Professional Documents
Culture Documents
Acid Base Balance and Disorders
Acid Base Balance and Disorders
Uploaded by
Ismail VokshiOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acid Base Balance and Disorders
Acid Base Balance and Disorders
Uploaded by
Ismail VokshiCopyright:
Available Formats
IsmaiI Vokshi
Acid Base Balance and Disorders
CLNCAL FEATURES
Respiratory
Acidosis Retention of CO2
Reduced ventilation
Reduced O2 levels
Dyspnoea
Reduced Consciousness
Coma
ncreased CO2 levels
Peripheral Vasodilatation
Decrease BP
Headaches raised CP due to vasodilatation
Reduced Cardiac Contractility if heart is enlarged
Papilloedema
Alkalosis ncreased Removal of CO2
ncreased ventilation
Reduced pH levels Neuromuscular irritability (also from low Ca)
Perioral and Extremity Paraesthesia and Numbness
Muscle Cramps, Hyperreflexia and Tetany
Tinitus
Seizures
Cerebral Vasoconstriction - pH receptors on vessels
Cardiac Dysrhythmias change in cardiac membrane potentials
HypocaIcemia symptoms dominate. Reduction in H+ leads to Ca
replacing its actions and binding to plasma proteins.
MetaboIic
Acidosis Gain of Acid or Loss of Bicarbonate
Kussmaul Breathing Deep Raid Ventilation ncrease CO2 expulsion
Hypotension - Acidity Reduction on Peripheral Resistance and Cardiac
Contractility
Pulmonary Oedema and Ventricular Arrest are Possible
Hypercalciuria Acid ncreased Ca release from Bone Excreted in Urine
Hyperkalaemia Moves Out of Cells Following Electrochemical Gradient.
Alkalosis Gain of Bicarbonate of Loss of Acid
Hypoventilation Low pH nhibition of Respiratory Centre
Hypokalaemia Weakness, Myalgia and Polyuria
Hypercalcemia Tetany (Chvostek sign, Trousseau sign) Change in Mental Status,
Seirures
Vomiting or Diarrhoea Can be a Cause Bulimia
Hypertension Comes with some of the causes
Volume status
Depletion Chloride sensitive causes
Expansion Chloride resistant causes
IsmaiI Vokshi
Acid Base Balance and Disorders
BIood
Gasses
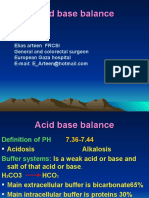
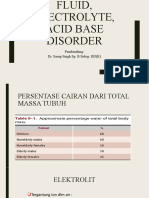
pH PaCO2 HCO3-
Compensatio
n
Respiratory
Acidosis
N or
(Compensated)
Metabolic
Respiratory
Alkalosis
N or
(Slight) Metabolic
Metabolic
Acidosis
N or
Respiratory
Metabolic
Alkalosis
N or
(Slightly)
Respiratory
pH o [HCO
3
-
] / PaCO
2
Controlled by Kidney
Altered by metabolic
disorders
Controlled by Respiration
Altered in respiratory
disorders
CAUSES
Respiratory Acidosis ncrease pCO2 and [H+], HCO3- Retention May Compensate [H+]
Causes - Almost always by Alveolar Hypoventilation. Others: ncrease CO2 in air or increase CO2
production
Lung or Chest Wall DefectsPneumothorax, PuImonary Oedema, Aspiration, PuImonary
Fibrosis (Restrictive Diseases), Adult Respiratory Distress Syndrome, Diaphragmatic paralysis and
Trauma; Flail Chest, Contusion, Haemothorax;
Airway Disorders Asthma/ COPD Exacerbations, Chronic Brochitis, Emphysema, Upper
Airway Obstruction (Tumour, Foreign Body), Laryngospasm
Central Respiratory Depression Drugs; Opiates, Sedatives, Anaesthetics; CervicaI
Cord Trauma (Above C4); Cardiac Arrest with CerebraI Hypoxia; CNS trauma, infarct, haemorrhage
or tumour. Pickwickian Syndrome (Hypoventilation due to Obesity), Central Neural Bloackade,
Poliomyelitis, Tetanus
Nerve and Muscle Disorders GuiIIain-Barre Syndrome, Myastheria Gravis, Muscle
Relaxants, Toxins (Organophosphates, Snake Venom) and other Myopathies.
Others ncreased CO2 Production Malignant Hyperthermia; ncreased CO2 ntake High Air CO2
Content, CO2 in Body Cavity Laparoscopic Surgery.
Questions
1. s the patient acidotic or alkalotic? Determined by arterial pH
2. s ventilation compensating pH change or causing it? Determined by PaCO2
3. s there metabolic acidosis? Look at the anion gap
IsmaiI Vokshi
Acid Base Balance and Disorders
CAUSES
Respiratory Alkalosis Decrease PaCO2 and [H+]
Causes An Acid-Base Disorder caused by Hyperventilation ncreased Alveolar Ventilation
Reduced pCO2 Peripheral Chemo r. Reduced Ventilation Rate
Hypoxaemia (Act via peripheral chemoreceptor's) Stimulates rapid deep breathing Alkalosis
(f Metabolic Acidosis is the cause it is considered a secondary change)
Pulmonary Causes (ntrapulmonary r.) PuImonary EmboIism, Asthma (Hyperventilation due to
hypoxia), Pneumonia, Pulmonary Oedema.
Central Causes(Act directly on respiratory centre) Anxiety-HyperventiIation Syndrome
(Psychogenic), Pain, Fear, Stress, VoIuntary, Head njury, Stroke, Drugs (Analeptics, Propanidid,
Salicylate ntoxication), Endogenous Compounds (Progesterone (during pregnancy), Cytokines (Sepsis),
Toxins (Chronic Liver Disease)
atrogenic Excessive Controlled Ventilation
Metabolic Acidosis ncrease in fixed acids in blood. ncrease [H+] Reduced [HCO3-]. This is
a primary decrease in [HCO3-], in contrast to the compensatory decrease in Chronic Resp. Alkalosis.
Causes gain of strong acid (Ketoacidosis or NH4Cl nfusion) loss of base (diarrhoea, carbonic
anhydrase inhibitors, renal tubular acidosis)
High Anion-Gap Acidosis Acid Addition
Ketoacidosis Diabetic, Starvation and Alcoholic (Starvation and Alcohol Toxicity to Liver
Lactic Acidosis - Type A mpaired perfusion Reduced O2 Delivery Sepsis, Shock
- Type B mpaired Carbohydrate Metabolism Reduced
Aerobic Capacity
Renal failure Uraemic Acidosis, Acute Renal Failure
Toxins Toxic Alcohol Metabolites Reduce Lactate (+Anions) Metabolism by Liver
Methanol, Ethylene Glycol. Saclicylates (Aspirin) Also causes; Tinnitus, Nausea and
Hyperventilation.
Normal Anion-Gap Acidosis (Hyperchloraemic Acidosis) Bicarbonate Loss
Renal Bicarbonate Loss Renal Tubular Acidosis, Carbonic Anhydrase nhibitors
Gut Bicarboinate Loss Severe Diarrhoea, Uretero-enterostomy; exchange of Cl- (in urine)
with HCO3- (in gut), Drainage of biliary or pr pancreatic secretions (high in HCO3-), Small
bowel fistiulla.
Other Addition of HCl, NH4Cl
Recovery from ketoacidosis
Metabolic Alkalosis Primary, Plasma Bicarbonate Rises Above Normal. Severity determined
by difference between actual and expected levels of Plasma Bicarbonate.
Loss of Gastric Acid(Vomiting + NG Drainage) and Diuretic Use = 90% of Metabolic
Alkalosis
Causes are divided into nitiating and Maintaining.
nitiating Causes Gain of Alkali from ECF
- From Exogenous Source (Sodium Bicarbonate nfusion, Massive Blood Transfusion (Citrate in
Transfused Blood), Exogenous Lactate,
- From Endogenous Source Recovery phase from organic acidosis hepatic metabolism of lactate or
ketoanions results in bicarbonate production, Milk Alkali Syndrome.
IsmaiI Vokshi
Acid Base Balance and Disorders
Loss of H
+
from ECF - via Kidneys use of diuretics, via Gut vomiting, NG suction, Pyloric
stenosis
Citrate and Ketoacidosis
An acid is defined as [HA] H
+
+ A
-
. The A
-
is a base 'Acid Anion' (Can Accept a H
+
)
e.g. Citrate is an acid anion of Citric Acid, Lactate is an acid anion of Lactic Acid
Liver Metabolises Acid Anions Lactate
Lactate dehydrogenase
Pyruvate A H
+
is used up in the process
[HCO3
-
]
n Massive Blood Transfusions High Citrate [HCO3
-
] (Metabolic Alkalosis) Only Transient, This will
recover unless there is a maintaining cause present.
Maintaining Causes
Chloride and Potassium Depletion
Chloride Depletion Causes alkalosis Renal Tubules Cl
-
exchanged HCO3
- (Secreted)
When Na
+
or K
+
is reabsorbed either Cl
-
or HCO3
-
is reabsorbed.
When Plasma [Cl
-
] are low Reduction in HCO3
-
excretion.
When [Na
+
] or [K
+
] is reabsorbed low [Cl
-
] leads to HCO3
-
re-absorption instead.
Hypovolaemia precipitates this condition as it leads to Aldosterone release.
