Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
1 viewsSurgical Infections
Surgical Infections
Uploaded by
Benja MutindaCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You might also like
- Topic 6: Microbiology, Immunity and Forensics Chapter 6B: ImmunityDocument3 pagesTopic 6: Microbiology, Immunity and Forensics Chapter 6B: ImmunitysalmaNo ratings yet
- Prep 2015Document358 pagesPrep 2015a alrabiaahNo ratings yet
- Acute Infections Oral and Paraoral TissuesDocument33 pagesAcute Infections Oral and Paraoral TissuesKarthik S'twinkles SNo ratings yet
- Agents of Wound Infections: S. Aureus & C. Albicans: Insert Name HereDocument1 pageAgents of Wound Infections: S. Aureus & C. Albicans: Insert Name HereCathy JenkinsNo ratings yet
- Surgical Infection 1Document39 pagesSurgical Infection 1uzma aijazNo ratings yet
- Dr. Hatem Elgohary Lecturer of General Surgery MD, MrcsDocument24 pagesDr. Hatem Elgohary Lecturer of General Surgery MD, MrcswinceNo ratings yet
- Rotar O.V. As - Prof. General Surgery, BSMUDocument63 pagesRotar O.V. As - Prof. General Surgery, BSMUOleksandr RotarNo ratings yet
- Post Op InfectionsDocument62 pagesPost Op InfectionsDr.Rudra PrasadNo ratings yet
- Surgical Wound InfectionDocument9 pagesSurgical Wound InfectionSRO oONo ratings yet
- Myco Viro Notes Module 6Document6 pagesMyco Viro Notes Module 6Kyle Jude Roberts SanesNo ratings yet
- 'Surgical Infection'Document21 pages'Surgical Infection'jannatul supti24No ratings yet
- Surgical InfectionsDocument20 pagesSurgical InfectionsDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- Antibiotic Selection GuideDocument37 pagesAntibiotic Selection GuideAbanoub Nabil100% (1)
- Pathogenesis of Bacterial InfectionDocument65 pagesPathogenesis of Bacterial Infectionsamsonraju07No ratings yet
- Infection in CancerDocument34 pagesInfection in CancerSheikNo ratings yet
- Necrotizing FasiitisDocument30 pagesNecrotizing FasiitisFadhly SharimanNo ratings yet
- Corynebacterium DiphtheriaeDocument21 pagesCorynebacterium DiphtheriaehercolaniumNo ratings yet
- Pemilihan Antibiotic Pada Pembedahan: By: Mas RizalDocument27 pagesPemilihan Antibiotic Pada Pembedahan: By: Mas RizalguterizalNo ratings yet
- 2017, 5 Anti Infeksi (Farmakologi Pada HIV-AIDS)Document46 pages2017, 5 Anti Infeksi (Farmakologi Pada HIV-AIDS)Jashmine RachlyNo ratings yet
- Microbiology Laboratory Faculty of Medicine Brawijaya UniversityDocument32 pagesMicrobiology Laboratory Faculty of Medicine Brawijaya UniversityfhfebriiNo ratings yet
- Bacterial PathogenesisDocument36 pagesBacterial Pathogenesisapi-19969058100% (3)
- Opportunistic MycosesDocument31 pagesOpportunistic MycosesMaxamed Faarax XaashiNo ratings yet
- All 45 BugsDocument26 pagesAll 45 Bugsroboat96No ratings yet
- Chemo For LabDocument117 pagesChemo For Labsinte beyuNo ratings yet
- Mycobacterium General Properties: Mycobacteria Cell Wall StructureDocument12 pagesMycobacterium General Properties: Mycobacteria Cell Wall StructureAhmed ExaminationNo ratings yet
- Microbiology PointsDocument17 pagesMicrobiology Points1031 Muhammad zaryabNo ratings yet
- Maxillofacial MicrobiologyDocument60 pagesMaxillofacial MicrobiologyAbel AbrahamNo ratings yet
- Mycology - Chapter Seven Opportunistic Mycoses: Let Us Know What You ThinkDocument9 pagesMycology - Chapter Seven Opportunistic Mycoses: Let Us Know What You ThinkAreeqa AliNo ratings yet
- Key Points Revision: 1 Structure and Classification of BacteriaDocument17 pagesKey Points Revision: 1 Structure and Classification of Bacteriatarun956519No ratings yet
- Soal UasDocument10 pagesSoal UasDila ZeinNo ratings yet
- Infection in The Immunocompromised Person: EtiologyDocument20 pagesInfection in The Immunocompromised Person: EtiologyCabdiNo ratings yet
