Professional Documents
Culture Documents
Read 1 CVS Org
Read 1 CVS Org
Uploaded by
Ezeudu Somto0 ratings0% found this document useful (0 votes)
5 views34 pagesThis document provides an overview of the cardiovascular system including its organization, circulation pathways, heart anatomy and function, cardiac muscle properties, conduction system, and nerve supply. Key points include the heart having four chambers that pump blood through two circuits, the properties that allow rhythmic and coordinated heart contraction, and the roles of the sympathetic and parasympathetic nervous systems in regulating heart rate.
Original Description:
Original Title
Read 1 CVS org(1)
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides an overview of the cardiovascular system including its organization, circulation pathways, heart anatomy and function, cardiac muscle properties, conduction system, and nerve supply. Key points include the heart having four chambers that pump blood through two circuits, the properties that allow rhythmic and coordinated heart contraction, and the roles of the sympathetic and parasympathetic nervous systems in regulating heart rate.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
5 views34 pagesRead 1 CVS Org
Read 1 CVS Org
Uploaded by
Ezeudu SomtoThis document provides an overview of the cardiovascular system including its organization, circulation pathways, heart anatomy and function, cardiac muscle properties, conduction system, and nerve supply. Key points include the heart having four chambers that pump blood through two circuits, the properties that allow rhythmic and coordinated heart contraction, and the roles of the sympathetic and parasympathetic nervous systems in regulating heart rate.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 34
PHG 216 / 231
Introductory Cardiovascular and Respiratory
Systems
CARDIOVASCULAR PART
By
Dr. A. A. ADEJARE
Department of Physiology
Faculty of Basic Medical Sciences
College of Medicine of the University of Lagos
Email: aadejare@unilag.edu.ng
Course outline
• Why CVS
• Organization of the cardiovascular system
• Physiological properties of the heart
• Control of heart rate
• Regulation of cardiac output
• Peripheral resistance
• Regulation of arterial blood pressure
• Regional circulation: cerebral, coronary and pulmonary
Why CVS
• Cardiovascular diseases are responsible for most of the morbidities and
mortalities worldwide.
• Hypertension, myocardial infarction, coronary artery diseases are among
the fallouts of our present lifestyles
• There is therefore a need to have good understanding of the physiology of
the heart and blood vessels
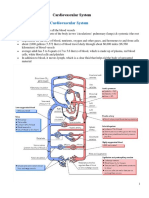
Organization of the cardiovascular system
• The three principal components that make up the circulatory system are the heart,
blood vessels, and the blood itself.
• As reported by the British physiologist William Harvey in 1628, the cardiovascular
system forms a closed loop, so that blood pumped out of the heart through one set
of vessels returns to the heart by a different set.
Systemic and pulmonary circulations
• There are actually two circuits both originating and terminating in the
heart
• The pulmonary circulation includes blood pumped from the right
ventricle through the lungs and then to the left atrium.
• The systemic circulation includes blood pumped from the left
ventricle through all the organs and tissues of the body except the
lungs, and then to the right atrium.
• In both circuits, the vessels carrying blood away from the heart are
called arteries, and those carrying blood from body organs and
tissues back toward the heart are called veins.
• Systemic circuit:
• LV
• aorta
• arteries
• microcirculation (arterioles capillaries venules)
• veins
• IVC and SVC
• RA
• Pulmonary circuit
• RV
• 2 Pulmonary arteries (right and left)
• Lung (right and left)
• Capillaries
• Venules
• 4 Pulmonary veins
• Left atrium
• It must be emphasized that the lungs receive all the blood pumped by the
right side of the heart, whereas each of the peripheral organs and tissues
receives only a fraction of the blood pumped by the left ventricle
Portal system
• Exceptions to the usual anatomical pattern
• Observed in the liver, kidneys, and pituitary,
• blood passes through two capillary beds, arranged in series, before
returning to the heart.
Functional anatomy of the heart
• Enclosed in a fibrous sac of pericardium
• Enclosed by another fibrous membrane of epicardium
• Space between pericardium and epicardium is filled by a lubricant fluid.
