Professional Documents
Culture Documents
Hepatitis Viruses
Hepatitis Viruses
Uploaded by
ClaraCopyright:
Available Formats
You might also like
- Animal Behavior GoodenoughDocument546 pagesAnimal Behavior GoodenoughDEBALIKA ROYNo ratings yet
- Virology Epidemology DiagnosticsDocument34 pagesVirology Epidemology DiagnosticsEleni HagosNo ratings yet
- Hepatitis VirusDocument83 pagesHepatitis VirusRudresh Shoorashetty ManoharNo ratings yet
- Hepatitis B Dan CDocument59 pagesHepatitis B Dan CNafizah Nurul AidaNo ratings yet
- (TM 2) Hepatitis B Dan CDocument59 pages(TM 2) Hepatitis B Dan CVivi OctaviaNo ratings yet
- Case Study Discussion HIVDocument31 pagesCase Study Discussion HIVAbby LiewNo ratings yet
- Hepatitis B VirusDocument31 pagesHepatitis B VirusFriyoga SyahrilNo ratings yet
- Hepatitis BDocument31 pagesHepatitis Bodakam.harrisNo ratings yet
- L22 - Viral Carcinogenesis-Part 2-S23Document23 pagesL22 - Viral Carcinogenesis-Part 2-S23waNo ratings yet
- Hepadna VirusesDocument30 pagesHepadna Virusesraymondvicent9No ratings yet
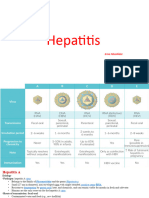
- HepatitisDocument24 pagesHepatitisAnn MariaNo ratings yet
- Seminar ProdiaDocument61 pagesSeminar ProdiaviraNo ratings yet
- Hepatitis B: Prepared By: Mina Zana Nozhin Ahmed Hoshyar Omer Hawkar IsmailDocument19 pagesHepatitis B: Prepared By: Mina Zana Nozhin Ahmed Hoshyar Omer Hawkar Ismailraman saeedNo ratings yet
- Microbiology Lecture - 20 Enterovirus & HepatitisDocument64 pagesMicrobiology Lecture - 20 Enterovirus & HepatitisChris Queiklin100% (1)
- Viral Hepatitis MBBS 2Document41 pagesViral Hepatitis MBBS 2Sohail ShahNo ratings yet
- Viral Hepatitis-Dr. A.M IyagbaDocument62 pagesViral Hepatitis-Dr. A.M IyagbaDr. Amb. Monday ZaccheausNo ratings yet
- Hep BDocument12 pagesHep BGracy PachoriNo ratings yet
- Hep B Group PresentationDocument23 pagesHep B Group PresentationShemiza BalmacoonNo ratings yet
- Hepatitis BDocument14 pagesHepatitis BLoc NguyenNo ratings yet
- DR YousifDocument28 pagesDR YousifAlex SamNo ratings yet
- Class 10 - Hepatitis Viruses: Ann Machablishvili, MD, PHDDocument23 pagesClass 10 - Hepatitis Viruses: Ann Machablishvili, MD, PHDqbcv4shshxNo ratings yet
- CMV & Ebv: A.ChancharoenDocument59 pagesCMV & Ebv: A.ChancharoenRapid MedicineNo ratings yet
- Hiv Hepc PresentationDocument16 pagesHiv Hepc Presentationapi-748224285No ratings yet
- Hepatitis B: Dr. Ruqaiyah NadeemDocument50 pagesHepatitis B: Dr. Ruqaiyah NadeemAulia Rahma NoviastutiNo ratings yet
- Therapeutic Strategies For Hepatitis B Virus Infection - Towards A CureDocument18 pagesTherapeutic Strategies For Hepatitis B Virus Infection - Towards A CureAdriana Villarreal FragaNo ratings yet
- TASH CI HepatitisDocument47 pagesTASH CI HepatitisBeamlak Getachew WoldeselassieNo ratings yet
- Heaptobiliary Disease by Lecturio.Document106 pagesHeaptobiliary Disease by Lecturio.louisegantierNo ratings yet
- Hepatitis BDocument9 pagesHepatitis BDivya DharshiniNo ratings yet
- Human Immunodeficiency Virus (Hiv)Document30 pagesHuman Immunodeficiency Virus (Hiv)Manesa ManeshaNo ratings yet
- VIRAL HEPATITIS IN PREGNANCY Copy 1Document48 pagesVIRAL HEPATITIS IN PREGNANCY Copy 1EndaleNo ratings yet
- Dr. G. Thiruvenkadam Post Graduate Dept of Pediatric & Preventive DentistryDocument31 pagesDr. G. Thiruvenkadam Post Graduate Dept of Pediatric & Preventive Dentistryதிருவேங்கடம் கோபாலன்No ratings yet
- Hepatitis BDocument21 pagesHepatitis Bapi-208983018No ratings yet
- HBV Easl 2017Document57 pagesHBV Easl 2017jessica100% (1)
- Muhammad Asaad Maidin Departement Microbiology Faculty of Medicine Hasanuddin University, MakassarDocument54 pagesMuhammad Asaad Maidin Departement Microbiology Faculty of Medicine Hasanuddin University, MakassarPratiwi PurnamaNo ratings yet
- Hepatitis VirusesDocument23 pagesHepatitis Viruses4jzbxz64kqNo ratings yet
- Viral Pathogenesis and Control of Viral DiseasesDocument55 pagesViral Pathogenesis and Control of Viral DiseasesSuresh KrishnaniNo ratings yet
- Elgouhari HM. Hepatitis B A Strategy For Evaluation and Management. 2009Document10 pagesElgouhari HM. Hepatitis B A Strategy For Evaluation and Management. 2009Revalitha PutriNo ratings yet
- CH 17Document10 pagesCH 17hannahbassett01No ratings yet
- Transfusion Transmitted InfectionDocument42 pagesTransfusion Transmitted InfectionNatalie JuntadoNo ratings yet
- Human Immunodeficiency VirusDocument26 pagesHuman Immunodeficiency ViruspraneethasruthiNo ratings yet
- Hepatitis CCRN KFSH&RC Asma AlshehriDocument33 pagesHepatitis CCRN KFSH&RC Asma AlshehriasmashNo ratings yet