Chloride Depletion
- Loss of Acidic Gastic Juice
- Diuretics Also Reduce K
+
levels. Hypovolaemia Aldosterone
- Post-hypercapnia
- Excess Faecal Loss (Villous Adenoma)
Potassium Depletion
- 1
0
and 2
0
Hyperaldesteronism K
+
Depletion, H
+
ATP-ase activation HCO3
-
Absorption
- Cushings Syndrome
- Diuretics and Other Drugs (Carbenoxolone)
- Excessive Licorice ntake ncrease Aldosterone Action Upregulated Mineralocorticoid R.
- Barett's Syndrome Defects on Renal Tubule on Channels
- Typ1 (Neonatal) Na-K-2Cl Symporter
- Typ2 ROMK K Channel in Ascending Limb
- Typ3 CLCNKB Cl
-
Channel
Others Laxative Abuse
IsmaiI Vokshi
Acid Base Balance and Disorders
Pathophysiology
Compensation Ventilation Controls [CO2] Kidneys Regulate [HCO3] Respiratory pathologies
lead to a 1
0
change in CO2 and in metabolic HCO3. f one changes the other compensates.
n.
Respiratory Acidosis the kidney increase [HCO3]. n acute condition the high CO2 drives
the carbonic anhydarse reaction towards the HCO3. n chronic conditions, there is an increase
secretion of H
+
by the Na/H+ exchange and increase re-absorption by Na HCO3 co-transport
Respiratory Alkalosis the same but opposite. There is a reduction in HCO3 production by
the Kidney.
Metabolic Acidosis there is a respiratory compensation to offload CO2. Stimulation of
peripheral chemoreceptor's increases depth and rate of breathing. The Kidney increase production
of HCO3. Acidosis stimulates the breakdown of glutamine acid (formed in liver; NH4
+
+HCO3
-
).
HCO3 is reabsorbed.
Metabolic Alkalosis is there isn't an maintaining factor, HCO3 will be secreted and the
alkalosis resolved. Low chloride maintains alkalosis.
Cl
-
is main anion used in exchange for HCO3
-
f Cl
-
is low HCO3
-
cant be re-absorbed
Cl
-
is reabsorbed with H
+
, is Cl
-
is low, less H
+
is reabsorbed
Potassium acidosis causes hyperkalaemia. n acidosis more
H
+
enters cells, to maintain electro-neutrality K
+
leaves cells.
n the Kidney (DCT) Aldosterone stimulates re-absorption of Na in exchange for K. n Acidosis H
+
is
exchanges with Na thus reducing the K excretion.
Hyperkalemia further stimulates Aldosterone.
Hypokalaemia promotes Alkalosis, because low K stimulates the
H/K ATPase exchanger leading to K reabsorption and H excretion
Promotes Na/HCO3 Co-transport leading to HCO3 absorption
IsmaiI Vokshi
Acid Base Balance and Disorders
Anion Gap Metabolic Acidosis is the difference between the measured cations and
anions in plasma. Plasma is always electrically neutral the difference is made up of unmeasured
anions e.g. proteins, organic acids, sulphate and phosphate (N: 6-16mmol/L).
Normal Anion Gap Acidosis= Loss of HCO3. Compensated by a rise in Cl reabsorption in
the kidney. Caused by:
Gut Bicarbonate Loss (Diarrhoea OR Drains in the Small ntestine, Pancreas or Biliary or Fistulae.
lleal Conduits, or Uretrosigmoidostomys = Hypokalemia and Acidosis. Na<->K and HCO3 <->Cl.
Urine > Na and Cl then K and HCO3).
Renal HCO3 Loss (Renal Tubular Acidosis).
ncrease NaCl ntake (Excess Saline nfusion Blood is normally slightly alkali, water slightly acidic.
Giving Water (Saline or Dextrose) without buffer will cause slight acidosis 'dilution acidosis'. Plasma
Cl is lower then Na. Giving NaCl will cause a proportionally bigger increase in Cl levels.
ncreased Anion Gap = Addition of New (Organic) Acid to the body, this uses up the HCO3
and Anions creating a gap, but there is NO compensatory rise in the level of Cl. Addition of non-
organic acids such as HCl. Cl replaces Anion Gap so its Normal.
Lactic Acidosis Very sick patients, haemodynamically shocked or septic inadequate tissue
oxygenation and impaired lactate metabolism poor liver perfusion.
Ketoacidosis B-hydroxybutyric acid and acetoacetic acid accumulate in diabetic patients, present in
urine and blood. Absence of nsulin Promotes Production, nhibits Catabolism. n People with DM
Typ2 (Non-nsulin Dependent) The Small amount of insulin present prevents this. Starvation and
Alcoholic Ketoacidosis produce excess ketoacids in urine and blood.
Toxic Alcohols Methanol and Ethylene Glycol (Antifreeze) cause a difference in predicted
osmolality and measured osmolality. The Alcohol Dehyrdogenase metabolises the alcohols into more
serious toxic metabolite. This can be prevented by saturating the enzyme with Ethanol, while the
toxic alcohol is removed via dialysis. Methanol Abd Pain, Vomiting, Headache, Visual Disturbances
or Blindness (Retinitis). Ethylene Glycol Same and acute or chronic renal failure but not Retinitis.
Aspirin ncrease Ventilation Respiratory Alkalosis. However Salicylic Acid then causes Metabolic
Acidosis. Also causes: tinnitus, nausea, hyperventilation, non-cardiogenic pulmonary oedema and an
elevated pro-thrombin time. Seizures and death when cerebral tissue levels are high.
Rare nborn Errors of metabolism e.g. aminoacidemia can produce metabolic acidosis after birth.
Failure of Acid Secretion Acute or Chronic Renal Failure Retention of phosphate, sulphate, and
organic anions. nitially there is buffering by bicarbonate and bone and intracellular buffers.
HORMONES
Aldosterone ncrease H+ excretion by stimulating H+ATPases in Distal Tubule
Angiotensin Promotes H+ secretion, stimulates Na/H exchange
Parathyroid Hormone Promotes HCO3 excretion via inhibiting Na/H+ exchangers
Catacholamines Promote Alkalosis
Anion Gap = ([Na
+
]+[K
+
])-([HCO
3
-
]+[CI
-
])
IsmaiI Vokshi
Acid Base Balance and Disorders
IsmaiI Vokshi
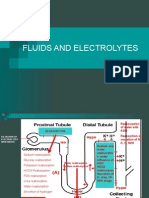
Fluid and Electrolyte Balance and Disorders
n normal persons, the total body water constitutes 50-60% of lean bodyweight in men
and 45-50% in women. n a healthy 70 kg male, total body water is approximately 42 L.
This is contained in three major compartments:
the intracellular fluid (28 L, about 35% of lean bodyweight)
the interstitial fluid that bathes the cells (9.4 L, about 12%)
plasma (4.6 L, about 4-5%).
Osmotic Pressuredetermines distribution of water among the three major compartments.
Conc of major solutes in these fluids differ, and each compartment has one solute that is primarily limited
to that compartment and therefore determines its osmotic pressure:
- K+ salts in the intra cellular fluid (most of the cell Mg2+ is bound and osmotically inactive),
- Na+ salts in the interstitial fluid
- Proteins in the plasma.
Plasma vol regulation is complicated because plasma proteins hold water in the vascular space by an
oncotic effect which is in part counterbalanced by the hydrostatic pressure in the capillary that is
generated
by cardiac contraction
ntravascular Volume Depletion
Caused: Trauma (Blood Loss, ECF Damaged Tissue) Surgery (Blood Loss, Loss of ECF)
Clinical features
Symptoms are variable. Thirst, muscle cramps, nausea and vomiting,
and postural dizziness may occur. Severe depletion of circulating volume causes hypotension and
impairs cerebral perfusion, causing confusion and eventual coma.
Signs can be
divided into those due to loss of interstitial fluid and those due to loss of circulating volume.
Loss of interstitial fluid leads to loss of skin elasticity ('turgor') - the rapidity with which the skin recoils to
normal after being pinched. Skin turgor decreases with age, particularly at the peripheries. The turgor
over
the anterior triangle of the neck or on the forehead is a very useful sign in all ages.
Loss of circulating volume leads to decreased pressure in the venous and (if severe) arterial
compartments.
Loss of up to 1 L of extracellular fluid in an adult may be compensated for by venoconstriction and may
cause no physical signs. Loss of more than this causes the following:
ntravascular Fluid Overload
Clinical features
Peripheral oedema - expansion of the extracellular volume by at least 2 L (15%) (ankles) Oedema may
be
in the face, particularly in the morning. n a patient in bed, oedema may accumulate in the sacral area.
Expansion of the interstitial volume also causes pulmonary oedema, pleural effusion, pericardial effusion
and ascites.
Expansion of the blood volume (overload) causes a raised jugular venous pressure, cardiomegaly,
added
heart sounds, basal crackles as well as a raised arterial blood pressure in certain circumstances.
IsmaiI Vokshi
Fluid and Electrolyte Balance and Disorders
Clinical Assessment of ntravascular Volume
Hypovolemia a fast and weak pulse, infrequent and low volume urination, dry mucous membranes,
poor
capillary Refill, decreased skin turgor, a pulse, orthostatic hypotension, cool extremities (e.g. cool
fingers)
Hypervolemia an elevated Jugular venous pressure (JVP)
Sodium and Potassium
What causes.