• Walls of the heart composed of myocardium
• Inner surface lined by endothelial cells or endothelium
• 4 chambers: 2 atria, 2 ventricles: seperated by atrioventricular valves: right valve
(tricuspid) and left valve (bicuspid/mitral)
• Atrioventricular flow is unidirectional
• Chordae tendinae fastens the valves to papillary muscles to prevent backflow
(prolapse)
• RV opens to pulmonary valve, LV opens to aortic valve (both called semilunar
valves): also for unidirectional flow
• All valves act passively: guided by pressure difference, offers no resistance to
flow
Cardiac muscle
• Cardiac muscle combines properties of both
skeletal and smooth muscle.
• Cardiac myocytes are short branched striated
muscle cells
• Involuntary
• Connected by gap junctions (low resistance
passages) like those in smooth muscles. The
gap junctions make the cells to be electrically
coupled.
• Cardiac myocytes act as a single functional
unit called syncytium (mass of cytoplasm with
numerous nuclei)
• Cardiac muscle cells are considerably
shorter than skeletal muscle fibers.
• They have several branching
processes.
• Adjacent cells are joined end to end
at structures called intercalated
disks (present along the Z-lines of
the sarcomeres), within which are
desmosomes that hold the cells
together and to which the myofibrils
are attached.
• The myocardial fibers are thus
tethered end-to-end for strong
cohesion
Physiological properties of the heart muscle
• Rhythmicity
• Excitability
• Conductivity
• Contractility
Rhythmicity
• Rhythmicity means the ability of the heart to
beat regularly without external stimulation
• It is myogenic in origin, not neurogenic
• The cells of SAN (posterior wall of RA) is the
primary pacemaker of the heart
• The nodal fibres and conducting system are
self-excitable
• SAN 110 bts/min.
• AVN 90
• Bundle of His (A-V bundle) 45
• Purkinje fibres 35
• Ventricular fibres 25
Excitability
• The heart muscle responds to stimuli which may be mechanical, electrical
or chemical
• Refractory Period
• The refractory period of the myocardial fibers is of much longer
duration than that of skeletal muscle fibers and lasts approximately as
long as the cardiac contraction--------- so no continous contraction without
relaxation (tetanus) can occur in heart.
Conductivity
• The ability to conduct impulse from
one cell to another---facilitated by
the presence of gap junctions that
transmit electrical currents
• From SAN→ atrial muscle &
atrioventricular node (AVN)
• From AVN (slowest) →
atrioventricular (AV) bundle (bundle
of His) →left & right bundles
→purkinje fibres (fastest)
Rules controlling contractility
• 1. All or none law
• The cardiac muscle contracts
either maximally or not at all
(under constant conditions)
• The Atria contract as one unit
& the ventricles contract as one
unit
• This is significant for efficient
pumping of the blood
• 2- Staircase or Treppe Phenomenon
• Rapidly Repeated stimulation of the cardiac
muscle produce gradual increase in the strength of
contraction
• The earlier contractions produce better
conditions (heat, less viscosity between muscle
fiber, more Ca) for the following contraction
• 3. Starling Law
• Within limits, the greater the initial length of cardiac muscle fibre
(stretch), the greater the force of contraction
• The initial length is determined by the volume of blood filling
ventricles at end of diastole (end-diastolic volume; EDV)
Fiber types in the cardiac muscle
• Nodal fibers
• Conducting fibers
• Contractile fibers
Cardiac muscle fibers
• Conducting system of the heart (1%) :
do not function in contraction, in
contact with the cardiac muscle cells via
gap junctions
• The conducting system initiates heart
beat
• Causes sequential rhythmic excitation of
the heart
• Helps spread the impulse rapidly
throughout the heart
• Atria cells secrete ANP
Sequence of cardiac excitation
Conducting system of the heart
• Composed of modified cardiac muscle, devoid of
contractile filaments
• SAN (Node of Keith & Flack): located in the
superior posterolateral wall of the right atrium
immediately below and slightly lateral to the
opening of the superior vena cava. contains P cells
that exhibit “pacemaker potential”. have the
capability of self-excitation. Innervated by the
right vagus
• Internodal pathways: SAN is connected to AVN by
1. anterior bundle of Bachmann, the middle bundle
of Wenckebach and the posterior bundle of Thorel
• AVN (Node of Tawara): contains the P cells,
Conducting system of the heart
Bundle of His: the bundle divides into 2. the minor left bundle (Left Bundle
Branch) and the major right bundle (Right Bundle Branch). The LBB
divides into the anterior fascicle and the posterior fascicle.