- Summary of Virology & ImmunologyDocument19 pagesSummary of Virology & ImmunologyElaf NaifNo ratings yet
- Viral HepatitisDocument51 pagesViral HepatitisIlmiah BagusNo ratings yet
- Finals For Med SurgDocument11 pagesFinals For Med SurgAyessa CortesNo ratings yet
- AntiviralsDocument6 pagesAntiviralsNur NajminaNo ratings yet
- Hepato-Billiary Diseases: Tutor: DR SocdaalDocument32 pagesHepato-Billiary Diseases: Tutor: DR SocdaalOmar mohamedNo ratings yet
- UNIT 4 - New Challenges: Urja JoshiDocument72 pagesUNIT 4 - New Challenges: Urja JoshiRadhey RavalNo ratings yet
- Diagnosis and Treatment of Chronic Hepatitis B: Raymond D'Souza Graham R FosterDocument4 pagesDiagnosis and Treatment of Chronic Hepatitis B: Raymond D'Souza Graham R FosterrayNo ratings yet
- Cardiovascular System VirologyDocument18 pagesCardiovascular System Virology46nv7gphxzNo ratings yet
- Case StudyDocument54 pagesCase StudysHaYnEsEy100% (1)
- Hepatitis VirusesDocument19 pagesHepatitis VirusesFort SalvadorNo ratings yet
- HBV GP PerspectiveDocument42 pagesHBV GP PerspectivePankaj IngleNo ratings yet
- Viral Hepatitis Training Manual: Federal Ministry of Health National Hepatitis Control Program 2017Document15 pagesViral Hepatitis Training Manual: Federal Ministry of Health National Hepatitis Control Program 2017Eleni HagosNo ratings yet
- Hepatitis 4th prof[1]Document15 pagesHepatitis 4th prof[1]Muhammad IkramNo ratings yet
- 1010 M Balm - Viral HepatitisDocument17 pages1010 M Balm - Viral HepatitisSaad KhanNo ratings yet
- Application Syllabus Gene TherapyDocument4 pagesApplication Syllabus Gene Therapyngyj_flashNo ratings yet
- Viral Hepatitis PC II 2023Document76 pagesViral Hepatitis PC II 2023Suhayb CumarNo ratings yet
- Presentation of AIDSDocument16 pagesPresentation of AIDSZainab AbdullahiNo ratings yet
- Chapter 5.2 - HBV and Liver Cancer - Compatibility ModeDocument9 pagesChapter 5.2 - HBV and Liver Cancer - Compatibility Modenhan le thi thanhNo ratings yet
- Hepatitis A GDocument23 pagesHepatitis A Gapi-3712326No ratings yet
- Hepatitis B Virus and Liver DiseaseFrom EverandHepatitis B Virus and Liver DiseaseJia-Horng KaoNo ratings yet
- Cell & Tissue Engineering Strategies - Development & Replacement of Musculoskeletal TissuesDocument7 pagesCell & Tissue Engineering Strategies - Development & Replacement of Musculoskeletal TissuesClaraNo ratings yet
- BoneDocument18 pagesBoneClaraNo ratings yet
- Skeletal MuscleDocument8 pagesSkeletal MuscleClaraNo ratings yet
- Metabolism - LipidDocument2 pagesMetabolism - LipidClaraNo ratings yet
- Jimin - Lesson12B (J)Document1 pageJimin - Lesson12B (J)ClaraNo ratings yet
- Tendon & LigamentDocument11 pagesTendon & LigamentClaraNo ratings yet
- CartilageDocument16 pagesCartilageClaraNo ratings yet
- Jimin - Lesson67P (J)Document2 pagesJimin - Lesson67P (J)ClaraNo ratings yet
- Jimin - Lesson19.3C (J)Document1 pageJimin - Lesson19.3C (J)ClaraNo ratings yet
- Prokaryotes & EukaryotesDocument8 pagesProkaryotes & EukaryotesClaraNo ratings yet
- Jimin - Lesson50.2P (J)Document6 pagesJimin - Lesson50.2P (J)ClaraNo ratings yet
- Metabolism - Nucleic AcidDocument2 pagesMetabolism - Nucleic AcidClaraNo ratings yet
- Jimin - Lesson15.2C (J)Document1 pageJimin - Lesson15.2C (J)ClaraNo ratings yet
- Jimin - Lesson10P (J)Document10 pagesJimin - Lesson10P (J)ClaraNo ratings yet
- Metabolism - CarbohydrateDocument5 pagesMetabolism - CarbohydrateClaraNo ratings yet
- Jimin - Lesson14.2B (J)Document1 pageJimin - Lesson14.2B (J)ClaraNo ratings yet
- DNA To CellsDocument4 pagesDNA To CellsClaraNo ratings yet
- Lipids, Membranes, TransportDocument9 pagesLipids, Membranes, TransportClaraNo ratings yet
- Metabolism - Amino AcidsDocument2 pagesMetabolism - Amino AcidsClaraNo ratings yet
- Cells & TissuesDocument17 pagesCells & TissuesClaraNo ratings yet
- Cell DivisionDocument5 pagesCell DivisionClaraNo ratings yet
- Genetics & Inheritance - QuestionsDocument10 pagesGenetics & Inheritance - QuestionsClaraNo ratings yet
- DNA Structure & Replication + RNADocument8 pagesDNA Structure & Replication + RNAClaraNo ratings yet
- Cell TraffickingDocument7 pagesCell TraffickingClaraNo ratings yet
- Cell SignallingDocument7 pagesCell SignallingClaraNo ratings yet
- Cellular Compartments & EnvironmentsDocument5 pagesCellular Compartments & EnvironmentsClaraNo ratings yet
- Cell Adaptation - DefenceDocument8 pagesCell Adaptation - DefenceClaraNo ratings yet
- CarbohydrateDocument6 pagesCarbohydrateClaraNo ratings yet
- ATP & Energy MetabolismDocument3 pagesATP & Energy MetabolismClaraNo ratings yet