- Case Study 2Document2 pagesCase Study 2Khizra AmjadNo ratings yet
- Antmicrobial AgentDocument93 pagesAntmicrobial Agentdrnuaman5No ratings yet
- Critica Brand PresentationDocument19 pagesCritica Brand PresentationkurutalaNo ratings yet
- Infectious Diseases NotesDocument34 pagesInfectious Diseases NotesNuha AL-YousfiNo ratings yet
- Immunological Aspects of Immunological Aspects of Infectious Disease Infectious Disease (Fungi & Parasite) (Fungi & Parasite)Document51 pagesImmunological Aspects of Immunological Aspects of Infectious Disease Infectious Disease (Fungi & Parasite) (Fungi & Parasite)miniwhiteyNo ratings yet
- Linton Chapter 13 Immune, Infection, InflammationDocument7 pagesLinton Chapter 13 Immune, Infection, InflammationJose FloresNo ratings yet
- Infectious DiseasesDocument37 pagesInfectious Diseasespolaris_027No ratings yet
- Patho A 1. 11 Infectious Diseases Tagayuna 2015Document10 pagesPatho A 1. 11 Infectious Diseases Tagayuna 2015Ala'a Emerald AguamNo ratings yet
- ClostridumDocument30 pagesClostridumFrancesca VargasNo ratings yet
- Surgical Infection: Gangr EneDocument121 pagesSurgical Infection: Gangr EnefatmawatiNo ratings yet
- Chapter 3.6 - Pathogenesis of Bacterial InfectionsDocument28 pagesChapter 3.6 - Pathogenesis of Bacterial InfectionsDkNo ratings yet
- Opportunistic MycosesDocument7 pagesOpportunistic MycosesAbhishek ChandraNo ratings yet
- Prophylactic Use of Anti-Microbial Agents: Presented By: Jagir R. Patel Assistant ProfessorDocument18 pagesProphylactic Use of Anti-Microbial Agents: Presented By: Jagir R. Patel Assistant ProfessorJagirNo ratings yet
- Bakteri Penyebab IMSDocument67 pagesBakteri Penyebab IMSuut14No ratings yet
- Antibiotic Selection in SepsisDocument4 pagesAntibiotic Selection in SepsisIndah AmisaniNo ratings yet
- Clostrdia: G Positive Spore Forming Anaerobic Toxin Producing RodsDocument36 pagesClostrdia: G Positive Spore Forming Anaerobic Toxin Producing Rodsjamal nasirNo ratings yet
- 5-Antifungal DrugssDocument32 pages5-Antifungal DrugssTasnim sarairehNo ratings yet
- Introduction To Pathology Infectious DiseasesDocument37 pagesIntroduction To Pathology Infectious DiseasesNirav PatelNo ratings yet
- NeisseriaDocument32 pagesNeisseriaKeshant SamarooNo ratings yet
- Surgical Infections Chapter 5 Shcwartz Principles of SurgeryDocument34 pagesSurgical Infections Chapter 5 Shcwartz Principles of Surgeryanas hindawi100% (4)
- Resident Flora and Its Mechanism of Invasion: Maryum FiazDocument14 pagesResident Flora and Its Mechanism of Invasion: Maryum FiazHasnain AliNo ratings yet
- StreptococciDocument39 pagesStreptococciالطاهر زروقNo ratings yet
- BacteriologyDocument23 pagesBacteriologyCHRISTIAN SIDAYANo ratings yet
- Surgical Infections PDFDocument9 pagesSurgical Infections PDFJohn Christopher LucesNo ratings yet
- Concepts of Infection ControlDocument53 pagesConcepts of Infection ControlNicoleNo ratings yet
- Bacterial InfectiousDocument7 pagesBacterial InfectioussamioNo ratings yet
- Surgical Infections AntibioticsDocument45 pagesSurgical Infections AntibioticsMohd ShoaibNo ratings yet
- Unit 2 CompleteDocument20 pagesUnit 2 CompleteSaima VictorNo ratings yet
- Management of Infections in the Immunocompromised HostFrom EverandManagement of Infections in the Immunocompromised HostBrahm H. SegalNo ratings yet
- Dermatology Pharmacology SkinDocument31 pagesDermatology Pharmacology SkinEuro UndisaNo ratings yet
- This Set of Microbiology Multiple Choice QuestionsDocument3 pagesThis Set of Microbiology Multiple Choice QuestionsMinh AnhNo ratings yet
- Imidazole and Its Biological Activities A Review PDFDocument12 pagesImidazole and Its Biological Activities A Review PDFKim LunaNo ratings yet
