Professional Documents
Culture Documents
6 Posning
6 Posning
Uploaded by
Waaqoo Guutuu Waaqoo Guutuu0 ratings0% found this document useful (0 votes)
2 views38 pagesPosning
Original Title
6 POSNING
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPosning
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
2 views38 pages6 Posning
6 Posning
Uploaded by
Waaqoo Guutuu Waaqoo GuutuuPosning
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 38
FIRST AID FOR
POISONED VICTIMS
Basic First Aid June, 2021 © Haramaya University, CHMS,
By:- Ame Mehadi (BSc, MSc) Department of Emergency and Critical Care Nursing
Definitions
• A poison is a substance which may cause temporary or permanent
damage, if taken in to the body in sufficient quantity
• Once in the body, they may inter the bloodstream and be carried to
all organs and tissues.
• A poison is any substance solid, liquid or gas that tends to impair
health or cause death when introduced in to the body or on to the
skin surface.
• Small children are especially likely to become poisoned since they
tend to put in their mouths nearly everything that they pick up.
• However, adults are subject to poisoning.
06/30/2024 DR DEREJE WAKGARI
Types of poisoning agents
• Man–made,
• such as chemicals and drugs
• found in the home as well as in industry.
• Natural
• poisonous plants that may irritate the skin or cause more
serious symptoms if ingested,
• various insects and creatures produce venom in their bites
and stings.
06/30/2024 DR DEREJE WAKGARI
Frequent causes of poisoning
• Poisons transferred from original containers to other containers or
soft drink bottles.
• Carelessness
• Improper storage
• Improper disposal
• Improper handling of spray equipment including
• the mixing of pesticides, insecticides and herbicides (weed killers).
06/30/2024 DR DEREJE WAKGARI
Examples of poisons around the home
• Poisonous substances with in the home env’t are extremely prevalent.
• A few typical household poisons are:
• Cosmetics and hair preparations
• Gasoline, kerosene and other petroleum products.
• Paint and turpentine
• Strong detergents • Ways in which poisoning may occur
• Bleaches
• Cleaning solutions – Through the mouth (by ingestion)
• Acids – Through the skin (by absorption)
• Ammonia
– Through the lung (by inhalation)
• Poisonous plants
• Non edible mushrooms – Through the subcutaneous (by injection)
• DDT
• Malathine
06/30/2024 DR DEREJE WAKGARI
TYPES OF POISONS
• Swallowed Poison
• Enters the body through the mouth, lips, esophagus, or stomach.
• Drinking bleach is an example of swallowed poisoning.
• Absorbed Poison
• Enters the body through the skin.
• Plants (such as poison ivy) and chemicals can cause absorbed
poisoning.
• Injected Poison
• Enters the body through bites or stings or as drugs injected with a
needle.
• Inhaled Poison
• Is breathed into the body.
• Breathing in CO from a car’s exhaust is an example of inhaled
poisoning.
06/30/2024 DR DEREJE WAKGARI
General Signs and Symptoms of Poisoning
• S/Sx of poisoning vary greatly.
• The following aids in determining whether or not a victim is poisoned:
• Information from the victim or from an observer.
• Presence of a container known to contain poison.
• an open or spilled container,
• Conditions of the victim
• sudden onset of pain or illness.
• Burns around the lips or mouth.
• a strange breath odor
• an unusual odor,
• Pupils condition (contracted Vs dilated) or
• other people in the area who are also ill.
06/30/2024 DR DEREJE WAKGARI
General Care for Poisoning
• If you think that a person has been poisoned, try to find out the
following key points so that you and others can give the most
appropriate care:
• The type of poison
• The quantity taken
• When it was taken
06/30/2024 DR DEREJE WAKGARI
General Care for Poisoning……
• General first aid care tips for poisoning include the following:
• Check safety
• Check ABCs and responsiveness
• Calling EMS
• Limit further exposure by moving either the person or the source of the poison.
• If the poison’s container is found nearby, give the information from the label to
the Poison Control Centre or EMS dispatcher.
• Do not give the person anything to eat or drink unless an EMS dispatcher or
Poison Control Centre staff member tells you to do so.
• If you do not know what the poison was and the person vomits, save a sample
to give to EMS personnel.
