
• Use double gloves where they are likely to be pierced as in fracture surgery. Quality of gloves
is important as many of them may have holes. Impermeable gloves are also available.
• Wear protective eyewear and mask if splatter with blood or body fluids is anticipated (e.g.
bronchoscopy, oral surgery).
• Wear gowns when splash with blood or body fluids is anticipated.
• Handle all linen soiled with blood and/or body secretions as potentially infectious.
• Refrain from patient care if you suffer from exudative or weeping skin lesion or dermatitis.
• Process all laboratory specimens as potentially infectious.
• Wear mask to protect against TB
ANTIRETROVIRAL DRUGS
• There are four major classes of antiretroviral drugs:
1. Nucleoside reverse transcriptase inhibitors (prevent
conversion of RNA to DNA.).
• Zidovudine (AZT)
• Didanosine (ddI)
• Zalcitabine (ddC)
• Stavudine (d4T)
• Lamivudine (3TC)
2. Non-nucleoside reverse transcriptase
inhibitors (prevent conversion of RNA to DNA).
They bind to reverse transcriptase.
• Delavirdine
• Nevirapine
• Efavirenz
• Tenofovir (nucleotide analogue)
3. Protease inhibitors (prevent cleavage of viral
proteins
into their functional forms by binding to viral
protease enzyme.
• Saquinavir
• Ritonavir
• Indinavir
4. Fusion inhibitors (interfere with entry of virus
into target cells). They bind to HIV–gp 41
• Enfuvirtide
NOTE:
Antiretroviral drugs can prevent progression of HIV to
AIDS.
Drug resistance can occur.
Second line drugs are more expensive.
Toxicity of drugs should be kept in mind.
Drug interactions are common and should be avoided.
Combination drug therapy is more effective and
prevents drug resistance; it is the standard of
treatment today to combine two or more drugs.
You might also like
- Epidemiology Exam Questions and AnswersDocument107 pagesEpidemiology Exam Questions and Answersdimitrios80% (35)
- Bandhu Annual Report 2022Document48 pagesBandhu Annual Report 2022somaiya2711No ratings yet
- Skin Manifestations of HIV DiseaseDocument31 pagesSkin Manifestations of HIV Diseaselovelots1234No ratings yet
- Hiv in Ent: Harshitha U S Roll No-97Document36 pagesHiv in Ent: Harshitha U S Roll No-97Harshitha LokeshNo ratings yet
- Hiv AidsDocument9 pagesHiv Aidschuramarak23No ratings yet
- Disorder of The Immune System 2Document58 pagesDisorder of The Immune System 2Daniel OkakaNo ratings yet
- Gulu Cohes Hiv Nelly MDDocument68 pagesGulu Cohes Hiv Nelly MDYIKI ISAACNo ratings yet
- Viral Infections of The Genitourinary TractDocument11 pagesViral Infections of The Genitourinary Tract46nv7gphxzNo ratings yet
- Presented By:-Pallavi Chawla Pallavi Dhiman (BDS - 3 Year)Document28 pagesPresented By:-Pallavi Chawla Pallavi Dhiman (BDS - 3 Year)tinu989No ratings yet
- Human Immunodeficiency Virus (HIV) and Opperortunistic InfectionDocument54 pagesHuman Immunodeficiency Virus (HIV) and Opperortunistic InfectionBikash SahNo ratings yet
- NewDocument75 pagesNewanon_167361167No ratings yet
- HIV 1 Associated Opportunistic Infections StatPearls NCBI BookshelfDocument17 pagesHIV 1 Associated Opportunistic Infections StatPearls NCBI BookshelfAlifah Ummu ZakiyahNo ratings yet
- STD and HYpersensitivityDocument15 pagesSTD and HYpersensitivitygpay98No ratings yet
- HIVDocument79 pagesHIVMehiella SatchiNo ratings yet
- Human Immunodeficency VirusDocument58 pagesHuman Immunodeficency VirusRandy BerryNo ratings yet
- AIDSDocument32 pagesAIDSJuwairia tariqNo ratings yet
- AIDSDocument10 pagesAIDSFaris ShamimNo ratings yet
- Chlamydia by Rosemary C. AgboDocument24 pagesChlamydia by Rosemary C. AgboRosemaryNo ratings yet
- Human Herpes VirusesDocument48 pagesHuman Herpes Virusesfiea241089100% (1)
- Vaccine Preventable DiseaseDocument72 pagesVaccine Preventable Diseasemehdikhalid09No ratings yet
