Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
1 viewsMyocardial Ischemia
Myocardial Ischemia
Uploaded by
Putu Bagus ArisadikaOMI jantung
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You might also like
- Unexpected Bone Resorption in Mentum ASIAN PATIENTSDocument9 pagesUnexpected Bone Resorption in Mentum ASIAN PATIENTSletty3gape100% (1)
- Anaesthesia For Cardiac DiseaseDocument26 pagesAnaesthesia For Cardiac DiseasePrabhu KumarNo ratings yet
- Cardiogenic ShockDocument20 pagesCardiogenic Shockanimesh pandaNo ratings yet
- Advance Stroke NursingDocument31 pagesAdvance Stroke NursingAlexisRoyENo ratings yet
- Controlled Hypotension: Moderator: DR V. Y. Srinivas Presenter: Dr. Ann Susan MathewDocument49 pagesControlled Hypotension: Moderator: DR V. Y. Srinivas Presenter: Dr. Ann Susan MathewAnn Susan MathewNo ratings yet
- Periodontal Treatment of Medically Compromised Patients2024Document47 pagesPeriodontal Treatment of Medically Compromised Patients202469alinabeel69No ratings yet
- Coronary Artery DiseaseDocument22 pagesCoronary Artery DiseaseMamoon Rashid100% (1)
- Stroke, Inc IcpDocument6 pagesStroke, Inc IcpJojo JustoNo ratings yet
- Neurogenic Shock in Critical Care NursingDocument25 pagesNeurogenic Shock in Critical Care Nursingnaqib25100% (4)
- III) Pharmacotherapy of Angina PectorisDocument23 pagesIII) Pharmacotherapy of Angina PectorisAyro Business CenterNo ratings yet
- Post-Cardiac Arrest CareDocument16 pagesPost-Cardiac Arrest CareJeremia KurniawanNo ratings yet
- Kardiogenik SyokDocument43 pagesKardiogenik SyokGalih Arief Harimurti WawolumajaNo ratings yet
- Nursing Mangement Client With Myocardial Infarction (Mi) Heart AttackDocument35 pagesNursing Mangement Client With Myocardial Infarction (Mi) Heart AttackTania Febria AzizahNo ratings yet
- SHOCKDocument17 pagesSHOCKChithra Saju100% (1)
- Cardiovascular Pharmacology: Ana Sharmaine S. Uera, MD DR PJGMRMC Anesthesiology Department 1st Year ResidentDocument68 pagesCardiovascular Pharmacology: Ana Sharmaine S. Uera, MD DR PJGMRMC Anesthesiology Department 1st Year ResidentLalay CabanagNo ratings yet
- Cardiogenic ShockDocument49 pagesCardiogenic Shockmaibejose0% (1)
- Patofisiologi Shock CardiogenicDocument44 pagesPatofisiologi Shock CardiogenicGalih Arief Harimurti Wawolumaja100% (1)
- Anesthesia For Electroconvulsive Therapy - UjoDocument17 pagesAnesthesia For Electroconvulsive Therapy - UjopujoNo ratings yet
- Heart Failure Dr. VishvasDocument31 pagesHeart Failure Dr. VishvasvishvasNo ratings yet
- Perioperative Management 1203114432600412 4Document53 pagesPerioperative Management 1203114432600412 4polushkyNo ratings yet
- Coronary Heart Disease: Angina Pectoris Myocardial InfarctionDocument44 pagesCoronary Heart Disease: Angina Pectoris Myocardial Infarctionalejandrino_leoaugustoNo ratings yet
- Journal Reading Circulatory Shock-1Document33 pagesJournal Reading Circulatory Shock-1bimanda aldoNo ratings yet
- Angiotensin I Angiotensin II, Angiotensin-Converting Enzyme (ACE) - Vasoconstrictor Angiotensin II Stimulates Aldosterone SecretionDocument11 pagesAngiotensin I Angiotensin II, Angiotensin-Converting Enzyme (ACE) - Vasoconstrictor Angiotensin II Stimulates Aldosterone SecretionAbdullah asadNo ratings yet
- Management of Hypertenisve Emergencies and Urgency: DR - Supriya 1 Year General MedicineDocument33 pagesManagement of Hypertenisve Emergencies and Urgency: DR - Supriya 1 Year General MedicineRahul NaniNo ratings yet