- Correlation Between Age and Tonsil Size in Patients With Chronic Tonsillitis at Aek Kanopan DistrictDocument8 pagesCorrelation Between Age and Tonsil Size in Patients With Chronic Tonsillitis at Aek Kanopan DistrictIJRASETPublicationsNo ratings yet
- VLE Pharma LeatrizeDocument29 pagesVLE Pharma LeatrizeKenneth ShayNo ratings yet
- A006 PDFDocument6 pagesA006 PDFfavourNo ratings yet
- IntroductionDocument57 pagesIntroductionFebitha FlNo ratings yet
- 08 - Microorganisms and Their Effects On Living ThingsDocument5 pages08 - Microorganisms and Their Effects On Living ThingsMie IsaNo ratings yet
- Avenue 7 E-CatalogueDocument44 pagesAvenue 7 E-CatalogueElias BinuNo ratings yet
- Septic Arthritis and Prosthetic Joint Infection in Older AdultsDocument15 pagesSeptic Arthritis and Prosthetic Joint Infection in Older AdultsajengmdNo ratings yet
- Practical 6 Microbes NEWDocument10 pagesPractical 6 Microbes NEWMohammad Shahid YaseenNo ratings yet
- Antib 2020 - LB Engl Prima Varianta Fara CorecturiDocument13 pagesAntib 2020 - LB Engl Prima Varianta Fara CorecturiIrina Panciu StefanNo ratings yet
- La Asuncion Montessori of Tagaytay Inc.: Patutong Malaki North, Tagaytay City Tel. No.: (046) 682 - 02 - 69Document4 pagesLa Asuncion Montessori of Tagaytay Inc.: Patutong Malaki North, Tagaytay City Tel. No.: (046) 682 - 02 - 69Cedrick PerenaNo ratings yet
- Citrus MaximaDocument11 pagesCitrus MaximanelisaNo ratings yet
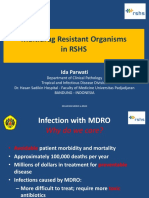
- Multidrug Resistant Organisms in RSHS: Ida ParwatiDocument48 pagesMultidrug Resistant Organisms in RSHS: Ida Parwatiarief kurniawanNo ratings yet
- 86f4be500e7cac40b5b214de9577dd2eDocument31 pages86f4be500e7cac40b5b214de9577dd2e10-Gia KhôiNo ratings yet
- Lecture 2a-Primary MetabolitesDocument50 pagesLecture 2a-Primary Metabolitesurmeen04khanNo ratings yet
- VILSAN CatalougeDocument97 pagesVILSAN CatalougeSầu VeNo ratings yet
- Templet RKO FOPI 2021Document270 pagesTemplet RKO FOPI 2021Karin ArinciaNo ratings yet
- Jurnal Antibiotik 2Document11 pagesJurnal Antibiotik 2Achmad YunusNo ratings yet
- Arabjc D 22 01250 - R1Document50 pagesArabjc D 22 01250 - R1Gabriela LopesNo ratings yet
- Otitis Externa in Dogs Microbiology and 20151116-999-Z6r7ns-With-Cover-Page-V2Document6 pagesOtitis Externa in Dogs Microbiology and 20151116-999-Z6r7ns-With-Cover-Page-V2Yến KimNo ratings yet
- Questions RleDocument2 pagesQuestions RleKent AlveNo ratings yet
- Ashok MehraDocument40 pagesAshok MehraFahim UddinNo ratings yet
- CD 2022 FundaICN Starters Basic - PDF - FOR REVIEWERDocument15 pagesCD 2022 FundaICN Starters Basic - PDF - FOR REVIEWERMeryville JacildoNo ratings yet
- Garp-Nepal - Sa (Global Antibiotic Resistance Partnership)Document90 pagesGarp-Nepal - Sa (Global Antibiotic Resistance Partnership)Nivea VazNo ratings yet
- To Err Is Human: DR Inas Alassar CPHQDocument96 pagesTo Err Is Human: DR Inas Alassar CPHQYahya HashmiNo ratings yet
- Antibiotik Pada Infeksi Tropis (PERSI)Document42 pagesAntibiotik Pada Infeksi Tropis (PERSI)YULINo ratings yet
- Azlocillin Can Be The Potential Drug Candidate Against Drug-Tolerant Borrelia Burgdorferi Sensu Stricto JLB31Document15 pagesAzlocillin Can Be The Potential Drug Candidate Against Drug-Tolerant Borrelia Burgdorferi Sensu Stricto JLB31Lauge BrimgiestNo ratings yet
Surgical Infections
Surgical Infections
Uploaded by
Benja Mutinda0 ratings0% found this document useful (0 votes)
1 views24 pagesCopyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
1 views24 pagesSurgical Infections
Surgical Infections
Uploaded by
Benja MutindaCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 24
Surgical Infections 1
Dr. Valentine Mbithi
General Surgeon
AIC Litein Hospital
Introduction
Surgical Infections include infections requiring
surgical management and those as a result of surgery.