- Transcriptional & Chromatin RegulationDocument11 pagesTranscriptional & Chromatin RegulationClaraNo ratings yet
- Seminar: Wen-Juei Jeng, George V Papatheodoridis, Anna S F LokDocument14 pagesSeminar: Wen-Juei Jeng, George V Papatheodoridis, Anna S F LokCristian AGNo ratings yet
- Questions From The Section On General and Special VirologyDocument21 pagesQuestions From The Section On General and Special VirologytiffylolaNo ratings yet
- Full Ebook of Edrolo Vce Biology Units 3 4 2Nd Edition Adam Craig Online PDF All ChapterDocument69 pagesFull Ebook of Edrolo Vce Biology Units 3 4 2Nd Edition Adam Craig Online PDF All Chapteramandilavfndfr16100% (4)
- Biology Syllabus GR11-12 (2022-2023)Document37 pagesBiology Syllabus GR11-12 (2022-2023)Amal HassanNo ratings yet
- Effect of Increased Uv On Melanin Production in AnimalsDocument2 pagesEffect of Increased Uv On Melanin Production in Animalsapi-371487254No ratings yet
- Class 11th Zoology Syllabi 1Document1 pageClass 11th Zoology Syllabi 1Zaid KumarNo ratings yet
- General Biology QuizwithanswerkeyDocument3 pagesGeneral Biology QuizwithanswerkeyQueng ElediaNo ratings yet
- Lecture Set 5Document32 pagesLecture Set 5Dirt KickNo ratings yet
- Buku GelatinDocument129 pagesBuku GelatinAwan MegantoroNo ratings yet
- Chemical Classification of HormonesDocument65 pagesChemical Classification of HormonesetNo ratings yet
- Transcription Factor - WikipediaDocument112 pagesTranscription Factor - WikipediaBaikuntha SabarNo ratings yet
- MediUnite Journal Monthly Magasine Vital - April 2024Document21 pagesMediUnite Journal Monthly Magasine Vital - April 2024MediUnite JournalNo ratings yet
- 22 PhysochlainaDocument11 pages22 PhysochlainasaleemNo ratings yet
- Torres Guzmán Moncayo Year 8Document18 pagesTorres Guzmán Moncayo Year 8John OsborneNo ratings yet
- Linkage Disequilibrium: Brenner's Encyclopedia of Genetics (Second Edition)Document6 pagesLinkage Disequilibrium: Brenner's Encyclopedia of Genetics (Second Edition)BobNo ratings yet
- Chapter 4: Amino Acids: MatchingDocument11 pagesChapter 4: Amino Acids: MatchingeliNo ratings yet
- Bethany Christian School of Tarlac Inc.: Before Each NumberDocument1 pageBethany Christian School of Tarlac Inc.: Before Each NumberHezron DamasoNo ratings yet
- Cells Study Guide 2020 KEYDocument4 pagesCells Study Guide 2020 KEYLaarni GeeNo ratings yet
- EchinoideaDocument35 pagesEchinoideaEvika Fatmala DeviNo ratings yet
- Haploid Production and Its ApplicationsDocument16 pagesHaploid Production and Its ApplicationsNikita JainNo ratings yet
- Application of Zoology NoteDocument32 pagesApplication of Zoology NoteShivam GuptaNo ratings yet
- 2021 BPDocument24 pages2021 BPErlita SaputriNo ratings yet
- Excretion in Humans (13.1.1) CIE IGCSE Biology Revision Notes 2023 Save My ExamsDocument1 pageExcretion in Humans (13.1.1) CIE IGCSE Biology Revision Notes 2023 Save My ExamslulogaspariNo ratings yet
- Dopamine Receptors: GlossaryDocument5 pagesDopamine Receptors: Glossarytirasi1214No ratings yet
- Glimmers of Hope For Targeting Oncogenic KRAS-G12D: Cancer Gene TherapyDocument3 pagesGlimmers of Hope For Targeting Oncogenic KRAS-G12D: Cancer Gene Therapychato law officeNo ratings yet
- Color Atlas of Diagnostic MicrobiologyDocument223 pagesColor Atlas of Diagnostic MicrobiologyOana Herea100% (2)
- Acs Analchem 0c04608Document9 pagesAcs Analchem 0c04608abhishek112934No ratings yet
- Biological ClassificationDocument35 pagesBiological Classificationsanjeevani rawatNo ratings yet
- My Answer in Our LaboratoryDocument4 pagesMy Answer in Our LaboratoryKris Marie DelaCruz DomingoNo ratings yet
Hepatitis Viruses
Hepatitis Viruses
Uploaded by
ClaraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hepatitis Viruses
Hepatitis Viruses
Uploaded by
ClaraCopyright:
Available Formats
MM
mm
• Pump the surface antigens
• First stepp top produce both HBeAg and HBsAg mm that doesn’t contain any
• Acute – eventually produce antibodies so acute DNA = exhaust immune
• Chronic: 1. no immune damage and lack of HBC-specific T cells 2. virus level comptrolled with 3. zero response to chronic
conversion of S so virus continuously produce S so no antibody production control infection
• HBV has ways to trigger innate immune response to trigger adaptive immunity • Receptor-mediated
endocytosis = clathrin-
• Liver sometimes ignore some pathogens from gut where from hepatic portal vein where tolerised so mediated endocytosis
HBV also hijak via this method (prevent over immunisation) • Partially positive strand