- Drugs of CvsDocument32 pagesDrugs of CvsAgus HaryantoNo ratings yet
- Angina Pectoris: Ischemic Heart DiseaseDocument17 pagesAngina Pectoris: Ischemic Heart DiseaseMahum SohailNo ratings yet
- СердечнаяDocument70 pagesСердечнаяDaniel FunkNo ratings yet
- Shock FinalDocument90 pagesShock Finalمجاهد إسماعيل حسن حسينNo ratings yet
- Anesthesia For Carotid EndarterectomyDocument89 pagesAnesthesia For Carotid EndarterectomyChavdarNo ratings yet
- Heart Failure DrugsDocument35 pagesHeart Failure Drugszmr27146No ratings yet
- Care of Patient With CADDocument22 pagesCare of Patient With CADBader ZawahrehNo ratings yet
- Kee: Pharmacology, 8th EditionDocument5 pagesKee: Pharmacology, 8th EditionLondera BainNo ratings yet
- Vasoactive TherapyDocument26 pagesVasoactive Therapylidya agustin100% (1)
- Vasoactive TherapyDocument26 pagesVasoactive Therapylidya agustinNo ratings yet
- Drugs For CHF & Angina PDFDocument15 pagesDrugs For CHF & Angina PDFAbdullah ElsayedNo ratings yet
- Care and Management of The Client With Cardiac Alterations: Presented By: Jessaly Joyce SiosonDocument38 pagesCare and Management of The Client With Cardiac Alterations: Presented By: Jessaly Joyce SiosonJoyce SiosonNo ratings yet
- Antihypertensive & Antianginal DrugsDocument5 pagesAntihypertensive & Antianginal Drugsdomememe1No ratings yet
- Antianginal Drugs RevisedDocument36 pagesAntianginal Drugs RevisedpradeephdNo ratings yet
- Hypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Document81 pagesHypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Alan K MhamadNo ratings yet
- Acute Coronary SyndromeDocument30 pagesAcute Coronary SyndromeEndar EszterNo ratings yet
- Acute Coronary Syndrome (ACS)Document20 pagesAcute Coronary Syndrome (ACS)Benjiber R. SilvaNo ratings yet
- Chapter 37 Cardiac Glycosides Antianginals and AntidysrhythmicsDocument5 pagesChapter 37 Cardiac Glycosides Antianginals and AntidysrhythmicsErika Joy Cabison TamayoNo ratings yet
- CH17 Cardiac Surgery in The Adult 5th Edition 2018Document26 pagesCH17 Cardiac Surgery in The Adult 5th Edition 2018ChengShiun ShiueNo ratings yet
- Pemicu 1 KGD: Muhammad Fahmi Rosyadi 405140220Document137 pagesPemicu 1 KGD: Muhammad Fahmi Rosyadi 405140220fahmi rosyadiNo ratings yet
- Cardiovascular Disease and Anaesthesia: HypertensionDocument4 pagesCardiovascular Disease and Anaesthesia: Hypertensionsatria wibawaNo ratings yet
- Antiarrhythmic DrugsDocument57 pagesAntiarrhythmic Drugsrossfancy736No ratings yet
- Neurologic Function Cerebrovascular DisordersDocument15 pagesNeurologic Function Cerebrovascular DisordersBalilea, Derwin Stephen T.No ratings yet
- Unit - 3.2 - Ahn-ShockDocument36 pagesUnit - 3.2 - Ahn-ShockAnnu DudiNo ratings yet
- SID For 4th YrsDocument76 pagesSID For 4th YrsABREHAM BUKULONo ratings yet
- Cardiogenic ShockDocument2 pagesCardiogenic ShockChristine QuironaNo ratings yet
- Ischemic Heart DiseaseDocument83 pagesIschemic Heart DiseaseAseelNo ratings yet
- Angina PectorisDocument17 pagesAngina PectorisRacel HernandezNo ratings yet
- Continuation (Altered Tissue Perfusion)Document59 pagesContinuation (Altered Tissue Perfusion)Grace Jane DionaldoNo ratings yet
- Cardivascular DrugsDocument27 pagesCardivascular DrugsYounas BhattiNo ratings yet