Purkinje fibers: they originate from the bundle branches. They move nerve
impulses from the Apex to the Base of the heart
Heartbeat Coordination
• The heart is a dual pump in that the left and right
sides of the heart pump blood separately, but
simultaneously, into the systemic and pulmonary
circuits.
• Atria contract first
• Ventricles contract last
• Contraction is triggered by depolarization of CM
that arises from the SAN:
• Gap junctions for easy spread of excitation
• The action potential spreads from the SA node
throughout the atria and then into and throughout
the ventricles.
Sequence of excitation
• SAN remains the pacemaker: determines HR
• Atrial depolarization: SAN to RA to LA: spread indpt of the
conducting system: rapid
• AVN links atrial depolarization with ventricular depolarization
• RA to AVN (the propagation of action potentials through the AV node
is relatively slow (requiring approximately 0.1 s))
• This results in a delay that allows atrial contraction to be completed
before ventricular excitation occurs.
• AVN to AVB (Bundle of His in the
interventricular septum) (the only electrical link
between the atria and the ventricles)
• AVB to Right and Left Bundle branches
• Right and Left Bundle branches to Purkinje
fibers
• Purkinje fibers to Ventricular cells
• Though depolarization and contraction begin
slightly earlier in the bottom (apex) of the
ventricles and spread upward, the result is a
more efficient contraction, like squeezing a tube
of toothpaste from the bottom up.
Nerve supply of the heart
• A) Sympathetic supply: fibers from stellate
ganglion to SAN to AVN to Atria to Ventricles.
Noradrenergic fibers are mainly epicardial
• 1.↑es all cardiac properties
• 2. ↑es the coronary blood flow.
• B) Parasympathetic supply: Right vagus to SAN;
Left vagus to AVN. Vagus innervation is only to
the atria, not to ventricle. Vagal fibers are mainly
endocardial
• 1.↓es all cardiac properties except the ventricles (not
supplied by vagus nerve)
• 2.↓es the coronary blood flow
You might also like
- EKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasFrom EverandEKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasRating: 3 out of 5 stars3/5 (5)
- Sean Burke - Virtual-Shark-Dissection QuestionsDocument5 pagesSean Burke - Virtual-Shark-Dissection Questionsapi-386190429No ratings yet
- Science 9 Teachers' GuideDocument336 pagesScience 9 Teachers' GuideMaragatas Integrated School100% (1)
- Igcse Notes Biology UpdatedDocument8 pagesIgcse Notes Biology UpdatedAlfy YuleNo ratings yet
- Fisiologoia Cardiaca Katz PDFDocument592 pagesFisiologoia Cardiaca Katz PDFMagic_OverNo ratings yet
- Adult Health Section Nclex QuestionsDocument296 pagesAdult Health Section Nclex QuestionsJohn Desir50% (2)
- Cardiovascular Physiology For University Students: S. I. Ogungbemi Department of Physiology University of LagosDocument136 pagesCardiovascular Physiology For University Students: S. I. Ogungbemi Department of Physiology University of LagosTeeNo ratings yet
- Cardiovascular and Circulatory FunctionDocument271 pagesCardiovascular and Circulatory FunctionARAGON GEMMA LYNNo ratings yet
- 1.cardiac Muscle The Heart As A Pump and Function of The Heart Valves 2022Document73 pages1.cardiac Muscle The Heart As A Pump and Function of The Heart Valves 2022Sezanur Taalaibek kyzyNo ratings yet