06/30/2024 DR DEREJE WAKGARI
Swallowed Poisons
• The following may indicate that a poisonous substance has been
swallowed:
• An open container of poison nearby
• Burns around the mouth
• Increased production of saliva or saliva that is an abnormal color
• Abdominal cramps, vomiting, or diarrhea
• Seizures
• Dizziness or drowsiness
• Unresponsiveness
• A burning sensation in the mouth, throat, or stomach
06/30/2024 DR DEREJE WAKGARI
Swallowed Poisons ……
• First Aid Measures
• Check safety
• Check ABCs and responsiveness
• If responsive &/alert, and ABCs are unaffected, call the local Poison Control
Centre.
• Call EMS if an altered level of responsiveness or difficulty breathing.
• If the person is not breathing, start CPR.
• Use a barrier device so that you don’t contaminate yourself with the poison.
• Check the packaging of the poison, if possible, so that you know what it is.
• If the person needs to go to the hospital, bring a sample of the poison (or its
original container).
06/30/2024 DR DEREJE WAKGARI
Swallowed Poisons ……
• First aid measures for a conscious victim
• Remove the sources
• Give him a drink of tepid water
• Do not induce vomiting.
• Safe the label or container of the suspected poison for identification.
• First aid measures for a unconscious victim
• Maintain an open airway and administer artificial respiration.
• Don’t give fluids and don’t induce vomiting.
• If the victim is vomiting, position him and turn the head so that the vomitus drains out of
the mouth.
• Safe the label or container of the suspected poison for identification.
• If the victim vomits safe a sample of the vomited material for analysis.
06/30/2024 DR DEREJE WAKGARI
Absorbed Poisons
• The following signs and symptoms can indicate
that a poisonous substance has been absorbed:
• Rash or hives (raised, itchy areas of skin)
• Burning or itching skin
• Swelling
• Blisters
• Burns
• Unresponsiveness
Basic First Aid June, 2021 © Haramaya University, CHMS,
By:- Ame Mehadi (BSc, MSc) Department of Emergency and Critical Care Nursing
Absorbed Poisons
• First Aid Measures
• Check safety
• Check ABCs and responsiveness
• Call EMS if an altered level of responsiveness or difficulty
breathing.
• If the person is not breathing, start CPR.
• If the poison is a dry powder, brush it off the person’s skin.
• Be careful to avoid contaminating yourself.
• Remove any clothing or items covered in the poison.
• Flush the skin with running water for at least 15 minutes.
• To prevent any further injury, make sure the water flushes away
from any unaffected areas of the body.
Basic First Aid June, 2021 © Haramaya University, CHMS,
By:- Ame Mehadi (BSc, MSc) Department of Emergency and Critical Care Nursing
Contact poisoning
• Harsh chemicals and corrosive poisons if spilled on the skin produce
chemical burns which require immediate action.
• First Aid for Contact Poisons chemicals
• Remove the contaminated clothing immediately,
• Immerse and flushes the affected skin with large amounts of water.
• If poisoning is from a pesticide, a corrosive substance (strong acid or alkali),
send for ambulance immediately.
• Keep the victims air way open, give artificial respiration if indicated
• Do not leave the victim alone.
06/30/2024 DR DEREJE WAKGARI
Contact with Poisonous Plants
• The majority of skin reactions following contact with offending plants
is allergic in nature and is ch’zed by:
• General symptoms of headache and fever
• Itching
• Redness
• Rash
• First Aid Measures for Poisonous Plants.
• Remove contaminated clothing.
• Wash all exposed areas thoroughly with water.
• Seek medical advice if a severe reaction occurs or if there is a known history
of previous sensitivity.
06/30/2024 DR DEREJE WAKGARI
Inhaled Poisons
• The following may indicate that a poisonous
substance has been inhaled:
• Breathing difficulties
• Irritated eyes, nose, or throat
• Dizziness
• Vomiting
• Seizures
• Bluish color around the mouth
• Unresponsiveness
• An unusual smell in the air
Basic First Aid June, 2021 © Haramaya University, CHMS,
By:- Ame Mehadi (BSc, MSc) Department of Emergency and Critical Care Nursing
Inhaled Poisons……
• First Aid Measures
• Check safety
• Check ABCs and responsiveness
• If responsive&/alert and ABCs are unaffected, call the local Poison Control
Centre.