HYPONATREMA reflects hypoosmolality (Unless there is a fall on another electrolyte e.g.
Glucose). Excess Water retention in relation to Na. Loss of sotonic fluids = hypovolaemia
Triggers Thirst + ADH. F Na doesn't match Water ntake = Hyponatremia.
*with Normal ECV Eouvolaemic Generally Dilution Excess Water ntake
Kidneys unable to excrete it fast enough
- Abn ADH Release Vagal Neuropathy (nability to nhibit), Deficiency of ACTH or
Glucocorticoids (Addison's), Hypothyroidism, Severe Hypokalemia.
- SADH
- Major Psychiatric llness Psychogenic Polydipsia, Non-osmotic ADH Resease,
Antidepressant Therapy.
- ncreased Sensitivity to ADH Chlorpropamide, Tolbutamide
- ADH-like Substances Oxytocin, Desmopressin
- Stimulation by Osmotic Substances Glucose, Chronic Alcohol Abuse, Mannitol, Sick-
cell Syndrome (Leakage of ntracellular ons).
*with Decreased ECV Hypovolaemic When Vol falls Thirst and ADH
Renal Causes Na not conserved Urine Osmolality High. Non-Renal Causes Na
Conserved Urine Osmolality Low.
- Extra-Renal (Urinary Na <20mmol/L) Vomiting, Diarrhoea, Haemorrhage, Burns,
Pancreatitis
- Renal (Urinary Na >20mmol/L) - Osmotic Diuresis (Hyperglycaemia, Severe
Uraemia), Diuretics, Adrenocortical nsufficiency, Tubelo-nterstitial Renal Disease,
Unilateral Renal Artery Sternosis, Recovery Phase of Acute Tubular Necrosis
*with ncrease ECV Hypervolaemic
- Heart Failure, Liver Failure, Oliguric Renal Failure, Hypoalbuminaemia
PSEUDOHYPONATREMA Excess Plasma Protein or Lipid Na/L of Water is the
same, but Water/L or Plasma is reduced, due to increased lipid. Also if sample is from arm where
Low Na infusion is given.
Signs and Symptoms Possible None Features of Hypovolaemia Neuro Lethargy,
Confusion, Agitation, Nausea, Reduced Tendon Reflexes, Muscle Cramps, Seizures and Coma
(Na<120mmol)
HYPERNATREMA - These Occur Only When there is a Deficit of Water ntake
- ADH Deficiency Diabetes nsipidus
- atrogenic Administration of hypertonic Na Solutions
- nsensitivity to ADH (Nephrogenic Diabetes nsipidus) Lithium, Tetracyclines,
Amphotericin B, Acute Tubular Necrosis.
- Osmotic Diuresis Total Parenteral Nutrition, Hyperosmolar, Hyperglycaemmic state,.
- Other Excessive Water Loss (Skin and Lungs), Reliance on 0.9% (150mmol/L)
Saline for Volume replacement.
Clinical Features nausea, vomiting, confusion, polyuria, polydipsia.
IsmaiI Vokshi
Fluid and Electrolyte Balance and Disorders
Management
Hyponatremia No treatment for mild Hyponatremia Just correct the cause.
Hypovolaemic - Voume replacemnt sotonic Saline V expanders may be required is BP is
affected.
Eouvolaemic - Fluid restriction 500ml/24hrs so Serum Na = 130mmol/L
- Demeclocycline (Tetracycline Antibiotic) can be given to induce
partial nephrogenic diabetes insipidus. Alt. Furosemide, Oral NaCl 3g/day
Hypervolaemic - Furosemide +/- ACE nhibitors +/- Water Restriction <1L/24Hrs
n Emergency
Acute Situation - Acute Hyponatremia Symptoms Drowsiness, Convulsion, Coma ncrease
Serum Na 2mmol/L/Hour Up to 120mmol/L. Caused by large 5% Dextrose nfusion.
n Euvolaemic Patients - Avoid - Hypertonic Saline. f Necessary ncrease Serum Na by
<0.5mmol/L/24hrs and stop at 120mmol/L
Hypertonic Saline (3%, 513mmo/L) For patients with severe symptoms Fits or Coma
Slow nfusion <70mmol/hour ncrease 8-10mmol/L in first 4 hrs
There should not be 15-20mmol/L over 48hrs. Plasma Na Should not be corrected to
>125-130mmol/L.
1ml/kg of 3% Na Raise Plasma Na by 1mmol/L
ADH R Antagonists on Trials Tolvaptan
Caution: Hypertonic Na should not be given to Hypovolaemic patients Acute Heart failure Use
20% Mannitol instead.
Rate of nfusion 3% NaCl (ml/hr) = Kg x Desired Rate of Collection (mmol/L/hr)
Hypernatremia Treat the underlying cause.
Administer ADH Desmopressin. Remove any nephrogenic drugs e.g. Lithium
n Severe (>170mmol/L) Give 0.9% NaCl (150mmol/L) nitially
Less Severe (>150mmol/L) 5% Dextrose or 0.45% NaCl (Presfered in Hyperosmolar Diabetic
Coma)
HYPOKALAEMA
ncreased Renal Excretion Urinary K >20mmol/day Diuretics Thiazides, Loop Diuretics
ncreased Aldosterone Secretion Liver and Heart Failure, Nephrotic Syndrome, Cushing's
Syndrome, Conn's Syndrome, ACTH-producing Tumours
Exogenous Mineralocortacoid Corticosteroids, Carbenoxolone, Liquorice (Potentiates Renal
Actions of Cortisol)
Renal Disease Renal Tubular Acidosis (Typ1+2), Renal Tubular Damage (Diuretic Phase), Acute
Leukaemia, Nephrotoxicity (Amphoterecin, Aminoglycosides, Cytotoxic Drugs), Release of Urinary
Tract Obstruction,
Syndromes Bartter's, Liddle's, Gitelman's
Reduced ntake of K
+
- ntravenous Fluids Without K
+
, Dietary Deficiency
Redistribution nto Cells B-Adrenergic Stimulation, Acute M, B-Agonistis (Fenoterol,
Salbutamol), nsulin Treatment (Treatment of Diabetic Ketoacidosis)
Correction of Megaloblastic Anaemia (B12 Deficiency), Alkalosis, Hypokalaemic Periodic
Paralysis.
G Loss Urinary K <20mmol/day Vomiting, Severe Diarrhoea, Purgative Abuse, Villous
Adenoma, leostomy or Uterosigmoidostomy, Fistulae, leus/ ntestinal Obstruction.
Clinical Features
Mild Asymptomatic Severe
IsmaiI Vokshi
Fluid and Electrolyte Balance and Disorders
When K<2.5mmol/L Serious Neuromuscular Problems Emerge ncluding, Paralysis,
Paraesthesia, Tetany
Management Treat the Cause, Stop Diuretics Can start K Sparing Diuretic, Measure Mg f
patient hypomagnesaemic K imbalance will not correct. Give Oral K Supplements. f metabolic
alkalosis KHCO can be given. Administer V K if: Cardiac Arrhythmias, Muscle Weakness, Severe
DKA.
ncrease intake of fresh fruit/ vegetables or oral K supplements (20-40mmol/day) Can cause G
irritation
Hyperaldosteronism (Cirrhosis, Thiazide Therapy) Spironolactone/Eplerenone K Sparing Diuretics
V Fluid Replacement Add 20mmol of K/L Monitor.
HYPERKALAEMA Acute self limiting Hyperkalaemia after exercise. This is normal. t is caused
by increased release from cells or decreased agreement. Renal mpairment and Drug nterference.
Drugs: ACE nhibitors with K Sparing Diuretics Dangerous
Decreased Excretion Renal Failure, Drugs (Amiloride, Spironolactone/Eplerenone, ACE
nhibitors, NSAD's,) Ciclosporin and Heparin Treatment, Aldoserone Deficiency, Hyporeninaemic,
Adison's Disease, Acidosis, Gordons Syndrome.
ncreased Release (reduced Na/K ATPase activity) Acidosis, Diabetic Ketoacidosis,
Rhabdomyolysis, Tumour Lysis, Succinylcholine, Digoxin Poisioning, Vigorous Exercise,
ncreased Extranous Load KCl, Salt Substitutes, Transfussion of Stored Blood
Spurious ncreased nvitro Relases (Abnormal Cells), Leukaemia, nfectious Mononucleosis,
Thrombocytosis, Familial (Pseudohyperkalaemia e.g. Haemolysis in Syringe), ncreased release
from muscle, vigorous fist clenching during phlebotomy.
Clinical Features When >7mmol/L Emergency Sudden Cardiac Death
Symptoms: Muscle Weakness, Kussmaul Breathing (Acidosis), Cardiac Shock (Low HR, Low BP)
Management Monitor the heart. V Ca Gluconate ( High K nactivates Cardiac Na Channels , Ca
Protects the Channels from K). nsulin and Glucose nsulin Driver K into Cells Up regulates:
Na/K ATPase. Glucose prevents hypoglycaemia. 1.26% Hypertonic NaHCO3 (Correct Severe
Acidosis pH<6.9).
Use of B2 Agonists, which drive K into cells is controversial. n Renal Failure Renal Dialysis,
Diuretics can also be used to take off more K (n long term). Polystyrene Sulphonate Resins,
Orally and Rectally to absorb K.
IsmaiI Vokshi
Fluid and Electrolyte Balance and Disorders
ECG Changes in..