- Microbiology PathologyDocument114 pagesMicrobiology Pathologykhaleelkhamjan100% (1)
- Medicine Lec.9 - Viral Infection IIDocument42 pagesMedicine Lec.9 - Viral Infection II7fefdfbea1No ratings yet
- Complications of HIVDocument60 pagesComplications of HIVgladz25No ratings yet
- Hiv/Aids: by Aisha MansurDocument34 pagesHiv/Aids: by Aisha MansurMpanso Ahmad AlhijjNo ratings yet
- HIV AIDs - FinalDocument99 pagesHIV AIDs - Finalsteven ONo ratings yet
- L10-HIV PathologyDocument13 pagesL10-HIV PathologymokolobetsiNo ratings yet
- DNA VirusesDocument99 pagesDNA VirusesCourtny Lenz Maygay GapaNo ratings yet
- Pertemuan Ke-2 REPRODocument74 pagesPertemuan Ke-2 REPROAbi Surya MandalaNo ratings yet
- Herpes Viruses 2Document36 pagesHerpes Viruses 2الطاهر زروقNo ratings yet
- HIV PresentationDocument19 pagesHIV PresentationpaulNo ratings yet
- Measles: EtiologyDocument14 pagesMeasles: EtiologyHan SANo ratings yet
- Manifestasi Klinis HIVDocument111 pagesManifestasi Klinis HIVFebrina EvaNo ratings yet
- Chapter 13 Viral PathogenesisDocument68 pagesChapter 13 Viral PathogenesisKelly WareNo ratings yet
- AIDS in The PhilippinesDocument29 pagesAIDS in The Philippinesjaninasuzette100% (1)
- Part IIDocument32 pagesPart IITofikNo ratings yet
- Hiv NewDocument85 pagesHiv NewJamil Muqtadir BhattiNo ratings yet
- Human Immunodeficiency Virus AND Acquired Immunodeficiency SyndromeDocument59 pagesHuman Immunodeficiency Virus AND Acquired Immunodeficiency SyndromeJose Joy IdicullaNo ratings yet
- Virology-2 MergedDocument258 pagesVirology-2 MergedLogyn SamNo ratings yet
- Aids HivDocument43 pagesAids Hivjoemarie SalduaNo ratings yet
- HIV Simplified 3Document7 pagesHIV Simplified 3MayAhmedNo ratings yet
- HIV in ENTDocument25 pagesHIV in ENTDeepak KumarNo ratings yet
- 8 - Cutaneous Manifestations of Hiv InfectionDocument10 pages8 - Cutaneous Manifestations of Hiv Infectiondianp_15No ratings yet
- CHAPTER 19sexually Transmitted Infection 1Document50 pagesCHAPTER 19sexually Transmitted Infection 1Nick Martin RequejoNo ratings yet
- HIV Infection / AIDS (Z21, B20-B24)Document37 pagesHIV Infection / AIDS (Z21, B20-B24)Shreya ThackerNo ratings yet
- Hiv 160420091349Document18 pagesHiv 160420091349tharapillaiiNo ratings yet
- Immunology 8Document37 pagesImmunology 8ukashazam19No ratings yet
- IFI Etiology and EpidemiolDocument36 pagesIFI Etiology and EpidemiolJuliusNo ratings yet
- STI Slides EditedDocument43 pagesSTI Slides Editedokureblessing33No ratings yet
- Hiv Aids 1Document23 pagesHiv Aids 1Homed OpriNo ratings yet
- Herpes VirusesDocument26 pagesHerpes VirusesUmar'Farouq OniNo ratings yet
- Viral Infection of The Respiratory SystemDocument18 pagesViral Infection of The Respiratory SystemAbdus SubhanNo ratings yet
- HIV and STIDocument43 pagesHIV and STIFeliza CustadoNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument40 pagesDr. Ali's Uworld Notes For Step 2 CKmarina shawkyNo ratings yet
- Biology Ip XiiDocument8 pagesBiology Ip XiiSugumaran MageshNo ratings yet
- Microbialdiseases 160303140348Document42 pagesMicrobialdiseases 160303140348proud.student2023No ratings yet
- Opportunistic Viral InfectionsDocument40 pagesOpportunistic Viral InfectionsjohndemoNo ratings yet
- Pertemuan Ke-2 REPRODocument74 pagesPertemuan Ke-2 REPROAdi Joyo NegoroNo ratings yet
- Common Childhood Infections For CIDocument89 pagesCommon Childhood Infections For CIBeamlak Getachew WoldeselassieNo ratings yet
- HerpervirusesDocument66 pagesHerperviruseskomalsaharan2001No ratings yet
- NeisseriaDocument32 pagesNeisseriaKeshant SamarooNo ratings yet
- Infection Case 45 - HIV & AIDSDocument2 pagesInfection Case 45 - HIV & AIDSkabal321No ratings yet