- Hypertension and AnaesthesiaDocument3 pagesHypertension and AnaesthesiaVerico PratamaNo ratings yet
- Critical Care: Fajar Wahyu PribadiDocument19 pagesCritical Care: Fajar Wahyu PribadiAngkat Prasetya Abdi NegaraNo ratings yet
- Tugas DR Yoma AncaDocument30 pagesTugas DR Yoma Ancaaby mayuNo ratings yet
- Anesthesia For Intracranial Aneurysm Case FileDocument3 pagesAnesthesia For Intracranial Aneurysm Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Intensive Care For The Critically Ill Adult: T.SunilkumarDocument47 pagesIntensive Care For The Critically Ill Adult: T.SunilkumarYamini ChowdaryNo ratings yet
- Critical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsNo ratings yet
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesFrom EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesRating: 5 out of 5 stars5/5 (1)
- Seminar Presentation On The Topic Rehabilitation CentersDocument13 pagesSeminar Presentation On The Topic Rehabilitation CentersIrshad HussainNo ratings yet
- Background of The Study: Anti - Thrombocytopenic Property of Sambong (Blumea Balsamifera) LeavesDocument31 pagesBackground of The Study: Anti - Thrombocytopenic Property of Sambong (Blumea Balsamifera) LeavesKrishan Carlos CredoNo ratings yet
- Concise DermatologyDocument279 pagesConcise DermatologyVivtor Silva100% (2)
- Drug Study DexamethasoneDocument4 pagesDrug Study Dexamethasoneamal abdulrahmanNo ratings yet
- Editing Exercise Read The Paragraph Below and Edit It For Punctuation and Grammar Mistakes. There Are Also Formality Errors That Need To Be CorrectedDocument3 pagesEditing Exercise Read The Paragraph Below and Edit It For Punctuation and Grammar Mistakes. There Are Also Formality Errors That Need To Be CorrectedMaiElGebaliNo ratings yet
- Nutrition Care ProcessDocument6 pagesNutrition Care ProcessGeraldine MaeNo ratings yet
- Locked in SyndromeDocument52 pagesLocked in SyndromeFarrukh Ali KhanNo ratings yet
- Lower Extremity Arterial Protocol 14 1Document2 pagesLower Extremity Arterial Protocol 14 1api-3494022400% (1)
- Afina Fitra Firdaus Ppds Ipd 50Document30 pagesAfina Fitra Firdaus Ppds Ipd 5050Afina Fitra FirdausNo ratings yet
- J Biochem Molecular Tox - 2020 - RavindranDocument11 pagesJ Biochem Molecular Tox - 2020 - RavindranMennatallah AliNo ratings yet
- PHYSICAL FITNESS TEST PFT SCORE SHEET FO-revisedDocument1 pagePHYSICAL FITNESS TEST PFT SCORE SHEET FO-revisedMary Grace DeramasNo ratings yet
- Seminars in Diagnostic Pathology: Mark R. WickDocument12 pagesSeminars in Diagnostic Pathology: Mark R. WickNancy ManriqueNo ratings yet
- FOURTH YEAR BSC NURSING Course Plan - For MergeDocument33 pagesFOURTH YEAR BSC NURSING Course Plan - For MergeBHUKYA USHARANI50% (2)
- Acrylic Partial DenturesDocument19 pagesAcrylic Partial Denturesahmad955mls100% (1)
- First Aid StrokeDocument11 pagesFirst Aid Strokeb4gsNo ratings yet
- GabapentinDocument4 pagesGabapentinElena MihalacheNo ratings yet
- Tracing:: ABILLAR, Rica MendozaDocument2 pagesTracing:: ABILLAR, Rica Mendozajzyryl abillarNo ratings yet
- Gestational Trophoblastic DiseaseDocument40 pagesGestational Trophoblastic DiseaseAayupta Mohanty100% (2)
- JurnalDocument7 pagesJurnalAdy Adha NorsanieNo ratings yet
- Trace ElementsDocument5 pagesTrace ElementsFaithNo ratings yet
- Al-Azhar Assiut Medical Journal Aamj, Vol 13, No 4, October 2015 Suppl-2Document6 pagesAl-Azhar Assiut Medical Journal Aamj, Vol 13, No 4, October 2015 Suppl-2Vincentius Michael WilliantoNo ratings yet