• Call EMS if altered level of responsiveness or difficulty breathing.
• If the person is not breathing, start CPR.
• Use a barrier device so that you don’t contaminate yourself with the poison.
• Get the person into fresh air but do not enter into a hazardous atmosphere in
order to do so.
• Inhaled poisons can affect everyone in an area.
• Stay out of the area if you suspect that the poison may still be in the air.
06/30/2024 DR DEREJE WAKGARI
Bites and stings
• Domestic pets cause most animal bites.
• Dogs are more likely to bite than cats.
• Rabies is more common in bats, raccoons, skunks and foxes than in cats and dogs.
• Human bites carry only a small risk of transmitting the hepatitis or HIV/AIDS viruses.
• Signs and Symptoms
• Wound and bleeding
• Redness at or around the bite sit
• Swelling
• Pus/drainage from the wound
• Increasing pain
• Localized warmth at the bite site
Wound by animal bite
• Red streaks leading away from the site of the bite.
06/30/2024 DR DEREJE WAKGARI
Bites and stings
• First aid measures
• Wash the bite wound thoroughly with soap and warm water
• to minimize the risk of infection.
• Raise and support the wound and cover dry with clean gauze swabs.
• Then cover with a sterile wound dressing.
• Arrange to take or send the casualty to the hospital if the bite breaks the skin;
• many will require antibiotics.
• If the animal's owner is available, find out if the animal's rabies shots are up to
date.
• Give this information to health care provider.
• If there is any risk of rabies infection, antirabies is recommend Tx.
• If the person's immunizations are not up to date, tetanus shot will be given.
06/30/2024 DR DEREJE WAKGARI
Snake Bites
• There are d/t kinds of poisonous snakes in d/t parts of the world
• All rxns from poisonous snake bites is aggravated by acute fear
and anxiety.
• Most deaths from venomous snakebites occur because:
• Too much time passed before the person received medical care.
• The person had an allergic reaction to the venom.
• The snake bite compounded an existing health condition in the
person.
• Factors affecting the outcome of poisonous snake bite:
• Type of snake
• the amount of venom injected
• the speed of absorption of the venom in to the victim circulation.
• Location of the bite
• Specific anti venom therapy as soon as possible
Basic First Aid June, 2021 © Haramaya University, CHMS,
By:- Ame Mehadi (BSc, MSc) Department of Emergency and Critical Care Nursing
Snake Bites
• Signs and symptoms of a possibly venomous snakebite include:
• A pair of puncture wounds in the skin
• Localized redness of the skin
• Pain and swelling in the area of the bite
• Major S/Sx
• Extremely painful,
• Rapid swelling
• General discoloration of the skin
• general weakness
• rapid pulse,
• nausea and vomiting,
• shortness of breath dimness of vision and shock.
• blurred vision, dropping eye lids,
• slurred speech, increased saliva and sweating,
• difficult, paralysis, convulsion and possible development of coma.
06/30/2024 DR DEREJE WAKGARI
Snake Bites
• Objectives of first aid
• To reduce the circulation of blood through the bite area
• To delay absorption of venom.
• To prevent aggravation of the local wound
• to sustain respiration
06/30/2024 DR DEREJE WAKGARI
Snake Bites
• First Aid Measures
• Check safety
• Check ABCs and responsiveness
• Call EMS.
• If you are not sure whether the snakebite was caused by a venomous snake,
call EMS anyway.
• Do not wait for life-threatening signs and symptoms of poisoning to appear.
• Before providing care, ensure that the snake is no longer present.
06/30/2024 DR DEREJE WAKGARI
Snake Bites
• First Aid Measures
• If you see the snake, remember what it looks like so that you can describe it
to EMS personnel.
• This information will help them provide the most appropriate treatment.
• Never attempt to capture or handle a potentially venomous snake.
• Keep the injured site still and level with the heart, if possible.
• If the bite is on a limb, remove any jewellery or tight clothing from the limb
and watch for swelling.
• Wash the wound with water.
• Cover the bite with a clean, dry dressing.