• Antigen-presentation is damped in liver – tolerising liver environment – not much immune response need to be repaired and
• Form perforin enzyme to kill pathogen-onfected cell completed in step 3-4
this makes cccDNA (mini
• If know where or how T cell got dysregulated or upset, can revert it
chromosome for HBV
• PD1 is the pathway for virus – can be based around for treatment DNA)
• Virus can block PD1 pathway so no interaction with T cell so can prevent inhibitory signal by the co- • Trapped within nucleus so
factors?? can’t be seen for cccDNA
• Amplification loop for 7b
• Treatment needs to be continuous – as or not cccDNA will start being made again step
• E antigen & surface
• Unless touching cccDNA – no cure just suppress replication
antigen produced and
MM secreted a lot in the serum
• Reduce viral infection then kick the immune response start at the end of cycle
• Mild chronic – live
without knowing
• If don’t convert e+ into e-
then will have the severe
cirrhosis
HEPATITIS VIRUS STUDY
Clinical Scenario Of Infection Prevention
• Viral infection that targets the liver • Prophylactic HBV vaccine (1982)
• Approximately 296 million people living with chronic • Requires at least 3 doses for approximately 95% efficacy = Compliance is poor
HBV • WHO recommends ALL infants to receive a dose at birth, preferably within 24 hours
• Young infants get infected & born by infected mothers in • Given to at-risk groups in UK & universal infant vaccination programme for HBV in
Asia side (Thailand, China) most countries
• 1.5 million new infections yearly • ONLY 36% coverage in countries with prevalence >8% (2006) & ineffective in
• 820,000 deaths in 2019 – cirrhosis / hepatocellular 5~15% of vaccinated children born to a HBV+ mother
carcinoma (primary liver cancer, HCC) • Worldwide < 5 years of age prevalence
• Approximately 1% of HBV+ individuals (2.7 million • 1.3% down from 4.7% in the pre-vaccination era
worldwide) infected with HIV • Can use drug, used to treat HBV, for HIV when co-infected
• Approximately 10.5% of people living with HBV aware
of their infection BUT ONLY 22% are on treatment
Global
History Of HBV Distribution Of
• 1965 – HBV discovered by Dr.Baruch Blumberg NIH (Nobel Prize in
Physiology and Medicine 1976) Chronic HBV
• 1967 – Australia antigen associated with hepatitis B
• 1969~1972 – chronic HBV infection linked to development of liver
cancer
• 1972~1982 – first vaccine developed to protect against HBV
• 1977 – discovery of delta antigen, discovery of HDV Global
• 1989 – HCV cloned from human serum
• 1998 – first direct-acting antiviral (lamivudine) for chronic HBV
Distribution Of
infection HBV Genotypes
• Blumberg & colleagues discovered HBV as abundant protein in the • Genotype varies depending
serum of an Australian aboriginal – ‘Australia antigen’ on region of infection
• HBV DNA found in ancient human remains • Satellite virus, HDV, can
• *hard to propagate in vitro = hard to study only exist with the
background of HBV
HEPATITIS VIRUS
Overview
• Hepadnaviridae family
1. Hepatotropism – should only be classified if infecting hepatocytes
2. Relatively strict species specificity (narrow host range)
3. Capacity to cause acute/chronic infection with viremia and antigenemia
• 10 genotypes (A-J) – differences in genome sequence; 4 major subtypes – adw, ayw, adr, ayr
• Non-cytopathic = Cause little or no direct damage to the hepatocyte [immune response to virus causes the issue]
• 42nm: outer envelope made of HBsAg (lipid layer) surrounding a nucleocapsid core of virus
• Small: partially double stranded DNA (approximately 3.2 kb in length – rcDNA)
• Compact: 4 overlapping frame-shifted open reading frames (ORF) – encoding 7 proteins
• Pregenomic RNA (= template for reverse transcription into relax circular DNA (rcDNA) within the nucleocapsid) – complete circular
negative strand & partial positive strand
• Synthesis of the core protein (C) and HBV polymerase (P)
• mRNA’s producing large, middle, small HBeAg surface antigen on lipid layer (preS – presurface domain /S – S most dominantly
expressed)
• X protein (X gene)
• Antigenicity
• All 3 envelope proteins are highly immunogenic & induce anti-HBs immunity (B cell humoral immunity)
• Structural viral proteins = Induce T cell responses (CD8 T cells & CTL cellular immunity)
STRUCTURE
• Core antigen is nuclear
capsid
• Different start codons =
Different polymerase for
transcription (4 types)
• E antigen = Give rise to
viral persistence
NOMENCLATURE OF HEPATITIS VIRUS
1.
LIFE CYCLE 1 2.
3.
Viruses have 1 goal – copying themselves giving rise to IDENTICAL
4.
progeny
Simplified Life Cycle 1 5.