Potassium
Hyper: Loss of P wave and ST Segment. Tented T wave, Broad QRS
Hypo: Flattened T wave, ST Depression, Prolonged PR QT ntervals, Tall U Waves, Atrial Arrhythmia,
Ventricular Tachycardia or Fibrillation - ncreases Automicity, Delays Repolarisation or Cardiac
Cells Predisposes to Arrhythmias e.g. ectopic beats, AF + VF
Sodium Does not affect ECG
Calcium
Hyper: Shortens QT Hypo: Long QT
Oral K Replacement
A 0.3mmol/L Serum K Reduction = 100mmol/L K Deficit in Body Stores
Foods High in K Bananas, Potatoes and Chocolate.
Supplements 40-120mmol/L KCl (Sando-K, Slow-K) When P is also depleted (Liver Cirrhosis, DKA),
K Phosphate can be given. When in Acidosis, KHCO3 can be given, e.g. distal renal tubular
acidosis.
n Severe Hypokalaemia (Arrhythmias, DKA) K <2.6mmol/L V KCl can be given. Heart should be
monitored. KCl conc. should not exceed 40mmo/L or 60mmol/L in emergency at 20mmol/hr. Bolus
nfusion can be fatal.
Side Effects + Complications
Emetic Taste and Effervescent, Slow-K tablets Very Large G Ulcerations (take with water while
standing). Overdose fatal arrhythmias, cardiac arrest (ntentional use in cardioplegia). Risk: CHF,
HD, Digoxin, DKA.
Muscle weakness, flaccid paralysilysis, rhabdomyolysis, nephrogenic diabeter insipidus, metabolic
alkalosis (incease HCO3 abstrption and Cl excretion). Paralytic leus, Hepatic Encephalopathy in
cirrhosis, chronic hypokalaemia in hypertension.
IsmaiI Vokshi
Fluid and Electrolyte Balance and Disorders
atrogenic Electrolyte Disorders
Diuretics can cause both Hyponatraemia and Hypokalaemia. Overgenerous use of 5% glucose solution
can
cause a dilutional euvolaemic hyponatramia.
Sodium
Hyper: Drugs with a high Na content e.g. piperacillin can cause
Potassium
Hyper: Potassium supplements, potassium-sparing diuretics, Spironolactone + ACE inhibitors. Other
drugs, which precipitate renal failure: Amiloride, Teiamterene, Spironolactone, ACE inhibitors,
NSAD's. B-Blockers block adrenaline from stimulating K reuptake. Others digoxin,
succinylcholine, and digitalis glycoside, Ciclosporin and heparin
Hypo: Exogenous mineralocorticoids (corticosteroids) e.g. carbenoxolone, high licorice in diet
Creatine clearance and GFR
To estimate the flow across the glomerulus, it is necessary to measure the clearance
of a substance which is freely filtered across the glomerulus and not reabsorbed
at all.
nulin fulfils this requirement exactly. Some Creatinine is in however actively secreted
into the tubule and so creatinine clearance rate slightly over estimates GFR. This
effect is exaggerated when renal function is impaired.
Diagnosing fluid and Electrolyte Disorders
Hyponatramia = Plasma Hypoosmolality. f the patient is Hypovolaemic and the losses are not through
the
Kidney, urine will not be concentrated.
Euvolaemic + Conc Urine = SADH (Another ADH Disorder)
Euvolaemic + Dilute Urine = H2O Overload, Hypothiroidism, Glucocorticoid Deficiency
Hypernatramia = Hyperosmolality
f urine osmolality is lower than the plasma = Diabetes nsipidus
f urine osmolality is high = Osmotic Diuresis
Potassium Balance
K = ntracellular Cation. mportant in electrical membrane potentials. Found in Muscle. K Levels Detected
by
Pancreas and Adrenals. K Levels altered by nsulin Drives K nto Cells and Aldosterone ncreases
Excretion. nsulin NOT responsible for homeostatic balance of K. K responds directly to acidosis and
alkalosis.
IsmaiI Vokshi
Urinary Tract nfections
Definitions
Bacteriuria - Presence of bacteria in the urine.
Urinary tract infection (UT) - Symptoms and Sig. Bacteruria 105 cfu/ml Kidney to Bladder.
Lower UT - Cystitis
Upper UT - Pyelitis and Pyelonephritis
Recurrent UT - Relapse or Re-infection. Number varies with age and sex.
Uncomplicated UT - nfection of the urinary tract by a usual pathogen in a person with a
normal urinary tract and with normal kidney function.
Complicated UT - anatomical, functional, or pharmacological factors predispose the person to
persistent infection, recurrent infection or treatment failure e.g. abnormal urinary tract.
52% - 90% Men with UT have prostatic involvement = Prostatic Abscesses or Prostatitis.
Microbiology
Common - Gram ve Enterics; scherichia coli, Staphylococcus saprophyticus, Proteus mirabilis
Rare mmuno Supressed or Catheterised; Klebsiella spp., Proteus Vulgaris, Candida Albicans,
Pseudomonas spp.
Risk Factors; Female, Antibiotic Use, Recent Sexual Activity, New Sexual Partner, Use of
Spermicide,
Diabetes, Presence of Catheter, nstitutionalisation, Pregnancy possible pregnancy should be sought in
women of child-bearing age
Clinical Features of Lower UT - Dysuria (burning on passing urine), Frequency (frequent need to
pass
urine), Urgency (compelling need to urinate), Urine can be cloudy with an offensive odour, Older men,
generalised symptoms such as confusion and incontinence can be present. Haematuria, Urinary
ncontinence, Suprapubic Pain, Acute Confusional State in older people especially.
Clinical Features of Upper UT (Ureter and Kidney) - Rapid onset over 1-2 days. There are
symptoms same as lower tract symptoms plus loin, back or suprapubic pain, fever and chills, nausea
and
vomiting. The patient may become septic showing increased Heart and respiratory rate, and lowered BP.
IsmaiI Vokshi
Urinary Tract nfections
Causes/Differential Diagnosis of Dysuria
Abdominal causes: Appendicitis and Ectopic Pregnancy (Due to rritation of Nearby Urinary
Structures).
Urinary tract causes: Bacterial UT, Urethritis, e.g. Chlamydia, Gonococcus or Non-Gonococcal
Urethritis;
in men aged <35, this is a common cause of dysuria, Urinary schistosomiasis, nterstitial cystitis,
Obstruction: prostatic enlargement, Urethral Stricture, Kidney stones in bladder or urethra,
Malignancy,
e.g. carcinoma of the bladder or urethral tumours.
Genital causes: Urethral or vaginal trauma, including sexual abuse or a foreign body, Genital herpes
simplex, Women: vaginitis, e.g. vaginal candidiasis, atrophic vaginitis, bacterial vaginosis ,
Men: prostatitis, epididymo-orchitis, epididymitis
Other disease: Spondyloarthropathy, e.g. Reiter's syndrome or Behcet's disease, Compression from
a pelvic mass
rritants: Drugs, e.g. cyclophosphamide, allopurinol, danazol, tiaprofenic acid, and possibly other
nonsteroidal anti-inflammatory drugs, Chemical irritants: allergic or irritant reaction to soaps, vaginal
lubricants, spermicides, contraceptive foams and sponges, tampons and toilet paper, Mechanical
irritation,
e.g. from a poorly fitting contraceptive diaphragm or vaginal ring pessary, Radiation or chemical
exposure.
nvestigations
Lower - Dipstick Urine - Treat as bacterial if + for nitrite and/or leukocytes.
Urine microscopy - Leukocytes indicate presence of infection.
Urine culture - Exclude Diagnosis or if high risk e.g. pregnant, immunosuppressed, renal tract
anomaly or
if failed to respond to earlier empirical treatment. Urine culture should always be performed in men with a
history suggestive of UT regardless of the results of the dipstick test. Urine culture is not required for
symptomatic lower UT in non-pregnant Women. Upper (Pyelonephritis)
Urinalysis: Cloudy with Offensive Smell. Urine dipstick +ve for blood, protein, leucocyte esterase and
nitrite. MSU should be sent off for microscopy and culture
nflammatory markers: CRP, ESR, Plasma Viscosity = Raised.
One study found that if a dimercaptosuccinic acid scintigraphy (DMSA scan) is not available (see
below), it is
reasonable to treat a Febrile UT as acute pyelonephritis if the CRP is >66.4 mg/L in a patient with >2
days
of fever or if the CRP is >27.3 mg/L in a patient febrile for >2 days.
Full blood count: this shows elevated white cell count with neutrophilia.
Blood cultures: these are positive in approximately 12-20% of patients with Pyelonephritis.
maging: Ultrasound is first-line in all patients with recurrent pyelonephritis and may help to identify
obstruction or stones. Contrast-enhanced helical/spiral CT scan (CECT) is the best investigation in
adults
where diagnosis is in doubt or deterioration occurs. DMSA scan is preferred in children where making
the
diagnosis is often more difficult an V injection of a radioactive gamma emmiter is given. Kidneys and
ureters are visualised using a gamma camera
The Fairley Test: this is used to determine whether infection is confined to the bladder or has spread
IsmaiI Vokshi
Urinary Tract nfections
Recurrent - nvestigations
Primary care - MSU Culture, Microscopy (Esp. in Children). US for anatomical anomalies.
Secondary care maging in Children (Age Related). DMSA Scanning Demonstrate Renal Function.