- Cadiac Cycle, Heart Sound, ECG, HypertensionDocument110 pagesCadiac Cycle, Heart Sound, ECG, HypertensionNilesh100% (1)
- NCM 103-Cardio Anatomy & PhysioDocument56 pagesNCM 103-Cardio Anatomy & Physiolouradel100% (1)
- 8.1 Transport System in MammalsDocument41 pages8.1 Transport System in MammalsTheresa IzaNo ratings yet
- Life's Progression Through Cardiac PhysiologyDocument91 pagesLife's Progression Through Cardiac PhysiologyprofcarleyNo ratings yet
- HeartDocument35 pagesHeartislamicmedia188No ratings yet
- Cardiovascular System: Prepared by Samjhana GautamDocument71 pagesCardiovascular System: Prepared by Samjhana GautamSamjhana GautamNo ratings yet
- Heart Physiology: Nabila Alifah Zahra Perkasa 1610211096Document35 pagesHeart Physiology: Nabila Alifah Zahra Perkasa 1610211096putri avriantiNo ratings yet
- Cardiovascular System: by DR Saad ZafarDocument154 pagesCardiovascular System: by DR Saad Zafarkhalidtalal8000No ratings yet
- The Cardiovascular System: A. KabweDocument117 pagesThe Cardiovascular System: A. KabwePeter ChipatelaNo ratings yet
- Cardiovascular SystemDocument53 pagesCardiovascular SystemPelin OktayNo ratings yet
- 1 Cardiovascular SystemDocument51 pages1 Cardiovascular SystemChryzl JoyNo ratings yet
- Capillary: Nutrients To, and Take Wastes Away From, CellsDocument7 pagesCapillary: Nutrients To, and Take Wastes Away From, CellseyhethNo ratings yet
- 11 The Cardiovascular SystemDocument27 pages11 The Cardiovascular SystemHarshika KDGNo ratings yet
- Cardiovascular Physiology 1Document44 pagesCardiovascular Physiology 1maxmus4No ratings yet
- Cardiac Anatomy and Physiology: Leaugeay Webre BS, CCEMT-P, Nremt-PDocument145 pagesCardiac Anatomy and Physiology: Leaugeay Webre BS, CCEMT-P, Nremt-Pa.abdullah.2005.111No ratings yet
- CVS Physiology of HeartDocument74 pagesCVS Physiology of HeartHEMACHANDRAN G (RA1821002010077)100% (2)
- CARDIOVASCULAR DISORDERS (CVD) OoDocument367 pagesCARDIOVASCULAR DISORDERS (CVD) OoMercy KeruboNo ratings yet
- 1.5 Heart & DiseasesDocument9 pages1.5 Heart & DiseasesRayonesh RayanaNo ratings yet
- AbhiDocument16 pagesAbhiAkash VigneshwarNo ratings yet
- Unit - Ii Cardiovascular InstrumentationDocument125 pagesUnit - Ii Cardiovascular InstrumentationYashaswiniNo ratings yet
- A&p (B&C) Handout 2015Document50 pagesA&p (B&C) Handout 2015Alisa BrownNo ratings yet
- Conducting System of The HeartDocument27 pagesConducting System of The HeartMuhammadNo ratings yet
- The Cardiovascular System: Click To Edit Master Subtitle StyleDocument65 pagesThe Cardiovascular System: Click To Edit Master Subtitle StyleBien EstrellaNo ratings yet
- Cardiac CycleDocument6 pagesCardiac CycleShahina ShayneNo ratings yet
- Anatomi Fisiologi Sistem Kardiovaskuler 1Document52 pagesAnatomi Fisiologi Sistem Kardiovaskuler 1Vaweli Putri Spelman DpNo ratings yet
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocument87 pagesOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreYoAmoNYCNo ratings yet
- Cardiovascular System SonDocument36 pagesCardiovascular System SonsmilingjudgeNo ratings yet
