Professional Documents
Culture Documents
NOTESs
NOTESs
Uploaded by
Ahmed Mohammed omar0 ratings0% found this document useful (0 votes)
4 views5 pagesCopyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
4 views5 pagesNOTESs
NOTESs
Uploaded by
Ahmed Mohammed omarCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 5
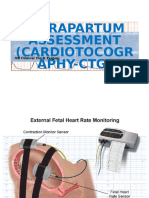
Acceleration: A visually apparent abrupt increase (onset to peak in <30 seconds) in the FHR.
These are mediated by the
sympathetic nervous system in response to fetal movements or scalp stimulation.
• At ≥32 weeks gestation, an acceleration has a peak of >15 beats/min above baseline, with a duration of >15 seconds but < 2
min from onset to return.
• At <32 weeks gestation, an acceleration has a peak of >10 beats/min above baseline, with a duration of >10 sec but <2 min
from onset to return.
Early deceleration: A visually apparent usually symmetrical gradual decrease and return of the FHR associated with a uterine
contraction. These are mediated by parasympathetic stimu- lation and occur in response to head compression.
• A gradual FHR decrease is defined as from the onset to the FHR nadir of >30 seconds.
• The decrease in FHR is calculated from the onset to the nadir of the deceleration.
• The nadir of the deceleration occurs at the same time as the peak of the contraction.
Late deceleration: A visually apparent usually symmetrical gradual decrease and return of the FHR associated with a uterine
contraction. These are mediated by either vagal stimulation or myocardial depression and occur in response to placental
insufficiency.
• A gradual FHR decrease is defined as from the onset to the FHR nadir of >30 seconds.
• The decrease in FHR is calculated from the onset to the nadir of the deceleration.
• The deceleration is delayed in timing, with the nadir of the deceleration occurring after the peak of the contraction.
Variable deceleration: A visually apparent abrupt decrease in FHR. These are mediated by umbilical cord compression.
• An abrupt FHR decrease is defined as from the onset of the deceleration to the begin- ning of the FHR nadir of <30
seconds.
• The decrease in FHR is calculated from the onset to the nadir of the deceleration.
• The decrease in FHR is >15 beats per minute, lasting >15 seconds, and<2 minutes in duration.
Sinusoidal pattern: • A visually apparent, smooth, sine wave-like undulating pattern in FHR baseline with a cycle
frequency of 3–5/min which persists for ≥20 min.
Category I: FHR tracings are normal
Criteria include all of the following:
• Baseline rate: 110-160 beats/min
• Baseline FHR variability: moderate
• Late or variable decelerations: absent
• Early decelerations: present or absent
• Accelerations: present or absent
Interpretation: strongly predictive of normal fetal acid-base status at time of observation
Action: monitoring in a routine manner, with no specific action required
Category II: FHR tracings are indeterminate
These include all FHR tracings not categorized as category I or III, and may represent an appreciable fraction of those
encountered in clinical care.
Interpretation: not predictive of abnormal fetal acid-base status
Action: evaluation and continued surveillance and reevaluation, taking into account the entire associated clinical
circumstances
Category III: FHR tracings are abnormal
Criteria include absent baseline FHR variability and any of the following:
• Recurrent late decelerations
• Recurrent variable decelerations
• Bradycardia
• Sinusoidal pattern
Interpretation: associated with abnormal fetal acid-base status at time of observation; requires prompt evaluation
Action: expeditious intrauterine resuscitation to resolve the abnormal FHR pattern; if tracing does not resolve with these
measures, prompt delivery should take place.
AMNIOTIC FLUID INDEX
The 4-quadrant amniotic fluid index test assesses in centimeters the deepest single vertical amniotic fluid pocket in each of the
4 quadrants of the uterus. The sum of the pockets is known as the amniotic fluid index, or AFI. Interpretation is as follows:
<5 cm—oligohydramnios/ 5–8 cm—borderline/ 9–25 cm—normal/ >25 cm—polyhydramnios
BIOPHYSICAL PROFILE (BPP): A complete BPP measures 5 components of fetal well-being: NST, amniotic fluid volume,
fetal gross body movements, fetal extremity tone, and fetal breathing movements. The last 4 components are assessed using
obstetric ultrasound. Scores given for each component are 0 or 2, with maximum possible score of 10 and minimum score of 0.