Cystography = Vesicoureteric Reflux (ndirect Nuclide Cystography).
Management
Uncomplicated Lower - General - Risk factors for Recurrent nfection. These nclude: Use of
Spermicide,
Frequent Sexual ntercourse, New Sexual Partner. Drink Plenty of Fluids. Cranberry Juice Treat &
Prevent
Pharmacological Trimethoprim. Nitrofurantoin and Cafalexin if Allergic, Topic Oestrogen in Post
Menopausal , Prophylactic Antibiotics if Associated with Sexual ntercourse. Paracetamol + NSADS for
Symptom Relief.
Acute Pyelonephritis
Mild - First-line therapy in mild cases of uncomplicated pyelonephritis is an OraI FIuoroquinoIone for
7
Days in areas where the rate of Fluoroquinolone-resistant . coli is still low i.e. <10%. Support: Rest,
Adequate Fluid ntake and Analgesia
Severe - HospitaI Admission: Healthy Patients Treated n Community. Admission for Pregnant
Women.
ndications: Severe Vomiting, Co-morbidity (Diabetes), Signs of Sepsis (Tachypnoea, Tachycardia,
Hypotension), Dehydration, Severe Pain/Debility, No Response to Treatment, UT Obstruction, Oliguria/
Anuria, Suspected Complications, Uncertain Diagnosis, Social ssues, Non-Concordance with
Treatment,
nadequate Access to Follow-up, Relapse of Symptoms after Antibiotics.
Antibiotics
Adults Ciprofloxacin(250-500mg PO BD 7days) or Co-Amoxiclav(500mg BD PO or 250
mg
PO 8-hrly 14days).
Kids V Antibiotics = Renal Scaring. Oral Cefixime or Short Courses (2-4 days) of V Therapy
Followed by
Oral Therapy. V Therapy: Cephalosporin Single Daily dosing, AminogIycosides added if there is no
improvement.
Surgery: Drain Renal or Periphrenic Abscesses, or Relieve Obstructions e.g. stones.
Genito-Urinary History
Presenting complaint may include the following symptoms and associated symptoms
Symptoms - Frequency, Nocturia (at night), Dysuria (pain on urinating), Polyuria (large
amount of urine) - Diabetes mellitus, diabetes insipidus, psychogenic, addison's, Oliguria (small amount
of
urine) Low luid intake, loss of renal function, anuria total obstruction, spinal damage, Haematuria
(presence of blood) ask if the female is menstruating, find out of blood is whole or more mixed in to
urine,
pneumaturia vesicocolic fistula, Stream, ncontinence, Urine colour and smell, Hesitancy (in male
patients: difficulty in starting), Urgency, Terminal dribbling (in male patients), Discharge (vaginal/
IsmaiI Vokshi
Urinary Tract nfections
Associated Symptoms - Pain (Suprapubic/ Loin/ Perineum/ Testis in Males), Fever, Anorexia,
Metallic
taste on eating, Fatigue, nsomnia, Hiccoughs, tching, Bruising, Oedema, Vomiting, Dry Mouth, Postural
Faintness, Cramp
HPC
Pain - Site - Renal Angle Pain Arises directly from kidney/Renal capsule | Renal Colic From the
Ureter
Supra Pubic Pain - From Bladder
- Onset/Character - Constant with Fever, Nausea, Chills Pyelonephritis |
Dull Chronic Pain Chronic nfection, scarring from Vesico Ureteric Refulx, PKD |
Dull Non-Localised Pain Glomerulonephritis, Stones |
Sudden Onset, Severe Obstruction (Renal Colic) |
Voiding Pain (Dysuria) with frequency Cystitis |
Testicular Pain Consider Tortion/ Strangulated Hernias
Storage Symptoms associated with bladder, prostate or urethral problems, e.g. lower urinary tract
infection, tumour, urinary stones or urinary tract obstruction, neuro problems, frequency, urgency,
nocturia
Voiding Symptoms obstruction such as due to BPH Hesitancy and intermittency
Post Micturition terminal dribbling may indicate BPH or Detrusor weakness
ncontinence Urge (Detrusor nstability), Stress (Pelvic Floor Weakness), Overflow (BPH), Constant
(Fistula). Ask: When, Frequency, Night, How many pads (Damp, Wet, Soaked), Enuresis (During Sleep),
Other
Symptoms, Provocative (Coughing, Sneezing, Exercising), PMH (Obstetric + Surgical), mpact on Daily
Living.
Causes of Urinary ncontinence - Degenerative Brain Diseases and Stroke, Spinal Cord Damage,
Neurological Diseases, e.g. Multiple Sclerosis, Pelvic Floor Weakness (Following Childbirth, Pelvic
Surgery,
Radiotherapy), Bladder Outlet Obstruction, UT, Detrusor nstability
PMH
Previous History of Renal System Disease, Specifically: HTN, DM (Neuropathy, Renovascular Disease),
CVS
Disease, UT Stones or Surgery, Recurrent nfection (UT Renal Scaring, URT Glomerulonephritis +
Vasculitis), Anaemia
Drug Hx
Drugs Accumulate in Renal Failure: Digoxin, Lithium, Aminoglycosides, Opioids, -Blockers, e.g.
Atenolol
Drugs Affect Renal Function: ACE nhibitors, AR blockers, and NSADs, Aminoglycosides,
Amphotericin, Lithium, Ciclosporin, Tacrolimus and, in overdose, Paracetamol is toxic to Kidneys,
Statins
can harm renal function because they can cause myositis leading to rhabdomyolysis.
IsmaiI Vokshi
Urinary Tract nfections
FHx
SHx
End-Stage Renal Failure Requiring Dialysis and/or transplantation has implications for Lifestyle,
Employment and Relationships. ncontinence: mplications for Daily Living. Find out about: Feelings,
deas,
Functioning and Expectations.
Smoking and Alcohol | Dietary Relevant to Stones | Occupation Hot Conditions (Sweating a Lot),
Toxic
Solvent Exposure
IsmaiI Vokshi
Renal Stones
Symptoms
Embedded in Kidney - Asymptomatic. Calyx System Stone Dull Loin Pain.
Pelvi-ureteric Junction - Ureteric Colic, Continuous, Sharp Exacerbations, Vomiting and Sweating.
Sudden Onset, Uncomfortable
Stone in Mid Ureter - Mimics Appendicitis or Diverticulitis.
Calyceal Stones - Asymptomatic.
Staghorn Calculi - Loin Pain, Upper UT.
Ureteric Colic - Peristalsis Proximal to Obstruction. Pain size of stone, loin to groin and into
testes/labia.
Gross/microscopic haematuria. Bladder stone sudden interruption of urinary stream, perineal pain, pain
at
tip penis.
Renal Obstruction: Pyonephrosis and Distension of Kidney, Pyelonephritis, Hydronephrosis.
Pelvi-ureteric Obstruction: Renal Colic, Haematuria, Hydronephrosis, Pyelonephritis
Vesico-ureteric Obstruction: Renal Colic, Haematuria, Hydronephrosis.
Bladder rritation: Haematuria, Frequency, Pain.
Bladder Outflow Obstruction: Acute Retention, Haematuria.
O/E - Normal, Renal Angle Percussion Tenderness (Retroperitoneal nflammation)
Dipstick: Haematuria in 90%, Confirm with microscopy.
Epidemiology: Common, lifetime incidence up to 15%. M:F 3:1. Early adult life. 3% Prev Europeans.
DD Loin Pain: AAA, appendicitis, Pyelonephritis, Diverticulitis, Gynae Causes.
Pathophysiology and Risk Factors - Hypercalciuria 65%. Ca Stones related to
Hyperparathyroidism,
Renal Tubular Acidosis = Medullary Sponge Kidney. Acidic urine ppts calcium oxalate and urate stones;
Alkaline phosphate stones.
Nucleation Theory: Crystal/foreign body as nucleus for crystallization of supersaturated urine.
Stone Matrix Theory: Protein matrix secreted by renal tubular cells acts as scaffold for crystallisation
of
supersaturated urine.
Reduced nhibition Theory: Reduced Urinary levels of naturally occurring inhibitors of
crystallization.
Dehydration - nfection: staghorm triple phosphate calculi formed by action of urease producing
Proteus, Klebsiella, Produces Ammonia -> alkaline urine stones.
Schistosomiasis Bladder Stones and Cancer.
Staghorm Stones are Large, fill renal pelvis and calices recurring Pyelonephritis, renal Parenchymal
damage. Other stones range from few mm to 1-2cm. Obstruction. Calyceal stones Haematuria
Bladder Stones - nfection. Chronically Sqamous Carcinoma of Bladder.
maging USS: pregnant, asthmatic, atopic so unsuitable for contast in VU. Can give VU with
steroid
cover. Baseline KUB Xray: 90% renal stones radio-opaque (urate stones translucent). 90% gallstones
radio-
lucent. VU in A+E: Check common obstruction sites: Pelviureteric junction, SJ, Vesicoureteric junction.
Block -> standing column of contrast above block, dilated renal pelvis, blunting of calyces.
PhIeboIiths (calcification of veins) common in this ares- multiple more rounded, radioluscent centre.
IsmaiI Vokshi
Renal Stones
Blood and Urine Tests
Bloods: renal function, screen Ca, urate, phosphate levels in recurrent episodes.
24h Urine Collection, sieve to find stone. Analyse urine collection.