Host Defense Mechanisms
A: Barriers
Skin
Mechanical barrier
Acidic pH 5-6
Relative lack of water
Constant epithelial cell turnover
Host Defense Mechanisms: Barriers
Respiratory Tract epithelium
Mucous blanket- traps inhaled particles
IgA produced by lymphoid tissue: Prevents microbe
adherence to respiratory epithelium
Cilliary mechanism: steadily rolls mucous to pharynx,
than expelled and coughed or swallowed
Barriers
Stomach: Acidic pH: prevents growth of most bacteria.
Antacids, PPI and H2 blockers increase risk of bacterial
and fungal colonisation and thus pneumonia especially in
the case of aspiration or in intubated patients
Urinary tract: IgA, long urethra in males
B)Microbial Flora
Small and Large Intestines: Abundant normal flora that
prevent growth of pathogenic microbes. Peristalsis
keeps population constant.
Normal Small intestine and Colon Flora
Anaerobes: Bacteroided Fragilis, Fusobacterium,
Peptostreptococcus, more that aerobes
Aerobes: Escherichia Coli, Enterococcus fecalis
C: Immunology
Phagocytic leukocytes ingest pathogens via
phagocytosis and act as Antigen Presenting Cells to T
cells.
Monocytes and granulocytes(neutrophils and eosinophils).
Macrophages are differentiated monocytes residing in all
body tissues but heavily concentrated in lungs, liver and
spleen.
Migrate to areas of inflammation by chemotaxis
Opsonisation by complement and immunoglobulins
facilitate recognition of pathogens.
Opsonisation and phagocytosis are body’s primary
defence mechanism against extracellular pathogens.
Immunology
Cellular Immunity: Deals with intracellular microbes:
viruses
Afferent limb: recognises foreign pathogen. Involves
antigen presentation and T cell activation
Efferent limb: destroys infected cell. Includes cytotoxic
T cells, monocytes, macrophages and granulocytes
Humoral responses
Immunoglobulins: IgA, IgD, IgE, IgG, IgM
Neutralise viruses and bacterial toxins
Inhibit microbial attachment to host cells
Opsonise pathogens
Activate complement cascade
Complement: a nonspecific defence system that is
activated by antibody and initiates a cascade of reactions
that lead to cell lysis.
Surgical Microbiology and Pathogenicity:
Viruses
Obligate intracellular pathogens
Viral infections of surgical importance
TORCH: Congenital Malformations
HIV: Altered Immune function
HTLV1, HPV increased cellular proliferation and
oncogenesies
Enterovirus: Appendicitis
CMV: Ulcerative Colitis
Adenovirus: Intussusception
Hepatitis B and C: End Stage Liver Disease requiring Liver
transplantation
Bacteria
Are pathogenic single cells: either rods, spheres or
spirals. Either gram positive or negative depending on
cell wall structure.
Pathogenicity: bacteria adheres to epithelial surface
and cause disease by
Invading host tissues e.g Streptococcus pneumoniae
Producing toxins : Endotoxins and exotoxins e.g.
Clostridium perfringens, C. difficile, S. Pyogenes, S.
Aureus
Inciting pathologic Immune response
Fungi
Rarely cause infection in immunocompetent host.
Risk factors for fungal infection: HIV, transplant
patients, diabetes, prolonged hospitalisation, Central
Lines, prolonged or broad spectrum antibiotic use,
parenteral nutrition, immunosupressive drugs, burns,
trauma and malnutrition.