• Score of 8 or 10—highly reassuring of fetal well-being. Management is to repeat the test weekly or as indicated. Fetal death
rate is only 1 per 1,000 in the next week. • Score of 4 or 6—worrisome. Management is delivery if the fetus is >36 weeks or
repeat the biophysical profile in 12–24 h if <36 weeks. An alternative is to perform a CST. • Score of 0 or 2—highly predictive
of fetal hypoxia with low probability of false posi- tive. Management is prompt delivery regardless of gestational age.
CONTRACTION STRESS TEST (CST):This test assesses the ability of the fetus to tolerate transitory decreases in intervillous
blood flow that occur with uterine contractions. It uses both external FHR and contraction moni- toring devices and is based on
the presence or absence of late decelerations. These are grad- ual decreases in FHR below the baseline with onset to nadir of ≥30
s. The deceleration onset and end is delayed in relation to contractions. If 3 contractions in 10 min are not spontane- ously
present, they may be induced with either IV oxytocin infusion or nipple stimulation. This test is rarely performed because of the
cost and personnel time required. The most com- mon indication is a BPP of 4 or 6.
• Negative CST requires absence of any late decelerations with contractions. This is reassuring and highly reassuring for fetal
well-being. Management is to repeat the CST weekly. Fetal death rate is only 1 per 1,000 in the next week.
• Positive CST is worrisome. This requires the presence of late decelerations associ- ated with at least 50% of contractions. Fifty
percent of positive CSTs are false positive (meaning the fetus is not hypoxemic). They are associated with good FHR variability.
The 50% of true positives are associated with poor or absent variability. Management is prompt delivery.
• Contraindications—CST should not be performed whenever contractions would be hazardous to the mother or fetus. Examples
include previous classical uterine incision, previous myomectomy, placenta previa, incompetent cervix, preterm membrane rup-
1. Have a written breastfeeding policy that is regularly communicated to all health-care staff
2. Train all staff in skills necessary to implement this policy
3. Inform all pregnant women about the benefits and management of breastfeeding
4. Help mothers initiate breastfeeding within an hour of birth
5. Show mothers how to breastfeed and how to sustain lactation, even if they should be separated from their infants
6. Feed newborns nothing but breast milk, unless medically indicated, and prioritize donor breast milk when supplementation
is needed
7. Practice rooming-in, which allows mothers and newborns to remain together 24 hours a day
8. Encourage breastfeeding on demand
9. Give no artificial pacifiers to breastfeeding newborns
10. Help start breastfeeding support groups and refer mothers to them
Advantage BF: Nutritional/ Immunological /Developmental /Psychological /Social /Economic /Environmental /Optimal
growth and development Decrease risks for acute and chronic diseases
First trimester care: Care team/Postpartum visits/Lactation support/Infant feeding plan/Reproductive life plan /Contraception/
Pregnancy complications /Cardiovascular risk assessment/ Mental health/ Postpartum problems /Chronic conditions
CONDUCTION OF DELIVERY: Delivery of the head: The principles to be followed are to maintain flexion of the head,
to prevent its early extension and to regulate its slow escape out of the vulval outlet.
The patient is encouraged for the bearing-down efforts during uterine contractions. This facilitates descent of the head.
Delivery of the shoulders: Not to be hasty in delivery of the shoulders. Wait for the uterine contractions to come and for the
movements of restitution and external rotation of the head to occur
Delivery of the trunk: After the delivery of the shoulders, the fore finger of each hand are inserted under the axillae and the
trunk is delivered gently by lateral flexion.