Management
nvestigations: FBC, U+E, serum creatinine, Ca,Phosphate, proteins and alk phos, urate.
-Urine microscopy for haematuria and crystals.
-urine culture: secondary infection
-plain AXR, VU
-renogram: staghorm calculi- assess renal function.
Analgesia: pethidine injection, or NSADs (rectal diclofenac) for ureteric colic.
Lots of fIuids (Vif cant take in orally).
Abx if infection: cefuroxime V.
VU: Venflon radiopaque contast injected. Film at 5min, another after micturition. f abnormal
delayed
film 1hr taken. Futher films until contast seen down to level of obstruction. 1,2,4,8,24hrs as necessary.
f pain resolves, not obstructed on VU home and oral analgesia, with urology clinic appmt.
f pain persists, kidney obstructed admit.
f obstructed kidney and dev fever, loin pain damage to kidney if not drained urgently. Abx, urgent
nephrostomy tube insertion to drain percutaneously.
Treatment size and position dependant
Renal: ESWL (Lithotripters use piezoelectrically generated ultrasound shock waves to shatter stone,
under image-intensifying control.) if <2cm in kidney. Small fragments passed spontaneously ->
acute colic.
Or percutaneous nephrostomy if >2cm or calyceal obstruction.
Lower poles of kidney hard to use ESWL flexi nephroscopy and laser ablation.
Upper 1/3 ureter: ESWL if <1cm, per cutaneous if >1cm.
Middle 1/3 ureter: difficult region as hard to visualise due to iliac bone/sacrum for ESWL. Too high for
retrograde ureteroscopy. Extracorporeal shock wave lithotripsy can still be used by adjusting position.
Sometimes can push stone back up and use ESWL. Day case/outpt.
Lower 1/3 ureter: uretero-rhinoscopy, contact lithotripsy or extraction with Dormia basket.
Bladder: ureteroscopy- endoscopic up ureter retrieval in wire basket or fragmented with pneumatic
instrument (lithoclast ie mechanical lithotrypsy) or laser Or open.
Percutaneous Nephrolithotomy: for large stones and staghorn. Ultrasound or fluoroscopic guided
needle inserted into calyx. Guide wire passed down needed into ureter, needle removed. Series of
dilators
inserted over guide wire to create tract to renal pelvis. Stone fragmented under direct vision and
fragments
removed.
Open surgery: Ureterolithotomy for impacted ureteric stone. Nephrolithotomy. Bladder stones.
Nephrectomy if irreparable damage to kidney.
IsmaiI Vokshi
Renal Stones
Role MDT: Urologist, radiologist, physician in Diagnosis and Managemnt.
Prevent Renal Stone.
Hydration, if urate (cut down cheese, port), prevent UTs (cranberry juice, early abx),
Thiazide diuretic if hypercalciuria to reduce Ca excretion.
Normal Ca intake low intake stimulates oxalate secretion.
Avoid high oxalate foods e.g. strawberries, rhubarb, leafy veg, tea, beetroot. (High oxalate also
complication
of losing terminal ileum). Pyridoxine.
Treat UT if phosophate stone.
Urate - Allopurinol, Urine Alkalinzation.
Cysteine - vigorous hydration to keep urine output >3L/d and urinary alkalinisation. D-penicillamine to
Chelate Cystine + Pyridoxine to prevent vitamin B6 deficit
nfected Obstructed Kidney and Percut Nephrostomy
Back pressure hydronephrosis. nfection (fever, loint tender, pyruria) and permanent loss of renal
function.
Acute calculous anuria if both ureters blocked.
Patient Maybe Uraemic Haemo/Peritoneal Dialysis
IsmaiI Vokshi
Acute Renal Failure
Classification
Prerenal Decreased Renal Perfusion
- Volume Deficit - Haemorrhage, Low ntake, Burns, Diuretics, G Loss, Third Space Fluids
(Pancreatitis, Peritonitis), Sweating, Osmotic Siuresis (Diabetes), Low Aldosterone (Addison's)
- CVS CHF, Pericardial Disease (Constrictive Pericarditis, Tamponade), Coarctation of Aorta
- Decreases Oncotic Pressure (Decreased Albumin) Nephrotic Syndrome, Catabolic States
- Decreased Sytemic Vascular Resistance (Shock) Spesis (Bacterial, Anaphalactic,
Neurogenic, Cardiogenic)
- Hepatorenal Sydnrome Kidney Disease 2
o
to Liver Disease (Normal Kidneys)
- Renal Artery Stenosis ACE inhibitors
Postrenal (5%) Obstruction to the flow of urine
- Staghorn calculus, Neoplasm, Clot in Ureter, Prostatic Hyperplasia, Strictures, Neurogenic
Bladder, Urethral Obstruction
ntrarenal
Tubulointerstitial
schemic Acute Tubular Necrosis schemia with toxic component. Hypotension (60% Surgical
40% Medical; Duration is critical, High Duration = High ncidence), Toxins, Contrast, Drugs,
Pigments (Rhabdomyolysis)
- Presentations Three Phases. Prodromal (Time from insult Renal failure), Oligouric (<400cc/d)
Anuric (<100cc/d), Postoliguric (Diuresis, Recovery Phase, Loss of Retained Fluid)
- Prerenal vs ATN
- Prerenal: Urine osm >500 | Urine Na
+
<20 | Fe Na
+
<1% | Urine Sediment Scant
- ATN: Urine osm <350 | Urine Na
+
>40 | Fe Na
+
>1% | Urine Sediment Full (Brownish
pigmented granular casts, epithelial casts)
n ATN Urine cannot concentrate. Prerenal you hold all free H
2
O and Na
+
.
Allergic nterstitial Nephritis Drugs (Also cause allergic reactions) NSADs, Penicillins,
Sulfonamides (Antibiotics + Diurestics; Thiarides, Furosemide, Acetazolamide), Tuberculosis
medication (Rifampin), Allopurinol (Also associated with hepatic injury). nfections any origin,
viral, bacterial or fungal.
Diagnosis Fever, Rash, Eosinophilia, Eosinouria, Hematuria, Proteinuria (<2g/24h). Biopsy
Normal glomeruli, with nterstitial Oedema and Eosinophils.
Treatment Stop Allergen, Steroids may help. Disease is normally self limiting.
Pigments (Haemo/Myoglobin) Haemoglobinuria from Haemolysis (ABO ncompatible
Transfusion), Myoglobinuria (Rhabdomyolysis). ATN occurs 2
o
to precipitation of pigment in
tubules and direct toxic injury.
Proteins (Myeloma Bence-Jones Protein) Nephrotic Syndrome
Crystals Oxalate Primary Hyperoxaluria, Ethylene glycol (Antifreeze) ingestion Anion gap
acidosis. Diagnosis Oxalate crystals in urine. Treat with alcohol (competes with ADH) and
dialysis. Urate Secondary to Tumour Lysis Syndrome, Chemo, Haematologic Malignancies and
Gout. Urate precipitates in an acidic environment (Opposite of Oxalate). Treat with allopurinol,
hydration and alkalisation of urine.
Hypercalcaemia Tubular epithelal damage, distal RTA, nephrogenic D
IsmaiI Vokshi
Acute Renal Failure
Toxins
Analgesics (2-10% in US and 20% AU End Stage Renal Disease). F:M 5:1. Phenacetin and
Aspirin (esp. in combination). nhibition of Prostaglandins Dilate afferent arteriole and increase
renal blood flow + renal papillary necrosis.
NSADs Combination of nterstitial nephritis, direct toxic effect, papillary necrosis, inhibition of
vasodilators (Prostaglandins)
Diagnosis Sterile Urine, Haematuria, Flank Pain, Mild Proteinuria, History (1g/d ; 1-3 yrs)
D/D; Papillary Nexrosis Analgesics, Diabetes, Sickle Cell Disease, Urinary Obstruction, Chronic
Pyelonephritis. Treatment; Non-specific
Amionoglycosides Renal Failure in 10-30%. Associated with Hypokalaemia and
Hypomagnesaemia. t is Non-oliogouric Disease (5-7d after Continuous Exposure)
Caphalosporin/Tetracycline
Amphotericin B: Nephrogenic D, Renal Tubular Acidosis. ncrease Blood Urea Nitrogen,
Creatinine, K wasting.
Contrast Agents V. Common. esp. with increase age, DM, dehyrdation, myeloma, baseline renal
disease. 2
o
to tubular damage, hypertonicity, intense vasoconstriction, tubular precipitation
Atheroembolic disease repeat cardiac procedures catheterisation, eosinouria.
Antineoplastics Cisplatin, methotrexate, cyclospornins, mitomycin
Radiation doses >2000 rads to kidneys
Metals Pb, Hg, Ag, Li (Nephrogenic D)
Cyclosporine
Treatment: Fluids, Diuretics, Dopamine and reduced protein intake.
Vascular
Wegeners Granulomatosis a form of polyarteriosis nodosa that has granulomas. Renal/Pulmonary
Disease. Presents; Haemoptysis, Sinusitis, Oral Lesions, Otitis. Presnece of Anti-neutrophil
cytoplasmic antibodies (ANCA). Treat: Cytotoxics and Steroids
Henoch-Schonelin Purpura Purpura, Arthralgias, G nvolvemnt (Colic and Bleeding), Renal Failure
and Fever. Haematouria and Proteinuria without oedema or HTN. gA deposition disease like
Berger but has extra renal involvement. No Specific treatment. Treated with steroids in severe
refractory cases.