1. Viral entry 6. Encapsidation
• HBV bind L-HBsAg to NTCP receptor (bile acid transporter) = HBV enters • pgRNA & template for core/pol = Template for DNA
hepatocytes synthesis by reverse transcriptase
• Requires low affinity interaction with heparin sulphate proteoglycans to • pgRNA encapsidation into nucleocapsid containing
initiate initial binding and transferrin receptors partially standard rcDNA with polymerase attached
2. Uncoating & rcDNA nuclear import • RNA to DNA conversion
• Internalisation – clathrin-mediated endocytosis 7. Maturation
• Removal of viral envelope and nucleocapsid • VIRION ASSEMBLY:
• Viral rcDNA transported into the nucleus via nuclear pores Maturing nucleocapsid traffic to the ER;
3. Conversion of rcDNA into cccDNA Enveloped by budding through the ER membrane
• Completion/Repair of partially stranded plus strand (not fully understood) where HBsAg are localised before budding from
• Nuclear rcDNA conversion by viral polymerase into covalently closed hepatocyte membrane;
circular (ccc) DNA Via Golgi
• cccDNA = Transcription template for all viral mRNAs by host RNA • GENOME AMPLIFICATION
polymerase II Early in infection, maturing capsids can be shuttled
4. INCLUDED WITHIN STEP 3 back to nucleus to replenish pool of cccDNA
5. Translation of viral mRNAs 8. Release of viral antigens
• Viral mRNAs exported to cytoplasm Viral mRNAs translated into various • Pre-C peptide transported to ER, trimmed, secreted as
HBV viral proteins pre-core antigen (HBsAg)
• Transcripts are polyadenylated for transport out of nucleus • Infected cell secretes non-infectious particles devoid of
• TRANSLATED PROTEINS: capsid and nucleic acids – empty HBsAg particles
1. Viral nucleocapsid and pre-core antigen (C, pre-C) detectable in serum (<104 ~ >109 / mL)
2. Polymerase (P) • Function of HBeAg is unknown
3. Envelope (L, M, S) • BUT Seroconversion from HBeAg+ to HBeAg- is a
4. X protein marker of reduced viral replication
5. pgRNA (3.5 kb species) spanning entire genome
LIFE CYCLE 2
Simplified Life Cycle 2
LIVER DISEASE
Spectrum Of Liver Disease Chronic HBV Infection
After HBV Infection CLINICAL PHASE DEVELOPMENT
• HBeAg & HBsAg production
Excess production of soluble and secreted proteins;
Diverts anti-Hs neutralisation of virions
• Lack of induction of an innate immune response
• Hepatotropic
• Dyregulates / Dysfunctional adaptive immune
response
• Persistence / Stability of cccDNA
Acute HBV Infection
CLINICAL PHASE
CHRONIC LIVER DISEASE DEVELOPMENT 1
Evasion Of Innate Immunity – as stealth virus Dysregulated / Dysfunctional Adaptive Immune Response
• Pattern recognition receptors (PPRs) culminating in • T cells are critical for control of HBV
induction of an antiviral IFN response • Recognise infected hepatocytes/cancerous cells
(upregulation of 100’s ISGs) HBV is invisible to Production of soluble mediators (cytokines, IFNg/TNFa)
PPRs of innate system Lack of hepatic Non-cytolytically kill them
expression of IFN and IFN-stimulated genes • Can kill cell / mediate clearance of virus by non-cytolytic
(ISGs) compared to HCV, associated with a strong methods (granzyme B elimination)
IFN response • Mechanism of immune failure
• Remains poorly understood why host innate • Pro-apoptotic Bim expression
immune responses Organ
fail to recognise • Lack CD3z expression
Immunological – liverHBV infection • TRAILR death R expression
• Processes over 30% of the total blood supply in 1 minute
• Receives antigen-rick blood from the portal vein • IL12 rescue of Tex
• Exposed to wide range of dietary and commensal products • MDSCs, low arginine
• First line of defence against blood borne pathogens • Metabolic dysfunction
• Exploited by viruses/tumours • PDL1-PD-1 signalling
• PD-1-PDL1 NK-mediated T cell inhibition
CHRONIC LIVER DISEASE DEVELOPMENT 2
Role of cccDNA / Removal & Dilution Of cccDNA
• cccDNA (viral minichromosome) is vital to HBV
persistence (molecular reservoir)
• cccDNA as the only transcriptional template for all
viral RNAs
• Nuclear location: hides replication intermediates
from the cellular machinery
• Unaffected by current therapies
• Direct targeting of cccDNA for
silencing/degradation/lethal mutation for HBV cure
TREATMENT
RARELY ACHIEVE CURE as they only suppress/stop replication
LIFELONG: cost, compliance, resistance, toxicity
Chronic HBV Infection
• Can treat with nucleos(t)ide analogues (NUCs)
(tenofovoir, entecavir)
• Pegylated IFNα – direct acting antiviral BUT
augments cell mediated immunity = various targets
Antivirals In Development
• ENTRY INHIBITORS
Myrcludex B – preS1 domain prevents HBV
entry;
Cyclosporin – inhibits function of NTCP
• ELIMINATION OF CCCDNA