- Cardiac Anatomy, Physiology, and Cardiac Cycle: Ayu Puspita SariDocument42 pagesCardiac Anatomy, Physiology, and Cardiac Cycle: Ayu Puspita SariAyu PuspitaNo ratings yet
- Cardiac Cycle and Myogenic Control of HeartbeatDocument25 pagesCardiac Cycle and Myogenic Control of HeartbeatFiona HennahNo ratings yet
- Cardiology: DR Isaak M Osman MBCHB, Mmed Int. Medicine/Cardiology 10 Sept 2019Document19 pagesCardiology: DR Isaak M Osman MBCHB, Mmed Int. Medicine/Cardiology 10 Sept 2019Imraan MohaNo ratings yet
- Components of The Cardiovascular SystemDocument23 pagesComponents of The Cardiovascular SystemMr. DummyNo ratings yet
- Heart Blood HistoDocument53 pagesHeart Blood HistoAnonymous 52lBinNo ratings yet
- 2 Days Training Module 1Document36 pages2 Days Training Module 1ArumNo ratings yet
- Basic ECG For BeginnersDocument109 pagesBasic ECG For BeginnersEmad Elhussein100% (1)
- Lecture Outline: Cardiovascular PhysiologyDocument146 pagesLecture Outline: Cardiovascular PhysiologyAlyssaNo ratings yet
- Mammalian CirculationDocument54 pagesMammalian Circulationron971No ratings yet
- Lecture 4 Properties of Myocardium and Cardiac Cycle 2020-2021Document43 pagesLecture 4 Properties of Myocardium and Cardiac Cycle 2020-2021badarbhai222No ratings yet
- Riya Arya - 21msc1279 - Biology For ChemistsDocument13 pagesRiya Arya - 21msc1279 - Biology For ChemistsSwadesh SenNo ratings yet
- 05 Cardiovascular System PhysiologyDocument34 pages05 Cardiovascular System PhysiologyKaye Alyssa EnriquezNo ratings yet
- Cardiovascular System - Lecture 3-2018-2019 PDFDocument27 pagesCardiovascular System - Lecture 3-2018-2019 PDFMary100% (1)
- The Circulatory System: The Heart, Blood Vessels, Blood TypesDocument51 pagesThe Circulatory System: The Heart, Blood Vessels, Blood Typescut irnandaNo ratings yet
- Lecture5 - Electrocardiogram Electromyogram - 1Document33 pagesLecture5 - Electrocardiogram Electromyogram - 1AbdullahNo ratings yet
- Unit 4 Cardiovascular System Anatomy and PhysiologyDocument117 pagesUnit 4 Cardiovascular System Anatomy and PhysiologyPetrus Heinrich100% (1)
- The Circulatory System: The Heart, Blood Vessels, Blood TypesDocument51 pagesThe Circulatory System: The Heart, Blood Vessels, Blood Typesghisma ocvintiaNo ratings yet
- لقطة شاشة ٢٠٢٤-٠٥-٠١ في ١٢.٤٠.١٨ مDocument16 pagesلقطة شاشة ٢٠٢٤-٠٥-٠١ في ١٢.٤٠.١٨ مcyc500haedrNo ratings yet
- WK 1& 2 LectureDocument149 pagesWK 1& 2 LectureElma SekikorolevuNo ratings yet
- Cardiovascular System - HeartDocument22 pagesCardiovascular System - HeartZyrick Laurence Eslao TimmangoNo ratings yet
- Cardiovascular PhysiologyDocument42 pagesCardiovascular PhysiologyancillaagraynNo ratings yet
- 2015A&PIntro CardiovascularHandoutDocument16 pages2015A&PIntro CardiovascularHandoutMaggieHameedNo ratings yet
- Cardiovascular Physiology: For HO StudentsDocument77 pagesCardiovascular Physiology: For HO StudentsMengistu GebeyehuNo ratings yet
- Cardiac NursingDocument26 pagesCardiac Nursingjgcriste95% (20)
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!From EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!No ratings yet
- A Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisFrom EverandA Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisRating: 5 out of 5 stars5/5 (1)