Polyarteritis Nodosa Vascular inflammation and destruction lads to glomerular ischemia. Treat:
Steroids and Cytotoxics like most vasculitides pANCA.
Thrombotic Thrombocytopenic Purpura (Adults) + Haemolytic Uremic Syndrome (Children) Renal
failure, Microangiographic haemolytic anaemia, Decreased platelets (Thrombotic thombocytopenic
purpura (Fever and Neurologic changes)). Treat: HUS self limiting. Steroids in severe cases.
TTP plasmapheresis and steroids
Cryoglobulins gM and gG Deposition Treat with Plasma Exchange.
Hypertension End stage renal disease.
Diabetes see Nephrotic Syndrome
IsmaiI Vokshi
Acute Renal Failure
Glomerular
Acute Glomerulonephritis
Post-infectious Any agent (Bacteria, Virus, Rickettsia, Protozoans. GrpA B-Haemolytic
Sterptococci most common. Present; 10d-weeks after pharyngitis or strep skin infection, smoky
urine (haematuria and proteinuria, HTN, Oedema (esp. periorbital). Course self-limiting, resolves
weeks-months.
Diagnosis Elevated ASLO (anti-streptolysin O) and AHT (anti-hyaluronidase), Decrease
Compiment 3 together with clincal presentation. Biopsy seldom necessary.
Treatemnt Symptomatic, control HTN and fluid retention
Systemic Lupus Erthematosus (Covered in rheumatology) variable presentation; from
chronic, asymptomatic proteinuria to rapidly progressive glomerulonephritis and need for dialysis.
Goodpasture Syndrome diopathic disorder Ab agains basemnt membranes. Present;
exclusively pulmonary and renal, haematuria and haemoptysis. Diagnosis: Rising createnine and
blood urea nitrogen, worsening chest x-ray, proteinureas confrimed by anti-basemnt membrane
Ab. Treat - Plasmapheresis to remove circulating Ab, with steroids and cyclophosphamide.
diopathic Rapidly Progressive Glomerulonephritis assoicated with numerous crescent
formation, acute renal failure, positive ANCA without immune deposistis. Severe disease that has
limited response to steroids.
gA Nephropathy (Berger Disease) Disease of the young (<35). Often following viral illness,
characterised by haematuria, increase serum gA and gA deposition in the skin. Similar to
Henoch-Schonlein Purpura, but with renal manifestations only.
Alport Syndrome Hereditary, renal failure with hearing loss and ocular defects.
*Nephrotic Syndrome can be caused by all vascular and glomerular diseases. DM, Amyloid,
Multiple Myeloma; systemic diseases which can cause renal abnormalities that can lead to
nephrotic syndrome. These are the main cause in adults. n children this represents only 1/10 of
the causes. The rest are diopathic:
Nil lesion - 90% Child, 15% Adult Nerphrotic Syndrome. Histologicaly, only EM
fusion of foot processes of podocytes are fused. No mmune Deposition. Treat with steroids (80%)
v. effective.
Membranous Nephropathy (most common idiopathic in adults) mmune Deposits
presents so steriods don't help (20%). Can be 2
o
to SLE, Cancer or Drugs (Ag, Penicillamine)
Mambranoproliferative characterised by immune deposits and low complement.
Assoc. with Hep C.
Mesangial
Focal Segmental Glomerulosclerosis Heroin Nephropathy and ADS. Presents with
Haematuria and increaseing BUN/ Createnine. Low (20%) response to Steroids. So cyctotoxic
drugs are used. ESRD progression over 5-10yrs.
Presents: Proteinuria (>3.5g/d), Hypoalbuminaemia (2
o
to previous), Oedema, Hyperlipidaemia,
Hyperlipiuria, (Hypercoagulability occurs 2
o
to Antithrombin loss), treated with Heparin and
Coumadin (Warfrin).
Diagnosis: 24hr Urine Sample (Document massive proteinuria), Raising BUN/ Creatinine, Biposy
to differentiate between the 5 idopathic types.
Treatment: Steroids are best initially. They respond differently. Cyclophosphamide, also Na
restriction, diuretics, statins for lipid elevation.
IsmaiI Vokshi
End-Stage Renal Disease
Etiology: African Americans > Whites, DM (30%), HTN (25%), Glomerulonephtitis (15%), Unknown
(15%), Cystic Disease (4%), Other (11%).
Clinical Signs:
Hyperkalaemia,
Hypocalcaemia/ Hyperphosphataemia 2
o
to reduced 1,25 dihydroxy vit D2 in kidney and peripheral
resistance to PTH. ncrease fecal Ca loss. Decrease urinary P loss. Deposition of Ca and P in soft
tissues. 2
o
hyperparathyroidism eventually leads to Ca leaching from bones.
Hypermagnaesia 2
o
to decreased urinary loss. Rarely symptomatic. Avoidn high Mg medication.
HTN and accelerated atherosclerosis 2
o
to high Na retention and altered Renin-Angiotensisn-
Aldosterone Axis. Atherosclerois due to increased lipids
Pericarditis
Anaemia major problem. 2
o
to decreased erythropetin production. Treated with erthropoetin and
trasnfusions.
nfections/ Altered Leukocyte Function leading cause of Morbidity and Death
ncreased Bleeding Unclear etiology, ?altered platelt function. ncreased bleeding time.
Osteodystrophy 2
o
to hyperparathyroidism and leaching of Ca from bones Osteomalacia and Osteitis
Fibrosa. Treat: Vit D, P Binders (Amphojel), and Ca replacement.
You might also like
- 9 - Internal Medicine Buzzwords Handout Oct 2023 John Michael RuizDocument8 pages9 - Internal Medicine Buzzwords Handout Oct 2023 John Michael RuizJohn Michael RuizNo ratings yet
- Easy Keto and Intermittent FastingDocument98 pagesEasy Keto and Intermittent FastingTony Multh100% (3)
- Urinary Tract Disorders, PowerpointDocument63 pagesUrinary Tract Disorders, Powerpointmutia mutia100% (5)
- Gout Diet Patient HandoutDocument3 pagesGout Diet Patient HandoutJenniferNo ratings yet
- MetabolicDocument23 pagesMetabolicbtidipNo ratings yet
- Abg 2Document6 pagesAbg 2Maine AsuncionNo ratings yet
- Acid-Base Disorder in SurgeryDocument52 pagesAcid-Base Disorder in SurgeryFree ZingNo ratings yet
- Acid Base Disorders Peter SehaDocument29 pagesAcid Base Disorders Peter SehaPeter SehaNo ratings yet
- Fluid, Electrolytes, Acid Base BalanceDocument18 pagesFluid, Electrolytes, Acid Base Balanceashdmb217100% (5)
- ContDocument76 pagesContIola JaneNo ratings yet
- Lab Values WorksheetDocument57 pagesLab Values WorksheetpcbthyNo ratings yet
- Arterial Blood Gas Interpretation: Joseph Brian L. Costiniano, MD, DPCPDocument39 pagesArterial Blood Gas Interpretation: Joseph Brian L. Costiniano, MD, DPCPGio Tamaño BalisiNo ratings yet
- Arterial Blood Gas Interpretation: Joseph Brian L. Costiniano, MD, DPCPDocument39 pagesArterial Blood Gas Interpretation: Joseph Brian L. Costiniano, MD, DPCPevbptrprnrmNo ratings yet
- Chloremia (Hypochloremia) & Acute and Chronic Respiratory Alkalosis (Carbonic Acid Deficit)Document4 pagesChloremia (Hypochloremia) & Acute and Chronic Respiratory Alkalosis (Carbonic Acid Deficit)KQarlo Luis Pestaño Maniaol100% (1)
- Blood Gas InterpretationDocument50 pagesBlood Gas InterpretationVebby 'bee' AstriNo ratings yet
- Acidosis and AlkalosisDocument10 pagesAcidosis and AlkalosisNealeth NanquilNo ratings yet
- Primary Changes and Compensations in Simple Acid-Base DisordersDocument4 pagesPrimary Changes and Compensations in Simple Acid-Base DisordersKimberly Trezona PlonkaNo ratings yet
- Acid Base Balance in ICU Summary 25122020Document8 pagesAcid Base Balance in ICU Summary 25122020Aya NassarNo ratings yet
- Acid Base Imbalance 2Document26 pagesAcid Base Imbalance 2Female calmNo ratings yet
- Tau Chempath - Acid Base Imbalance & Pahology of Resp FailureDocument31 pagesTau Chempath - Acid Base Imbalance & Pahology of Resp FailureChipego ChiyaamaNo ratings yet
- Alkalosis AcidosisDocument31 pagesAlkalosis Acidosiskirti thakurNo ratings yet
- ABIDocument27 pagesABIekramNo ratings yet
- Metabolic AlkalosisDocument8 pagesMetabolic AlkalosisPauline PerezNo ratings yet