Infection occurs by
Inhalation e.g. aspergillosis, histoplasmosis , blastomycosis
Innoculation of subcutaneous tissues: sporotrichosis
Colonisation of mucosal surfaces: oral or esophageal
candidiasis
Antimicrobial Therapy
Proper Selection of antibiotic requires knowledge of
The most common pathogens causing specific infection
The mechanism of action of the selected agent
Potential side effects of selected agent
Sensitivity patterns of most common microbes in the
area.
Inhibitors of Cell Wall Synthesis: B-Lactam
Antibiotics
The B lactam ring inhibits cell wall peptidoglycan synthesis
causing cell lysis.
Resistance is caused by bacterial production of B-lactamase.
Penicillins: Penicillin G, Amoxicillin, ampicillin,
flucloxacillin, Piperacillin: different bacterial coverages.
Allergic reaction is major adverse effect.
Cephalosporins: 1st to 4 th generation antibiotics. Do not
cover enterococcus. Cross allergic reaction with penicillins
more common in lower generations
Imipenem and Meropenem: Broadest spectrum
Vancomycin: Good gram positive coverage, good for MRSA
Inhibitors of ribosomal Protein Synthesis
Aminoglycosides e.g gentamycin, amikacin
Bactericidal. Adverse effect of renal and ototoxicity.
Aerobic gram negative coverage
Macrolides: Erythromycin, clindamycin
Tetracyclines: Tetracycline, minocycline.
Broadspectrum.
Chloramphenicol: Broad spectrum, good BBB
penetration
Inhibitors of folic acid synthesis
Sulfonamides and Trimethoprim: synergistic action
Good for UTI, MRSA, PCP.
Sulfur allergy
Inhibitors of DNA synthesis
Fluoroquinilones: Ciprofloxacin, Norfloxacin,
Ofloxacin: Good for GI and GU infections
Metronidazole: Anaerobes.
Antifungals
Fluconazole: few adverse effects
Amphotericin B: nephrotoxicity, electrolyte
disturbance, leukopenia, anemia, thrombocytopenia
Chlotrimazole
Griseofulvin
Capsofungin
Surgical Prophylaxis and prevention of
surgical Site infections
SSIs are most common nosocomial infections and result
in prolonged hospitalisation, increased costs and
significant morbidity.
Wound infections can be attributed to endogenous
contamination from skin flora and GI contamination or
exogenous contamination from break in sterile technique.
Operative site should be scrubbed using germicidal
detergent folowed by application of povidone or
chlorhexidine paint.
Hair clipping and not shaving.
If GI or GU tracts entered, gloves should be changed after
dirty part of procedure is done
Pre-operative antibiotics reduce infection risk for
clean- contaminated and contaminated wounds
Clean cases do not require antibiotic prophylaxis
except in implant or bioprosthetic material placement.
Cefazolin for most wounds. Vancomycin if allergic to
penicillins and cephalosporins
Second generation antibiotic eg cefotetan or cefoxitin
in bowel surgery plus metronodazole
Other measures to decrease operative wound infections
include: obliteration of dead space, removal of necrotic
tissue, wound closure without tension, hemostasis.
Drains may help evacuate hematoma or seroma but are
foreign bodies and increase infection risk and should
not be used routinely.