06/30/2024 DR DEREJE WAKGARI
Snake Bites
• First Aid Measures
• The most important step is to get a snake bite victim to hospital quickly.
• Meanwhile. Keep the victim from moving around
• Calm the victim
• Immobilize the bitten extremity and keep it at or below the heart level.
• Apply a firm but not tight cord just above the bite.
• Wipe the wound of venom which may have spilled from the fangs at the time
of biting.
06/30/2024 DR DEREJE WAKGARI
Snake Bites
• Cautions:
• Do NOT allow them to become over-exerted. If necessary, carry them to
safety.
• Do NOT apply a tourniquet or cold compresses to a snake bite.
• Do NOT cut into a snake bite with a razor & suck out the venom by mouth.
• Do NOT give the person stimulants or pain medicines unless prescribed.
• Do NOT give the person anything by mouth.
• Do NOT raise the site of the bite above the level of the person's heart
06/30/2024 DR DEREJE WAKGARI
DOG BITES
• Dog bites can cause cuts in the skin, bruising, crush injuries or
punctures.
• Animal quarantine is required if rabies• status is unknown..
S & Sx on human bitten by dog with rabies
– Pain
Likely OF
• • SIGNS to require antibiotic
A DOG WITH RABIESTx – Wound (teeth marks)
– Dog becomes wild – Restlessness
– Behaves like a dog
– Restlessness – Loss of appetite
– Foam around the mouth – Thirst
– Loss of body weight
– May die between 4–7 days
– Fever
after biting
06/30/2024 DR DEREJE WAKGARI
DOG BITES
• First aid measure
1. Stay Safe and Secure the dog or the victim
2. practice universal precautions and wear personal protective equipment if available.
3. Control any bleeding
4. Clean the wound with soap and warm water.
5. Don’t cover the wound
6. Always refer the victims to the hospital for medical attention if…………
• Any unidentified dog runs the risk of carrying rabies.
• If the dog cannot be identified and the owner cannot show proof of rabies vaccination, the victim must seek
medical attention.
• Rabies is always fatal to humans if not treated.
7. Watch for signs of infection:
• Redness & Swelling
• Heat &Weeping pus
06/30/2024 DR DEREJE WAKGARI
Dog Bite
• wash the wound with soap and running water & cover with a dry dressing.
• Do not suture or stitch the wound
• Immediate transport to health facility
• TAT is required.
• The owner of the dog or a Veterinarian should be informed immediately to check for
symptoms of rabies.
• Ask if the dog has stopped eating ordinary food, barks in unusual ways and Saliva runs
out of mouth.
• The dog should not be killed, but should be kept under observation for 10-15 days to
see whether it develops symptoms of rabies.
• If there is a suspicion of the dog being infected with rabies, it is better to take the
course of anti-rabies Tx to provide immunity against the disease.
06/30/2024 DR DEREJE WAKGARI
Insect Stings
• merely uncomfortable.
• However, allergic rxns & anaphylaxis are always a concern.
• Some insects, such as bees, leave their stingers embedded in the person’s skin.
• Others, such as wasps, can sting multiple times, but leave no stinger behind.
• What to Look For?
• The following can indicate an insect sting, especially if you see insects nearby:
• Quick, sharp pain at the site of the sting
• Pain, redness, or swelling at the site of the sting
• A stinger embedded in the skin
• Check the sting site to see if a stinger and venom sac are embedded in the skin.
• Reactions generally localized pain, itching, and swelling.
• Allergic reaction (anaphylaxis), if occurs, will be a life threatening.
06/30/2024 DR DEREJE WAKGARI
• First aid measures
• If the stinger is still in the person’s skin, remove it by scraping it away from the skin.
• Use a plastic card (such as a debit card) to do this.
• Wash the area with clean water.
• Cover the site with an adhesive bandage.
• Apply ice or a cold pack to help control swelling. Put a thin cloth between the cold source
and the person’s skin to avoid freezing the skin.
• Continue to watch for signs of infection, an allergic reaction, or anaphylaxis.
• Prevention
• To reduce the risk of insect stings:
• Wear a long-sleeved shirt, long pants, and closed-toe shoes.
• Don’t wear perfume, cologne, or other products with strong scents.