- Special Chemistry: Test Name Current Result Previous Result Unit Normal RangeDocument1 pageSpecial Chemistry: Test Name Current Result Previous Result Unit Normal RangeSyed Muhammad Rafay AhmedNo ratings yet
- CDC - Toxoplasmosis - BiologyDocument2 pagesCDC - Toxoplasmosis - BiologyReynalth Andrew SinagaNo ratings yet
- Sept 4, 2015Document8 pagesSept 4, 2015Deity CelleNo ratings yet
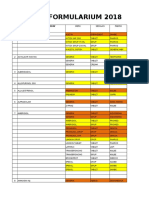
- Formularium Pengajuan 2018Document44 pagesFormularium Pengajuan 2018Nuri IriyaniNo ratings yet
- First Aid Cards: Fractures NosebleedsDocument2 pagesFirst Aid Cards: Fractures NosebleedsTasheenaNo ratings yet
- Fracture of Radius, Ulna, and HumerusDocument21 pagesFracture of Radius, Ulna, and HumeruspunikaNo ratings yet
- Dan CV WordDocument4 pagesDan CV WorddsnavarretteNo ratings yet
- Lyceum-Northwestern University College of Medicine Medicine 1 - Clinical Workshop 1 Topic-Back Pain Group-1Document9 pagesLyceum-Northwestern University College of Medicine Medicine 1 - Clinical Workshop 1 Topic-Back Pain Group-1Sachin KpNo ratings yet
Myocardial Ischemia
Myocardial Ischemia
Uploaded by
Putu Bagus Arisadika0 ratings0% found this document useful (0 votes)
1 views10 pagesOMI jantung
Original Title
Myocardial ischemia
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentOMI jantung
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
1 views10 pagesMyocardial Ischemia
Myocardial Ischemia
Uploaded by
Putu Bagus ArisadikaOMI jantung
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 10
Intraoperative Management
• Goals are to prevent myocardial ischemia
by optimizing
myocardial oxygen supply and reducing myocardial oxygen
demand and to monitor for and treat ischemia.
• Avoid persistent and excessive changes in heart rate and systemic
blood pressure.
• A common recommendation is to keep the heart rate and blood
pressure within 20% of the normal awake value.
• Increased heart rate increases myocardial oxygen requirements
while decreasing supply because of decreased diastolic coronary
artery perfusion time.
• HTN results in increased myocardial oxygen demand that is only
partially offset by increased coronary perfusion pressure.
• Maintenance of the balance oxygen
between myocardial supply and demand specific
is technique
anesthetic more or drugsimportant than anesthesia
selected to produce the
and muscle relaxation.
Induction of
Anesthesia
• Many different induction drugs are appropriate.
• (Ketamine is an unlikely choice because it increases heart rate
and systemic blood pressure.)
• Myocardial ischemia may accompany the sympathetic nervous
system stimulation that results from direct laryngoscopy and
tracheal intubation.
• Short-duration direct laryngoscopy (≤ 15 seconds) and/or
administration of drugs to minimize the pressor response, such
as laryngotracheal lidocaine, intravenous lidocaine, esmolol,
and/or fentanyl, is indicated.
Maintenance of
Anesthesia
• Drug selection for maintenance of anesthesia is based in part on
the patient’s estimated left ventricular function.
• In patients with normal left ventricular function, controlled
myocardial depression with a volatile anesthetic (with or without
nitrous oxide) may minimize sympathetic nervous system activity
during intense stimulation.