- Immediate Life Support for healthcare Practitioners: A Step-By-Step GuideFrom EverandImmediate Life Support for healthcare Practitioners: A Step-By-Step GuideNo ratings yet
- Review Test - Blood and CV SystemDocument11 pagesReview Test - Blood and CV SystemMa Anna Cris LumongsudNo ratings yet
- Circulatory SystemDocument6 pagesCirculatory SystemchelliNo ratings yet
- Respiration, Muscles and The Internal EnvironmentDocument11 pagesRespiration, Muscles and The Internal Environmentmii chanrNo ratings yet
- Adult Echocardiography Protocol 13Document10 pagesAdult Echocardiography Protocol 13api-276847924No ratings yet
- Sample of Exam Questions-2Document6 pagesSample of Exam Questions-2api-3700599100% (5)
- Reocor D S User GuideDocument38 pagesReocor D S User GuideTuchilo ViorelNo ratings yet
- Breathing Is The Process That Brings Oxygen in The Air Into Your Lungs and MovesDocument6 pagesBreathing Is The Process That Brings Oxygen in The Air Into Your Lungs and MovesJaimeCrispinoNo ratings yet
- Central Venous Pressure Monitoring: Assisting With CVP PlacementDocument3 pagesCentral Venous Pressure Monitoring: Assisting With CVP PlacementGlare RhayneNo ratings yet
- Wiggers Diagram SlidesDocument15 pagesWiggers Diagram SlidesKuro ShiroNo ratings yet
- M2F Cardiovascular SystemDocument8 pagesM2F Cardiovascular SystemMeteor 858No ratings yet
- CHAPTER Respiration and CirculationDocument5 pagesCHAPTER Respiration and CirculationlatasabarikNo ratings yet
- Jeopardy Game. CIRCULATORY AND URINARY SYSTEM 2Document52 pagesJeopardy Game. CIRCULATORY AND URINARY SYSTEM 2Ji WasonNo ratings yet
- Chapter 5: Analyzing A Rhythm StripDocument7 pagesChapter 5: Analyzing A Rhythm StriptellyNo ratings yet
- Dr. Md. Rezwanul Hoque: Associate Professor Department of Cardiac Surgery BSMMU, Dhaka, BangladeshDocument48 pagesDr. Md. Rezwanul Hoque: Associate Professor Department of Cardiac Surgery BSMMU, Dhaka, BangladeshRezwanul Hoque Bulbul100% (1)
- Case StudyDocument41 pagesCase StudychaSeph292784100% (6)
- Learning Module For Science 9 First Quarter: Camarines Norte College IncDocument24 pagesLearning Module For Science 9 First Quarter: Camarines Norte College IncCrisanto VelascoNo ratings yet
- WEEK 8 LAB EXERCISE - CVS & Bood VesselsDocument6 pagesWEEK 8 LAB EXERCISE - CVS & Bood VesselsJoselito JardielNo ratings yet
- 1000 Words EssayDocument6 pages1000 Words Essaynhbtoxwhd100% (1)
- NEET 2019 Exam Paper (Odisha) : Contact Number: 9667591930 / 8527521718Document23 pagesNEET 2019 Exam Paper (Odisha) : Contact Number: 9667591930 / 8527521718Suchitra BeniwalNo ratings yet
- Anatomical and Pathophysiological Classification of Congenital Heart DiseaseDocument16 pagesAnatomical and Pathophysiological Classification of Congenital Heart DiseasePietro PensoNo ratings yet
- ? - Pedia MidtermsDocument18 pages? - Pedia Midtermsysabel.mendozaNo ratings yet
- Cardiac L4Document19 pagesCardiac L4Qutaybah JahmanyNo ratings yet
- Cape Biology Unit 2 Circulatory SystemDocument20 pagesCape Biology Unit 2 Circulatory SystemKemoy Francis100% (1)
- 26 Patofisiologi Edema FK Unhas TGL 5 Mei 2015Document65 pages26 Patofisiologi Edema FK Unhas TGL 5 Mei 2015sri ayu lestari wulandariNo ratings yet
- 321 Lecture ECGDocument38 pages321 Lecture ECGCea Mikee Mitch BartolomeNo ratings yet