• Remove or cover items that will attract insects, such as garbage or food.
06/30/2024 DR DEREJE WAKGARI
• First aid measures
• Call EMS if there are any signs of a severe allergic reaction.
• Ask the victim if he/she has had a reaction before.
• Bees are the only stinging insects that leave their stingers
and venom sacs behind.
• Scrape the stinger and venom sac away with a hard object
such as a long fingernail, credit card, scissor edge, or knife
blade.
• Wash the sting site with soap and water to prevent
infection.
• Apply an ice pack over the sting site to slow absorption of
the venom and relieve pain.
• Because bee venom is acidic, a paste made of baking soda
and water can help.
• Seek medical attention if necessary.
Basic First Aid June, 2021 © Haramaya University, CHMS,
By:- Ame Mehadi (BSc, MSc) Department of Emergency and Critical Care Nursing
Stings from Marine Life
• Many forms of marine life (e.g., jellyfish,
stingrays, sea urchins, stinging coral, and spiny
fish) cause stinging wounds.
• In Canada, stings from marine life are usually
from jellyfish, though stingrays can also cause
injury.
• Stings from marine life can have effects that
range from merely painful to potentially life-
threatening.
Abdominal thrusts
Basic First Aid June, 2021 © Haramaya University, CHMS,
By:- Ame Mehadi (BSc, MSc) Department of Emergency and Critical Care Nursing
Stings from Marine Life
• The signs and symptoms of a sting from marine
life include the following:
• Pain
• Rash
• Redness
• Swelling
• Puncture wounds
• Lacerations
Abdominal thrusts
Basic First Aid June, 2021 © Haramaya University, CHMS,
By:- Ame Mehadi (BSc, MSc) Department of Emergency and Critical Care Nursing
Stings from Marine Life
• First Aid measures
• Check ABCs
• Call EMS if the person is having airway or breathing problems, the person was
stung on the face or neck, or you do not know what caused the sting.
• To care for a person who has been stung by a jellyfish:
• Get the person out of the water as soon as possible.
• Flush the injured area with vinegar for at least 30 seconds to
counteract the toxin.
• If vinegar is not available, mix baking soda and water into a
paste and leave it on the area for 20 minutes.
06/30/2024 DR DEREJE WAKGARI
Stings from Marine Life
• First Aid measures
• While wearing gloves or using a towel, carefully remove any stingers,
tentacles, or pieces of the animal.
• Immerse the affected area in water as hot as the person can tolerate
(no more than about 45°C (113°F)) for at least 20 minutes or until the
pain is relieved.
• If hot water is not available, use dry hot packs, or, as a second choice,
dry cold packs to help decrease the pain.
• Remember to wrap the hot or cold packs in a thin, dry towel or
cloth to protect the skin.
• Do not rub the area or apply a bandage.
06/30/2024 DR DEREJE WAKGARI
06/30/2024 DR DEREJE WAKGARI
You might also like
- The Secret of Being HappyDocument282 pagesThe Secret of Being Happylcs1234678100% (4)
- Orthopaedic Physiotherapy Assessment Chart For Physiotherapists by Dr. Krishna N. SharmaDocument7 pagesOrthopaedic Physiotherapy Assessment Chart For Physiotherapists by Dr. Krishna N. SharmaDr. Krishna N. Sharma86% (58)
- Project Report On Sugarcane Plantation and Organic Jaggery Plant (100 TCD)Document8 pagesProject Report On Sugarcane Plantation and Organic Jaggery Plant (100 TCD)EIRI Board of Consultants and Publishers100% (2)