IFNα and LTbR agonist – upregulates
APOBEC3A/3B which induce non-hepatotic
degradation of cccDNA;
CRISPR/Cas9 – targets mutations in cccDNA
• DAA (DIRECT ACTING ANTIVIRALS)
Inhibits viral enzymatic activity OR viral protein
function;
Prodrugs of tenofovir
• CORE ALLOSTERIC MODULATORS
Interferes with encapsidation process = Targets
HBc protein = Prevent mature capsid formation
• RNA INTERFERENCE (RNAi)
Delivery of small interfering RNAs to infected
hepatocytes
HEPATITIS D VIRUS (HDV) – satellite virus of HBV
15~20 million HBV+ patients are co-infected with HDV
Chronic HDV infection = Most severe form of viral hepatitis – accelerating
chronic HBV progression to cirrhosis/HCC
Only treatment currently available is pegIFNα (efficient in 20~35% of
patients)
Smallest virus known to infect humans
Uses the same entry receptors as HBV BUT Requires HBV envelope (L;
HBsAg) for infectivity = Can’t propagate without HBV
HDV virions composed of outer lipoprotein envelope made of HBsAg &
inner ribonucleoprotein struction, in which HDV genome resides (circular
RNA; 1.7 kb in length)
Simultaneous infection with HBV (co-infection) OR Superimposed on
chronic HBV patients (superinfection)
Vaccine for HBV protects against HDV
You might also like
- Animal Behavior GoodenoughDocument546 pagesAnimal Behavior GoodenoughDEBALIKA ROYNo ratings yet
- Virology Epidemology DiagnosticsDocument34 pagesVirology Epidemology DiagnosticsEleni HagosNo ratings yet
- Hepatitis VirusDocument83 pagesHepatitis VirusRudresh Shoorashetty ManoharNo ratings yet
- Hepatitis B Dan CDocument59 pagesHepatitis B Dan CNafizah Nurul AidaNo ratings yet
- (TM 2) Hepatitis B Dan CDocument59 pages(TM 2) Hepatitis B Dan CVivi OctaviaNo ratings yet
- Case Study Discussion HIVDocument31 pagesCase Study Discussion HIVAbby LiewNo ratings yet
- Hepatitis B VirusDocument31 pagesHepatitis B VirusFriyoga SyahrilNo ratings yet
- Hepatitis BDocument31 pagesHepatitis Bodakam.harrisNo ratings yet
- L22 - Viral Carcinogenesis-Part 2-S23Document23 pagesL22 - Viral Carcinogenesis-Part 2-S23waNo ratings yet
- Hepadna VirusesDocument30 pagesHepadna Virusesraymondvicent9No ratings yet
- HepatitisDocument24 pagesHepatitisAnn MariaNo ratings yet
- Seminar ProdiaDocument61 pagesSeminar ProdiaviraNo ratings yet
- Hepatitis B: Prepared By: Mina Zana Nozhin Ahmed Hoshyar Omer Hawkar IsmailDocument19 pagesHepatitis B: Prepared By: Mina Zana Nozhin Ahmed Hoshyar Omer Hawkar Ismailraman saeedNo ratings yet
- Microbiology Lecture - 20 Enterovirus & HepatitisDocument64 pagesMicrobiology Lecture - 20 Enterovirus & HepatitisChris Queiklin100% (1)
- Viral Hepatitis MBBS 2Document41 pagesViral Hepatitis MBBS 2Sohail ShahNo ratings yet
- Viral Hepatitis-Dr. A.M IyagbaDocument62 pagesViral Hepatitis-Dr. A.M IyagbaDr. Amb. Monday ZaccheausNo ratings yet
- Hep BDocument12 pagesHep BGracy PachoriNo ratings yet
- Hep B Group PresentationDocument23 pagesHep B Group PresentationShemiza BalmacoonNo ratings yet
- Hepatitis BDocument14 pagesHepatitis BLoc NguyenNo ratings yet
- DR YousifDocument28 pagesDR YousifAlex SamNo ratings yet
- Class 10 - Hepatitis Viruses: Ann Machablishvili, MD, PHDDocument23 pagesClass 10 - Hepatitis Viruses: Ann Machablishvili, MD, PHDqbcv4shshxNo ratings yet
- CMV & Ebv: A.ChancharoenDocument59 pagesCMV & Ebv: A.ChancharoenRapid MedicineNo ratings yet
- Hiv Hepc PresentationDocument16 pagesHiv Hepc Presentationapi-748224285No ratings yet
- Hepatitis B: Dr. Ruqaiyah NadeemDocument50 pagesHepatitis B: Dr. Ruqaiyah NadeemAulia Rahma NoviastutiNo ratings yet
- Therapeutic Strategies For Hepatitis B Virus Infection - Towards A CureDocument18 pagesTherapeutic Strategies For Hepatitis B Virus Infection - Towards A CureAdriana Villarreal FragaNo ratings yet
- TASH CI HepatitisDocument47 pagesTASH CI HepatitisBeamlak Getachew WoldeselassieNo ratings yet
- Heaptobiliary Disease by Lecturio.Document106 pagesHeaptobiliary Disease by Lecturio.louisegantierNo ratings yet
- Hepatitis BDocument9 pagesHepatitis BDivya DharshiniNo ratings yet
- Human Immunodeficiency Virus (Hiv)Document30 pagesHuman Immunodeficiency Virus (Hiv)Manesa ManeshaNo ratings yet
- VIRAL HEPATITIS IN PREGNANCY Copy 1Document48 pagesVIRAL HEPATITIS IN PREGNANCY Copy 1EndaleNo ratings yet
- Dr. G. Thiruvenkadam Post Graduate Dept of Pediatric & Preventive DentistryDocument31 pagesDr. G. Thiruvenkadam Post Graduate Dept of Pediatric & Preventive Dentistryதிருவேங்கடம் கோபாலன்No ratings yet
- Hepatitis BDocument21 pagesHepatitis Bapi-208983018No ratings yet
- HBV Easl 2017Document57 pagesHBV Easl 2017jessica100% (1)