You might also like
- Clinical Obstetrics/Gynecology Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2From EverandClinical Obstetrics/Gynecology Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Rating: 4 out of 5 stars4/5 (1)
- CTG Interpretation Made EasyDocument11 pagesCTG Interpretation Made EasySeneeth Peramuna100% (2)
- Adapting Organization To Environment UncertaintyDocument19 pagesAdapting Organization To Environment UncertaintySameer MiraniNo ratings yet
- Project Report On e BikesDocument57 pagesProject Report On e Bikesrh21940% (5)
- Rapala Catalog 2018Document164 pagesRapala Catalog 2018gcu93No ratings yet
- Ante Partum and Intra Partum Fetal MonitoringDocument63 pagesAnte Partum and Intra Partum Fetal MonitoringasdfNo ratings yet
- 1835 FHR MonitoringDocument47 pages1835 FHR MonitoringjackNo ratings yet
- Fetal SurveillanceDocument5 pagesFetal SurveillanceĶHwola ƏľsHokryNo ratings yet
- Fetal Monitoring Orientation Day-1Document50 pagesFetal Monitoring Orientation Day-1Scott CalfeeNo ratings yet
- Intrapartum Assessment: Factors That Affect Oxygenation During LaborDocument10 pagesIntrapartum Assessment: Factors That Affect Oxygenation During LabornicewanNo ratings yet
- Abnormal Cardiotohography in NewbornDocument37 pagesAbnormal Cardiotohography in NewbornAdityaRahaneNo ratings yet
- Antepartum Surveillance 2Document23 pagesAntepartum Surveillance 2Julia kwapeNo ratings yet
- Antenatal Assessment of Fetal WellbeingDocument52 pagesAntenatal Assessment of Fetal Wellbeing6ixSideCreate MNo ratings yet
- Physiology of 1st Stage of LaborDocument134 pagesPhysiology of 1st Stage of LaborVijith.V.kumar50% (2)
- Chapter 14Document5 pagesChapter 14Kelly HeartsillNo ratings yet
- CTG InterpretasiDocument86 pagesCTG Interpretasiprimaindra27No ratings yet
- Antepartum Fetal SurveillanceDocument74 pagesAntepartum Fetal Surveillanceachala sahaiNo ratings yet
- Intrapartum AssesmentDocument71 pagesIntrapartum AssesmentHusain ChherawalaNo ratings yet
- How To Read A CTGDocument12 pagesHow To Read A CTGyehezkieldward100% (1)
- Assessment of Fetal WellbeingDocument24 pagesAssessment of Fetal WellbeingMukesh ThakurNo ratings yet
- Assessment of Fetal Well BeingDocument61 pagesAssessment of Fetal Well Beingsana khan008No ratings yet
- 2 Obg Seminar at NST J Inal (1) SSTDocument19 pages2 Obg Seminar at NST J Inal (1) SSTAmritaNo ratings yet
- Procedures ObgDocument12 pagesProcedures Obgraghuram reddyNo ratings yet
- NST CSTDocument9 pagesNST CSTNadiya RashidNo ratings yet
- Fetal SurvillanceDocument26 pagesFetal SurvillanceBetelhem EjiguNo ratings yet
- Assessment of Fetal WellbeingDocument71 pagesAssessment of Fetal WellbeingDanny Apw100% (2)
- Google - Fetal Surveillance During Labor - 天津醫院Document56 pagesGoogle - Fetal Surveillance During Labor - 天津醫院OANo ratings yet
- Antenatal AssessmentDocument84 pagesAntenatal AssessmentRitbano AhmedNo ratings yet
- Post Term PregnancyDocument35 pagesPost Term PregnancyNishaThakuri100% (2)
- Assessment of Fetal G&DDocument75 pagesAssessment of Fetal G&DHillary Praise AquinoNo ratings yet
- Basic Fetal Heart Monitoring - 12 - 15Document10 pagesBasic Fetal Heart Monitoring - 12 - 15elishaNo ratings yet
- CTG Interpretation: Dr. Areen AlnasanDocument37 pagesCTG Interpretation: Dr. Areen AlnasanMohammad AlrefaiNo ratings yet
- Antepartum Fetal MonitoringDocument4 pagesAntepartum Fetal MonitoringChristoperJ.ErecreNo ratings yet
- Government College of Nursing Jodhpur (Raj.) : Procedure On-Cordiotocography Subject-Obstetrics & Gynecology Specialty-IDocument6 pagesGovernment College of Nursing Jodhpur (Raj.) : Procedure On-Cordiotocography Subject-Obstetrics & Gynecology Specialty-Ipriyanka100% (1)