Immunotherapy: Tetanus toxoid for dirty wounds
Classification of Operative wounds
Clean: Elective, nontraumatic, primarily closed, no
acute inflammation, no break in sterile technique. No
entry to respiratory, GI, GU, biliary tract
Clean Contaminated: Urgent or emergent cases that are
otherwise clean, elective with opening of GI, GU,
Biliary,respiratory tracts, not encountering infeected
bile or urine, minor break in sterile technique
Contaminated: Nonpurulent inflammantion, gross
spillage from GI tract, entry to infected GU or biliary
tract, major break in sterile technique, penetrating
trauma < 4 hrs old, chronic wounds for grafting
Dirty: Purulent inflammation, preoperative perforation
of GI, GU, biliary, resp tracts, penetrating trauma > 4
hrs
Surgical Infections 2
Intra-abdominal Infections
Cellulitis
Necrotising Soft Tissue Infection
Gram Negative Bacterial Sepsis
Catheter and Prosthetic Device Infection
UTI
HIV in the Surgical Patient
Diabetic Foot
Empyema Thoracis
You might also like
- Topic 6: Microbiology, Immunity and Forensics Chapter 6B: ImmunityDocument3 pagesTopic 6: Microbiology, Immunity and Forensics Chapter 6B: ImmunitysalmaNo ratings yet
- Prep 2015Document358 pagesPrep 2015a alrabiaahNo ratings yet
- Acute Infections Oral and Paraoral TissuesDocument33 pagesAcute Infections Oral and Paraoral TissuesKarthik S'twinkles SNo ratings yet
- Agents of Wound Infections: S. Aureus & C. Albicans: Insert Name HereDocument1 pageAgents of Wound Infections: S. Aureus & C. Albicans: Insert Name HereCathy JenkinsNo ratings yet
- Surgical Infection 1Document39 pagesSurgical Infection 1uzma aijazNo ratings yet
- Dr. Hatem Elgohary Lecturer of General Surgery MD, MrcsDocument24 pagesDr. Hatem Elgohary Lecturer of General Surgery MD, MrcswinceNo ratings yet
- Rotar O.V. As - Prof. General Surgery, BSMUDocument63 pagesRotar O.V. As - Prof. General Surgery, BSMUOleksandr RotarNo ratings yet
- Post Op InfectionsDocument62 pagesPost Op InfectionsDr.Rudra PrasadNo ratings yet
- Surgical Wound InfectionDocument9 pagesSurgical Wound InfectionSRO oONo ratings yet
- Myco Viro Notes Module 6Document6 pagesMyco Viro Notes Module 6Kyle Jude Roberts SanesNo ratings yet
- 'Surgical Infection'Document21 pages'Surgical Infection'jannatul supti24No ratings yet
- Surgical InfectionsDocument20 pagesSurgical InfectionsDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- Antibiotic Selection GuideDocument37 pagesAntibiotic Selection GuideAbanoub Nabil100% (1)
- Pathogenesis of Bacterial InfectionDocument65 pagesPathogenesis of Bacterial Infectionsamsonraju07No ratings yet
- Infection in CancerDocument34 pagesInfection in CancerSheikNo ratings yet
- Necrotizing FasiitisDocument30 pagesNecrotizing FasiitisFadhly SharimanNo ratings yet
- Corynebacterium DiphtheriaeDocument21 pagesCorynebacterium DiphtheriaehercolaniumNo ratings yet
- Pemilihan Antibiotic Pada Pembedahan: By: Mas RizalDocument27 pagesPemilihan Antibiotic Pada Pembedahan: By: Mas RizalguterizalNo ratings yet
- 2017, 5 Anti Infeksi (Farmakologi Pada HIV-AIDS)Document46 pages2017, 5 Anti Infeksi (Farmakologi Pada HIV-AIDS)Jashmine RachlyNo ratings yet
- Microbiology Laboratory Faculty of Medicine Brawijaya UniversityDocument32 pagesMicrobiology Laboratory Faculty of Medicine Brawijaya UniversityfhfebriiNo ratings yet
- Bacterial PathogenesisDocument36 pagesBacterial Pathogenesisapi-19969058100% (3)
- Opportunistic MycosesDocument31 pagesOpportunistic MycosesMaxamed Faarax XaashiNo ratings yet
- All 45 BugsDocument26 pagesAll 45 Bugsroboat96No ratings yet
- Chemo For LabDocument117 pagesChemo For Labsinte beyuNo ratings yet
- Mycobacterium General Properties: Mycobacteria Cell Wall StructureDocument12 pagesMycobacterium General Properties: Mycobacteria Cell Wall StructureAhmed ExaminationNo ratings yet