- Muhammad Asaad Maidin Departement Microbiology Faculty of Medicine Hasanuddin University, MakassarDocument54 pagesMuhammad Asaad Maidin Departement Microbiology Faculty of Medicine Hasanuddin University, MakassarPratiwi PurnamaNo ratings yet
- Hepatitis VirusesDocument23 pagesHepatitis Viruses4jzbxz64kqNo ratings yet
- Viral Pathogenesis and Control of Viral DiseasesDocument55 pagesViral Pathogenesis and Control of Viral DiseasesSuresh KrishnaniNo ratings yet
- Elgouhari HM. Hepatitis B A Strategy For Evaluation and Management. 2009Document10 pagesElgouhari HM. Hepatitis B A Strategy For Evaluation and Management. 2009Revalitha PutriNo ratings yet
- CH 17Document10 pagesCH 17hannahbassett01No ratings yet
- Transfusion Transmitted InfectionDocument42 pagesTransfusion Transmitted InfectionNatalie JuntadoNo ratings yet
- Human Immunodeficiency VirusDocument26 pagesHuman Immunodeficiency ViruspraneethasruthiNo ratings yet
- Hepatitis CCRN KFSH&RC Asma AlshehriDocument33 pagesHepatitis CCRN KFSH&RC Asma AlshehriasmashNo ratings yet
- Summary of Virology & ImmunologyDocument19 pagesSummary of Virology & ImmunologyElaf NaifNo ratings yet
- Viral HepatitisDocument51 pagesViral HepatitisIlmiah BagusNo ratings yet
- Finals For Med SurgDocument11 pagesFinals For Med SurgAyessa CortesNo ratings yet
- AntiviralsDocument6 pagesAntiviralsNur NajminaNo ratings yet
- Hepato-Billiary Diseases: Tutor: DR SocdaalDocument32 pagesHepato-Billiary Diseases: Tutor: DR SocdaalOmar mohamedNo ratings yet
- UNIT 4 - New Challenges: Urja JoshiDocument72 pagesUNIT 4 - New Challenges: Urja JoshiRadhey RavalNo ratings yet
- Diagnosis and Treatment of Chronic Hepatitis B: Raymond D'Souza Graham R FosterDocument4 pagesDiagnosis and Treatment of Chronic Hepatitis B: Raymond D'Souza Graham R FosterrayNo ratings yet
- Cardiovascular System VirologyDocument18 pagesCardiovascular System Virology46nv7gphxzNo ratings yet
- Case StudyDocument54 pagesCase StudysHaYnEsEy100% (1)
- Hepatitis VirusesDocument19 pagesHepatitis VirusesFort SalvadorNo ratings yet
- HBV GP PerspectiveDocument42 pagesHBV GP PerspectivePankaj IngleNo ratings yet
- Viral Hepatitis Training Manual: Federal Ministry of Health National Hepatitis Control Program 2017Document15 pagesViral Hepatitis Training Manual: Federal Ministry of Health National Hepatitis Control Program 2017Eleni HagosNo ratings yet
- Hepatitis 4th prof[1]Document15 pagesHepatitis 4th prof[1]Muhammad IkramNo ratings yet
- 1010 M Balm - Viral HepatitisDocument17 pages1010 M Balm - Viral HepatitisSaad KhanNo ratings yet
- Application Syllabus Gene TherapyDocument4 pagesApplication Syllabus Gene Therapyngyj_flashNo ratings yet
- Viral Hepatitis PC II 2023Document76 pagesViral Hepatitis PC II 2023Suhayb CumarNo ratings yet
- Presentation of AIDSDocument16 pagesPresentation of AIDSZainab AbdullahiNo ratings yet
- Chapter 5.2 - HBV and Liver Cancer - Compatibility ModeDocument9 pagesChapter 5.2 - HBV and Liver Cancer - Compatibility Modenhan le thi thanhNo ratings yet
- Hepatitis A GDocument23 pagesHepatitis A Gapi-3712326No ratings yet
- Hepatitis B Virus and Liver DiseaseFrom EverandHepatitis B Virus and Liver DiseaseJia-Horng KaoNo ratings yet
- Cell & Tissue Engineering Strategies - Development & Replacement of Musculoskeletal TissuesDocument7 pagesCell & Tissue Engineering Strategies - Development & Replacement of Musculoskeletal TissuesClaraNo ratings yet
- BoneDocument18 pagesBoneClaraNo ratings yet
- Skeletal MuscleDocument8 pagesSkeletal MuscleClaraNo ratings yet
- Metabolism - LipidDocument2 pagesMetabolism - LipidClaraNo ratings yet
- Jimin - Lesson12B (J)Document1 pageJimin - Lesson12B (J)ClaraNo ratings yet
- Tendon & LigamentDocument11 pagesTendon & LigamentClaraNo ratings yet
- CartilageDocument16 pagesCartilageClaraNo ratings yet
- Jimin - Lesson67P (J)Document2 pagesJimin - Lesson67P (J)ClaraNo ratings yet
- Jimin - Lesson19.3C (J)Document1 pageJimin - Lesson19.3C (J)ClaraNo ratings yet
- Prokaryotes & EukaryotesDocument8 pagesProkaryotes & EukaryotesClaraNo ratings yet
- Jimin - Lesson50.2P (J)Document6 pagesJimin - Lesson50.2P (J)ClaraNo ratings yet
- Metabolism - Nucleic AcidDocument2 pagesMetabolism - Nucleic AcidClaraNo ratings yet
- Jimin - Lesson15.2C (J)Document1 pageJimin - Lesson15.2C (J)ClaraNo ratings yet
- Jimin - Lesson10P (J)Document10 pagesJimin - Lesson10P (J)ClaraNo ratings yet
- Metabolism - CarbohydrateDocument5 pagesMetabolism - CarbohydrateClaraNo ratings yet
- Jimin - Lesson14.2B (J)Document1 pageJimin - Lesson14.2B (J)ClaraNo ratings yet
- DNA To CellsDocument4 pagesDNA To CellsClaraNo ratings yet
- Lipids, Membranes, TransportDocument9 pagesLipids, Membranes, TransportClaraNo ratings yet