- Intrapartum Fetal Monitoring: Dalal AljarrahDocument44 pagesIntrapartum Fetal Monitoring: Dalal Aljarrahhacker ammerNo ratings yet
- How To Read A CTGDocument11 pagesHow To Read A CTGjNo ratings yet
- CTG Finding S-GuidelinesDocument15 pagesCTG Finding S-GuidelinesAyman AlmugaddamiNo ratings yet
- OSCE OB - PDF Version 1Document15 pagesOSCE OB - PDF Version 1FNaF is love FNaF is lifeNo ratings yet
- 9fetal Well Being in PregnancyDocument10 pages9fetal Well Being in PregnancyuouoNo ratings yet
- Antepartum Fetal Assessment 2018Document39 pagesAntepartum Fetal Assessment 2018amena mahmoudNo ratings yet
- Learn Mat 6Document14 pagesLearn Mat 6Shyla ManguiatNo ratings yet
- Assessment of Fetal WellbeingDocument42 pagesAssessment of Fetal WellbeingMLV AbayNo ratings yet
- Antepartum Fetal SurveillanceDocument48 pagesAntepartum Fetal SurveillanceDr.P.NatarajanNo ratings yet
- Antepartum AssessmentDocument14 pagesAntepartum Assessmentamena mahmoudNo ratings yet
- Labor and Delivery NoteDocument26 pagesLabor and Delivery NoteyagyaNo ratings yet
- Fetal Assessment During LaborDocument3 pagesFetal Assessment During LaborMariya ZafraniNo ratings yet
- Labor and DeliveryDocument10 pagesLabor and DeliveryDelia Ramirez0% (1)
- CTG ReportingDocument89 pagesCTG ReportingKevin Marcial AralarNo ratings yet
- CTGDocument11 pagesCTGMustafa Abd-Al SahibNo ratings yet
- Antepartum Assessment PPT KoDocument20 pagesAntepartum Assessment PPT Kosupladitasha_75100% (1)
- Antenatal Assessment of Fetal WellbeingDocument67 pagesAntenatal Assessment of Fetal WellbeingPaunami Dey50% (2)
- Intrapartum AssessmentDocument89 pagesIntrapartum AssessmentYanyan PanesNo ratings yet
- Fetal Surveillance: By: Kristine R. Niñonuevo-Dayao, M.DDocument43 pagesFetal Surveillance: By: Kristine R. Niñonuevo-Dayao, M.DSanjay Kumar SanjuNo ratings yet
- Normal LaborDocument70 pagesNormal LaborAmlodipine BesylateNo ratings yet
- Assessment of Fetal Growth and DevelopmentDocument30 pagesAssessment of Fetal Growth and DevelopmentWild Rose100% (2)
- Assessment of Fetal Well BeingDocument46 pagesAssessment of Fetal Well BeingAumrin Fathima100% (1)
- 1 - Antenatal AssessmentDocument44 pages1 - Antenatal AssessmentIbrahim RamizNo ratings yet
- How To Read A CTGDocument11 pagesHow To Read A CTGiwennieNo ratings yet
- Partograph and CTG Intrapartum Fetal MonitoringDocument56 pagesPartograph and CTG Intrapartum Fetal MonitoringPEÑAFLOR, Shealtiel Joy G.No ratings yet
- CARDIOTOCOGRAPHYDocument5 pagesCARDIOTOCOGRAPHYPadma100% (1)
- Dental Management of the Pregnant PatientFrom EverandDental Management of the Pregnant PatientChristos A. SkouterisNo ratings yet
- Pediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesFrom EverandPediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesRating: 5 out of 5 stars5/5 (2)
- Barrier Methods.Document35 pagesBarrier Methods.Ahmed Mohammed omarNo ratings yet
- Clift LipDocument2 pagesClift LipAhmed Mohammed omarNo ratings yet
- Coc and PopDocument22 pagesCoc and PopAhmed Mohammed omarNo ratings yet
- Discharge FormDocument11 pagesDischarge FormAhmed Mohammed omarNo ratings yet
- Reading Circle Group RolesDocument3 pagesReading Circle Group RolesAhmed Mohammed omarNo ratings yet
- Reparoductive SystemDocument4 pagesReparoductive SystemAhmed Mohammed omarNo ratings yet
- Setting AnalysisDocument3 pagesSetting AnalysisAhmed Mohammed omarNo ratings yet
- LIBRARIESDocument3 pagesLIBRARIESAhmed Mohammed omarNo ratings yet