- Acidosis AlkalosisDocument5 pagesAcidosis Alkalosisaljosa_21No ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument15 pagesDr. Ali's Uworld Notes For Step 2 CKBoogy WoogyNo ratings yet
- What Are Acidosis and Alkalosis?Document5 pagesWhat Are Acidosis and Alkalosis?Nelofar ShaikNo ratings yet
- Acid-Base Balance PDFDocument3 pagesAcid-Base Balance PDFjanet roosevelt100% (2)
- Body FluidsDocument6 pagesBody FluidsMemory MahwendaNo ratings yet
- Asam BasaDocument47 pagesAsam BasaMilikPremiumstock90No ratings yet
- Hydrogen Ion HomeostasisDocument51 pagesHydrogen Ion Homeostasisjusticeboakye100% (1)
- Blood Gas Analysis: - Arterial Blood Gases MeasuresDocument39 pagesBlood Gas Analysis: - Arterial Blood Gases Measuresapi-19641337No ratings yet
- Fluid and ElectrolytesDocument14 pagesFluid and Electrolytesstring44100% (2)
- Acid Base: Prep by Clement UWASE PGY2Document48 pagesAcid Base: Prep by Clement UWASE PGY2TWISUNGANE PROTOGENENo ratings yet
- Parameters of Interest: - PH - pCO2 - Po2 - Hco3 Normal ValuesDocument25 pagesParameters of Interest: - PH - pCO2 - Po2 - Hco3 Normal ValuesPrincess Dumpit100% (1)
- Acidosis and Alkalosis SlidesDocument8 pagesAcidosis and Alkalosis SlidesNikhatNo ratings yet
- Keseimbangan Asam-Basa (2) : Sudarno, DR M.KesDocument47 pagesKeseimbangan Asam-Basa (2) : Sudarno, DR M.Kesanny lusheniaNo ratings yet
- Acid Base: Heather Wacholz TCCCDocument33 pagesAcid Base: Heather Wacholz TCCCahmadNo ratings yet
- Acidosis and AlkalosisDocument4 pagesAcidosis and Alkalosis'Rumsha SyedNo ratings yet
- ABGs Respiratory/MetabolicDocument3 pagesABGs Respiratory/MetabolicJoe B100% (1)
- Acid BaseDocument33 pagesAcid BaseParvathy R NairNo ratings yet
- Acid-Base Homeostasis: Dr. Abeer KhurshidDocument42 pagesAcid-Base Homeostasis: Dr. Abeer Khurshidسلة فواكة100% (2)
- Acid BaseDocument21 pagesAcid BaseAngela Danielle TanNo ratings yet
- Acid Base BalanceDocument61 pagesAcid Base BalanceAshwin ChandNo ratings yet
- Acid - Base Basics: Dr. Fawzeya Aboul Fetouh Prof of Anesthesia Cairo UnversityDocument54 pagesAcid - Base Basics: Dr. Fawzeya Aboul Fetouh Prof of Anesthesia Cairo UnversityPaolo Uccello100% (1)
- Abg PPT NewDocument69 pagesAbg PPT NewMalaka Atapattu100% (3)
- Acid Base PresentationDocument34 pagesAcid Base PresentationIza AsadNo ratings yet
- Basic Ionic Salt Alkali Metal Alkaline Earth Metal ElementDocument3 pagesBasic Ionic Salt Alkali Metal Alkaline Earth Metal ElementMing SakaluranNo ratings yet
- Acid Base BalanceDocument69 pagesAcid Base BalanceAli AttarNo ratings yet
- Fluid Electrolye Acid Base Disorder EraldDocument21 pagesFluid Electrolye Acid Base Disorder EraldM. R. EmeraldNo ratings yet
- Diabetic Ketoacidosis: Dr. Kaustuv de Fellow (3 Yr.) Critical Care MedicineDocument31 pagesDiabetic Ketoacidosis: Dr. Kaustuv de Fellow (3 Yr.) Critical Care MedicineKaustuv DeNo ratings yet
- Anion Gap Metabolic Acidosis: More Then Just A Mud PileDocument21 pagesAnion Gap Metabolic Acidosis: More Then Just A Mud PileFarah SyazanaNo ratings yet
- Interpretation of Arterial Blood Gases (Abgs) I David A. Kaufman, MD DDocument17 pagesInterpretation of Arterial Blood Gases (Abgs) I David A. Kaufman, MD DingridpuspitaNo ratings yet
- Acid Base ImbalanceDocument18 pagesAcid Base ImbalanceLanzen DragneelNo ratings yet
- Acid Base Disorders MBBSDocument44 pagesAcid Base Disorders MBBSphuyalaryan666No ratings yet
- Medical Surgical Nursing Reviewer BulletsDocument8 pagesMedical Surgical Nursing Reviewer Bulletsgrey26100% (3)
- Acid Base Fall 2008Document34 pagesAcid Base Fall 2008anon-252165No ratings yet
- Physioloical Integrity Acute Biologic CrisisDocument42 pagesPhysioloical Integrity Acute Biologic CrisisJohn Paul M. TagapanNo ratings yet
- Metabolic AlkalosisDocument2 pagesMetabolic AlkalosisKath ComodaNo ratings yet
- Acid-Base Disorders and AbgsDocument46 pagesAcid-Base Disorders and AbgsAlonso Rodriguez EscobedoNo ratings yet
- Clinical Therapeutics Hazel Mae B. ValdezDocument29 pagesClinical Therapeutics Hazel Mae B. ValdezMichelle Vera GabunNo ratings yet
- Acid Base ImbalanceDocument50 pagesAcid Base ImbalanceDian Pratiwi BurnamaNo ratings yet
- Bullets in Medical Surgical NursingDocument8 pagesBullets in Medical Surgical Nursingapi-3731294100% (2)
- Hematology Notes for Medical StudentsFrom EverandHematology Notes for Medical StudentsRating: 5 out of 5 stars5/5 (1)
- Clincal 1 SAS v2022 (1) - 104-111Document8 pagesClincal 1 SAS v2022 (1) - 104-111Jannah Mikhaela Alibay VillarinNo ratings yet
- PDF of Dua Hati Majarani Full Chapter EbookDocument69 pagesPDF of Dua Hati Majarani Full Chapter Ebookmefielrheta687100% (7)
- Homeopathic Remedies For Kidney Stones - HompathDocument5 pagesHomeopathic Remedies For Kidney Stones - HompathBGNo ratings yet
- NCP of Renal CalculiDocument3 pagesNCP of Renal Calculidextroid1289% (9)
- Formulation and Evaluation of Herbal Syrup Used in The Management of Cholesterol and Kidney StonesDocument11 pagesFormulation and Evaluation of Herbal Syrup Used in The Management of Cholesterol and Kidney StonesDicky KobandahaNo ratings yet
- Why Oxalic Acid Is Very Important To Your HealthDocument3 pagesWhy Oxalic Acid Is Very Important To Your HealthAhmad Afifi Ibrahim100% (1)
- Mutations in SLC26A1 Cause Nephrolithiasis: Table S1Document7 pagesMutations in SLC26A1 Cause Nephrolithiasis: Table S1Johnny GoteNo ratings yet
- Case Study of Vataja Brama With Renal CalculiDocument9 pagesCase Study of Vataja Brama With Renal CalculiNagabharana Hm HollattiNo ratings yet
- Kidney Stones: An IntroductionDocument3 pagesKidney Stones: An IntroductionSisti AninditaNo ratings yet
- Organic Wellness Products BrochureDocument18 pagesOrganic Wellness Products Brochureorganic wellnessNo ratings yet
- SurgeryDocument31 pagesSurgeryGayathiri SureshNo ratings yet
- PPTDocument27 pagesPPTmonicanasutionNo ratings yet
- NDT Post Mid Term AnswersDocument36 pagesNDT Post Mid Term AnswersAnonymousTargetNo ratings yet
- Effect of Phenolic Compounds From Bergenia Ciliata Leaves On Experimental Kidney StonesDocument4 pagesEffect of Phenolic Compounds From Bergenia Ciliata Leaves On Experimental Kidney StonesSilfia LayliyahNo ratings yet
- Teaching Plan-Renal CalculiDocument4 pagesTeaching Plan-Renal CalculiKathleen Martinez PecuaNo ratings yet
- Diet and Health - Scientific Perspectives by Walter VeithDocument424 pagesDiet and Health - Scientific Perspectives by Walter VeithD o u g l a sNo ratings yet
- Generic Name:: ElectrolytesDocument9 pagesGeneric Name:: ElectrolytesEleazar Desillarico GonzalesNo ratings yet
- NCP UrolithiasisDocument6 pagesNCP UrolithiasisOnieBoy CurayagNo ratings yet
- Stones in The Urinary BladderDocument6 pagesStones in The Urinary Bladderjoseosteopatia3693No ratings yet
- The Mineralogy and Chemistry of Urinary Stones From The United Arab EmiratesDocument14 pagesThe Mineralogy and Chemistry of Urinary Stones From The United Arab EmiratesAhmed Mohamed SalahNo ratings yet
- Open Staghorn Stone SurgeryDocument17 pagesOpen Staghorn Stone SurgeryHardiTariqHammaNo ratings yet
- Vol15 Iss1 CentenaroDocument7 pagesVol15 Iss1 CentenaroMuhammad FaridNo ratings yet
- Child With HematuriaDocument42 pagesChild With HematuriaalaaNo ratings yet
- 10 Doh Approved Herbal PlantsDocument7 pages10 Doh Approved Herbal PlantsLaura VillegasNo ratings yet
- Retrograde Intrarenal Surgery An Expanding Role inDocument10 pagesRetrograde Intrarenal Surgery An Expanding Role inNenny HariyantoNo ratings yet
- Renal and Urinary SystemDocument5 pagesRenal and Urinary SystemStaceyNo ratings yet