- Metabolism - Amino AcidsDocument2 pagesMetabolism - Amino AcidsClaraNo ratings yet
- Cells & TissuesDocument17 pagesCells & TissuesClaraNo ratings yet
- Cell DivisionDocument5 pagesCell DivisionClaraNo ratings yet
- Genetics & Inheritance - QuestionsDocument10 pagesGenetics & Inheritance - QuestionsClaraNo ratings yet
- DNA Structure & Replication + RNADocument8 pagesDNA Structure & Replication + RNAClaraNo ratings yet
- Cell TraffickingDocument7 pagesCell TraffickingClaraNo ratings yet
- Cell SignallingDocument7 pagesCell SignallingClaraNo ratings yet
- Cellular Compartments & EnvironmentsDocument5 pagesCellular Compartments & EnvironmentsClaraNo ratings yet
- Cell Adaptation - DefenceDocument8 pagesCell Adaptation - DefenceClaraNo ratings yet
- CarbohydrateDocument6 pagesCarbohydrateClaraNo ratings yet
- ATP & Energy MetabolismDocument3 pagesATP & Energy MetabolismClaraNo ratings yet
- Transcriptional & Chromatin RegulationDocument11 pagesTranscriptional & Chromatin RegulationClaraNo ratings yet
- Seminar: Wen-Juei Jeng, George V Papatheodoridis, Anna S F LokDocument14 pagesSeminar: Wen-Juei Jeng, George V Papatheodoridis, Anna S F LokCristian AGNo ratings yet
- Questions From The Section On General and Special VirologyDocument21 pagesQuestions From The Section On General and Special VirologytiffylolaNo ratings yet
- Full Ebook of Edrolo Vce Biology Units 3 4 2Nd Edition Adam Craig Online PDF All ChapterDocument69 pagesFull Ebook of Edrolo Vce Biology Units 3 4 2Nd Edition Adam Craig Online PDF All Chapteramandilavfndfr16100% (4)
- Biology Syllabus GR11-12 (2022-2023)Document37 pagesBiology Syllabus GR11-12 (2022-2023)Amal HassanNo ratings yet
- Effect of Increased Uv On Melanin Production in AnimalsDocument2 pagesEffect of Increased Uv On Melanin Production in Animalsapi-371487254No ratings yet
- Class 11th Zoology Syllabi 1Document1 pageClass 11th Zoology Syllabi 1Zaid KumarNo ratings yet
- General Biology QuizwithanswerkeyDocument3 pagesGeneral Biology QuizwithanswerkeyQueng ElediaNo ratings yet
- Lecture Set 5Document32 pagesLecture Set 5Dirt KickNo ratings yet
- Buku GelatinDocument129 pagesBuku GelatinAwan MegantoroNo ratings yet
- Chemical Classification of HormonesDocument65 pagesChemical Classification of HormonesetNo ratings yet
- Transcription Factor - WikipediaDocument112 pagesTranscription Factor - WikipediaBaikuntha SabarNo ratings yet
- MediUnite Journal Monthly Magasine Vital - April 2024Document21 pagesMediUnite Journal Monthly Magasine Vital - April 2024MediUnite JournalNo ratings yet
- 22 PhysochlainaDocument11 pages22 PhysochlainasaleemNo ratings yet
- Torres Guzmán Moncayo Year 8Document18 pagesTorres Guzmán Moncayo Year 8John OsborneNo ratings yet
- Linkage Disequilibrium: Brenner's Encyclopedia of Genetics (Second Edition)Document6 pagesLinkage Disequilibrium: Brenner's Encyclopedia of Genetics (Second Edition)BobNo ratings yet
- Chapter 4: Amino Acids: MatchingDocument11 pagesChapter 4: Amino Acids: MatchingeliNo ratings yet
- Bethany Christian School of Tarlac Inc.: Before Each NumberDocument1 pageBethany Christian School of Tarlac Inc.: Before Each NumberHezron DamasoNo ratings yet
- Cells Study Guide 2020 KEYDocument4 pagesCells Study Guide 2020 KEYLaarni GeeNo ratings yet
- EchinoideaDocument35 pagesEchinoideaEvika Fatmala DeviNo ratings yet
- Haploid Production and Its ApplicationsDocument16 pagesHaploid Production and Its ApplicationsNikita JainNo ratings yet
- Application of Zoology NoteDocument32 pagesApplication of Zoology NoteShivam GuptaNo ratings yet
- 2021 BPDocument24 pages2021 BPErlita SaputriNo ratings yet
- Excretion in Humans (13.1.1) CIE IGCSE Biology Revision Notes 2023 Save My ExamsDocument1 pageExcretion in Humans (13.1.1) CIE IGCSE Biology Revision Notes 2023 Save My ExamslulogaspariNo ratings yet
- Dopamine Receptors: GlossaryDocument5 pagesDopamine Receptors: Glossarytirasi1214No ratings yet
- Glimmers of Hope For Targeting Oncogenic KRAS-G12D: Cancer Gene TherapyDocument3 pagesGlimmers of Hope For Targeting Oncogenic KRAS-G12D: Cancer Gene Therapychato law officeNo ratings yet
- Color Atlas of Diagnostic MicrobiologyDocument223 pagesColor Atlas of Diagnostic MicrobiologyOana Herea100% (2)
- Acs Analchem 0c04608Document9 pagesAcs Analchem 0c04608abhishek112934No ratings yet
- Biological ClassificationDocument35 pagesBiological Classificationsanjeevani rawatNo ratings yet
- My Answer in Our LaboratoryDocument4 pagesMy Answer in Our LaboratoryKris Marie DelaCruz DomingoNo ratings yet

















































![Hepatitis 4th prof[1]](https://imgv2-2-f.scribdassets.com/img/document/747791524/149x198/f2955d0d13/1720070352?v=1)