- Microbiology PointsDocument17 pagesMicrobiology Points1031 Muhammad zaryabNo ratings yet
- Maxillofacial MicrobiologyDocument60 pagesMaxillofacial MicrobiologyAbel AbrahamNo ratings yet
- Mycology - Chapter Seven Opportunistic Mycoses: Let Us Know What You ThinkDocument9 pagesMycology - Chapter Seven Opportunistic Mycoses: Let Us Know What You ThinkAreeqa AliNo ratings yet
- Key Points Revision: 1 Structure and Classification of BacteriaDocument17 pagesKey Points Revision: 1 Structure and Classification of Bacteriatarun956519No ratings yet
- Soal UasDocument10 pagesSoal UasDila ZeinNo ratings yet
- Infection in The Immunocompromised Person: EtiologyDocument20 pagesInfection in The Immunocompromised Person: EtiologyCabdiNo ratings yet
- Case Study 2Document2 pagesCase Study 2Khizra AmjadNo ratings yet
- Antmicrobial AgentDocument93 pagesAntmicrobial Agentdrnuaman5No ratings yet
- Critica Brand PresentationDocument19 pagesCritica Brand PresentationkurutalaNo ratings yet
- Infectious Diseases NotesDocument34 pagesInfectious Diseases NotesNuha AL-YousfiNo ratings yet
- Immunological Aspects of Immunological Aspects of Infectious Disease Infectious Disease (Fungi & Parasite) (Fungi & Parasite)Document51 pagesImmunological Aspects of Immunological Aspects of Infectious Disease Infectious Disease (Fungi & Parasite) (Fungi & Parasite)miniwhiteyNo ratings yet
- Linton Chapter 13 Immune, Infection, InflammationDocument7 pagesLinton Chapter 13 Immune, Infection, InflammationJose FloresNo ratings yet
- Infectious DiseasesDocument37 pagesInfectious Diseasespolaris_027No ratings yet
- Patho A 1. 11 Infectious Diseases Tagayuna 2015Document10 pagesPatho A 1. 11 Infectious Diseases Tagayuna 2015Ala'a Emerald AguamNo ratings yet
- ClostridumDocument30 pagesClostridumFrancesca VargasNo ratings yet
- Surgical Infection: Gangr EneDocument121 pagesSurgical Infection: Gangr EnefatmawatiNo ratings yet
- Chapter 3.6 - Pathogenesis of Bacterial InfectionsDocument28 pagesChapter 3.6 - Pathogenesis of Bacterial InfectionsDkNo ratings yet
- Opportunistic MycosesDocument7 pagesOpportunistic MycosesAbhishek ChandraNo ratings yet
- Prophylactic Use of Anti-Microbial Agents: Presented By: Jagir R. Patel Assistant ProfessorDocument18 pagesProphylactic Use of Anti-Microbial Agents: Presented By: Jagir R. Patel Assistant ProfessorJagirNo ratings yet
- Bakteri Penyebab IMSDocument67 pagesBakteri Penyebab IMSuut14No ratings yet
- Antibiotic Selection in SepsisDocument4 pagesAntibiotic Selection in SepsisIndah AmisaniNo ratings yet
- Clostrdia: G Positive Spore Forming Anaerobic Toxin Producing RodsDocument36 pagesClostrdia: G Positive Spore Forming Anaerobic Toxin Producing Rodsjamal nasirNo ratings yet
- 5-Antifungal DrugssDocument32 pages5-Antifungal DrugssTasnim sarairehNo ratings yet
- Introduction To Pathology Infectious DiseasesDocument37 pagesIntroduction To Pathology Infectious DiseasesNirav PatelNo ratings yet
- NeisseriaDocument32 pagesNeisseriaKeshant SamarooNo ratings yet
- Surgical Infections Chapter 5 Shcwartz Principles of SurgeryDocument34 pagesSurgical Infections Chapter 5 Shcwartz Principles of Surgeryanas hindawi100% (4)
- Resident Flora and Its Mechanism of Invasion: Maryum FiazDocument14 pagesResident Flora and Its Mechanism of Invasion: Maryum FiazHasnain AliNo ratings yet
- StreptococciDocument39 pagesStreptococciالطاهر زروقNo ratings yet
- BacteriologyDocument23 pagesBacteriologyCHRISTIAN SIDAYANo ratings yet
- Surgical Infections PDFDocument9 pagesSurgical Infections PDFJohn Christopher LucesNo ratings yet
- Concepts of Infection ControlDocument53 pagesConcepts of Infection ControlNicoleNo ratings yet
- Bacterial InfectiousDocument7 pagesBacterial InfectioussamioNo ratings yet
- Surgical Infections AntibioticsDocument45 pagesSurgical Infections AntibioticsMohd ShoaibNo ratings yet