• However, volatile agents can be detrimental if drug-induced
hypotension leads to decreases in coronary perfusion pressure.
• Equally acceptable is use of a nitrous oxide–opioid technique
with the addition of a volatile anesthetic to treat undesirable
increases in blood pressure at critical points.
Maintenance of
Anesthesia
• In patients with severely impaired left ventricular function,
opioids may be selected for maintenance of anesthesia.
• The addition of nitrous oxide, a benzodiazepine, or a low dose
volatile anesthetic should be considered because total amnesia
cannot be ensured with an opioid alone.
• Regional anesthesia is acceptable in patients with ischemic heart
disease, but decreases in blood pressure associated with epidural
or spinal anesthesia must be controlled.
Maintenance of Anesthesia
• Hypotension that exceeds 20% of the preblock blood pressure
should be treated promptly.
• Despite presumed benefits of regional anesthesia, the
postoperative cardiac morbidity and mortality are not
significantly different between general and regional anesthesia.
Choice of Muscle Relaxant
• Muscle relaxants with minimal or no effect on heart rate and
systemic blood pressure (vecuronium, rocuronium,
cisatracurium) are preferred.
• Histamine release and the resulting
pressure
decrease causedin by atracurium
blood are less desirable.
• Glycopyrrolate is preferred to atropine for the anticholinergic
component in combination therapy to reverse neuromuscular
blockade, because it is associated with less increase in heart
rate.
Monitoring
• Intraoperative monitoring should aim for early detection of
myocardial ischemia.
• However, most myocardial ischemia occurs in the absence of
hemodynamic alterations, so one should be cautious when
endorsing routine use of expensive or complex monitors to
detect myocardial ischemia.
Postoperative Management
1. Prevent or treat events that increase
demand, such as pain,
myocardial shivering, hypercarbia, sepsis.
oxygen
2. Avoid or treat conditions that lead to decreased myocardial
oxygen supply, such as anemia hypoxemia, hypovolemia,
hypotension.
3. Continue treatments in the perioperative period, such as β-
blockers, that reduce the risks of adverse cardiac events.
4. Manage the timing of weaning and tracheal extubation to
avoid detrimental alterations in blood pressure and heart
rate.
5. Continuous ECG monitoring is useful for
detecting
postoperative myocardial ischemia, which is often silent.
You might also like
- Unexpected Bone Resorption in Mentum ASIAN PATIENTSDocument9 pagesUnexpected Bone Resorption in Mentum ASIAN PATIENTSletty3gape100% (1)
- Anaesthesia For Cardiac DiseaseDocument26 pagesAnaesthesia For Cardiac DiseasePrabhu KumarNo ratings yet
- Cardiogenic ShockDocument20 pagesCardiogenic Shockanimesh pandaNo ratings yet
- Advance Stroke NursingDocument31 pagesAdvance Stroke NursingAlexisRoyENo ratings yet
- Controlled Hypotension: Moderator: DR V. Y. Srinivas Presenter: Dr. Ann Susan MathewDocument49 pagesControlled Hypotension: Moderator: DR V. Y. Srinivas Presenter: Dr. Ann Susan MathewAnn Susan MathewNo ratings yet
- Periodontal Treatment of Medically Compromised Patients2024Document47 pagesPeriodontal Treatment of Medically Compromised Patients202469alinabeel69No ratings yet
- Coronary Artery DiseaseDocument22 pagesCoronary Artery DiseaseMamoon Rashid100% (1)