- Encyclopedia of Metagenomics 2015 PDFDocument766 pagesEncyclopedia of Metagenomics 2015 PDFJordan RuizNo ratings yet
- Gestational Diabetes Case Study With Questions For The Undergraduate NurseDocument46 pagesGestational Diabetes Case Study With Questions For The Undergraduate NurseAndrea Donmyer100% (1)
- First Aid: PoisoningDocument82 pagesFirst Aid: PoisoningSmaili TotoNo ratings yet
- Spraying Pesticides HazardDocument15 pagesSpraying Pesticides HazardJulio PutraNo ratings yet
- Chapter 3.exposure To Biological Hazards, Poison, Hypoxia, ChokingDocument36 pagesChapter 3.exposure To Biological Hazards, Poison, Hypoxia, ChokingHayat AL AKOUMNo ratings yet
- Poisoning and Its ManagementDocument25 pagesPoisoning and Its ManagementAnant kushwahaNo ratings yet
- ABSORPTIONDocument6 pagesABSORPTIONtantan sisonNo ratings yet
- PoisoningDocument17 pagesPoisoningdoctorshimaa147No ratings yet
- 2.9.poisonus AidDocument96 pages2.9.poisonus AidSufian MohammedNo ratings yet
- ToxicologyDocument42 pagesToxicologyJefferson OrgaNo ratings yet
- Toxicology: General Nursing Management of Poisoning Emergencies EmergenciesDocument26 pagesToxicology: General Nursing Management of Poisoning Emergencies EmergenciesأمينةأحمدNo ratings yet
- Occupational First Aid Training: Other Emergencies - 2Document17 pagesOccupational First Aid Training: Other Emergencies - 2myco samNo ratings yet
- Spillage Response Awareness TrainingDocument27 pagesSpillage Response Awareness Trainingtsc.aambidNo ratings yet
- Acute Toxicity 2Document39 pagesAcute Toxicity 2Meraol HusseinNo ratings yet
- First Aids For PoisoningDocument11 pagesFirst Aids For PoisoningGysha Puna TemudNo ratings yet
- PoisoningDocument28 pagesPoisoningGysha Puna TemudNo ratings yet
- Poisoning First AidDocument13 pagesPoisoning First AidGerra Mae Tubio CandelasaNo ratings yet
- Pharmacotherapy Acid PoisoningDocument5 pagesPharmacotherapy Acid PoisoningMeera ChikhaleNo ratings yet
- Airborne-Precautions 081019Document1 pageAirborne-Precautions 081019Munir A MughalNo ratings yet
- Common 1 (Infection Control)Document46 pagesCommon 1 (Infection Control)kristaNo ratings yet
- Allergy, Bites and Stings 2021Document31 pagesAllergy, Bites and Stings 2021عبدالرحمن الحربيNo ratings yet
- Droplet Precautions - 221019Document2 pagesDroplet Precautions - 221019Gunawan iriantoNo ratings yet
- Lecture 5 First Aid and Antidotes Against Pesticides PoisoningDocument45 pagesLecture 5 First Aid and Antidotes Against Pesticides PoisoningMuhammad Shahrooz NaseerNo ratings yet
- PoisoningDocument103 pagesPoisoningC Hendra Wijaya100% (2)
- FS Poison PDFDocument1 pageFS Poison PDFBrad TennentNo ratings yet
- Chemical PoisoningDocument14 pagesChemical PoisoningpinkgirljojiNo ratings yet
- 1.first AidDocument50 pages1.first AidKamran NadeemNo ratings yet
- Disscussion On Q & ADocument16 pagesDisscussion On Q & AFARAH MAE MEDINANo ratings yet
- Novel Coronavirus Confirmed Case - What You Need To Know V1.3Document4 pagesNovel Coronavirus Confirmed Case - What You Need To Know V1.3Eddie GuoNo ratings yet
- Medical Emergencies - PoisoningDocument21 pagesMedical Emergencies - PoisoningbrentupdegraffNo ratings yet
- PoisoningDocument35 pagesPoisoningMUKESH SUNDARARAJANNo ratings yet
- Xiaolong Wang PHD Emergency Department The 2 Affiliated Hospital of CqmuDocument51 pagesXiaolong Wang PHD Emergency Department The 2 Affiliated Hospital of CqmuNidya PutrijNo ratings yet
- Drowning and PoisoningDocument26 pagesDrowning and PoisoningMihir Patel100% (1)