- LanguageDocument4 pagesLanguageAhmed Mohammed omarNo ratings yet
- River Between Us 10-11 RevisedDocument10 pagesRiver Between Us 10-11 RevisedCaydenNo ratings yet
- Lesson 2 - Duties of A Painting (Coatings) InspectorDocument55 pagesLesson 2 - Duties of A Painting (Coatings) InspectorFarhad AsadulovNo ratings yet
- Parametric Kerf Bending - ArticleDocument25 pagesParametric Kerf Bending - ArticleMIS-TRYNo ratings yet
- Crim 1 BDocument1 pageCrim 1 BJose Antonio Peralta Achaval Jr.No ratings yet
- Damping Modification for Spectrum: Lap-Loi Chung (鍾立來)Document39 pagesDamping Modification for Spectrum: Lap-Loi Chung (鍾立來)陳俊鴻No ratings yet
- Classes and Breeds of Cattle and BuffaloDocument30 pagesClasses and Breeds of Cattle and Buffalowaleed elhawarryNo ratings yet
- Unit 2 B TR Family and Friends 5Document12 pagesUnit 2 B TR Family and Friends 5Toàn Nguyễn Đỗ ThanhNo ratings yet
- Code Addicts - The Python Starter Kit - An In-Depth and Practical Course For Beginners To Python Programming. Including Detailed Step-By-step Guides and Practical Demonstrations. (2017)Document136 pagesCode Addicts - The Python Starter Kit - An In-Depth and Practical Course For Beginners To Python Programming. Including Detailed Step-By-step Guides and Practical Demonstrations. (2017)Roland Rawlins Igabor100% (2)
- Math 2270 - Lecture 27: Calculating Determinants: Dylan Zwick Fall 2012Document7 pagesMath 2270 - Lecture 27: Calculating Determinants: Dylan Zwick Fall 2012Civil GeomaticNo ratings yet
- NMM Gold TutorialDocument7 pagesNMM Gold TutorialTane67No ratings yet
- Sanskrit Participles - Overview - Sanskrit Studio PDFDocument14 pagesSanskrit Participles - Overview - Sanskrit Studio PDFRskrsk RskNo ratings yet
- S.No Acc No Title of The BookDocument12 pagesS.No Acc No Title of The BookmechhodNo ratings yet
- Regina D Perry CV 2015Document8 pagesRegina D Perry CV 2015api-284587833No ratings yet
- EcologyDocument14 pagesEcologyHaritha HaridasNo ratings yet
- Asp Convent English High SchoolDocument4 pagesAsp Convent English High SchoolSimran Sachdev100% (1)
- Computation Theory: Lecture TwoDocument9 pagesComputation Theory: Lecture TwoColmain NassiriNo ratings yet
- Summer Report 2018-2019Document23 pagesSummer Report 2018-2019ajin shajuNo ratings yet
- X X X X X X X X X X X X X X: Sec Tan Sin Tan Sin CSC Cot Cos CSC Cot Cot Cos Tan SecDocument7 pagesX X X X X X X X X X X X X X: Sec Tan Sin Tan Sin CSC Cot Cos CSC Cot Cot Cos Tan SecKevin Christian Plata100% (1)
- Reflections in A Plane Mirror - PPT SlidesDocument41 pagesReflections in A Plane Mirror - PPT SlidesSaptarshi MazumderNo ratings yet
- B1 Reading-Gapped Sentences-Addicted To SoapsDocument2 pagesB1 Reading-Gapped Sentences-Addicted To SoapsuriordiziaNo ratings yet
- V-Carve Garota e GolfDocument332 pagesV-Carve Garota e GolfCarlos CardiauNo ratings yet
- Eurosa Furniture (Co) Pte LTD: Quality Control/Inspection/Enduring Testing ManualDocument6 pagesEurosa Furniture (Co) Pte LTD: Quality Control/Inspection/Enduring Testing ManualBelal AhmedNo ratings yet
- High Lift Hydraulic Transmission Jacks "AF25082" "AF50080" "AF100080"Document6 pagesHigh Lift Hydraulic Transmission Jacks "AF25082" "AF50080" "AF100080"Alain DefoeNo ratings yet
- Pubscatalog de LA Aabb 2018Document27 pagesPubscatalog de LA Aabb 2018AndresPimentelAlvarezNo ratings yet
- Method Statement For Survey WorksDocument13 pagesMethod Statement For Survey WorksSagun Almario100% (1)
- Sony CCD-TR67 PDFDocument80 pagesSony CCD-TR67 PDFClemente GuerraNo ratings yet
- IRS Questions QbankDocument2 pagesIRS Questions Qbanktest1qaz100% (1)