- Stroke, Inc IcpDocument6 pagesStroke, Inc IcpJojo JustoNo ratings yet
- Neurogenic Shock in Critical Care NursingDocument25 pagesNeurogenic Shock in Critical Care Nursingnaqib25100% (4)
- III) Pharmacotherapy of Angina PectorisDocument23 pagesIII) Pharmacotherapy of Angina PectorisAyro Business CenterNo ratings yet
- Post-Cardiac Arrest CareDocument16 pagesPost-Cardiac Arrest CareJeremia KurniawanNo ratings yet
- Kardiogenik SyokDocument43 pagesKardiogenik SyokGalih Arief Harimurti WawolumajaNo ratings yet
- Nursing Mangement Client With Myocardial Infarction (Mi) Heart AttackDocument35 pagesNursing Mangement Client With Myocardial Infarction (Mi) Heart AttackTania Febria AzizahNo ratings yet
- SHOCKDocument17 pagesSHOCKChithra Saju100% (1)
- Cardiovascular Pharmacology: Ana Sharmaine S. Uera, MD DR PJGMRMC Anesthesiology Department 1st Year ResidentDocument68 pagesCardiovascular Pharmacology: Ana Sharmaine S. Uera, MD DR PJGMRMC Anesthesiology Department 1st Year ResidentLalay CabanagNo ratings yet
- Cardiogenic ShockDocument49 pagesCardiogenic Shockmaibejose0% (1)
- Patofisiologi Shock CardiogenicDocument44 pagesPatofisiologi Shock CardiogenicGalih Arief Harimurti Wawolumaja100% (1)
- Anesthesia For Electroconvulsive Therapy - UjoDocument17 pagesAnesthesia For Electroconvulsive Therapy - UjopujoNo ratings yet
- Heart Failure Dr. VishvasDocument31 pagesHeart Failure Dr. VishvasvishvasNo ratings yet
- Perioperative Management 1203114432600412 4Document53 pagesPerioperative Management 1203114432600412 4polushkyNo ratings yet
- Coronary Heart Disease: Angina Pectoris Myocardial InfarctionDocument44 pagesCoronary Heart Disease: Angina Pectoris Myocardial Infarctionalejandrino_leoaugustoNo ratings yet
- Journal Reading Circulatory Shock-1Document33 pagesJournal Reading Circulatory Shock-1bimanda aldoNo ratings yet
- Angiotensin I Angiotensin II, Angiotensin-Converting Enzyme (ACE) - Vasoconstrictor Angiotensin II Stimulates Aldosterone SecretionDocument11 pagesAngiotensin I Angiotensin II, Angiotensin-Converting Enzyme (ACE) - Vasoconstrictor Angiotensin II Stimulates Aldosterone SecretionAbdullah asadNo ratings yet
- Management of Hypertenisve Emergencies and Urgency: DR - Supriya 1 Year General MedicineDocument33 pagesManagement of Hypertenisve Emergencies and Urgency: DR - Supriya 1 Year General MedicineRahul NaniNo ratings yet
- Drugs of CvsDocument32 pagesDrugs of CvsAgus HaryantoNo ratings yet
- Angina Pectoris: Ischemic Heart DiseaseDocument17 pagesAngina Pectoris: Ischemic Heart DiseaseMahum SohailNo ratings yet
- СердечнаяDocument70 pagesСердечнаяDaniel FunkNo ratings yet
- Shock FinalDocument90 pagesShock Finalمجاهد إسماعيل حسن حسينNo ratings yet
- Anesthesia For Carotid EndarterectomyDocument89 pagesAnesthesia For Carotid EndarterectomyChavdarNo ratings yet
- Heart Failure DrugsDocument35 pagesHeart Failure Drugszmr27146No ratings yet
- Care of Patient With CADDocument22 pagesCare of Patient With CADBader ZawahrehNo ratings yet
- Kee: Pharmacology, 8th EditionDocument5 pagesKee: Pharmacology, 8th EditionLondera BainNo ratings yet
- Vasoactive TherapyDocument26 pagesVasoactive Therapylidya agustin100% (1)
- Vasoactive TherapyDocument26 pagesVasoactive Therapylidya agustinNo ratings yet
- Drugs For CHF & Angina PDFDocument15 pagesDrugs For CHF & Angina PDFAbdullah ElsayedNo ratings yet