- Poisoning PPT Nursing FoundationDocument16 pagesPoisoning PPT Nursing FoundationMahimaNo ratings yet
- Gesta - SDS Ex 5Document6 pagesGesta - SDS Ex 5jlgestaNo ratings yet
- Created By: Ade Irma Dhea Fiften Mandeyka Gita Putri Kusumawardani Rafit Arjeni Veronika SulistianiDocument17 pagesCreated By: Ade Irma Dhea Fiften Mandeyka Gita Putri Kusumawardani Rafit Arjeni Veronika SulistianiAde IrmaNo ratings yet
- Presentasi Bahasa Inggris MSDS Kel. 2Document20 pagesPresentasi Bahasa Inggris MSDS Kel. 2Salim SanjayaNo ratings yet
- Poisoning: Drug OverdoseDocument34 pagesPoisoning: Drug Overdosejawad_ahmedNo ratings yet
- Standard First Aid and CPR/AEDDocument81 pagesStandard First Aid and CPR/AEDkumkang productionNo ratings yet
- Lab Safety TrainingDocument105 pagesLab Safety TrainingSabry SaidNo ratings yet
- Diseases/Sickness Resulting From Exposure To Decaying MaterialsDocument23 pagesDiseases/Sickness Resulting From Exposure To Decaying MaterialsManelyn TagaNo ratings yet
- Washing and LaundryDocument11 pagesWashing and LaundryLevi PosadasNo ratings yet
- Pesticides and Human Health: Pesticide Applicator Core Training ManualDocument34 pagesPesticides and Human Health: Pesticide Applicator Core Training ManualYohanes FirmansyahNo ratings yet
- Home Health CareDocument222 pagesHome Health CareMylody Villaflor Magallon100% (1)
- Title Layout: SubtitleDocument73 pagesTitle Layout: Subtitlenaila100% (1)
- Class Notes Element 7Document9 pagesClass Notes Element 7danish asrarNo ratings yet
- Webinar On Pandemic and DisasterDocument29 pagesWebinar On Pandemic and DisasterAdrian AbonNo ratings yet
- First Aid UpdatedDocument116 pagesFirst Aid UpdatedOmar SaturnoNo ratings yet
- IC Clinical StaffDocument41 pagesIC Clinical StaffphysioNo ratings yet
- Week 8and 9powerpoint SLP Forensic ChemistryDocument60 pagesWeek 8and 9powerpoint SLP Forensic ChemistrySheena De Guzman MorenoNo ratings yet
- CME - REC Part 2Document50 pagesCME - REC Part 2david battNo ratings yet
- BDS Practical Notebook.Document77 pagesBDS Practical Notebook.Hamda AnjumNo ratings yet
- Infection Control ModuleDocument16 pagesInfection Control ModuleKomite PpiNo ratings yet
- Universal Safety (Health) PrecautionsDocument61 pagesUniversal Safety (Health) Precautionstummalapalli venkateswara rao100% (2)
- Action at An EmergencyDocument37 pagesAction at An EmergencyDawn KleinNo ratings yet
- Presentation 2Document37 pagesPresentation 2Lav ZurcNo ratings yet
- A IntroductionDocument55 pagesA IntroductionYohanes FirmansyahNo ratings yet
- 2OlUJdeS78s9n2sL - 9q8JWPuUo-sLucxW-Public Health Training SlidesDocument29 pages2OlUJdeS78s9n2sL - 9q8JWPuUo-sLucxW-Public Health Training Slideskadek ayu ichaNo ratings yet
- Guidelines For People With COVID-19 Symptoms in MontrealDocument2 pagesGuidelines For People With COVID-19 Symptoms in MontrealamyluftNo ratings yet
- HHChapter 11 of Home Aid Care For Free (Education) YAAAYDocument85 pagesHHChapter 11 of Home Aid Care For Free (Education) YAAAYSamuel PerezNo ratings yet
- First Aid Cdrrmo 2019Document373 pagesFirst Aid Cdrrmo 2019fenan sollanoNo ratings yet
- Anthropology Power PointDocument63 pagesAnthropology Power PointWaaqoo Guutuu Waaqoo GuutuuNo ratings yet
- Antimicrobial Prophylaxis For Surgical ProceduresDocument60 pagesAntimicrobial Prophylaxis For Surgical ProceduresWaaqoo Guutuu Waaqoo GuutuuNo ratings yet