- MD LogbookDocument47 pagesMD LogbookAhmad fayazNo ratings yet
- @RastarLib انگیزه انسانیDocument217 pages@RastarLib انگیزه انسانیAhmad fayazNo ratings yet
- Pharyngeal AbscessDocument7 pagesPharyngeal AbscessAhmad fayazNo ratings yet
- Laryngeal CancerDocument11 pagesLaryngeal CancerAhmad fayazNo ratings yet
- Sources For Nelson Mandela History ProjectDocument4 pagesSources For Nelson Mandela History Projectapi-498174875No ratings yet
- Services Provided at Art CentersDocument4 pagesServices Provided at Art Centersprabha krishnanNo ratings yet
- English p5 Mid Term TestDocument7 pagesEnglish p5 Mid Term Testuzabakirihojeanbosco3No ratings yet
- CHN 1 Module 4 Communicable DiseasesDocument23 pagesCHN 1 Module 4 Communicable Diseases202270189No ratings yet
- WAD Report - F4 1Document60 pagesWAD Report - F4 1peter mboleNo ratings yet
- ICASA 2011 Programme BookDocument259 pagesICASA 2011 Programme BookErmias AbelnehNo ratings yet
- Bang Tra Gia Tri Toi HanDocument16 pagesBang Tra Gia Tri Toi HanPhan DiệpNo ratings yet
- Peer Facilitators's Role To Support Pregnant Women in Utilizing HIV Services During The COVID-19 PandemicDocument8 pagesPeer Facilitators's Role To Support Pregnant Women in Utilizing HIV Services During The COVID-19 PandemicIJPHSNo ratings yet
- Ethiopia Consolidated ART Guideline 2014Document165 pagesEthiopia Consolidated ART Guideline 2014TayeNo ratings yet
- Chapter 28 - InfectionsDocument6 pagesChapter 28 - InfectionsEunice CortésNo ratings yet
- Hiv-Aids: Gladys Ziregbe (MRS.)Document25 pagesHiv-Aids: Gladys Ziregbe (MRS.)Esther Anabu EzimaNo ratings yet
- CSYah Tambo 2018 JIPHDocument12 pagesCSYah Tambo 2018 JIPHadhiniNo ratings yet
- HIV - Human Immunodeficiency Virus.: The Greatest Medical Science Challenge of The Last 40 Years!Document37 pagesHIV - Human Immunodeficiency Virus.: The Greatest Medical Science Challenge of The Last 40 Years!blueblemishNo ratings yet
- New Queer Cinema A Critical Reader 0748617248 0748617256 9781474463768 1474463762 - CompressDocument34 pagesNew Queer Cinema A Critical Reader 0748617248 0748617256 9781474463768 1474463762 - Compressimcheng.liuNo ratings yet
- Hiv Infection in PregnancyDocument19 pagesHiv Infection in PregnancyFathima NazarNo ratings yet
- Isaac Ochiengs Revision Series Answers To The Assorted VirologyDocument37 pagesIsaac Ochiengs Revision Series Answers To The Assorted VirologyPowell KitagwaNo ratings yet
- Form P (Weekly Reporting Format - IDSP) : Oriana Hospital PVT - LTDDocument2 pagesForm P (Weekly Reporting Format - IDSP) : Oriana Hospital PVT - LTDRavi ParmarNo ratings yet
- Current Affairs Q&A PDF December 2 2022 by Affairscloud 1Document18 pagesCurrent Affairs Q&A PDF December 2 2022 by Affairscloud 1Krishna AKř ŘaĶiNo ratings yet
- Abstract AnkitaDocument2 pagesAbstract AnkitaAlok BhardwajNo ratings yet
- Recount TextDocument28 pagesRecount Textnur lailyNo ratings yet
- Bio PPT inDocument13 pagesBio PPT inVicky SinghNo ratings yet
- Q3 PPT Health 8 Myths and Misconception of Communicable DiseasesDocument32 pagesQ3 PPT Health 8 Myths and Misconception of Communicable DiseasesJeal Amyrrh CaratiquitNo ratings yet
- The Man Who Sold The Eiffel Tower ExeDocument2 pagesThe Man Who Sold The Eiffel Tower ExeDi LukasNo ratings yet
- Project Design Document - Model Answers-RAG ProjectDocument19 pagesProject Design Document - Model Answers-RAG ProjectGis ThaNo ratings yet
- Retinal Vasculitis DDDocument17 pagesRetinal Vasculitis DDPopuri SandhyaNo ratings yet
- STISTD BrochureDocument2 pagesSTISTD BrochurejoshNo ratings yet
- TB Prev CTRL Program 4.5.2021Document123 pagesTB Prev CTRL Program 4.5.2021JeslineNo ratings yet
- ASEAN Declaration of CommitmentDocument9 pagesASEAN Declaration of CommitmentsitisuhailaidrisNo ratings yet