- Care and Management of The Client With Cardiac Alterations: Presented By: Jessaly Joyce SiosonDocument38 pagesCare and Management of The Client With Cardiac Alterations: Presented By: Jessaly Joyce SiosonJoyce SiosonNo ratings yet
- Antihypertensive & Antianginal DrugsDocument5 pagesAntihypertensive & Antianginal Drugsdomememe1No ratings yet
- Antianginal Drugs RevisedDocument36 pagesAntianginal Drugs RevisedpradeephdNo ratings yet
- Hypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Document81 pagesHypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Alan K MhamadNo ratings yet
- Acute Coronary SyndromeDocument30 pagesAcute Coronary SyndromeEndar EszterNo ratings yet
- Acute Coronary Syndrome (ACS)Document20 pagesAcute Coronary Syndrome (ACS)Benjiber R. SilvaNo ratings yet
- Chapter 37 Cardiac Glycosides Antianginals and AntidysrhythmicsDocument5 pagesChapter 37 Cardiac Glycosides Antianginals and AntidysrhythmicsErika Joy Cabison TamayoNo ratings yet
- CH17 Cardiac Surgery in The Adult 5th Edition 2018Document26 pagesCH17 Cardiac Surgery in The Adult 5th Edition 2018ChengShiun ShiueNo ratings yet
- Pemicu 1 KGD: Muhammad Fahmi Rosyadi 405140220Document137 pagesPemicu 1 KGD: Muhammad Fahmi Rosyadi 405140220fahmi rosyadiNo ratings yet
- Cardiovascular Disease and Anaesthesia: HypertensionDocument4 pagesCardiovascular Disease and Anaesthesia: Hypertensionsatria wibawaNo ratings yet
- Antiarrhythmic DrugsDocument57 pagesAntiarrhythmic Drugsrossfancy736No ratings yet
- Neurologic Function Cerebrovascular DisordersDocument15 pagesNeurologic Function Cerebrovascular DisordersBalilea, Derwin Stephen T.No ratings yet
- Unit - 3.2 - Ahn-ShockDocument36 pagesUnit - 3.2 - Ahn-ShockAnnu DudiNo ratings yet
- SID For 4th YrsDocument76 pagesSID For 4th YrsABREHAM BUKULONo ratings yet
- Cardiogenic ShockDocument2 pagesCardiogenic ShockChristine QuironaNo ratings yet
- Ischemic Heart DiseaseDocument83 pagesIschemic Heart DiseaseAseelNo ratings yet
- Angina PectorisDocument17 pagesAngina PectorisRacel HernandezNo ratings yet
- Continuation (Altered Tissue Perfusion)Document59 pagesContinuation (Altered Tissue Perfusion)Grace Jane DionaldoNo ratings yet
- Cardivascular DrugsDocument27 pagesCardivascular DrugsYounas BhattiNo ratings yet
- Hypertension and AnaesthesiaDocument3 pagesHypertension and AnaesthesiaVerico PratamaNo ratings yet
- Critical Care: Fajar Wahyu PribadiDocument19 pagesCritical Care: Fajar Wahyu PribadiAngkat Prasetya Abdi NegaraNo ratings yet
- Tugas DR Yoma AncaDocument30 pagesTugas DR Yoma Ancaaby mayuNo ratings yet
- Anesthesia For Intracranial Aneurysm Case FileDocument3 pagesAnesthesia For Intracranial Aneurysm Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Intensive Care For The Critically Ill Adult: T.SunilkumarDocument47 pagesIntensive Care For The Critically Ill Adult: T.SunilkumarYamini ChowdaryNo ratings yet
- Critical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsNo ratings yet
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesFrom EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesRating: 5 out of 5 stars5/5 (1)
- Seminar Presentation On The Topic Rehabilitation CentersDocument13 pagesSeminar Presentation On The Topic Rehabilitation CentersIrshad HussainNo ratings yet
- Background of The Study: Anti - Thrombocytopenic Property of Sambong (Blumea Balsamifera) LeavesDocument31 pagesBackground of The Study: Anti - Thrombocytopenic Property of Sambong (Blumea Balsamifera) LeavesKrishan Carlos CredoNo ratings yet