- Chapter Three: Theory of Consumer BehaviorDocument34 pagesChapter Three: Theory of Consumer BehaviorWaaqoo Guutuu Waaqoo GuutuuNo ratings yet
- Bayan XahaDocument6 pagesBayan XahaWaaqoo Guutuu Waaqoo GuutuuNo ratings yet
- Nurse-Led Empowerment Strategies For Patients With Hypertension: A Questionnaire SurveyDocument10 pagesNurse-Led Empowerment Strategies For Patients With Hypertension: A Questionnaire SurveyChristina Putri BongzueNo ratings yet
- Needle Temperature and PainDocument5 pagesNeedle Temperature and PainCici PatresiaNo ratings yet
- The Neurophysiology of Acupuncture - A Viewpoint PDFDocument10 pagesThe Neurophysiology of Acupuncture - A Viewpoint PDFgigicarvajalNo ratings yet
- Prof BSP - Neurologic Paraneoplastic SyndromesDocument122 pagesProf BSP - Neurologic Paraneoplastic SyndromesSavitha BasriNo ratings yet
- Presentation On Hepatic Failure: Presented By: Sandhya Harbola M.SC Nursing 1 Year PcnmsDocument54 pagesPresentation On Hepatic Failure: Presented By: Sandhya Harbola M.SC Nursing 1 Year PcnmsShubham Singh BishtNo ratings yet
- An Introduction To Haematopoiesis Prof Vernon Louw Clinical Haematology University of Cape TownDocument35 pagesAn Introduction To Haematopoiesis Prof Vernon Louw Clinical Haematology University of Cape TownAmmaarah IsaacsNo ratings yet
- Davidson's Self-Assessment in Medicine (Edited) PDFDocument111 pagesDavidson's Self-Assessment in Medicine (Edited) PDFAhMad MaGdyNo ratings yet
- Gamma World GM ScreenDocument14 pagesGamma World GM ScreenThe Lyon100% (7)
- Psychology Sham)Document5 pagesPsychology Sham)Rey MendozaNo ratings yet
- ENDO ThyroidDocument10 pagesENDO ThyroidHajime NakaegawaNo ratings yet
- Nina Kirana - Health Psychology - The Biopsychosocial and Spiritual Benefits of Fasting in DetailDocument8 pagesNina Kirana - Health Psychology - The Biopsychosocial and Spiritual Benefits of Fasting in DetailNina Kirana100% (1)
- Test Bank For Introduction To Medical Surgical Nursing 6th Edition Adrianne Dill LintonDocument24 pagesTest Bank For Introduction To Medical Surgical Nursing 6th Edition Adrianne Dill LintonStephanieCooperpkyf100% (47)
- Writing B1Document15 pagesWriting B1Khánh AnNo ratings yet
- DOH Citizen's Charter 2021 1st EditionDocument960 pagesDOH Citizen's Charter 2021 1st EditionCecibloom Shara Hiludo-CabreraNo ratings yet
- English Secondary 5Document6 pagesEnglish Secondary 5amilia2509No ratings yet
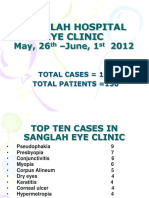
- SanglahDocument13 pagesSanglahIzzarIzzarNo ratings yet
- Dermal FillersDocument13 pagesDermal FillersAhmed Badawy100% (1)
- Rizal Did Not Really RetractedDocument4 pagesRizal Did Not Really RetractedMia Loren LimosNo ratings yet
- Training For A 5K: Lucozade RunningDocument3 pagesTraining For A 5K: Lucozade RunningKevin JordanNo ratings yet
- NWFile 491Document6 pagesNWFile 491Sachin BoradeNo ratings yet
- S. No. Audit Question Scoring I Design & Facilities: RetailDocument2 pagesS. No. Audit Question Scoring I Design & Facilities: Retailmnegm2890No ratings yet
- Paclitaxel HandoutDocument5 pagesPaclitaxel HandoutFikaNo ratings yet
- Import Requirements (NEW)Document15 pagesImport Requirements (NEW)Thiago NunesNo ratings yet
- A Universal Model of Diagnostic Reasoning.14Document7 pagesA Universal Model of Diagnostic Reasoning.14Emília SantocheNo ratings yet
- Difference Disability Medieval Islamic World: and in TheDocument169 pagesDifference Disability Medieval Islamic World: and in TheAnonymous k1NWqSDQiNo ratings yet