- Unit 2 CompleteDocument20 pagesUnit 2 CompleteSaima VictorNo ratings yet
- Management of Infections in the Immunocompromised HostFrom EverandManagement of Infections in the Immunocompromised HostBrahm H. SegalNo ratings yet
- Dermatology Pharmacology SkinDocument31 pagesDermatology Pharmacology SkinEuro UndisaNo ratings yet
- This Set of Microbiology Multiple Choice QuestionsDocument3 pagesThis Set of Microbiology Multiple Choice QuestionsMinh AnhNo ratings yet
- Imidazole and Its Biological Activities A Review PDFDocument12 pagesImidazole and Its Biological Activities A Review PDFKim LunaNo ratings yet
- Correlation Between Age and Tonsil Size in Patients With Chronic Tonsillitis at Aek Kanopan DistrictDocument8 pagesCorrelation Between Age and Tonsil Size in Patients With Chronic Tonsillitis at Aek Kanopan DistrictIJRASETPublicationsNo ratings yet
- VLE Pharma LeatrizeDocument29 pagesVLE Pharma LeatrizeKenneth ShayNo ratings yet
- A006 PDFDocument6 pagesA006 PDFfavourNo ratings yet
- IntroductionDocument57 pagesIntroductionFebitha FlNo ratings yet
- 08 - Microorganisms and Their Effects On Living ThingsDocument5 pages08 - Microorganisms and Their Effects On Living ThingsMie IsaNo ratings yet
- Avenue 7 E-CatalogueDocument44 pagesAvenue 7 E-CatalogueElias BinuNo ratings yet
- Septic Arthritis and Prosthetic Joint Infection in Older AdultsDocument15 pagesSeptic Arthritis and Prosthetic Joint Infection in Older AdultsajengmdNo ratings yet
- Practical 6 Microbes NEWDocument10 pagesPractical 6 Microbes NEWMohammad Shahid YaseenNo ratings yet
- Antib 2020 - LB Engl Prima Varianta Fara CorecturiDocument13 pagesAntib 2020 - LB Engl Prima Varianta Fara CorecturiIrina Panciu StefanNo ratings yet
- La Asuncion Montessori of Tagaytay Inc.: Patutong Malaki North, Tagaytay City Tel. No.: (046) 682 - 02 - 69Document4 pagesLa Asuncion Montessori of Tagaytay Inc.: Patutong Malaki North, Tagaytay City Tel. No.: (046) 682 - 02 - 69Cedrick PerenaNo ratings yet
- Citrus MaximaDocument11 pagesCitrus MaximanelisaNo ratings yet
- Multidrug Resistant Organisms in RSHS: Ida ParwatiDocument48 pagesMultidrug Resistant Organisms in RSHS: Ida Parwatiarief kurniawanNo ratings yet
- 86f4be500e7cac40b5b214de9577dd2eDocument31 pages86f4be500e7cac40b5b214de9577dd2e10-Gia KhôiNo ratings yet
- Lecture 2a-Primary MetabolitesDocument50 pagesLecture 2a-Primary Metabolitesurmeen04khanNo ratings yet
- VILSAN CatalougeDocument97 pagesVILSAN CatalougeSầu VeNo ratings yet
- Templet RKO FOPI 2021Document270 pagesTemplet RKO FOPI 2021Karin ArinciaNo ratings yet
- Jurnal Antibiotik 2Document11 pagesJurnal Antibiotik 2Achmad YunusNo ratings yet
- Arabjc D 22 01250 - R1Document50 pagesArabjc D 22 01250 - R1Gabriela LopesNo ratings yet
- Otitis Externa in Dogs Microbiology and 20151116-999-Z6r7ns-With-Cover-Page-V2Document6 pagesOtitis Externa in Dogs Microbiology and 20151116-999-Z6r7ns-With-Cover-Page-V2Yến KimNo ratings yet
- Questions RleDocument2 pagesQuestions RleKent AlveNo ratings yet
- Ashok MehraDocument40 pagesAshok MehraFahim UddinNo ratings yet
- CD 2022 FundaICN Starters Basic - PDF - FOR REVIEWERDocument15 pagesCD 2022 FundaICN Starters Basic - PDF - FOR REVIEWERMeryville JacildoNo ratings yet
- Garp-Nepal - Sa (Global Antibiotic Resistance Partnership)Document90 pagesGarp-Nepal - Sa (Global Antibiotic Resistance Partnership)Nivea VazNo ratings yet
- To Err Is Human: DR Inas Alassar CPHQDocument96 pagesTo Err Is Human: DR Inas Alassar CPHQYahya HashmiNo ratings yet
- Antibiotik Pada Infeksi Tropis (PERSI)Document42 pagesAntibiotik Pada Infeksi Tropis (PERSI)YULINo ratings yet
- Azlocillin Can Be The Potential Drug Candidate Against Drug-Tolerant Borrelia Burgdorferi Sensu Stricto JLB31Document15 pagesAzlocillin Can Be The Potential Drug Candidate Against Drug-Tolerant Borrelia Burgdorferi Sensu Stricto JLB31Lauge BrimgiestNo ratings yet