- Concise DermatologyDocument279 pagesConcise DermatologyVivtor Silva100% (2)
- Drug Study DexamethasoneDocument4 pagesDrug Study Dexamethasoneamal abdulrahmanNo ratings yet
- Editing Exercise Read The Paragraph Below and Edit It For Punctuation and Grammar Mistakes. There Are Also Formality Errors That Need To Be CorrectedDocument3 pagesEditing Exercise Read The Paragraph Below and Edit It For Punctuation and Grammar Mistakes. There Are Also Formality Errors That Need To Be CorrectedMaiElGebaliNo ratings yet
- Nutrition Care ProcessDocument6 pagesNutrition Care ProcessGeraldine MaeNo ratings yet
- Locked in SyndromeDocument52 pagesLocked in SyndromeFarrukh Ali KhanNo ratings yet
- Lower Extremity Arterial Protocol 14 1Document2 pagesLower Extremity Arterial Protocol 14 1api-3494022400% (1)
- Afina Fitra Firdaus Ppds Ipd 50Document30 pagesAfina Fitra Firdaus Ppds Ipd 5050Afina Fitra FirdausNo ratings yet
- J Biochem Molecular Tox - 2020 - RavindranDocument11 pagesJ Biochem Molecular Tox - 2020 - RavindranMennatallah AliNo ratings yet
- PHYSICAL FITNESS TEST PFT SCORE SHEET FO-revisedDocument1 pagePHYSICAL FITNESS TEST PFT SCORE SHEET FO-revisedMary Grace DeramasNo ratings yet
- Seminars in Diagnostic Pathology: Mark R. WickDocument12 pagesSeminars in Diagnostic Pathology: Mark R. WickNancy ManriqueNo ratings yet
- FOURTH YEAR BSC NURSING Course Plan - For MergeDocument33 pagesFOURTH YEAR BSC NURSING Course Plan - For MergeBHUKYA USHARANI50% (2)
- Acrylic Partial DenturesDocument19 pagesAcrylic Partial Denturesahmad955mls100% (1)
- First Aid StrokeDocument11 pagesFirst Aid Strokeb4gsNo ratings yet
- GabapentinDocument4 pagesGabapentinElena MihalacheNo ratings yet
- Tracing:: ABILLAR, Rica MendozaDocument2 pagesTracing:: ABILLAR, Rica Mendozajzyryl abillarNo ratings yet
- Gestational Trophoblastic DiseaseDocument40 pagesGestational Trophoblastic DiseaseAayupta Mohanty100% (2)
- JurnalDocument7 pagesJurnalAdy Adha NorsanieNo ratings yet
- Trace ElementsDocument5 pagesTrace ElementsFaithNo ratings yet
- Al-Azhar Assiut Medical Journal Aamj, Vol 13, No 4, October 2015 Suppl-2Document6 pagesAl-Azhar Assiut Medical Journal Aamj, Vol 13, No 4, October 2015 Suppl-2Vincentius Michael WilliantoNo ratings yet
- Special Chemistry: Test Name Current Result Previous Result Unit Normal RangeDocument1 pageSpecial Chemistry: Test Name Current Result Previous Result Unit Normal RangeSyed Muhammad Rafay AhmedNo ratings yet
- CDC - Toxoplasmosis - BiologyDocument2 pagesCDC - Toxoplasmosis - BiologyReynalth Andrew SinagaNo ratings yet
- Sept 4, 2015Document8 pagesSept 4, 2015Deity CelleNo ratings yet
- Formularium Pengajuan 2018Document44 pagesFormularium Pengajuan 2018Nuri IriyaniNo ratings yet
- First Aid Cards: Fractures NosebleedsDocument2 pagesFirst Aid Cards: Fractures NosebleedsTasheenaNo ratings yet
- Fracture of Radius, Ulna, and HumerusDocument21 pagesFracture of Radius, Ulna, and HumeruspunikaNo ratings yet
- Dan CV WordDocument4 pagesDan CV WorddsnavarretteNo ratings yet
- Lyceum-Northwestern University College of Medicine Medicine 1 - Clinical Workshop 1 Topic-Back Pain Group-1Document9 pagesLyceum-Northwestern University College of Medicine Medicine 1 - Clinical Workshop 1 Topic-Back Pain Group-1Sachin KpNo ratings yet